#nhs england
Text
Why on earth is anyone taking this shoddy cass review seriously?
I'm sorry but it's baffling how an actual government is uncritically taking this review at face value. It literally only comes to the conclusion it does because it ignore literally all other evidence. They excluded a shit ton of studies because they didn't have enough controls, which sounds reasonable but in order to have those controls they'd have to unknowingly give patients placebos instead of the hormonal therapy and puberty blockers they asked for.
That would be an extremely unethical thing to do, and would achieve nothing because the effects of hormonal therapy and puberty blockers are extremely obvious.
Just let that sit with you for a moment. All that clinical evidence completely thrown out the window because they didn't do a horrific and unethical test on their patients. All that clinical evidence ignored because the study was ethical. This is an extreme oversight at BEST and deliberate misinformation at worst. Either way, it makes the review extremely unreliable.
That's just one issue. But the fact that the vast, VAST majority of research was completely ignored due to a ridiculous and unethical requirement should be enough for you to oppose anyone using this as evidence for anything other than why queer people need to be included in scientific discussions about our communities. Because this review is being used to roll back LGBT rights.
#cass review#cass report#queer#queerphobia#transphobia#trans#transgender#nhs england#trans rights#lgbt rights#transgender rights#lgbtq#lgbt#lgbtqia#lgbtq community#queer community#pseudoscience#bad science#feminism#feminist#intersectional feminism#uk#britain#england
154 notes
·
View notes
Text
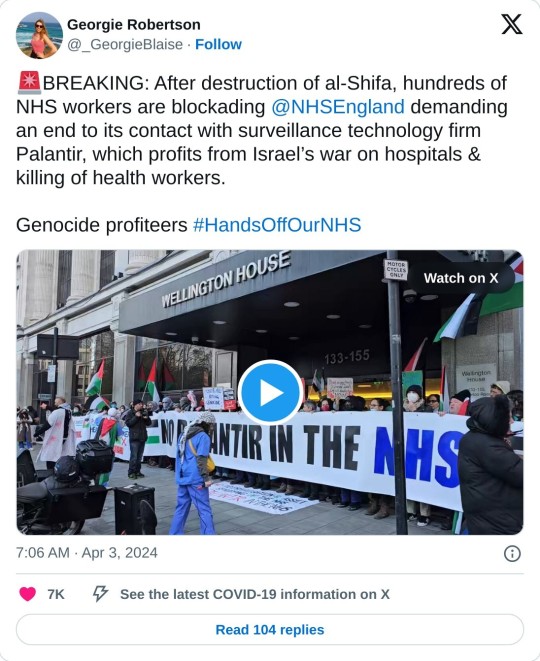
#feminist#social justice#free palestine#palestine#free gaza#current events#current news#settler violence#settler colonialism#settler terrorism#england#british government#nhs england#end the occupation#stop funding genocide#genocide#war on gaza#israel is a terrorist state#israel is evil#global news#healthcare workers#protest#solidarity#al shifa hospital
232 notes
·
View notes
Text
"6 out of 10 people who died from Covid between March and July 2020 were disabled"
As part of the UK covid inquiry, evidence has now been brought to light which shows that "Do Not Attempt Resuscitation" notices, were put on the files of patients with Down's Syndrome, Autism & other learning disabilities.
These people were healthy, before contracting Covid19.
The NHS watchdog we know as NICE, (the National Institute for Health and Care Excellence), issued guidance for trusts and hospitals advising them to apply a “clinical frailty scale” to decide whether patients should be admitted to intensive care.
Older and more frail patients were viewed as being less likely to survive even with critical care treatment.
The original NICE guidance also suggested that those who could not do everyday tasks like cooking, managing money and personal care independently, would be considered frail & not receive intensive care treatment.
This original guidance has since been removed....
Which leads us to the Do not attempt Resuscitation notices...
The DNAR notices were often placed on the files of the patients without their consent, or with limited understanding of its meaning.
Patients with learning disabilities were classed as 'clinically frail'
NHS England have of course denied this, yet the evidence shows they let them die, as to not overwhelm the NHS in the early days of a pandemic.
Yet many specialist nurses have come forward to say that they were constantly put in place for people with learning disabilities and often "inappropriately."
_____
I feel utterly sick. I remember at the start of the pandemic, talking about how disabled people will become a target, that we will be killed off, and people looked at me like I was purple.
4 years later we're here. In case you need to read it again, 6 in 10 people with covid that died during March to June 2020, were disabled. 6 in 10. I can't stop repeating that number.
Read more here:
https://archive.ph/4BQ3s
#covid 19#covid pandemic#long covid#disability#covid inquiry#chronic illness#chronic life#chronically ill#spoonie problems#Disabled not disposable#learning disability#vulnerable#down syndrome#nhs#nhs england#aneurin bevan#Would be spinning in his grave
129 notes
·
View notes
Text
Getting gender-affirming care from NHS England as a trans person can be like
Patient: I'm trans. I'd like gender-affirming healthcare please.
NHS: No.
Patient: WTF?
NHS: Come back in a month. If you're still trans, we'll consider it.
Patient: WTAF?
NHS: Urgh. Fine. I'll refer you to a gender identity clinic.
