#CRANIOFACIAL PAIN
Text

Orofacial/Craniofacial pain is a field of dentistry that deals with the diagnosis and care of non dental pain that presents in the head, face or neck, or inside your mouth. These types of disorders all have unique causes and treatments. People with persistent pain in the form of headaches or migraines, pain in their teeth, mouth, face, neck, shoulder, and all the way down to their feet often turn to their dentist for any suspicious toothaches.
1 note
·
View note
Note
I'm writing a character with large, nasty, and veey noticeable burn scars on one part of his face. Any tips on things I should include?
this is what the scars look like

[image description: sketch of a character from the shoulders up with a burn scar on the left side of his face, ear, neck, and shoulder. end image description]
Hello,
I'm not a burn survivor myself so I'll talk about facial differences in general and link some stuff that might be more specific to your question.
First thing that I noticed about this ask is the wording - calling a facial difference "nasty". Which some people do say about themselves, but I discourage authors who aren't part of the FD community to use that in a neutral setting because it's not a neutral term. Facial differences, including scars, burns, craniofacial conditions, and every other difference aren't ugly, gross, or anything of that sort. Your character does have a large and noticeable burn, true! But he doesn't have anything "nasty" on his face. Neither do real life people with FD who might not want to read about a character looking like them or people from their community being referred to as "nasty" as a state-of-fact neutral descriptor.
To know what to include, you should research the medical side of burns; what kind of burn it is (chemical/thermal/electrical/other? they can cause different symptoms), what exactly is affected and how much (feeling, mobility) and how to care for burns long term (like preventing infections, pain management or physical/occupational therapy). Knowing how burns work outside of being a visual difference will make it more realistic. Researching (referencing) images of actual burn survivors might also be helpful to see how the skin might look like and interact with the rest of the person's face outside just being a different color (compare: a flat port wine stain and a burn scar).
Here is a post about drawing and writing burn survivors specifically. You can also read this post that I made that talks about facial differences in general. It's long but I've heard that it's informative :-) (smiley face)
As always, I heavily encourage anyone making a character with a facial difference to research face equality, as it's vital to making positive representation. I've written more about it in the links above.
I also encourage anyone sending an image to include a description of it so that those of us who use a screenreader can access it as well.
mod Sasza
#polypd#mod sasza#terminology#face difference#writing advice#writing disabled characters#writeblr#writing resources#writing tips#writing help#burn survivor representation
124 notes
·
View notes
Text
one of the little things about pollack's run that i deeply appreciate:
dorothy is able to come into her powers and reclaim them and move past some of her trauma because she meets another congenitally disabled young girl and finds kinship with her. dorothy has been bullied for her craniofacial difference her entire life, and her powers partially or even primarily manifest to protect her and provide companionship because of that trauma. but when she sees jennie, another child bullied for her disability, finding love and joy in her powers, dorothy is able to find those things, too. it doesn't get rid of the pain either of them have been through, but they're able to find solidarity and companionship in each other the same way they used to only be able to find with imaginary friends.
29 notes
·
View notes
Note
I might write this idea myself but I thought I should share it with you. So there’s this really rare condition where you can be born without your sixth chromosome and in an extremely rare case - there’s literally only one known person with this - you can exhibit all three symptoms that come with this condition: you will never feel hungry, you will never feel tired and you will never feel pain. And that just made me think of how with Wei Wuxian or Lan Wangji would feel if either (or both) of them were born with this condition.
I've actually never heard of that condition and googled it to fact check and holy hell this thing is super rare and rather brutal.
"For example, there have been some reported cases in which children with Chromosome 6 Ring have few physical abnormalities and normal intelligence. However, many with the chromosomal abnormality are affected by growth retardation; varying degrees of mental retardation; mild to severe delays in the acquisition of skills requiring the coordination of mental and physical activities (psychomotor retardation); and/or various abnormalities of the skull and facial (craniofacial) region." (Rarediseases.org)
43 notes
·
View notes
Text
i have several complex chronic health conditions and one of those conditions is hyperhidrosis which for those who don't know is excessive sweating which can be localised such as just the hands or just the feet or just the armpits etc or generalised which is all over the body or several areas all once or craniofacial which which is localised to the head and face area. I have generalised and craniofacial and it is absolutely soul destroying, it's embarressing and debilitating, its uncomfortable and stops me from doing so much. I did however begin treatment for it last year which although initially took some time to find the right doasage and some time for it to start wprking fully, did eventually work absolute wonders! As it turned out the medication i was on for the hyperhidrosis also seemed to work on the symptoms of my conditions too! As it was a medication uused to treat bladder urgency and spasms of the bladder it therefore helped with that issue (so well) but... it also stopped the spasms in my back and my bowel, i felt fantastic on it, id never been better, yep thats right there's a BUT coming!.... The tablets stopped being manufactured! they were no longer available, just like that! No warning, no chance to prepare, just stopped! So there i was with no medication and left to go back to suffering! I had by this time been discharged by the dermatogist as the condition was being managed and under control. So i had to start back right at the beginning, back to the gp to request another referal to the dermatologist, to be put back on their waiting list, and then to wait for an appointment and then the sress of trying to get someone to give me a lift there (as i dont drive and no public transport goes that way), all while being left untreated and just like that all the above mentioned conditions returned. Eventually i got my appointment and i'm now on a different medication but it is proving not to be anywhere near as affective, i still have uncontollable attacks of sweating, my bladder has become over active again and the spasm is back in my back. I feel aboslutley awful, in pain, slugglish, sweating and habbing to dash to the lav what feels like every five minutes and half a dozen times during the night. It has left me feeling extremely dejected and depressed, disappointed and so upset that i had my miracle cure all right there, only to have it snatched away and it is competely out of my control because it's just gone, it's not like i can try and fight to get it back because it's just not being produced. So here i am once again miserable, sad and at a loss. It just goes to prove that no matter how good times can be it can all be taken away and lost in a hearbeat, just like that!
