#eliminate medicare advantage
Text
youtube
😳
Please watch this!
#singlepayer sunday#eliminate medicare advantage#medicare disadvantage#universal healthcare#medicare for all#singlepayer#think for yourself#question everything#Youtube
48 notes
·
View notes
Text
By Jessica Corbett
Common Dreams
March 20, 2024
"Trump has tried to walk back his support for Social Security and Medicare cuts," said the head of Social Security Works. "This budget is one of many reasons why no one should believe him."
Defenders of Social Security and Medicare on Wednesday swiftly criticized the biggest caucus of Republicans in the U.S. House of Representatives for putting out a budget proposal for fiscal year 2025 that takes aim at the crucial programs.
The 180-page "Fiscal Sanity to Save America" plan from the Republican Study Committee (RSC) follows the release of proposals from Democratic President Joe Biden and U.S. House Budget Committee Chair Jodey Arrington (R-Texas)—who is leading the fight to create a fiscal commission for the programs that critics call a "death panel" designed to force through cuts.
The RSC document features full sections on "Saving Medicare" and "Preventing Biden's Cuts to Social Security," which both push back on the president's recent comments calling out Republican attacks on the programs that serve seniors.
The caucus plan promotes premium support for Medicare Advantage plans administered by private health insurance providers as well as changes to payments made to teaching hospitals. For Social Security, the proposal calls for tying retirement age to rising life expectancy and cutting benefits for younger workers over certain income levels, including phasing out auxiliary benefits.
The document also claims that the caucus budget "would promote trust fund solvency by increasing payroll tax revenues through pro-growth tax reform, pro-growth energy policy that lifts wages, work requirements that move Americans from welfare to work, and regulatory reforms that increase economic growth."
In a lengthy Wednesday statement blasting the RSC budget, Social Security Works president Nancy Altman pointed out that last week, former President Donald Trump, the presumptive Republican nominee to face Biden in the November election, "toldCNBC that 'there's a lot you can do' to cut Social Security."
"Everyone who cares about the future of these vital earned benefits should vote accordingly in November."
"Now, congressional Republicans are confirming the party's support for cuts—to the tune of $1.5 trillion. They are also laying out some of those cuts," Altman said. "This budget would raise the retirement age, in line with prominent Republican influencer Ben Shapiro's recent comments that 'retirement itself is a stupid idea.' It would make annual cost-of-living increases stingier, so that benefits erode over time. It would slash middle-class benefits."
"Perhaps most insultingly, given the Republicans' claim to be the party of 'family values,' this budget would eliminate Social Security spousal benefits, as well as children's benefits, for middle-class families. That would punish women who take time out of the workforce to care for children and other loved ones," she continued. "This coming from a party that wants to take away women's reproductive rights!"
The caucus, chaired by Rep. Kevin Hern (R-Okla.), included 285 bills and initiatives from 192 members in its budget plan—among them are various proposals threatening abortion care, birth control, and in vitro fertilization (IVF) nationwide.
"The RSC budget would also take away Medicare's new power to negotiate lower prices on prescription drugs, putting more money into the pockets of the GOP's Big Pharma donors," Altman warned. "And it accelerates the privatization of Medicare, handing it over to private insurance companies who have a long history of ripping off the government and delaying and denying care to those who need it."
"In recent days, Trump has tried to walk back his support for Social Security and Medicare cuts," she noted. "This budget is one of many reasons why no one should believe him. The Republican Party is the party of cutting Social Security and Medicare, while giving tax handouts to billionaires."
"The Democratic Party is the party of expanding Social Security and Medicare, paid for by requiring the ultrawealthy to contribute their fair share," Altman added. "Everyone who cares about the future of these vital earned benefits should vote accordingly in November."
Biden campaign communications director Michael Tyler also targeted the Republican presidential candidate while slamming the RSC plan, saying that "Donald Trump's MAGA allies in Congress made it clear today: A vote for Trump is a vote to make the MAGA 2025 agenda of cutting Social Security, ripping away access to IVF, and banning abortion nationwide a hellish reality."
"While Trump and his allies push forward their extreme agenda, the American people are watching," Tyler added, suggesting that the RSC proposal will help motivate voters to give Biden and Vice President Kamala Harris four more years in the White House.
86 notes
·
View notes
Text
If You Don't Know Medicare Advantage Is a Scam, You're Not Paying Attention
We’re on the edge of the open enrollment period for Medicare, and the Advantage scammers will be carpet-bombing America with advertisements over the next few months. Don't be fooled about what it is—and who is profiting.
Thom Hartmann
Oct 07, 2023
Common Dreams
President George W. Bush and Republicans (and a handful of on-the-take Democrats) in Congress created the Medicare Advantage scam in 2003 as a way of routing hundreds of billions of taxpayer dollars into the pockets of for-profit insurance companies.
Those companies, and their executives, then recycle some of that profit back into politicians’ pockets via the Citizens United legalized bribery loophole created by five corrupt Republicans on the Supreme Court.
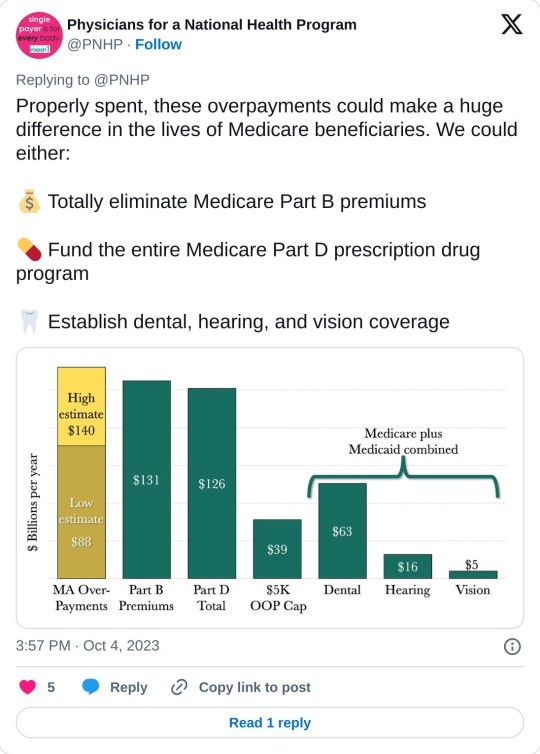
Just the overcharges happening right now in that scam are costing Americans over $140 billion a year: more than the entire budget for the Medicare Part B or Part D programs. These ripoffs — that our federal government seems to have no interest in stopping — are draining the Medicare trust fund while ensnaring gullible seniors in private insurance programs where they’re often denied life-saving care.