Patient: How long will that take?
NHS: I dunno. Maybe 2-5 years for a first appointment, depending on which clinic you're referred to.
Patient: WTF? Can't you give me healthcare now? At least HRT?
NHS: Fuck no! We're not qualified for that!
Patient: But you do it all the time for cis people.
NHS: That's entirely different and no, I won't explain why.
Patient: Urgh. Fine. If I get care from a private clinic, will you at least agree to work with them on a shared care basis?
NHS: Hell no!
Patient: Not even if I choose a clinic where the folks running it also still work for the NHS?
NHS: No.
Patient: WTF? I'll just turn to DIY HRT then.
NHS: No! Don't do that! My sudden deep knowledge of HRT tells me that this will be unsafe!
Patient: Then give me an alternative!
NHS: No.
#NHS#trans#transgender#gender-affirming care#healthcare#trans healthcare#transition#England#NHS England#trans rights are human rights#queer#LGBTQ+#LGBTQIA+#non binary#enby#trans fem#trans masc#trans women#trans men
231 notes
·
View notes
Text

#palantir#nhs#nhs england#free palestine#palestine#gaza#free gaza#israel#current events#healthcare#healthcare workers#keep protesting#global protest#protest#protests#uk news#united kingdom#england#england news#hospital#al shifa hospital#stop funding genocide#stop arming israel#stop funding israel
47 notes
·
View notes
Text

#fuck the tories#tories#tory scum#tory party#tory#united kingdom#uk politics#nhs england#uk nhs#nhs crisis#nhs#uk police#ukpol#uk government#uk govt#ukgov#fuck the gop#fuck the police#fuck the supreme court#fuck the patriarchy#ausgov#politas#auspol#tasgov#taspol#australia#neoliberal capitalism#fuck neoliberals#anthony albanese#albanese government
140 notes
·
View notes
Text
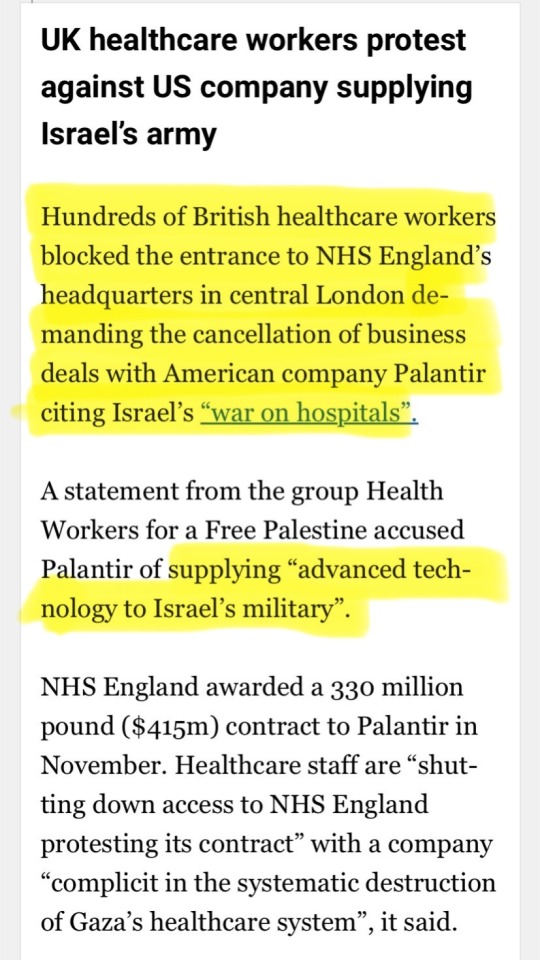
Rowling on the Cass Review.



One of those doubling down on the lies.




#JK Rowling#women#gender critical#Cass Review#The Cass Review#NHS#NHS England#gids#detrans#trans medicine#medical malpractice#trans insanity#Emma Watson#Daniel Radcliffe#I stand with JK Rowling#we were right all along#unfortunately too late for those harmed#Twitter
44 notes
·
View notes
Text


By: SEGM
Published: Apr 15, 2024
The Cass Review of England’s gender services for children and young people, initiated four years ago, culminated earlier this week in the publication of the final 388-page report. The report was accompanied by 9 systematic reviews of evidence supporting the recommendations. Within hours, NHS England responded, thanking Dr. Hilary Cass and her team for “stepping up to lead such a complex review.” NHS England committed to following through on Dr. Cass’ recommendations, and acknowledged the national and international significance of this seminal work: “Your final report will not just shape the future of healthcare in this country for children and young people experiencing gender distress but will be of major international importance and significance.”
A wide range of stakeholders–from patients and clinicians to bioethicists, legal scholars and healthcare historians–will undoubtedly be studying the hundreds of pages of the Cass report and the accompanying studies for weeks and probably years to come. However, there is also considerable urgency to understand its key take-aways and the likely implications.
Balancing two conflicting priorities–the need for an unrushed, thorough and accurate analysis, as well as our commitment to the members of the healthcare community to inform them of key developments in the field–SEGM has decided to release our preliminary analysis. We chose to focus only on the most salient aspects of the Cass Report that will likely lead to a change in clinical practice.