#healthcare#chronic illness#hyperhidrosis#medication#nhs crisis#nhs england#disappointed#stress#health conditions and diseases
2 notes
·
View notes
Text

Guest post from John Martin Rare Book Room
At the Hardin Library for the Health Sciences
MÜTTER, Thomas Dent (1811–1859). A report on the operations for fissures of the palatine vault. Printed in Philadelphia by Merrihew & Thompson, 1843. 28 pages. 23 cm tall.
The University of Iowa is a worldwide leader in cleft palate research and repair, so we thought it only appropriate to recognize National Cleft and Craniofacial Awareness Month.
Many of you have no doubt heard of the Mütter Museum in Philadelphia, with its famous collection of anatomical specimens and medical instruments. The namesake of the museum, Thomas Dent Mütter, was a 19th-century American surgeon who overcame personal tragedy to become a renowned surgeon and educator.
One area that fascinated him was cleft palate and lip repair. This month's book, A report on the operations for fissures of the palatine vault, written by Mütter and printed in 1843, details his straightforward repair for a cleft palate.
The earliest evidence of cleft lip repair comes from the Jin Dynasty (265-420 CE) in China. The earliest detailed description of a repair is from Jehan Yperman (c.1260–c.1331), a pioneering medieval Flemish surgeon. The first known detailed description of a cleft palate comes from 16th-century French surgeon Pierre Franco (1505-1578). Franco emphasized the importance of the palate to speech development and the congenital origin of the malformation.
Clefts could also be caused by syphilis, however, and during the 16th and 17th centuries, surgical repairs were not advised. Instead, our old friend, Ambroise Paré, along with the Portuguese surgeon Amatus Lusitanus (aka João Rodrigues de Castelo Branco), wrote of using obturators - custom prosthetic devices used to close the palate.
Interest in surgical repair continued, though, especially for congenital clefts. By the 19th century, several Fench surgeons had devised their own methods for repair, including Guillaume Dupuytren, who Mütter trained with while continuing his medical education in Paris.
The Mütter Museum in Philadelphia is celebrated for its collection of anatomical specimens of rare conditions, from the famous (and infamous), as well as medical instruments. The museum was founded with an original donation from the collection of Thomas Dent Mütter.
Mütter was born in 1811 in Richmond, Virginia. Sickness is a common theme in Mütter's life, and he lost both of his parents by the time he was eight. He was raised by a distant relative in a seemingly supportive environment.
Money left to him by his parents allowed him to attend Hampden-Sydney College in Virginia and medical school at the University of Pennsylvania. Mütter himself fell ill during medical school. He left for Europe after graduation in the hopes of improving his health in a different climate and to further pursue his medical education.
In Paris, he worked with the aforementioned Dupuytren and in London with Robert Liston. Mütter eventually put together a collection of lectures by Liston, which he annotated with 250 pages of his own.
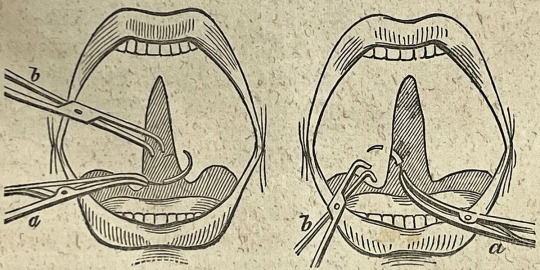
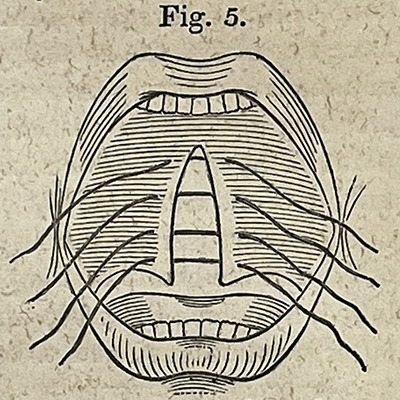
Dupuytren was known for his exacting nature and Liston for his speed when performing a surgical procedure (which could mean the difference between life and death in the days before anesthesia and antibiotics). Mütter seems to have embraced the teachings of both his mentors, stressing the need for the simplest of tools and techniques when performing his reconstructive surgeries while trying to keep the pain and blood loss to a minimum.