Real Medicare pays bills when they’re presented. Medicare Advantage insurance companies, on the other hand, get a fixed dollar amount every year for each of the people enrolled in their programs, regardless of how much they spent on each customer.
As a result, Medicare Advantage programs make the greatest profits for their CEOs and shareholders when they actively refuse to pay for care, something that happens frequently. It’s a safe bet that nearly 100 percent of the people who sign up for Advantage programs don’t know this and don’t have any idea how badly screwed they could be if they get seriously ill.
Not only that, when people do figure out they’ve been duped and try to get back on real Medicare, the same insurance companies often punish them by refusing to write Medigap plans (that fill in the 20% hole in real Medicare). They can’t do that when you first sign up when you turn 65, but if you “leave” real Medicare for privatized Medicare Advantage, it can be damn hard to get back on it.
The doctors’ group Physicians for a National Health Program (PNHP) just published a shocking report on the extent of the Medicare Advantage ripoffs — both to individual customers and to Medicare itself — that every American should know about.
The report, titled Our Payments, Their Profits, opens with this shocking exposé:
“By our estimate, and based on 2022 spending, Medicare Advantage overcharges taxpayers by a minimum of 22% or $88 billion per year, and potentially by up to 35% or $140 billion. By comparison, Part B premiums in 2022 totaled approximately $131 billion, and overall federal spending on Part D drug benefits cost approximately $126 billion. Either of these — or other crucial aspects of Medicare and Medicaid — could be funded entirely by eliminating overcharges in the Medicare Advantage program.
“Medicare Advantage, also known as MA or Medicare Part C, is a privately administered insurance program that uses a capitated payment structure, as opposed to the fee-for-service (FFS) structure of Traditional Medicare or TM. Instead of paying directly for the health care of beneficiaries, the federal government gives a lump sum of money to a third party (generally a commercial insurer) to ‘manage’ patient care.”
With real Medicare and a Medigap plan, you talk with your physician or hospital and decide on your treatment, they bill Medicare, and you never see or hear about the bill. There is nobody between you and your physician or hospital and Medicare only goes after the payment they’ve made if they sniff out a fraud.
With Medicare Advantage, on the other hand, your insurance company gets a lump-sum payment from Medicare every year and keeps the difference between what they get and what they pay out. They then insert themselves between you and your doctor or hospital to avoid paying for whatever they can.
Whatever you decide on regarding treatment, many Advantage insurance company will regularly second-guess and do everything they can to intimidate you into paying yourself out-of-pocket. Often, they simply refuse payment and wait for you to file a complaint against them; for people seriously ill the cumbersome “appeals” process is often more than they can handle.
As a result, hospitals and doctor groups across the nation are beginning to refuse to take Medicare Advantage patients. California-based Scripps Health, for example, cares for around 30,000 people on Medicare Advantage and recently notified all of them that Scripps will no longer offer medical services to them unless they pay out-of-pocket or revert back to real Medicare.
They made this decision because over $75 million worth of services and procedures their physicians had recommended to their patients were turned down by Medicare Advantage insurance companies. In many cases, Scripps had already provided the care and is now stuck with the bills that the Advantage companies refuse to pay.
Scripps CEO Chris Van Gorder told MedPage Today:
“We are a patient care organization and not a patient denial organization and, in many ways, the model of managed care has always been about denying or delaying care – at least economically. That is why denials, [prior] authorizations and administrative processes have become a very big issue for physicians and hospitals...”
Similarly, the Mayo Clinic has warned its customers in Florida and Arizona that they won’t accept Medicare Advantage any more, either. Increasing numbers of physician groups and hospitals are simply over being ripped off by Advantage insurance companies.
Not only is the Medicare Advantage scam a screw job for healthcare providers and people who are on the programs and are unfortunate enough to get sick, it’s also preventing Americans from getting expanded benefits from real Medicare.
As the PNHP report notes, for real Medicare to provide comprehensive vision, dental, and hearing benefits to all Medicare recipients would cost the system around $84 billion a year, according to the Congressional Budget Office.
Instead, though, the Medicare system is burdened with at least that amount of money in over-payments to Medicare Advantage providers — over-payments that have no health benefit whatsoever and merely inflate the companies’ profits.
A hundred billion dollars in excess profits can be put to a lot of uses, and the health insurance industry is quite good at it. The former CEO of UnitedHealth, “Dollar” Bill McGuire, for example, made off with over $1.5 billion dollars for his efforts.
And, because five corrupt Republicans on the Supreme Court legalized political bribery with their Citizens United decision, some of these companies allocate millions every year (a mere drop in the bucket) to pay off loyal members of Congress and to dangle high-paying future jobs to high-level employees of CMS who have the power to keep the gravy train going and thwart prosecutions.
As PNHP noted:
“Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American health care, siphoning money from vulnerable patients while delaying and denying necessary and often life-saving treatment. While there is obvious reason to fix these issues in MA and to expand Traditional Medicare for the sake of all beneficiaries, the deep structural problems with our health care system will only be fixed when we achieve improved Medicare for All.”
We’re on the edge of the open enrollment period for Medicare, and the Advantage scammers will be carpet-bombing America with advertisements over the next few months. Representatives Pocan, Khanna, and Schakowsky have introduced the “Save Medicare Act” that would ban Advantage companies from using the word Medicare in their advertising.
They made a video about it that’s well worth sharing with friends and family:
youtube
As Schakowsky, Khanna, and Pocan note, “Only Medicare is Medicare.” Don’t be fooled by the Medicare Advantage scam.
And now that you know, pass it on and save somebody else’s health!
41 notes
·
View notes
Text
Editor's note: The following testimony was presented to the House Committee on Small Business, Subcommittee on Oversight, Investigations, and Regulations on July 19, 2023.
Chair Van Duyne, Ranking Member Mfume, and members of the subcommittee, thank you for inviting me here today. My name is Matthew Fiedler, and I am a health economist and a Senior Fellow with the Schaeffer Initiative on Health Policy at the Brookings Institution. My research focuses on a range of topics in health care policy, including health care provider payment and health insurance regulation.
My testimony will examine the administrative costs that health care providers incur to interact with health insurers (including both public insurers like Medicare and Medicaid and private insurers), as well as how public policy can reduce those costs. I will make four main points:
Health care providers incur substantial costs to interact with insurers, likely totaling hundreds of billions of dollars per year, costs that are ultimately borne in large part by consumers and taxpayers. Costly activities include negotiating contracts, collecting information about patients’ insurance coverage, obtaining prior authorization for care, submitting claims for payment, and reporting on quality performance. There are likely economies of scale in performing many of these activities, so the associated administrative burdens likely fall more heavily on smaller providers than on larger.