What we present below is SEGM’s interpretation of the key messages in the report. We do not doubt that every person who reads the report will find a new “angle” and perhaps have a different interpretation. As always, we welcome disagreement and debate. The “many eyes of science” are needed now more than ever.
Summary
The Cass Review marks the end in England of the era of a highly medicalized approach to the treatment of young people with gender-related distress, which has come to be known as “gender-affirming care.” While the treatment protocol for youth comprising of puberty blockers, cross-sex hormones, and surgery, known as the “Dutch Protocol,” was invented in the Netherlands in the 1990’s, the report points out the concept of “gender-affirming care”–the notion that the doctors must accept children’s declarations of identity at face value and must assist them in gender change as early as possible–actually originated in the United States, and only then spread internationally.
The Cass Review provides a scathing assessment of the gender-affirming approach in general, and the gender-clinic model of care, which operationalized this approach of on-demand provision of gender-reassignment interventions, in particular. Going forward, England will treat gender dysphoric youth <18 using standard psychological and psychotherapeutic approaches, with very few young people receiving endocrine gender reassignment interventions (gender-transition surgeries for <18s have never been allowed in England). Further, the review noted that the group of young adults 18-25 is subject to many of the same concerns as the <18s, and recommended that the new regional “hubs” being set up to help gender dysphoric youth be expanded to include patients up to 25 years old.
NHS England (NHSE) welcomed the Cass Review’s recommendations and expressed a firm commitment to implement the recommended changes. However, NHSE went one major step further, announcing that they will be initiating a Cass-style review into the adult gender dysphoria clinics (GDCs) in England. NHSE had already decided to bring forward to 2024 its periodic review of the adult “service specifications,” which set out what clinical services adult clinics provide; as a consequence of Cass’ recommendations, they are additionally launching a much broader review of the entire adult gender clinic system. This was in part due to the concerns raised by the Cass Review that a vulnerable group of 17-25-year-olds represents fundamentally the same group of youth as the <18s, and needs similar protections from non-evidence-based practices. Further, whistleblower complaints from adult clinics corroborated concerns that vulnerable adults were not receiving proper evidence-based care. The refusal by all but one adult gender clinic to cooperate in the outcome analysis for the 9000 patients as part of the Cass Review likely contributed to NHSE’s determination to investigate the adult service. Adult gender dysphoria clinics see patients aged 17 and upwards, and NHSE has written to require them to halt appointments with 17-year-olds.
In summary, the care for <18s in England will no longer be based on the “gender-affirming” model of care but instead will treat youth with gender distress similarly to how it treats youth with other developmental struggles. Further, with the announcement of the adult gender clinic review, England starts a new chapter in the history of gender medicine, with a new focus on vulnerable gender-dysphoric young adults.
Many more developments are expected from England in the coming months. To what extent the UK changes will impact the West’s approach to helping young gender-dysphoric individuals remains to be seen. In SEGM’s view, the impact will likely be significant, even if delayed, as other countries contend with England’s findings and their implications for evidence-based clinical practice.
Detail Regarding Social Transition, Puberty Blockers, Cross-Sex Hormones, Surgery, and Overall Care Delivery Model
Social Gender Transition
The Cass Review positions social transition as an active healthcare intervention “because it may have significant effects on the child or young person in terms of their psychological functioning and longer-term outcomes.” (UK and other countries’ clinicians increasingly use “social prescribing” interventions in order to impact health outcomes).
For young children, the review strongly discourages social transition, noting that “sex of rearing” may profoundly alter a child’s developmental trajectory, with long-ranging consequences. Should parents insist on it, the review recommended that a healthcare professional be involved in helping parents understand the risk-benefit ratio of such a profound and likely life-altering decision.
For older teens, the review recognizes the autonomy of young people’s self-expression but strongly recommends that parents be involved in the decision, noting that secret transitions cause a rift between teens and their families, destabilizing the very support networks that are essential for young people’s long-term well-being.
More generally, should social transitions be undertaken, the review recommended only a partial, rather than complete, social transition, especially for younger children, noting how many children currently live in fear of being “found out.” The discontinuation of the use of puberty blockers (discussed next) will make that fear a certainty. Thus, it would be highly unwise for a parent to create a situation where a young child is living in “stealth.”
These recommendations were supported by interviews with patients and families, and by a systematic review of evidence of social transition published in a peer-reviewed BMJ journal. The review found a dearth of evidence and concluded, “professionals working in the area of gender identity and those seeking support should be aware of the absence of robust evidence of the benefits or harms of social transition for children and adolescents.”
The recognition of not only the potential benefits, but also the potential harms, and the unknown benefit-harm ratio of social gender transition is noteworthy.
Puberty Blockers
The use of puberty blockers to stop normally-timed puberty will no longer be offered as part of England’s publicly funded healthcare system. This is not a “new development” as the problems with using puberty blockers for gender dysphoria were already part of the Cass Review’s interim report, and NHSE had updated its puberty blocker policy a month before the issuing of the final Cass Review.