In 1841, he joined the faculty of the Jefferson Medical College in Philadelphia. It was there that he made a name for himself as an excellent speaker and engaging teacher. He used his ever-expanding anatomical and instrument collection to provide his students with hands-on experience.
Unfortunately, his ill health never truly subsided and he was forced to retire in 1856. He died three years later at the age of 48.
A report on the operations for fissures of the palatine vault demonstrates Mütter's adherence to his surgical principles. It is not a long book, only 28 pages, but it provides insight into his process and surgical philosophy. It includes several small illustrations of the steps of the procedure and the instruments used, examples of which you can see above.
The book is covered in a "library binding" of black cloth and the textblock shows evidence of having been trimmed (see the ownership mark in the upper right corner of the title page above). Indeed, this book was at some point pulled from the circulating Hardin collection and added to the Rare Book Room collection. It still contains the date due slip (last checked out in 1967!) and barcode sticker.
Contact Curator Damien Ihrig to view this tiny but mighty book or any others from this or past newsletters: [email protected] to arrange a visit in person or over Zoom.
#cleft palate#medical#medical history#jmrbr#hardin library#special collections#rare books#uiowa#libraries#Mütter
11 notes
·
View notes
Text
Enhance Your Expertise with TMJ CE Courses
Temporomandibular Joint (TMJ) disorders affect millions of people worldwide, causing pain, discomfort, and functional limitations. As dental professionals, understanding TMJ disorders and their treatment is essential for providing comprehensive care to patients. At DrStevenOlmos.com, we offer specialized TMJ continuing education (CE) courses designed to equip dental practitioners with the knowledge, skills, and techniques needed to effectively diagnose and treat TMJ disorders. Let's delve into the world of TMJ CE and discover how it can enhance your expertise and transform your practice.
Comprehensive TMJ Education TMJ disorders encompass a wide range of conditions affecting the temporomandibular joint, surrounding muscles, and associated structures. From myofascial pain to disc displacement and degenerative joint disease, these disorders present complex challenges that require specialized knowledge and expertise to address effectively.
At DrStevenOlmos.com, our TMJ CE courses provide comprehensive education on the diagnosis, assessment, and treatment of TMJ disorders. Led by Dr. Steven Olmos, a renowned expert in dental sleep medicine and craniofacial pain management, our courses offer a unique blend of clinical insights, evidence-based practices, and hands-on training to empower dental professionals to confidently manage TMJ cases in their practice.
Advanced Treatment Techniques Effective treatment of TMJ disorders requires a multidisciplinary approach that addresses the underlying causes of dysfunction and alleviates symptoms. Our TMJ CE courses cover a range of treatment modalities, including occlusal splint therapy, trigger point injections, physical therapy techniques, and more.
Participants will learn how to develop personalized treatment plans tailored to each patient's unique needs, incorporating evidence-based interventions to restore optimal function and alleviate pain. Whether you're new to TMJ treatment or seeking to refine your skills, our courses provide the knowledge and resources you need to deliver exceptional care and achieve successful outcomes for your patients.
Why Choose DrStevenOlmos.com for TMJ Education? At DrStevenOlmos.com, we're committed to providing dental professionals with unparalleled TMJ education that empowers them to make a meaningful difference in the lives of their patients. Our courses are led by Dr. Steven Olmos, a leading authority in craniofacial pain management and TMJ treatment, and are backed by decades of clinical experience and research-based evidence.
Elevate Your TMJ Practice Today Ready to elevate your expertise in TMJ Treatment? Explore our TMJ CE courses at DrStevenOlmos.com and embark on a journey of lifelong learning, growth, and professional success. Join us in our mission to transform TMJ care and improve the quality of life for patients suffering from TMJ disorders.
To know more about TMJ CE please visit the website.
0 notes
Text
For Pain-Free Tooth Extraction Anchorage, visit All Alaska Oral & Craniofacial Surgery!
0 notes
Text
Unveiling the Power of Mewing: Sculpt Your Way to Facial Harmony and Health

Introduction:
In a world obsessed with quick fixes and cosmetic enhancements, one ancient technique is gaining traction for its transformative effects on both appearance and well-being. Enter Mewing – a practice rooted in proper tongue posture and nasal breathing that promises to not only redefine your facial aesthetics but also improve your overall health. Join us as we explore the fascinating world of Mewing and discover how this simple yet powerful technique can revolutionize your life.
Understanding Mewing:
At its core, Mewing revolves around the concept of maintaining correct oral posture, specifically by resting the tongue against the roof of the mouth with the lips closed and breathing through the nose. Developed by Dr. John Mew, a British orthodontist, Mewing aims to encourage proper craniofacial development, leading to a more balanced facial structure and enhanced oral health. While initially popularized as a method for achieving a chiseled jawline and defined cheekbones, Mewing has since garnered attention for its broader health benefits.
The Aesthetic Appeal:
For many, the allure of Mewing lies in its potential to sculpt facial features naturally, without the need for invasive procedures or cosmetic interventions. By maintaining proper tongue posture, individuals may notice improvements in jawline definition, cheekbone prominence, and overall facial symmetry over time. Additionally, adopting a Mewing regimen can contribute to better facial muscle tone and alignment, resulting in a more harmonious appearance that exudes confidence and vitality.