Many administrative processes serve valuable purposes, so efforts to reform them can involve tradeoffs and should be approached thoughtfully. For example, it is essential to have some set of procedures for compensating providers. Similarly, insurers’ prior authorization requirements can prevent delivery of inappropriate services, and audit processes can be effective tools for identifying and deterring fraud.
Certain targeted reforms could reduce administrative burdens with few substantive downsides. One is eliminating Medicare’s Merit-Based Incentive Payment System, which places large reporting burdens on clinicians, with few benefits. Another is replacing the cumbersome arbitration process that is used to determine payment rates for certain out-of- network services under the No Surprises Act with a simpler “benchmark” payment A third is reforming Medicare Advantage’s risk adjustment system to reduce plans’ ability to increase their payments by documenting additional diagnoses.
Standardizing billing, coverage, and quality reporting rules across insurers could generate larger savings but would also present more significant tradeoffs. Changes like these could help address a major reason that administrative burdens are larger in the United States than in other countries: the wide variation in rules across the United States’ many public and private insurers. However, mandating greater standardization would also limit insurers’ ability to tailor rules to their unique circumstances or experiment with novel approaches. Setting rules through a centralized process might also produce rules that are systematically better or worse than current rules.
The remainder of my testimony will examine these points in greater detail.
Read the full testimony here.
8 notes
·
View notes
Text
5 Ways For Small Business Owners To Reduce Their Taxable Income
Taxes can be anxious for a small business owner. You wear multiple hats, and one of the last things you want to do is give more of your hard-earned business profits to the nation.
Fortunately, there are many tax savings methods to reduce your taxable liability as a business owner. If you need methods to reduce your taxable income, consider some of the following ways below.
Employ a Family Member
The most suitable way to reduce taxes for your small business is by hiring one of your family members. The Internal Revenue Service allows for a variety of opportunities, all with the potential advantage of sheltering income from taxes. You can even hire your kids.
By hiring family members, small business owners can pay a lower marginal rate, or eliminate the tax on the income paid to their kids.
It is crucial to point out that earnings need to come from justified business goals. The IRS also lets small business owners have the benefit of reducing their taxes by hiring a spouse.
Depending on the advantages they may have through another job, you can even put aside retirement savings for them.
Start a Retirement Plan
As a small business owner, you give up a 401(k) contest compared to an employer. However, different retirement account options maximize retirement savings and reap valuable tax benefits. There are a variety of different retirement plan opportunities for business owners on the IRS website as a tax savings strategy.
Save Money for Healthcare Needs
One of the best methods to reduce small business taxes is by setting aside money for healthcare necessities. Medical costs continue to grow, and while you may be healthy now, saving money for unpredictable or future healthcare needs is crucial.
You can complete this through a Health Savings Account if you have a qualified high-deductible health plan.
By using HSAs, the business, and the employees can decrease taxes and potentially associated medical expenses.
Change Your Business Structure
As a small business owner, you do not have the advantage of an employer paying a part of your taxes. You are on the hook for the whole amount of Social Security and Medicare taxes.
As a limited liability company if your business is taxed you have to pay those taxes, though in distinctive circumstances you can eliminate half of those two tax responsibilities.
While there are different things to consider in this switch, like paying yourself adequate pay and other risks, it is a good way to reduce your taxable responsibility.
Deduct Travel Expenses
If you travel so much, you can reduce your business taxes. Business travel is completely deductible, though individual travel does not enjoy the same benefit. However, to maximize their business travel, small business owners can mix individual journeys with a justifiable business strategy.
With smart business tax planning, you can decrease your taxable revenue as a small business owner and maintain more of your funds operating for you. Just remember to consult a tax expert to assure you qualify for the possible savings.
2 notes
·
View notes
Text
UnitedHealth Group will eliminate cost-sharing for insulin and certain other prescription drug for many policyholders as soon as next year, CEO Andrew Witty said during an earnings call Friday.
The company's UnitedHealthcare subsidiary will no longer require out-of-pocket spending from fully insured group members for the following medications:
Insulin for diabetes
Epinephrine for severe allergic reactions
Albuterol for acute asthma attacks
Glucagon for hypoglycemia
and Naloxone for opioid overdoses.
"While this is an important step for vulnerable people's health, the larger and longer-term cost containment of drugs depends upon manufacturers restraining and lowering the list price of their products, which is a fundamental driver of costs," Witty said during the call. The company expects the change in its pharmacy benefits to reduce overall spending by preventing patients from becoming sicker, he said.
The average cash price for a single unit of insulin rose 41% between 2014 and 2021, data from the prescription drug discount company GoodRx show. Prices fell between 2019 and 2021 in part because the Food and Drug Administration approved several generic versions of the biologic drug, according to GoodRx.
UnitedHealthcare's announcement demonstrates that insurers ultimately decide what patients pay out-of-pocket for prescription drugs, a Pharmaceutical Research and Manufacturers of America spokesperson wrote in an email.
About 688,000 of UnitedHealthcare's 8 million fully insured group members use these medicines, a spokesperson wrote in an email. UnitedHealthcare plans to encourage its self-funded employer customers to consider including this benefit in their plan designs for 2023, a UnitedHealthcare spokesperson said.
More than 37 million Americans, or 11% of the population are diagnosed with diabetes, and 8.4 million rely on insulin to survive, according to the American Diabetes Association. The disease cost $327 billion in 2017, the organization said. One in four insulin users report rationing the medication–by skipping doses or taking less than they need–because of cost.
Other insurers and pharmacy benefit managers have policies designed to reduce insulin costs for patients.
Insulin and other glucose-lowering agents were the most common items covered pre-deductible among 300 businesses the Employee Benefit Research Institute surveyed in 2019. Two-thirds of employer-sponsored health plans paid the full cost for enrollees, according to the report. Forty-three percent also covered inhaled corticosteroid inhalers for asthma before their deductibles, the survey found.
In 2020, CVS Health's Caremark PBM began allowing plan sponsors to offer all categories of diabetes medications at zero cost for members without raising premiums. The year before, Cigna and its PBM Express Scripts began capping out-of-pocket costs for insulin at $25 per month.
Waiving cost-sharing for drugs doesn't lead to higher spending or premium increases, said Paul Fronstin, director of health benefits research at the Employee Benefit Research Institute. Because people with chronic conditions are likely to reach their out-of-pocket maximums each year, covering the insulin costs will not raise expenses for health plans, he said.
Fifteen states have adopted insulin copay caps and legislation is pending in 22 others, according to the diaTribe Foundation, a diabetes patient advocacy group.
The high cost of insulin has attracted intensifying political attention. President Donald Trump and President Joe Biden both promoted policies to make the medication more affordable. The House passed a bill in March that would cap monthly out-of-pocket insulin costs at $35 for those with private health insurance and Medicare.