The rationale for withdrawing puberty blockers from medical practice is manifold. It ranges from unclear treatment aims (besides altering a child’s body), a lack of credible evidence that stopping normally-timed puberty leads to improvements in mental health, safety concerns (e.g., bone health), and profound unknowns across a range of health domains, especially brain development. The fact that nearly 100 percent of puberty-blocked youth proceeded with cross-sex hormones was treated as a negative signal that puberty blockers may be setting children on an irreversible path of gender transition.
As we noted in our earlier analysis, the NHS guidance regarding discontinuing the use of puberty blockers for stopping normally-timed puberty affects only the NHS clinics. Private clinics (including the single non-NHS youth clinic operating in the UK, as well as online clinics based abroad but serving UK citizens) are not subject to the NHS policies. This created a loophole that could be exploited to circumvent NHS actions to safeguard England’s youth from harmful medical interventions. In response to these concerns, Health Minister Victoria Atkins made clear the government’s intention to limit private gender care for under 18s and to eradicate the online trade in hormones, following Cass’ recommendations.
As we noted earlier, the NHS intends to conduct research into puberty blockers, and there has been much speculation about research design in general, and the eligibility for research in particular. The quote below from the final Cass Review suggests that eligibility may be limited only to natal males with early-onset and long-lasting gender dysphoria. It appears to suggest that natal females may not be eligible, as they can successfully undergo convincing masculinization with the help of testosterone at virtually any age:
14.56 Transgender males masculinise well on testosterone, so there is no obvious benefit of puberty blockers in helping them to “pass” in later life, particularly if the use of puberty blockers does not lead to an increase in adult Height.
14.57 For transgender females, there is benefit in stopping irreversible changes such as lower voice and facial hair. This has to be balanced against adequacy of penile growth for vaginoplasty, leaving a small window of time tо achieve both these aims.
14.58 In summary, there seems to be а very narrow indication for the use of puberty blockers in birth-registered males as the start of a medical transition pathway in order to stop irreversible pubertal changes. Other indications remain unproven at this time.
As we noted earlier, the NSHE made it clear in its puberty blocker update policy that there are no guarantees that such research will obtain the necessary ethical approval.
Like other recommendations in the Cass Review, the puberty blockers recommendation was based on extensive stakeholder consultation, and supported by a systematic review of evidence, which showed no credible psychological benefits of puberty suppression in the treatment of gender dysphoric youth. As we explained earlier, the original 2020 NICE systematic evidence review was updated in 2023, but newly-identified studies did not change its conclusions.
Cross-Sex Hormones
Shortly before the publication of the final Cass Review, NHSE issued an updated policy about the cross-sex hormones. As we noted at the time in our earlier analysis, the policy was only a minor update, necessitated by the launch of the new gender services, and it represented only minor changes. Cross-sex hormones for those around their 16th birthday were still allowed, although a new centralized team not directly involved in care of the young person would need to approve the medical necessity. At the time, SEGM posited that following the final Cass Review, the NHS will commit to a more thorough review of the cross-sex hormones policy, and further updates. This indeed has occurred.
According to NHS England’s response to the final Cass Report:
NHS England will review the use of gender affirming hormones through a process of updated evidence review and public consultation, similar to the rigorous process that was followed to review the use of puberty suppressing hormones.
NHS England has made clear that there will be a single cross-sex hormones policy “which will cover all people over the age of 16,” with further details to follow.
NHSE acknowledged Dr. Cass’s recommendation that “the new providers should be ‘extremely cautious’ when considering whether to refer young people under 18 years for consideration of hormone intervention.” To support this recommendation while the new cross-sex hormones policy is being developed, NHSE has “established a national multi-disciplinary team (MDT) that will review and need to agree all recommendations for hormone intervention.” Further, NHSE noted that the “first meeting of this new national MDT will take place later this month” chaired initially by Professor Judith Ellis, former CEO of the Royal College of Paediatric and Child Health.
The original NICE systematic review of evidence for the effects of cross-sex hormones was conducted in 2020, and it found similar problems in the evidence base as the puberty blockers review (unreliable evidence base), but with a signal that there may be some small short-term improvements in mental health following cross-sex hormones administration. The new systematic review of cross-sex hormones confirmed these findings.
The final Cass Review expressed concern over how small these changes were, considering the fact that the introduction of the long-awaited cross-sex hormones and desired physical changes is expected to lead to short-term improvements in mood. This suggests that the Cass Review is concerned not only with the low certainty of the reported benefits due to poor study designs, but also with the possibility that the small improvements may be short-lived and due to the potential placebo effect:
15.27 When a young person has been on puberty blockers, a short-term boost in mental wellbeing is to be expected when sex hormones are introduced. Testosterone is faster to produce physical changes than oestrogen, and birth-registered girls can expect to start seeing body changes in line with their identified gender within a few months. The start of long anticipated physical changes would be expected to improve mood, at least in the short term, and it is perhaps surprising that there is not a greater effect size. However, much longer term follow-up is needed to understand the full psychological impact of medical transition.
The NHSE’s announcement made it clear that the final cross-sex hormones policy will be based on the updated systematic review of evidence.