Beyond Beauty: The Health Benefits of Mewing:
While the aesthetic benefits of Mewing are undeniable, its impact extends far beyond mere appearances. Proper tongue posture and nasal breathing are essential components of optimal oral and overall health. Here are some of the health benefits associated with incorporating Mewing into your daily routine:
Improved Breathing: Nasal breathing, a cornerstone of the Mewing technique, promotes better oxygen exchange and respiratory function, reducing the risk of conditions such as snoring, sleep apnea, and asthma.
Enhanced Posture: By aligning the tongue and jaw properly, Mewing encourages better head and neck posture, alleviating strain on the cervical spine and reducing the likelihood of tension headaches and neck pain.
Dental Health: Maintaining the tongue in the correct position against the palate can aid in proper dental alignment, potentially reducing the need for orthodontic intervention and mitigating issues such as malocclusion and temporomandibular joint (TMJ) dysfunction.
Incorporating Mewing into Your Lifestyle:
Embracing the Mewing technique is a journey that requires dedication and consistency. Start by practicing proper tongue posture throughout the day, particularly during moments of rest and relaxation. Focus on breathing deeply through your nose, allowing the diaphragm to fully engage and promoting relaxation and mindfulness. Over time, these simple habits will become second nature, leading to lasting improvements in both appearance and well-being.
Conclusion:
In a world inundated with quick fixes and temporary solutions, Mewing stands out as a natural, holistic approach to facial aesthetics and health. By embracing proper tongue posture and nasal breathing, individuals can unlock their full potential, both in terms of appearance and overall well-being. So, dare to embark on this transformative journey, and discover the beauty and vitality that lie within. With Mewing, the power to sculpt your destiny is within reach – one breath, one posture, at a time. If you want to more articles or blogs on these type of topics so
visit here👉https://www.refersms.com/
#health#Health#Healthbenefits#Mewing#Exercise#Lifestyle#Relaxation#Technique#Confidence#Faceexercise#Beauty#Improvement#Focus#Solutions
0 notes
Text
A Comprehensive Guide to Analyzing X-Ray Skull AP & Lateral Views
X-ray imaging is a valuable diagnostic tool used in various medical scenarios to visualize the internal structures of the body. Among the different types of X-ray examinations, the X-ray skull AP and lateral views are commonly performed to assess the structures of the skull from different angles. This article aims to elucidate the purpose and indications for X-ray skull AP and lateral views.
Purpose of X-Ray Skull AP & Lateral View:
X-ray skull AP and lateral view provide detailed images of the bony structures of the skull, including the cranium and facial bones. These images offer valuable information to healthcare professionals for diagnosing various conditions and injuries related to the skull. The primary purposes of X-ray skull AP and lateral views include:
1. Evaluation of Trauma:
X-ray skull AP and lateral views are often ordered in cases of head trauma, such as fractures or injuries resulting from accidents or falls. These images help identify fractures, dislocations, or other abnormalities in the cranial and facial bones.
2. Assessment of Craniofacial Development:
In pediatric patients, X-ray skull AP and lateral views are utilized to evaluate the development of craniofacial structures. These images assist in detecting abnormalities or developmental disorders affecting the skull and facial bones.
3. Diagnosis of Skull Pathologies:
X-ray skull AP and lateral views are valuable for diagnosing various pathologies affecting the skull, including brain tumors, infections, and degenerative conditions. These images enable healthcare providers to visualize abnormalities in bone density, shape, or structure.
4. Preoperative Planning:
Before certain surgical procedures involving the skull or facial bones, X-ray skull AP and lateral views may be performed to aid in surgical planning. These images provide detailed information about the anatomy of the skull, assisting surgeons in determining the most appropriate approach for the procedure.
Indications for X-Ray Skull AP & Lateral View:
X-ray skull AP and lateral views may be indicated in the following situations:
1. Head Trauma:
Patients presenting with head injuries, such as suspected skull fractures or facial trauma, may require X-ray skull AP and lateral views to assess the extent of injury and aid in treatment decisions.
2. Craniofacial Abnormalities:
Individuals with congenital craniofacial abnormalities or developmental disorders may undergo X-ray skull AP and lateral views to evaluate the severity of the condition and plan appropriate interventions.
3. Skull Pathologies:
Patients with symptoms suggestive of skull pathologies, such as persistent headaches, facial pain, or swelling, may undergo X-ray skull AP and lateral views to investigate underlying causes.
4. Preoperative Evaluation:
Before certain surgical procedures involving the skull or facial bones, X-ray skull AP and lateral views may be performed as part of the preoperative assessment to guide surgical planning and ensure optimal outcomes.
Conclusion:
X-ray skull AP and lateral views play a crucial role in the diagnosis and management of various conditions affecting the skull and facial bones. By providing detailed images of bony structures, these imaging modalities assist healthcare professionals in evaluating trauma, identifying abnormalities, and planning surgical interventions. Understanding the purpose and indications for X-ray skull AP and lateral views is essential for the appropriate utilization of this imaging technique in clinical practice.