Differing regulations governing drug rebates likely led UnitedHealthcare to limit its new policy to fully insured plans, as opposed to government-sponsored products such as Medicare Advantage, said Antonio Ciaccia, CEO of drug pricing research firm 46brooklyn Research and president of the consulting firm 3 Axis Advisors. "There are better and more stricter regulations in the Medicare space that require most of those rebates to essentially be passed through," he said.
During the second quarter, UnitedHealth Group reported $80.3 billion in revenue, up 13% from $71.3 billion. Net income rose 18.9% to $5.1 billion. UnitedHealthcare membership grew from 49.6 million to 51.2 million compared to the year-ago quarter.
source, it's behind a paywall.
3 notes
·
View notes
Text
Bulk Billing Doctors Hornsby: Ensuring Affordable Healthcare
In today's world, access to quality healthcare is paramount. However, for many individuals and families, the cost of medical services can often be a barrier to receiving the care they need. This is where Bulk Billing Doctors Hornsby step in, providing a crucial service that ensures everyone can access medical care without financial strain.
Located in the heart of Hornsby, Bulk Billing Medical Centre is dedicated to offering bulk billing services to patients, easing the burden of medical expenses. Bulk billing is a payment option under Australia's universal healthcare system, Medicare, where doctors bill Medicare directly for their services, resulting in little to no out-of-pocket expenses for patients.
One of the primary benefits of bulk billing is its affordability. By eliminating or significantly reducing the cost of medical services at the point of care, it ensures that individuals and families can seek medical attention when needed, without worrying about the financial implications. This is particularly important for those on low incomes, pensioners, and individuals facing financial hardship.
At Bulk Billing Medical Centre, patients can access a wide range of healthcare services without the added stress of hefty medical bills. From general consultations and preventive care to specialized treatments and allied health services, the clinic caters to diverse healthcare needs. Whether it's a routine check-up, immunizations, chronic disease management, or minor procedures, patients can rest assured that they will receive the care they need without financial strain.
Moreover, the convenience of bulk billing cannot be overstated. With no upfront payments required, patients can focus solely on their health without the hassle of dealing with invoices or reimbursement processes. This streamlined approach to billing simplifies the healthcare experience, making it more accessible and user-friendly for patients of all backgrounds.
Another advantage of bulk billing is its contribution to preventive healthcare. By removing financial barriers to medical services, individuals are more likely to seek regular check-ups and screenings, leading to early detection and intervention for potential health issues. This proactive approach not only improves individual health outcomes but also reduces the burden on the healthcare system by addressing issues before they escalate.
In conclusion, Bulk Billing Doctors Hornsby play a vital role in ensuring affordable and accessible healthcare for the local community. By offering bulk billing services, Bulk Billing Medical Centre empowers patients to prioritize their health without financial constraints. In a society where healthcare costs continue to rise, bulk billing stands as a beacon of affordability and inclusivity, ensuring that quality healthcare remains within reach for all.
0 notes
Text
Enhancing Access to Quality Healthcare: The Significance of Bulk Billing at Keysborough Superclinic
In the pursuit of improving healthcare accessibility, Keysborough Superclinic emerges as a beacon of quality and affordability. At the heart of our commitment is the practice of bulk billing for medical services, ensuring that individuals in Keysborough and its surrounding areas have unhindered access to essential healthcare. This offsite blog delves into the significance of bulk billing at Keysborough Superclinic, highlighting how this practice contributes to the well-being of the community.

Understanding Bulk Billing for Medical Services
Bulk billing is a billing practice in the Australian healthcare system that holds paramount importance for both healthcare providers and patients. It involves the direct billing of Medicare for medical services, eliminating the need for patients to pay any out-of-pocket expenses. Keysborough Superclinic proudly embraces the bulk billing model, recognizing its role in fostering equal access to healthcare for everyone.
Affordable Healthcare for All
The cornerstone of Keysborough Superclinic's ethos is to make healthcare accessible without financial barriers. Bulk billing allows us to extend medical services to individuals from various walks of life, ensuring that the cost of healthcare does not deter anyone from seeking necessary medical attention. Our commitment to bulk billing aligns with the broader goal of creating an inclusive healthcare environment that prioritizes the well-being of the entire community.
Eliminating Financial Barriers to Care
One of the primary advantages of bulk billing is its ability to eliminate financial barriers to healthcare. Patients can visit Keysborough Superclinic for a range of medical services, including general practitioner consultations, pathology services, and allied health services, without incurring any upfront costs. This approach is particularly beneficial for individuals who may face financial constraints but require essential medical care.

Comprehensive Medical Services Under Bulk Billing
Keysborough Superclinic operates as a Bulk Billing Medical Centre, offering a comprehensive range of medical services under the bulk billing model. From routine check-ups and preventive care to the management of chronic conditions, our experienced team of healthcare professionals is dedicated to providing accessible and high-quality medical services to the Keysborough community.
Convenience and Peace of Mind
Bulk billing not only promotes affordability but also contributes to the convenience and peace of mind of patients. Knowing that they can access medical services without the burden of upfront costs allows individuals to prioritize their health without hesitation. This is especially crucial for preventive care and early intervention, contributing to better health outcomes for the community.
How Bulk Billing Works at Keysborough Superclinic
At Keysborough Superclinic, the process of bulk billing is designed to be straightforward and patient-friendly. Individuals with a valid Medicare card can enjoy the benefits of bulk billing for eligible medical services. Our reception and billing teams are here to assist patients in understanding the billing process, ensuring transparency and clarity in every interaction.
Keysborough Superclinic: Your Trusted Bulk Billing Medical Centre
Choosing Keysborough Superclinic means choosing a healthcare provider that places your well-being at the forefront. As a Bulk Billing Medical Centre, we are committed to providing accessible, affordable, and high-quality medical services to the Keysborough community. Our dedicated team of healthcare professionals is here to support you on your health journey, ensuring that financial considerations do not impede your access to essential healthcare services.
Conclusion: A Commitment to Community Well-being
In conclusion, the practice of bulk billing at Keysborough Superclinic reflects our unwavering commitment to community well-being. By eliminating financial barriers to care, we empower individuals to prioritize their health and seek medical attention when needed. Keysborough Superclinic stands as a testament to the belief that quality healthcare should be accessible to all, and our dedication to bulk billing is a reflection of this core value.
At Keysborough Superclinic, your health is our priority, and our commitment to bulk billing underscores our mission to provide inclusive, accessible, and patient-centric healthcare services to the Keysborough community and beyond.
Reference url on Enhancing Access to Quality Healthcare: The Significance of Bulk Billing at Keysborough Superclinic
0 notes
Text
Is Physiotherapy Covered by Medicare?