Surgery
Surgeries have never been available to under 18’s in England, so no systematic reviews of surgeries has been conducted, and no additional changes to the policy for youth under 18 are needed. However, NHSE’s announcement of the Cass-style review into the adult gender clinics raises questions about whether surgical interventions for young adults will now come under scrutiny as well.
Change in the Delivery Care Model Overall
In addition to making specific recommendations overall about social transition and endocrine interventions, the review challenged the concept that gender dysphoria/gender incongruence in youth as an exceptional condition that needs exceptional treatments delivered via exceptional models of care exemplified by gender clinics.
The healthcare delivery system for gender dysphoric youth will be restructured to provide a fundamentally different model of care, and realign it with the way care is typically organized in England. Every gender-dysphoric child or young person will have a dedicated primary care provider (a pediatrician or a GP) overseeing their care and well-being. Children and young people with mental health conditions, or those whose gender incongruence is causing distress, will receive psychotherapeutic and psychological services from the second level of care at the Child and Adolescent Mental Health Services (CAMHS).
Very few young people will be referred to super-specialized tertiary services, which will carefully examine the medical necessity of cross-sex hormones. The referring clinicians will need to demonstrate why cross-sex hormones delivered to under-18’s are medically indicated and preferred over allowing the young person to reach maturity, and a centralized team not directly involved in the care of the young person will need to agree with this assessment. It is expected that in the end, very few young people will be treated with interventions to alter their bodies.
Other notable aspects of the final report
The final Cass Review made a number of other highly consequential statements and observations. It is impossible to do a thorough overview of all of them given the short time since the report’s release, but we will highlight several that stood out to SEGM as particularly noteworthy.
Although chiefly forward-looking, the review described the alarming inadequacies of clinical practice at GIDS.
While the focus is on service improvement, the legal ramifications of the unsafe practice at GIDS in the longer term must be apparent to NHSE. GIDS refused to participate in the review’s research study, to compare clinical practice at a range of European pediatric gender clinics, therefore the report (at Appendix 9) of the Multi-Professional Review Group (MPRG) which oversaw GIDS’s referrals for puberty blockers is the major source of information about what went on there. The MPRG painted an extraordinary picture. It was not clear how thoroughly different treatment options had been discussed, and most children and parents were asking to obtain puberty blockers from their first appointment with GIDS, having “turned for information to the media and online resources, with many accessing LGBTQ+ and GD support groups which appear to be mainly affirmative in nature.”
Concerns of over treatment of neurodiverse and same-sex attracted youth.
Neurodiversity was suspected or diagnosed in a majority of children referred for puberty blockers and where sexuality was discussed “most cases are of same sex, opposite-gender attracted children.” The MPRG were “concerned about the lack of evidence of professional curiosity” about these children’s lives shown by GIDS clinicians. A recurrent concern was “the inadequacy and on occasion inaccuracy of answers given to children and their families by GIDS and their failure to correct child and parental misconceptions about puberty, puberty blockers and hormones.” Unsurprsingly, then, they note that the Care Quality Commission’s (CQC) observation that consent taking was judged to be “not in line with NHS and GMC requirements.” Records varied “from succinct to disorganised.”
A scathing assessment of poor quality and lack of independence for the guidelines by WPATH, The American Academy of Pediatrics (AAP), and the Endocrine Society (ES).
As part of the Cass Review, an independent team of research methodologists assessed all the current treatment guidelines and recommendations for quality in a systematic review, using the internationally recognized AGREE II methodology for evaluating guideline quality. The AAP 2018 treatment recommendations guidelines scored amongst those at the bottom of the 23 reviewed guidelines. The WPATH and the ES treatment recommendations did not fare much better. The review noted a marked lack of independence in guideline authorship, noting circular referencing: one non-evidence-based guideline was used to justify another non-evidence-based guideline’s recommendation. The significant overlap in authorship between the guidelines (especially between WPATH and ES) was noted as a significant cause for concern, as was WPATH’s refusal to acknowledge the results of their own systematic review in its adolescent section. The report points out that only the Swedish and Finnish treatment recommendations appear credible, but even they lack the specificity needed for the NHS to operationalize the treatment recommendations in the UK context. The concern over the proliferation of non-evidence-based guidelines, which at times do acknowledge the poor quality evidence but then issue strong recommendations to medically transition youth anyway, has been seconded in the BMJ article dedicated to this specific aspect of the Cass review findings.
Condemnation of the “toxic” nature of debate within which standard psychological therapies were rebranded "conversion practices."
The Cass Review drew attention to the difficulty of undertaking the review amid an “increasingly toxic, ideological and polarized public debate” that ill-served children. The report noted that it is essential to explore children’s complex needs and stated that it is “harmful to equate this approach to conversion therapy as it may prevent young people from getting the emotional support they deserve.” Furthermore, potential accusations of conversion practice “when following an approach that would be considered normal clinical practice” in other scenarios made clinicians wary of offering support to young people, leaving them without the help they deserve. The report highlighted the potential for legislation on conversion practices to complicate the situation and emphasized that “strong safeguards must be built into any potential legislation” to guard against the risk that clinical staff feel that discharging their duty of care would expose them to legal challenge.
Questioning the assumption of the gender identity theory.