0 notes
Text
Role of SURGISPON® in Dog’s Dental Surgery

Clefts of the lip, alveolus, and palate are among the most common craniofacial birth abnormalities found in both humans and animals. Traditional treatments, such as autogenous bone grafts, have long been regarded as the gold standard. However, these methods have substantial disadvantages, including limited bone availability and donor-site problems such as post-operative pain, changes in sensation, and the risk of infections and scarring. Fortunately, recent approaches in cell therapy and tissue engineering provide promising solutions to these issues. One interesting strategy is to use a gelatin sponge scaffold combined with cultured stem cells to repair cleft alveoli in dogs. In this blog, we’ll explore how combining these innovative approaches particularly utilizing a gelatin sponge scaffold with cultured stem cells, can revolutionize the treatment of craniofacial defects in dogs.
Role of Gelatin Sponge, Cell therapy, and Tissue Engineering
Gelatin Sponge Scaffold: The gelatin sponge acts as a three-dimensional scaffold, providing structural support to the repair site. Its porous shape enables for the penetration of cells and growth substances, which promotes tissue regeneration and repair.
Cell therapy: It involves the use of stem cells, which have the unique capacity to differentiate into multiple cell types such as bone and soft tissue cells. These cells can be obtained from the patient’s own tissues or from compatible donors which lowers the chance of rejection and other complications.
Tissue engineering enhances cell treatment by creating a favourable environment for cell proliferation and tissue regeneration. Gelatin sponge excels in hemostasis, which ensures that blood flow is efficiently controlled. This is especially important in veterinary surgery, when patients are unable to verbalise their distress, making precision and safety critical. In some circumstances, gelatin sponge serves as a scaffold for bone graft materials, facilitating the formation of new bone and tissue regeneration.Gelatin is notable for being both absorbent and non-adherent. It will eventually absorb within the body after it serves its purpose of controlling bleeding. This eliminates the need for a second surgery to remove it resulting indecreasing post-operative complications and ensuring a faster and smoother recovery for the animal patient.
Clinical Study Insights:
A clinical study involving 12 healthy mongrel dogs utilized Gelatin Sponge (SURGISPON®, Aegis Life Science, India) as a scaffold, along with stem cells, to repair alveolar bone defects.This study concluded that stem cells cultured on gelatin scaffold accelerated the healing and regeneration of alveolar cleft and new bone formation in dogs [1].
Fig.1: A. The surgical site was covered with sterile surgical towels. B. A standardized alveolar bone defect defects (0.8Å~0.5Å~0.5 mm). C. The defect filled with a scaffold Surgispon® (Aegis Life Sciences) [1].
Further Advancements:
Aegis Lifesciences has introduced a new product HaemoVet® Dental sponges which comprised of Absorbable Gelatin Sponge and offer alternatives for veterinary dental surgeries.When implanted in tissues in appropriate amounts, it completely absorbs within<4 weeks. In oral and dental surgery, HAEMOVET® Sponges serve as a valuable aid in achieving hemostasis. HaemoVet® may be used either dry or moistened, depending upon conditions present at operation and preference of the surgeon. Isotonic saline is suitable for use with HaemoVet®.
Additionally, HaemoVet® Dental sponge, impregnated with colloidal silver, provides additional antibacterial properties, ensuring optimal healing conditions in the oral cavity.
HaemoVet® Dental Sponge
HaemoVet® Silver Sponge
References
Eman A. El Ashiry, Najlaa M. Alamoudi, Reem M. Allarakia, Amr M. Bayoumi, Essam E. Ayad, Amani A. Al Tuwirqi, Maha M. Mounir, RahafSahhaf, Mohmed A. Abd El hamid, Omar A. El Meligy. Histological and histomorphometrical evaluation of adipose tissue and bone marrow-derived mesenchymal stem cells in regeneration of the cleft alveolus in dogs. Medical Science, 2020, 24(102), 750-764.
0 notes
Text
Orthodontic Technology and Treatment Precision: A Winning Combination

Orthodontics is one of the areas of contemporary dentistry that is constantly developing, using cutting-edge technologies to improve patient results and treatment accuracy. Modern technology has completely changed the planning, carrying out, and monitoring of orthodontic treatments, providing a winning mix of efficiency and efficacy for patients as well as practitioners. Orthodontic technology, from digital imaging to 3D printing and computer-aided design, has opened the door for individualized treatment plans that put patient comfort and accuracy first. This article explores how orthodontic technology is changing the way that treatments are performed precisely and how it helps orthodontists and their patients.
Digital Imaging: A Foundation for Precision
Orthodontic practice nowadays relies heavily on digital imaging, which has taken the place of more antiquated techniques like plaster models and analog radiography for patient records. With unmatched accuracy, orthodontists may get precise 3D pictures of their patients' dentition, surrounding tissues, and craniofacial features by using methods such as intraoral scanners and cone-beam computed tomography (CBCT). Using these digital imprints as a starting point for treatment planning, orthodontists may examine the patient's occlusion, spot irregularities, and create specialized treatment plans based on their particular anatomical characteristics.