The answer to the question “is physiotherapy covered by Medicare?” depends on your specific Medicare coverage. Medicare Advantage Plans may require prior authorization for outpatient therapy services, and providers must submit documentation proving the treatment is medically necessary.
Medicare Part A covers inpatient physical therapy if you spend at least three days in the hospital as an inpatient. Medicare Part B covers outpatient physiotherapy at doctors' offices, therapy clinics and rehabilitation facilities. To know more about is physiotherapy covered by Medicare, visit the MVP Rehab Physiotherapy website or call 0450603234.
The Medicare Part B (Medical Insurance) portion of the Medicare system pays for physiotherapy sessions. However, beneficiaries are responsible for the Part B deductible and 20% coinsurance.
Medicare determines if services are "reasonable and necessary" on a case-by-case basis. For physiotherapy, the sessions must be deemed by an approved doctor as an essential component of treatment for a chronic or long-term condition. Medicare considers a chronic or long-term condition one that has been present for at least six months. Moreover, the condition must also require ongoing care from three or more different healthcare practitioners—including your GP, a physical therapist, and a physician or nurse practitioner who manages your overall health.
Medicare Advantage plans—the bundled Medicare options that private insurance companies administer—often have their own rules on when and how they cover physiotherapy. For instance, they may limit the number of physiotherapy sessions or impose prior authorization requirements. Also, they might have their own deductibles. These limitations can be costly.
Medicare Part C, also known as Medicare Advantage, offers a different way to get your physiotherapy treatment. With Medicare Advantage, you receive your care from a private Medicare Advantage plan sponsor that pays a fixed payment to cover your health expenses. You can receive physiotherapy in your doctor’s office, at a hospital outpatient therapy department, or as part of home health services from a therapist hired by the plan.
The type of physiotherapy you receive depends on your condition and treatment plan. Physiotherapy can include manual techniques that involve moving parts of your body, such as pushing or pulling them; electrotherapy, which uses electrical currents to stimulate nerves and muscles; and heat or cold treatments, such as placing ice packs on your skin.
Previously, there were limits, called a therapy cap, on how much outpatient physical therapy Medicare would pay per year. This limit has been eliminated and Medicare patients can continue to receive physiotherapy as long as it is medically necessary.
If you’re looking to recover from surgery or reduce chronic pain and stiffness, physical therapy may be the answer. Whether you need to improve mobility, or just maintain your current ability and slow a decline, Medicare can help you get the care you need.
If the doctor agrees that physiotherapy is medically necessary, Medicare Part B covers outpatient treatments in doctors’ offices, physical therapy clinics, or rehabilitation hospitals. Medicare Advantage Plans, which are bundled Medicare programs managed by private companies, also provide physiotherapy coverage. These plans usually require you to use providers within their network.
Most Medicare Advantage plans require prior authorization for physical therapy, which means the plan must approve the services before they will cover them. A recent government report looked at coverage denials from 15 Medicare Advantage Plans and found that 13 percent were inappropriate. Many of these denials came from requesting prior authorization when a service was medically unnecessary. This type of coverage denial could lead to you paying more for the treatment you need.
Medicare covers physiotherapy as part of its Chronic Disease Management program. Beneficiaries can receive PT sessions at their doctor’s office, in an outpatient clinic, or in a skilled nursing facility. The therapist can also come to the patient’s home if they need help with daily tasks.
Prior authorization is required for some services in order to be covered by Medicare. The doctors or other health care providers who are treating you will contact Medicare on your behalf to request approval. If the service is approved, you will receive a letter stating that Medicare has authorized your coverage. If the service is denied, you will be given a notice that explains why and a description of any costs you may have to pay. To know more about is physiotherapy covered by Medicare, visit the MVP Rehab Physiotherapy website or call 0450603234.
If you disagree with the decision to deny your request, you can appeal it. This process can take up to a year and involves a complicated cascade of phone calls, faxes and emails between the insurance company and your physician or health care provider.
#ndis physiotherapy fees#physiotherapy bonnyrigg#bonnyrigg physio#ndis physiotherapy providers#physio bonnyrigg#ndis physiotherapy rates#physiotherapy in penrith#medicare physiotherapy#doctor of physiotherapy#physiotherapy in liverpool#physiotherapy sydney#best physiotherapy sydney#Physiotherapy Silverdale#ndis registered physiotherapy#is physiotherapy covered by medicare
0 notes
Text
The Benefits of $0 Premium Medicare Advantage Plans
As seniors navigate the complex landscape of healthcare options, the concept of $0 premium Medicare Advantage plans has become an enticing prospect. These plans offer a unique proposition, providing comprehensive coverage without the burden of a monthly premium.
Let's delve into the advantages of these plans and understand why they are gaining popularity among Medicare beneficiaries.
One of the primary attractions of $0 premium Medicare Advantage plans lies in their affordability. Traditional Medicare plans often require beneficiaries to pay premiums for Part B coverage, but $0 premium Advantage plans eliminate this financial burden. This means seniors can access a wide range of medical services, including hospital stays, doctor visits, and preventive care, without a recurring monthly cost.
Moreover, $0 premium plans frequently include additional benefits not covered by Original Medicare. These may include prescription drug coverage, vision and dental care, wellness programs, and even fitness memberships. By bundling these services into a single plan, beneficiaries can enjoy a more holistic approach to their healthcare, promoting overall well-being.
For those on a fixed income, the predictability of $0 premium plans provides peace of mind. Knowing that essential healthcare services are covered without an extra financial strain allows seniors to focus on their health rather than worrying about the cost of medical care. This financial relief can be particularly beneficial for individuals living on a tight budget.
It's crucial for Medicare beneficiaries to carefully evaluate the specific details of $0 premium Medicare Advantage plans, as coverage can vary. While the absence of a monthly premium is undoubtedly appealing, understanding copayments, deductibles, and network restrictions is essential for making informed decisions about healthcare.
In conclusion,
$0 premium Medicare Advantage plans offer seniors an affordable and comprehensive alternative to traditional Medicare. As the healthcare landscape continues to evolve, exploring these plans may be a key step in securing accessible and cost-effective medical coverage for the aging population.
#0 premium medicare advantage plans#heartwise#turning 65 medicare checklist#medicare provider tempe az#medicare health benefits tucson#zero premium medicare advantage plans
1 note
·
View note
Text
Health insurance has been the primary driver of inflated and unclear pricing of healthcare services since its inception.
We need an actual system of universal healthcare based on patient outcomes rather than corporate income.
#singlepayer sunday#universal healthcare#medicare for all#singlepayer#eliminate medicare advantage#eliminate medicare part c#medicare disadvantage
31 notes
·
View notes
Text
By Jake Johnson
Common Dreams
Oct. 4, 2023
"Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare," says a new report from Physicians for a National Health Program.