While some have criticized the Cass Review for relying on constructs coming from the gender identity theory (e.g., referring to “gender identity” without critically assessing the origin and validity of this concept), the report did briefly address the outdated nature of the assumptions on which the “gender-affirming” care model is based. The report noted that the theory of gender identity development was set forth in 1966 by Kohlberg, who described a typical progression whereby by the age of 5-6, children develop gender identity constancy.
The report noted the obvious fact that the current patterns of both identifying as transgender for the first time at much older ages and also the growing phenomenon of detransition and re-identification with natal sex demonstrably contradict this theory.
The review considered a range of factors that may have contributed to the current phenomenon of a sharp rise of trans identification in youth. It noted that while biology likely plays a role, “since biological factors have not changed in the last 10 years it is necessary to look at other possible reasons for the increase in referrals and the disproportionate representation of birth-registered females.”
8.23 For children and young people with gender incongruence, ‘innate’ or biological factors may play a part in some individuals, in ways that are not yet understood, and in others psychosocial factors, including life experiences, societal and cultural influences, may be more important. Since biological factors have not changed in the last 10 years it is necessary to look at other possible reasons for the increase in referrals and the disproportionate representationof birth-registered females.
Recognition that the challenges in the mental health of Generation Z are likely at the root of the current phenomenon of trans identification in youth.
The report acknowledged the likely multi-factorial basis for the current explosion of gender-dysphoric youth, with a focus on “Gen Z” and the significant mental health crisis affecting this population more generally, as well as the role of social media.
7.21 The striking increase in young people presenting with gender incongruence/dysphoria needs to be considered within the context of poor mental health and emotional distress amongst the broader adolescent population, particularly given their high rates of co-existing mental health problems and neurodiversity.
7.22 Internationally, there have been increasing concerns about the mental health of Generation Z. The reasons for this are highly speculative, although there is ongoing debate about the contribution of excessive smartphone use and social media as discussed above.
Suggestion that the invention and the availability of the Dutch protocol likely contributed to the rapid rise in gender dysphoria in youth.
The report noted that the sharp rise in the numbers of gender dysphoric youth in the West also coincided with the introduction of puberty blockers into general medical practice. Of note, the Netherlands experienced a similar spike several years before the rest of the West–and incidentally, the Netherlands introduced the Dutch protocol/blockers into clinical use several years before the rest of the West. This lends further credibility to the theory that the very availability of the Dutch protocol treatment may have contributed to the growing numbers of youth seeing their developmental struggles through the “gender identity” lens and pursing medical interventions.
8.50 The dramatic increase in presentations to NHS gender clinics from 2014, as well as in several other countries, coincided with puberty blockers being made available off protocol and to a wider group of young people. The only country with an earlier acceleration in referrals is the Netherlands, where the Dutch protocol was developed.
Clear attribution of the “gender-affirming” model of care to the United States.
While it was the Dutch clinicians who came up with the “innovative clinical practice” to use puberty blockers in an off-label way to stop normally-timed puberty of gender-dysphoric youth, the report suggests that it was the Americans who propagated the approach of allowing the child to direct what medical interventions they need based on their self-declared identity.
Specifically, the review credits an American psychologist Diane Ehrensaft, who pioneered and promulgated this theory, which has become the core of the “gender-affirming” model of care. The report describes the model as a belief that “a child of any age may be cognizant of their authentic identity and will benefit from a social transition at any stage of development.”
2.13 In 2007 Norman Spack established a clinic in Boston, USA modelled on the Dutch protocol and began prescribing puberty blockers from early puberty (Tanner stage 2).
2.14 Practice in the USA began to diverge from the models of care in Canada and the Netherlands, following instead a gender affirmative model advocated by Diane Ehrensaft (Eherensaft, 2017). She described the three approaches as follows (Ehrensaft, 2017):
“The first model, represented in the work of Drs Susan Bradley and Ken Zucker [Canada], assumes that young children have malleable gender brains, so to speak, and that treatment goals can include helping a young child accept the gender that matches the sex assigned to them at birth.
The second model, represented in the work of practitioners in the Netherlands, allows that a child may have knowledge of their gender identity at a young age, but should wait until the advent of adolescence before engaging in any full transition from one gender to another.
The third model, represented in the work of an international consortium of gender affirmative theoreticians and practitioners, allows that a child of any age may be cognizant of their authentic identity and will benefit from a social transition at any stage of development.”
2.15 The third model - the ‘affirmative model’ - has subsequently become dominant in many countries. As a result, some gender services have moved away from a more exploratory approach, and this is seen by some advocacy and support groups as a move to ‘gatekeeping’ model.
Incidentally, (a fact the the report does not mention), Ehrensaft was also a notable figure in promoting the now-defunct theory of repressed memory of satanic abuse, and published on the subject. This subject is outside the scope of this analysis, but notably, the epidemic stopped only after successful lawsuits demonstrating that some psychologists facilitated the patients’ “recovering” non-existing memories of abuse as an explanation of the patient's distress.
Clear acknowledgment of detransition as a growing phenomenon that can no longer be ignored.