Orthodontists may more accurately forecast and treat patients by using digital diagnostics to properly evaluate skeletal connections, jaw discrepancies, and dental malocclusions. Moreover, digital imaging provides better vision and manipulation of tooth structures while reducing patient pain related to conventional impression materials. Digital imprints are easily incorporated into computer-aided design (CAD) software, which allows orthodontists to model treatment results, modify tooth motions, and predict problems before starting therapy. This increases treatment accuracy and efficiency.
Computer-Aided Design and 3D Printing: Personalized Treatment Solutions
The creation of orthodontic equipment has been completely transformed by the combination of computer-aided design (CAD) and 3D printing technology, ushering in a new era of individualized treatment plans catered to the specific requirements of each patient. Using computer-aided design (CAD) software, orthodontists may create personalized orthodontic products, like as retainers, braces, and clear aligners, by carefully mapping out the necessary tooth motions and occlusal modifications. Subsequently, these digital designs are converted into tangible models or printed outright via sophisticated additive manufacturing methods.
By reducing the variability inherent in traditional production processes, 3D printing allows for the quick development of orthodontic equipment with unparalleled accuracy and repeatability. Orthodontists may use additive manufacturing and digital workflows to create patient-specific appliances that maximize comfort, fit, and treatment effectiveness. Additionally, the capacity to rapidly iterate designs facilitates the adjustment of treatment plans and guarantees the best possible therapeutic results while cutting down on chairside time and patient visits.
Precision Mechanics and Self-Ligating Brackets
Apart from the digital developments, the introduction of new bracket systems like self-ligating brackets has improved treatment accuracy due to advancements in orthodontic mechanics. Self-ligating brackets include built-in clips or doors that secure the archwire, minimizing friction and allowing for more controlled tooth movement. This is in contrast to standard brackets, which use elastic or metal ligatures to keep the wire in place. This design makes wire replacements easier, reduces the need for frequent adjustments, and improves patient comfort during treatment.
Orthodontists may regulate tooth movement and alignment more precisely with self-ligating brackets, which leads to more predictable treatment outcomes and shorter treatment times overall. In addition, compared to conventional brackets, their smooth curves and low-profile design enhance mouth hygiene and lessen irritation of soft tissues. Orthodontists may maximize patient comfort and happiness while optimizing treatment efficiency by integrating precision mechanics into orthodontic equipment.
Enhanced Monitoring and Treatment Tracking
Orthodontic technology includes continuous patient progress monitoring and tracking throughout treatment, in addition to treatment planning and execution. Orthodontists may now remotely monitor tooth mobility, archwire changes, and treatment milestones with the use of digital platforms and software solutions. This allows for prompt interventions and corrections as needed. Virtual simulations that display anticipated results and interactive interfaces provide patients with additional insight into how their therapy is progressing.
Orthodontists can identify early treatment plan deviations, swiftly address new concerns, and optimize treatment trajectories to get the best possible outcomes by utilizing computerized monitoring systems. Clinicians may make data-driven choices, improve treatment protocols, and reduce the risk of complications or relapse with the use of real-time data analytics and predictive modeling. Furthermore, improved communication between patients and orthodontists encourages participation and teamwork, enabling people to actively participate in their orthodontic journey.
Conclusion
A new age of precision and individualized care has been brought about by orthodontic technology, which has completely changed the orthodontic profession and increased treatment results to previously unheard-of levels. Technological advances continue to propel advancements in orthodontic care, providing clinicians with the resources necessary to deliver customized treatment solutions with unparalleled accuracy and speed. Examples of these developments include digital imaging, computer-aided design, 3D printing, and precision mechanics. Orthodontists may change patients' smiles, improve their experiences, and influence the direction of orthodontics by utilizing technology.
0 notes
Text
Oculoauriculovertebral Syndrome_Sound therapy session_Sounds of nature

Oculoauriculovertebral Syndrome (OAVS), also known as Goldenhar Syndrome, is a rare congenital disorder characterized by facial and craniofacial abnormalities. Traditional medicine offers various interventions to manage the symptoms and improve the quality of life for individuals with OAVS. However, emerging as a potential adjunctive treatment is resonant frequency sound therapy. This holistic approach utilizes sound vibrations to promote healing and balance within the body.
Resonant frequency sound therapy involves the use of specific sound frequencies to resonate with the body's cells, tissues, and organs. By exposing the body to these frequencies, the therapy aims to restore harmony and balance, promoting overall well-being. The frequencies used are carefully selected based on the individual's condition and needs.
OAVS patients often experience immune system dysregulation, leading to increased susceptibility to infections and other health issues. Resonant frequency sound therapy can help strengthen the immune system by promoting cellular regeneration, optimizing the body's natural defense mechanisms, and improving overall immune function. This can lead to a reduced frequency and severity of infections associated with OAVS.
Inflammation is a common feature of OAVS, contributing to pain, discomfort, and further complications. Resonant frequency sound therapy has shown promise in reducing inflammation by promoting relaxation, increasing circulation, and stimulating the body's natural healing processes. By reducing inflammation, this therapy can help alleviate symptoms and improve the overall well-being of individuals with OAVS.