A report published Wednesday estimates that privately run, government-funded Medicare Advantage plans are overcharging U.S. taxpayers by up to $140 billion per year, a sum that could be used to completely eliminate Medicare Part B premiums or fully fund Medicare's prescription drug program.
Physicians for a National Health Program (PNHP), an advocacy group that supports transitioning to a single-payer health insurance system, found that Medicare Advantage (MA) overbills the federal government by at least $88 billion per year, based on 2022 spending.
That lower-end estimate accounts for common MA practices such as upcoding, whereby diagnoses are piled onto a patient's risk assessment to make them appear sicker than they actually are, resulting in a larger payment from the federal government.
But when accounting for induced utilization—"the idea that people with supplemental coverage are likely to use more health care because their insurance pays for more of their cost"—PNHP estimated that the annual overbilling total could be as high as $140 billion.
"This is unconscionable, unsustainable, and in our current healthcare system, unremarkable," says the new report. "Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare, siphoning money from vulnerable patients while delaying and denying necessary and often lifesaving treatment."
Even if the more conservative figure is accurate, PNHP noted, the excess funding that MA plans are receiving each year would be more than enough to expand traditional Medicare to cover dental, hearing, and vision. Traditional Medicare does not currently cover those benefits, which often leads patients to seek out supplemental coverage—or switch to an MA plan.
The Congressional Budget Office has estimated that adding dental, vision, and hearing to Medicare and Medicaid would cost just under $84 billion in the most costly year of the expansion.
"While there is obvious reason to fix these issues in MA and to expand traditional Medicare for the sake of all beneficiaries," the new report states, "the deep structural problems with our healthcare system will only be fixed when we achieve improved Medicare for All."
Bolstered by taxpayer subsidies, Medicare Advantage has seen explosive growth since its creation in 2003 even as it has come under fire for fraud, denying necessary care, and other abuses. Today, nearly 32 million people are enrolled in MA plans—more than half of all eligible Medicare beneficiaries.
Earlier this year, the Biden administration took steps to crack down on MA overbilling, prompting howls of protest and a furious lobbying campaign by the industry's major players, including UnitedHealth Group and Humana. Relenting to industry pressure, the Biden administration ultimately agreed to phase in its rule changes over a three-year period.
Leading MA providers have also faced backlash from lawmakers for handing their top executives massive pay packages while cutting corners on patient care and fighting reforms aimed at rooting out overbilling.
As PNHP's new report explains, MA plans are paid by the federal government as if "their enrollees have the same health needs and require the same levels of spending as their traditional Medicare counterparts," even though people who enroll in MA plans tend to be healthier—and thus have less expensive medical needs.
"There are several factors that potentially contribute to this phenomenon," PNHP's report notes. "Patients who are sicker and thus have more complicated care needs may be turned off by limited networks, the use of prior authorizations, and other care denial strategies in MA plans. By contrast, healthier patients may feel less concerned about restrictions on care and more attracted to common features of MA plans like $0 premiums and additional benefits (e.g. dental and vision coverage, gym memberships, etc.). Insurers can also use strategies such as targeted advertising to reach the patients most favorable to their profit margins."
A KFF investigation published last month found that television ads for Medicare Advantage "comprised more than 85% of all airings for the open enrollment period for 2023."
"TV ads for Medicare Advantage often showed images of a government-issued Medicare card or urged viewers to call a 'Medicare' hotline other than the official 1-800-Medicare hotline," KFF noted, a practice that has previously drawn scrutiny from the U.S. Senate and federal regulators.
PNHP's report comes days after Cigna, a major MA provider, agreed to pay $172 million to settle allegations that it submitted false patient diagnosis data to the federal government in an attempt to receive a larger payment.
Dr. Ed Weisbart, PNHP's national board secretary, toldThe Lever on Wednesday that such overpayments are "going directly into the profit lines of the Medicare Advantage companies without any additional health value."
"If seniors understood that the $165 coming out of their monthly Social Security checks was going essentially dollar for dollar into profiteering of Medicare Advantage, they would and should be angry about that," said Weisbart. "We think that we pay premiums to fund Medicare. The only reason we have to do that is because we're letting Medicare Advantage take that money from us."
13 notes
·
View notes
Text
Comprehensive Coverage: AARP United Healthcare Medicare Advantage Explained
Introduction:
Medicare Advantage plans play a pivotal role in providing comprehensive healthcare coverage to individuals eligible for Medicare. Among the various options available, the AARP United Healthcare Medicare Advantage plan stands out for its extensive coverage and unique features. This article aims to delve into the intricacies of this plan, exploring its components, benefits, and potential drawbacks to help individuals make informed decisions about their healthcare coverage.

Understanding Medicare Advantage:
Medicare Advantage plans, also known as Medicare Part C, are private health insurance plans that offer an alternative to Original Medicare. They are designed to provide a comprehensive approach to healthcare by combining coverage for hospital stays (Medicare Part A) and medical services (Medicare Part B) into a single plan. Additionally, many Medicare Advantage plans often include coverage for prescription drugs (Medicare Part D), dental, vision, and other wellness programs.
Key Components of AARP United Healthcare Medicare Advantage:
Hospital and Medical Services Coverage: The AARP United Healthcare Medicare Advantage plan typically includes coverage for both inpatient hospital care and outpatient medical services. This encompasses a wide range of treatments, from surgeries to doctor visits, ensuring that beneficiaries have access to essential healthcare services.
Prescription Drug Coverage (Part D): One notable feature of this plan is its inclusion of Medicare Part D, providing coverage for prescription medications. This is crucial for individuals who require ongoing medications for chronic conditions, as it helps manage out-of-pocket expenses and ensures consistent access to necessary drugs.
Additional Benefits: AARP United Healthcare Medicare Advantage often goes beyond the basic Medicare coverage by offering additional benefits such as dental, vision, and hearing coverage. These extra perks contribute to the overall well-being of beneficiaries by addressing crucial aspects of healthcare that may not be covered by Original Medicare.
Benefits of AARP United Healthcare Medicare Advantage:
Cost Savings: One of the primary advantages of opting for AARP United Healthcare Medicare Advantage is the potential for cost savings. Unlike Original Medicare, which involves separate premiums for Part A and Part B, Medicare Advantage plans often come with a bundled premium, potentially resulting in lower overall costs for beneficiaries.
Comprehensive Coverage: The comprehensive nature of AARP United Healthcare Medicare Advantage ensures that beneficiaries receive a wide array of healthcare services under a single plan. This simplifies healthcare management, eliminating the need for multiple insurance policies and reducing administrative complexities.