There was a chapter dedicated to detransitioners, and the term “detransition” was mentioned in the report over 80 times, citing a number of studies from the UK and internationally. The report recognized that the rate of detransition and regret among the novel population of youth is unknown, but suggested it is no longer negligible, citing a UK study of double-digit detransition in a relatively short follow-up period. Of note, a recent US study found that among participants who were medically transitioning, almost 30 percent ceased medical transition based on a 4-year average followup, but the reasons for the cessation were not explored.
Suggestion of lack of data integrity in gender clinics.
The Cass Review revealed that in a truly unexpected turn of events, all but one adult gender clinic refused to cooperate in a data analysis project that would have allowed tracking of longer-term outcomes of 9,000 gender dysphoric young people, which included both those who underwent gender transitions as well as those who chose less invasive options. The responsibility for the research, which has obtained ethics permission, has now been handed over to NHSE, which will conduct the review without the gender clinics’s cooperation. The objection of the gender clinics and the responses to those objections (both contained in the appendices to the report) suggest that the reasons for the lack of cooperation may be ideological.
Further, there are indications through the report that there may be a lack of integrity in the gender clinic approach to data collection and reporting more generally. For example, the Cass team was advised by GIDS/Tavistock (the youth gender clinic) that only 27 percent of the referred cases were referred for endocrine interventions (puberty blockers and/or cross-sex hormones), creating the impression that only a minority of gender dysphoric youth are intervened with medically.
However, the context of the report signaled that this figure is open to misinterpretation (without directly calling it misleading). The report noted that the 27 percent only applies to the young people who were referred directly to the two adolescent endocrine centers. Among the 73 percent “non-referred” for endocrine interventions, 69 percent actually went on to adult gender clinics, where most likely received hormonal interventions.
The question of what percentage of youth referred to gender clinics end up transitioning is an open one. In the Netherlands, which claims a cautious approach, this number appears to be around 70-80 percent. It is reasonable to expect similar or even higher numbers among gender clinic staff who subscribe to the “gender-affirming” model of care.
Problems with applying the Dutch protocol to the “wrong” population.
The report clarifies that GIDS/Tavistock’s approach to validating the Dutch protocol failed on at least 3 accounts. As previously discussed, the clinic started scaling the treatment before they analyzed and published the results and they also changed the protocol where the minimum age of 12 for puberty blocked was dropped and replaced by pubertal tanner stage 2 stage–which can be as young as ages 8-9 in girls. However, the report highlights another important deviation, which may be responsible for the sheer scale of the current problem.
While the research study (aka “Early Intervention Study”) was only approved to include youth with the classic early childhood, the pre-pubertal onset of gender dysphoria that intensified in adolescence with no other significant mental health problems (to replicate the Dutch research), when the clinic chose to scale it widely, it expanded eligibility to all youth including those whose gender dysphoria emerged post-puberty and in the context of complex mental health problems (p. 73). The latter group currently represents the single biggest affected demographic.
The fact that the Dutch research is currently being applied to the very demographic which was originally contra-indicated for gender transition and that this problem is not confined to the UK but is a worldwide problem, has been highlighted in a number of recent publications and emphasized in the Cass report.
The current “suicide and suicidality narrative” surrounding gender-dysphoric youth is misleading.
The Cass Review noted that “balanced information, which is realistic and practical, and does not over-exaggerate or underestimate the risks, is essential to support everyone involved and identify young people in most urgent need of help.” The review commented on the thankfully low rates of completed suicides in the population of trans-identified youth, pointing out the latest evidence from Finland. However, the review appropriately recognized every suicide is a tragic event and the causes in each individual case must be clearly understood. The report noted a recent UK analysis of suicides using the National Child Mortality Database (NCMD). The analysis of 91 cases of youth suicides between April 2019 and March 2020 (1-year span) identified 108 total deaths across the entire population of the UK that were likely due to suicide. In examining the factors contributing to suicides, the Child Death Overview Panel concluded that Household functioning was found to be the most common contributing factor (69%), followed by mental health problems (55%), bullying (23%), and neurodevelopmental conditions (16%). Sexual orientation, sexual identity, and gender identity were assessed as a factor in 9 percent of total suicides. The Cass report did not provide an additional breakdown for sexual orientation vs gender identity. However, the report did note that systematic reviews failed to provide evidence that endocrine interventions reduce suicides.
The problem with the notion of the “diagnostic assessment.”
The report zooms in on a central argument leveled by gender-affirming clinicians that “gender-affirming” treatments are only provided following a diagnostic assessment, and therefore are medically necessary. The review aptly points out that neither the DSM-5 diagnosis of “gender dysphoria,” nor the “de-pathologized” ICD-11 diagnosis of “gender incongruence,” have a known predictive validity. In other words, a young person can meet the diagnostic criteria today, but nothing is known about how likely the young person is to continue to experience gender-incongruent feelings in the future.
16.8 A formal diagnosis of gender dysphoria is frequently cited as a prerequisite for accessing hormone treatment. However, it is not reliably predictive of whether that young person will have longstanding gender incongruence in the future, or whether medical intervention will be the best option for them. Depending on what has caused their distress or dysphoria, it may be resolved by medical treatment, but it may also be resolved in other ways.