Resonant frequency sound therapy not only focuses on the physical aspect of healing but also takes into account the emotional and energetic well-being of the individual. The therapy promotes relaxation, stress reduction, and emotional balance, which are crucial aspects of managing the challenges associated with OAVS. By addressing the holistic well-being of the individual, resonant frequency sound therapy can contribute to an improved overall quality of life.
Resonant frequency sound therapy shows promise as an adjunctive treatment for Oculoauriculovertebral Syndrome when used in combination with traditional medicine interventions. By harnessing the power of sound vibrations, this therapy can enhance the immune system, reduce inflammation, and provide personalized support for individuals with OAVS.
TO ACHIEVE A POSITIVE RESULT, DAILY LISTENING TO VIDEOS IS REQUIRED.
I wish you health and prosperity!
#resonantfrequencytherapy#oculoauriculovertebralsyndrome#adjunctivetreatment#traditionalmedicine#holistichealing#soundtherapy#immunesystem#inflammation#personalizedtreatment
1 note
·
View note
Text
Breathe Easy: Navigating the Landscape of Sleep Apnea Jaw Surgery
A restful night's sleep is essential for overall well-being, and when obstructive sleep apnea disrupts this crucial aspect of health, individuals often find themselves seeking effective solutions. Sleep apnea jaw surgery, specifically orthognathic surgery, emerges as a significant intervention to alleviate the breathing difficulties associated with this sleep disorder. This exploration aims to provide a comprehensive understanding of sleep apnea jaw surgery, shedding light on its purpose, the surgical process, and the potential life-changing impact it can have on improving sleep quality and overall health.

Understanding Sleep Apnea:
Obstructive sleep apnea (OSA) is a sleep disorder characterized by repetitive pauses in breathing during sleep. These pauses, known as apneas, result from the partial or complete collapse of the upper airway, leading to decreased airflow. Common symptoms of sleep apnea include loud snoring, abrupt awakenings accompanied by a choking or gasping sound, excessive daytime sleepiness, and difficulty concentrating.
Central to the treatment of sleep apnea is the identification of its underlying causes. While lifestyle modifications, continuous positive airway pressure (CPAP) therapy, and oral appliances are often effective for mild to moderate cases, severe sleep apnea may require more comprehensive interventions, including surgery.
Purpose of Sleep Apnea Jaw Surgery:
Sleep apnea jaw surgery, specifically orthognathic surgery, aims to address the anatomical factors contributing to airway obstruction during sleep. In cases where the lower jaw (mandible) is set back, the tongue and soft tissues at the back of the throat may collapse more easily, exacerbating airway blockage.
Orthognathic surgery involves repositioning the upper and/or lower jaw to enhance the structural integrity of the airway. By advancing the jaw forward, surgeons create more space for the soft tissues, reducing the likelihood of airway collapse and improving airflow during sleep. This surgical approach is particularly beneficial for individuals with craniofacial abnormalities contributing to sleep apnea.
The Surgical Process:
The journey through sleep apnea jaw surgery begins with a comprehensive evaluation by a team of healthcare professionals, including sleep specialists, oral and maxillofacial surgeons, and orthodontists. The evaluation includes sleep studies, imaging, and a thorough assessment of the patient's overall health and medical history.
Once identified as a suitable candidate, the patient undergoes pre-surgical orthodontic treatment. This phase involves aligning the teeth within each jaw to optimize the surgical process and ensure a stable bite after the surgery.
The surgical procedure itself is performed under general anesthesia. Depending on the specific needs of the patient, the surgeon may reposition the upper jaw, lower jaw, or both. Precision is paramount as the surgeon carefully advances the jaw to create the desired alignment. In some cases, additional procedures such as genioglossus advancement or hyoid suspension may be performed to further stabilize the airway.
Recovery and Post-Surgery Care:
The recovery period following sleep apnea jaw surgery involves managing pain, swelling, and adapting to changes in oral function. Patients are typically required to follow a modified diet to accommodate the healing process, and pain medication may be prescribed to alleviate discomfort.
Post-surgery, patients continue orthodontic treatment to fine-tune the bite and ensure long-term stability. Regular follow-up appointments with the surgical and orthodontic teams are integral during the recovery phase to monitor progress and address any concerns.
Life-Changing Impact:
The potential life-changing impact of sleep apnea jaw surgery extends beyond improved sleep quality. By addressing the root cause of airway obstruction, this surgical intervention contributes to:
Enhanced Sleep Quality: The primary goal of sleep apnea jaw surgery is to promote uninterrupted airflow during sleep, leading to improved sleep quality and reduced daytime sleepiness.
Overall Health Benefits: Effective management of sleep apnea has broader health implications. Addressing sleep apnea reduces the risk of associated health issues, including cardiovascular problems, hypertension, and metabolic disorders.
Quality of Life Improvement: Individuals often report a significant enhancement in their overall quality of life post-surgery. Improved sleep contributes to better cognitive function, mood regulation, and a heightened sense of well-being.
Reduced Reliance on CPAP: For individuals who find CPAP therapy challenging, sleep apnea jaw surgery offers an alternative that may reduce or eliminate the need for continuous positive airway pressure devices.