Wellness Programs and Preventive Care: Many Medicare Advantage plans, including AARP United Healthcare, offer wellness programs and preventive care services. This proactive approach to healthcare can contribute to better overall health outcomes by identifying and addressing potential issues before they become more serious.
Drawbacks and Considerations:
Network Restrictions: A potential drawback of Medicare Advantage plans, including the AARP United Healthcare plan, is the reliance on a network of healthcare providers. Beneficiaries may face limitations in choosing healthcare providers, and going out of the network may result in higher out-of-pocket costs.
Plan Limitations and Changes: Medicare Advantage plans can undergo changes annually, affecting coverage and costs. It's crucial for beneficiaries to review plan documents regularly to stay informed about any modifications. Additionally, plan limitations, such as prior authorization requirements, may impact the ease of accessing certain healthcare services.
Conclusion:
In conclusion, the AARP United Healthcare Medicare Advantage plan offers a comprehensive approach to healthcare coverage for eligible individuals. Its bundled services, inclusion of prescription drug coverage, and additional benefits make it an appealing option for those seeking a more holistic approach to managing their healthcare needs. However, it's essential for beneficiaries to carefully consider factors such as network restrictions, potential plan changes, and limitations before enrolling. Making an informed decision based on individual healthcare needs and preferences is key to maximizing the benefits of AARP United Healthcare Medicare Advantage.
0 notes
Text
How to Qualify for Medicare if You Have a Disability?

Qualifying for Medicare due to a disability involves meeting specific criteria set by the Social Security Administration (SSA). Individuals under 65 who have a qualifying disability or medical condition may be eligible for Medicare benefits.
Here's a guide on how to qualify for Medicare if you have a disability.
Meet the Social Security Definition of Disability: To qualify for Medicare based on disability, you must meet the Social Security Administration's definition of disability. The SSA considers you disabled if you are unable to engage in substantial gainful activity (SGA) due to a medically determinable physical or mental impairment that is expected to last at least 12 months or result in death.
Work Credits: While work credits are typically associated with Social Security retirement benefits, they are also relevant for those qualifying for disability-based Medicare. The number of work credits required depends on your age at the time you become disabled. Work credits are earned based on your work history and payment of Social Security taxes.
Duration of Disability: To qualify for Medicare, your disability must be expected to last for at least 12 continuous months or result in death. The SSA evaluates the severity and expected duration of your disability when determining eligibility.
Apply for Social Security Disability Benefits: Initiating the application process for Social Security Disability Insurance (SSDI) is a crucial step. You can apply online through the SSA website, by phone, or by scheduling an appointment at your local Social Security office. Provide detailed medical and work history information to support your claim.
Waiting Period: After approval for SSDI, there is a mandatory waiting period before Medicare coverage begins. Individuals become eligible for Medicare 24 months after their Social Security Disability onset date. This waiting period helps ensure that Medicare resources are directed toward those with long-term disabilities.
Automatic Enrollment: Individuals receiving SSDI are generally automatically enrolled in Medicare after the 24-month waiting period. Medicare coverage includes Part A (hospital insurance) and Part B (medical insurance). The enrollment process is handled by the SSA, and Medicare cards are typically sent in the mail.
Medicare Advantage and Part D: In addition to original Medicare (Part A and Part B), individuals may choose to enroll in Medicare Advantage (Part C) plans offered by private insurers. These plans often include prescription drug coverage (Part D) and may offer additional benefits. It's important to review and select the coverage options that best meet your healthcare needs.
Medicare Savings Programs: Some individuals with disabilities may qualify for Medicare Savings Programs (MSPs) that help cover Medicare premiums, deductibles, and copayments. MSPs are state-run programs, and eligibility is based on income and resource limits.
Extra Help for Prescription Drug Costs: The Extra Help program assists individuals with limited income and resources in paying for prescription drug costs associated with Medicare Part D. This subsidy helps reduce or eliminate out-of-pocket expenses for medications.
Continuous Medical Review: Individuals receiving disability-based Medicare are subject to periodic medical reviews by the SSA to assess ongoing eligibility. It's important to stay informed about reporting any changes in your medical condition or employment status.
In conclusion, qualifying for Medicare due to a disability involves meeting specific criteria related to the severity and duration of the disability, earning sufficient work credits, and successfully applying for Social Security Disability Insurance. The process requires attention to detail, timely application, and an understanding of the waiting period before Medicare coverage begins. Exploring additional assistance programs and coverage options ensures that individuals with disabilities can access the healthcare support they need.
0 notes
Text
Virtual Psychological Wellness Support Is Transforming The Means We Look After Our Minds
Authored By-Atkins Busk
During the COVID-19 pandemic, telehealth services have helped people access psychological health care. These solutions can range from video seminar sessions to remote surveillance.
Telehealth provides many benefits for clients, including comfort, cost-effectiveness and simplicity of scheduling. However, it is necessary to recognize how these tools work prior to utilizing them.
Availability
Telehealth, or making use of telecoms modern technologies for health care solutions, is a popular alternative for customers throughout the COVID-19 pandemic. This service enables digital visits between individuals and their medical care specialists.
The primary advantage of telehealth is its enhanced accessibility and ease for individuals. It eliminates geographical barriers and permits individuals to see a psychological health specialist without traveling long distances or enduring long wait times.
Furthermore, telepsychiatry allows individuals to set up sessions around their active lives. https://www.forbes.com/sites/forbescommunicationscouncil/2020/08/10/ppc-advertising-tips-for-acquiring-home-care-clients/ is particularly vital for individuals with minimal wheelchair or those that can not take some time off work for in-person therapy sessions.
Convenience
For individuals incapable to take a trip as a result of COVID-19 or various other factors, telehealth uses a convenient alternative. They can have a therapy session from the convenience of their own homes, without needing to worry about transportation or organizing.
Nonetheless, it is essential to note that the ability to read non-verbal cues is decreased throughout virtual sessions. Nevertheless, it's still an efficient means to give psychological health services to customers. On top of that, telehealth permits clients to choose from a wide variety of therapists, so they can find the right one for them.
Adaptability
With telehealth counseling solutions, clients can access psychological medical care from the comfort of their homes, decreasing social preconception. Additionally, individuals can prevent the expense of traveling and car parking, making these services extra economical for both clients and medical care systems.
Doctor need flexibility in telehealth policies and reimbursement. While lots of states have parity laws that need personal insurers to repay telehealth brows through on the exact same basis as in-person brows through, Medicare offers much less flexibility.
Handling these issues will allow extra extensive use telehealth therapy services in the US. This will certainly additionally make certain that individuals obtain the treatment they require when they require it, no matter their area or insurance policy protection.
Cost-Effectiveness
With telehealth solutions, individuals can access psychological health care without needing to pay for expenses such as travel, vehicle parking, or child care. This makes telehealth a lot more affordable for both clients and medical care systems.
In addition, telehealth counseling solutions get rid of geographical barriers that protect against people from seeking psychological medical care. It allows individuals to select a specialist that they can construct a strong restorative connection with, regardless of their location.
Several researches have actually shown that customers are very pleased with telehealth services. They offer hassle-free, flexible, and top notch treatment, along with enhanced employee efficiency by eliminating pause for travel.
Reduce of Scheduling
Telehealth supplies versatile organizing, making it simpler for people to get in touch with their psychological health suppliers. Usually, this includes night and weekend break consultations, an essential advantage for those with restricted accessibility or hectic routines.
FTTH additionally enhances performance and performance for mental healthcare providers, permitting them to offer more clients in a shorter period of time. Furthermore, telehealth lowers expenses related to maintaining physical clinics and traveling expenditures.
Several individuals stay clear of looking for treatment for their psychological wellness concerns due to social preconception, which can be tough to conquer when getting treatment face to face. However, telehealth can eliminate these obstacles, encouraging even more people to look for the aid they require.
Tracking
Telehealth solutions provide a variety of benefits along with boosted access and benefit. These include adaptability, cost-effectiveness, and tracking of progress.
With telehealth, individuals can connect with mental wellness specialists despite their location. The technology removes geographical barriers and reduces traveling expenses for individuals. It likewise aids to improve the quality of therapy for those with minimal accessibility to in-person care.
Furthermore, telehealth counseling sessions are offered outside of standard workplace hours and on the weekend break, permitting even more adaptability in organizing consultations. https://www.goodhousekeeping.com/beauty/anti-aging/a22850819/best-skincare-routine/ offers clients with a more comfy and exclusive experience, encouraging them to seek treatment.
Partnership
While the term "telehealth" might be associated with digital gos to, it is essential to keep in mind that it's a broad collection of approaches for improving healthcare delivery. For techniques looking to provide mental health services, telehealth devices can be handy for both collaboration and sychronisation.
FTTH permits patients to look for treatment from the convenience of their home, reducing preconception and making mental health care much more accessible for individuals that require it. In addition, telehealth can help to ensure that customers obtain consistent support from their specialists, also when exterior elements like job or traveling disrupt their routines.

0 notes
Text
Digital Mental Health Support Is Transforming The Means We Look After Our Minds
Content Author-Oneal Busk
During the COVID-19 pandemic, telehealth solutions have actually aided individuals gain access to mental health care. These solutions can range from video seminar sessions to remote monitoring.
Telehealth supplies lots of benefits for patients, including comfort, cost-effectiveness and ease of scheduling. Nonetheless, it is very important to comprehend just how these devices work before using them.
Access
Telehealth, or using telecoms innovations for healthcare services, is a prominent alternative for customers during the COVID-19 pandemic. This service enables virtual visits in between people and their healthcare experts.
The major advantage of telehealth is its boosted ease of access and benefit for people. It eliminates geographical obstacles and allows people to see a psychological wellness professional without taking a trip fars away or enduring long haul times.
Additionally, telepsychiatry enables individuals to schedule sessions around their hectic lives. This is specifically essential for individuals with limited movement or those who can not take time off benefit in-person treatment sessions.
Convenience
For individuals not able to travel because of COVID-19 or other reasons, telehealth uses a practical option. They can have a therapy session from the convenience of their very own homes, without having to fret about transportation or organizing.
Nonetheless, it's important to keep in mind that the ability to check out non-verbal signs is diminished during digital sessions. Nevertheless, it's still an efficient means to offer mental health services to clients. In addition, telehealth permits clients to select from a wide variety of therapists, so they can locate the appropriate one for them.
Flexibility
With telehealth counseling solutions, patients can access psychological health care from the convenience of their homes, decreasing social preconception. In addition, clients can avoid the cost of traveling and auto parking, making these services much more economical for both clients and health care systems.
Doctor require versatility in telehealth plans and reimbursement. While lots of states have parity legislations that call for private insurance firms to repay telehealth sees on the exact same basis as in-person sees, Medicare offers much less flexibility.
Resolving these concerns will certainly allow extra extensive use telehealth therapy solutions in the United States. This will certainly also guarantee that patients receive the care they need when they need it, despite their area or insurance policy coverage.
Cost-Effectiveness
With telehealth services, people can access psychological healthcare without needing to pay for expenditures such as travel, vehicle parking, or child care. This makes telehealth a lot more inexpensive for both customers and medical care systems.
In visit the following internet site , telehealth counseling solutions get rid of geographical obstacles that avoid individuals from looking for mental medical care. It enables patients to pick a therapist that they can develop a strong restorative partnership with, despite their area.
A number of research studies have revealed that customers are highly pleased with telehealth services. They offer convenient, flexible, and top notch care, along with improved worker performance by eliminating pause for traveling.
Alleviate of Scheduling
Telehealth supplies adaptable scheduling, making it simpler for individuals to connect with their psychological wellness companies. Typically, this includes evening and weekend appointments, a crucial benefit for those with restricted availability or active routines.
FTTH additionally raises efficiency and productivity for mental healthcare providers, allowing them to serve more people in a shorter amount of time. Additionally, telehealth decreases costs related to preserving physical centers and traveling expenditures.
Lots of people stay clear of looking for treatment for their mental health issues due to social preconception, which can be hard to overcome when receiving treatment personally. However, telehealth can remove these obstacles, urging even more people to seek the aid they need.
Tracking
Telehealth services supply a wide range of benefits in addition to enhanced availability and benefit. These consist of versatility, cost-effectiveness, and monitoring of progress.
With https://www.verywellhealth.com/resident-centered-food-services-197752 , people can connect with psychological health and wellness specialists despite their area. The modern technology eliminates geographical obstacles and minimizes traveling expenses for individuals. It also helps to improve the high quality of therapy for those with limited accessibility to in-person care.
Additionally, telehealth therapy sessions are offered outside of basic office hours and on the weekend break, enabling more flexibility in scheduling consultations. This supplies clients with an extra comfy and private experience, encouraging them to look for therapy.
Partnership
While the term "telehealth" might be associated with digital brows through, it is very important to keep in mind that it's a broad set of approaches for boosting healthcare shipment. For techniques looking to deliver mental health services, telehealth devices can be useful for both cooperation and sychronisation.
FTTH allows individuals to look for treatment from the convenience of their home, lowering stigma and making psychological health care more easily accessible for individuals who need it. In addition, telehealth can help to ensure that clients get constant assistance from their therapists, even when external factors like job or traveling interrupt their routines.
0 notes