Conclusion:
Navigating the landscape of sleep apnea jaw surgery involves not only addressing the physical aspects of airway obstruction but also reclaiming the essential and rejuvenating experience of a good night's sleep. As individuals embark on this transformative journey, the collaboration between healthcare professionals, effective patient communication, and a commitment to post-surgery care are integral components.
By understanding the purpose, process, and potential outcomes of sleep apnea jaw surgery, individuals can make informed decisions regarding their treatment. Ultimately, the goal is to breathe easy, free from the interruptions that characterize sleep apnea, and embrace a healthier and more restorative sleep pattern that positively influences overall health and vitality.
0 notes
Text
5 Best Ways to Choose a TMJ Specialist Near You
TMJ can be a painful and debilitating condition that affects the jaw joint and the surrounding muscles. If you are experiencing TMJ symptoms like jaw pain, headaches, or difficulty chewing, seeking the expertise of a qualified TMJ specialist is crucial. However, finding the right TMJ specialist can be a daunting task.

ICCMO is the right place if you need a TMJ diagnosis from expert healthcare professionals. This blog discusses five essential ways to choose a TMJ specialist near you who can effectively address your concerns and provide the necessary treatment.
How Can You Find The Right TMJ Specialist?
Credentials and Training
Look for a specialist who has completed relevant education and training in the field of orofacial pain and TMJ disorders. Dentists with additional certifications in orofacial pain or oral medicine often have the necessary expertise to diagnose and treat TMJ disorders effectively. You can also check if the specialist is a member of professional organizations such as the American Academy of Orofacial Pain (AAOP) or the American Academy of Craniofacial Pain (AACP). Membership in these organizations often indicates a commitment to staying updated on the latest research and treatment methods.
Experience and Expertise
Experience matters when it comes to choosing a TMJ specialist. An experienced specialist is more likely to have encountered a wide range of TMJ cases and developed effective treatment plans. You can ask the specialist about their experience with cases similar to yours and inquire about their success rates in providing relief to TMJ patients. Experienced specialists are also more likely to have access to advanced diagnostic tools and treatment options.
Patient Testimonials and Reviews
Reading patient testimonials and online reviews can provide valuable insights into the quality of care provided by a TMJ specialist. Look for reviews on reputable websites and forums to learn about the experiences of other patients. Pay attention to both positive and negative feedback, as it can help you gauge the specialist's communication skills, bedside manner, and overall effectiveness in treating TMJ disorders.
Consultation and Communication
A good TMJ specialist should be an effective communicator. During your initial consultation, pay attention to how the specialist listens to your concerns, asks questions about your symptoms, and explains the diagnosis and treatment options. They should take the time to educate you about your condition and involve you in the decision-making process. Open and clear communication is essential for a successful patient-specialist relationship.
Treatment Approach and Technology
Different TMJ specialists may have varying treatment approaches. Some may focus on conservative, non-invasive therapies, while others may recommend surgical interventions in severe cases. The best approach for you will depend on the severity of your condition and your individual needs. Ensure that the specialist discusses the available treatment options and the pros and cons of each. Additionally, inquire about the technology and equipment they use for diagnosis and treatment. Advanced diagnostic tools, such as 3D imaging or electromyography, can improve the accuracy of the diagnosis and the effectiveness of treatment.
Restore Your Comfort With ICCMO
Choosing a TMJ specialist near you is a significant decision, as it can have a profound impact on your quality of life. Don't hesitate to seek a second opinion if you have doubts about the treatment plan or if your symptoms persist.

Our organization's unwavering dedication to providing the best diagnosis for TMJ/TMD is a testament to our mission of restoring comfort and confidence to the lives of those affected by these conditions. Through a combination of cutting-edge techniques and compassionate care, we have made it our purpose to alleviate the pain and suffering that TMJ/TMD can bring. Check our website today to know more about us.
0 notes
Text
when someone tells me I don't look disabled or chronic:
Mental health issues prevail throughout the lifetime of individuals with 22q. In stark contrast to the general public rates of ADHD, ASD, anxiety and mood disorders are greatly elevated in the 22q population. Psychotic symptoms arising in approx. 50% of adolescents progress to psychotic disorders in 10-25% of individuals.
Attention Deficit Hyperactivity Disorder (ADHD) is the most prevalent MH diagnosis in children with 22q.
Problems with sleep are very common in patients with 22q11.2 deletion syndrome. Sleep disordered breathing, including obstructive sleep apnea is seen in about 50% of patients with 22q in craniofacial clinic compared to about 11% in the general population. There are many contributing factors: facial anatomy and palate repairs, and medical issues, for example cardiorespiratory problems. Sleep can also be disrupted with night leg pains. Many patients have anxiety and difficulty falling asleep at bedtime.
Individuals with 22q11.2 deletion syndrome are born with a genetic predisposition to mental ill-health. The majority are faced with a myriad of physical health issues, learning difficulties and a variety of mental health concerns. Poor sleep and sleep disturbances are more common in childhood but can occur at any time and for varying reasons and for some, they can remain a problem over the lifespan.
...lol
0 notes