The Cass Report notes, “The Review was unable to obtain clear criteria from the GIDS team on their criteria for referral for endocrine intervention.” The report also points out that if the causes for gender-related stress are “psychosocial,” “sociocultural” and/or “dynamic,” providing invasive and irreversible interventions to such young people presents a challenging ethical dilemma.
16.9 As discussed in Chapter 8, the nature and causes of gender dysphoria/incongruence are complex and poorly understood, and there is very limited understanding of the currently presenting population of predominantly birth registered adolescent females. Each individual will have a different mix of biopsychosocial factors, but if potentially dynamic psychosocial or sociocultural factors predominate in a significant proportion of people, one of the most challenging ethical questions is whether and/ or when medical intervention is the correct response.
Further, the report takes on the notion of the “diagnostic assessment” itself, noting that there is no formalized assessment process whereby one can determine how to conduct such an assessment, and how to arrive at predictable outcomes as to which young person is referred to the endocrine interventions and which one is not. The report notes:
10.17 There was also a general lack of understanding among service users participating in the lived experience focus groups about what the assessment was for and confusion about what was assessment and what was diagnosis. Thoughts on the purpose of the assessment included:
• To support young people to explore their options and access the care that’s right for them.
• To get validation of their trans identity and access to the medication pathway.
• To make the person comfortable and focus on what they’re looking for from the service.
• To ensure patients have an understanding of the healthcare options available.
The report concluded that, following a review of international clinical practice, “there was no approach to assessment that could be directly adopted for use in the NHS.” One needs to be developed to meet key goals (support identification of individual needs, allow outcomes to be measured more consistently and ensure children and young people have a similar experience of the service.)
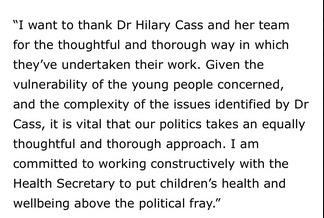
The fundamentally new model will focus on assessment with the goal of “case formulation” followed by psychotherapy as the first line of treatment.
The new treatment framework will be comprised of the assessment, case formulation, diagnosis, care plan. Due to the problems described above (lack of specificity of what the goal of the “assessment” are), the report sets out a new and clear expectation of the role of the assessment. Rather than attempting to identify which young person should be referred to endocrine interventions, the goal is to “derive a multi-level formulation for a child or young person who presents to the NHS seeking help around their gender or experience of gender-related distress.”
The starting point of the assessment is to assess immediate risk and assess complex care needs. Assuming any immediate risks (if any) are addressed using standard psychotherapeutic approaches, the next goal is to come up with a “case formulation.” A case formulation is a standard psychotherapeutic process whereby clinicians synthesize the complexity of the young person’s situation to develop an individualized treatment plan.
The report makes it clear that if any interventions are indicated, standard psychotherapeutic interventions for mental health conditions, as well as more specific exploration of gender-related distress (if indicated), will be the primary treatment. Referrals to endocrine interventions will only be accepted from the Child and Adolescent Mental Health Services (CAMHS) with onus on the clinician making the referral to demonstrate to a centralized team that includes members not directly involved in the care the medical necessity of cross-sex hormones. As mentioned elsewhere, Cass recommended extreme caution in prescribing cross-ses hormones to youth, and the NHS has committed to updating its current cross-sex hormones policy to align it with the final report recommendations.
Recognition of the need to update the diagnostic categories to meet the changing clinical presentations of gender-related distress, and the phenomenon of detransition.
The Cass Review subtly but powerfully signals that the DSM-5 “gender dysphoria” diagnosis appears to be preferred by most clinicians, while the attempt to “de-pathologize” the condition in ICD-11 is less clinically useful.
At the same time, the report recognizes that neither of these diagnostic categories are adequate for the current complexity of the presentations. The diagnosis itself was criticized for relying on outdated notions of preferences for sexed stereotypes from “previous decades,” and the “DSM-5 diagnostic criteria for gender dysphoria has a low threshold based on overlapping criteria” leading to the risk of overdiagnosis and overtreatment. Further, the report indicated that the diagnosis is unhelpful in the care for the growing number of detransitioners as it does not have any specific categories for this growing patient population.
New focus on young adults.
The report recognized the new understanding of adolescent development and that adolescence does not stop at 18 but extends into mid-20s. Noting the disproportionate number of non-neurotypical individuals struggling with gender identity, the report noted that neurodiverse young people are particularly vulnerable “into their early 20s or longer because of their tendency to want black-and-white answers, and their difficulty in tolerating uncertainty.”
Consistent with that, the report recommends that the restructured approach to gender-dysphoric youth does not stop at 18, but subsumes the category of young adults. In addition, the report notes that while the provision of adult gender services fell outside of the review’s remit, several staff in adult gender clinics “contacted the Review in confidence with concerns about their experiences working in adult gender services.” Adult clinic “whistleblowers” shared that adult services experienced a similar influx of young adults, primarily females with complex mental health problems, presenting to adult gender clinics with an expectation of rapid provision of “gender-affirming” medical interventions, as well as growing numbers of detransitioners. The whistleblowers expressed deep concerns about the harm to the vulnerable population of young adults which seemed to represent the same demographic that began to be seen at the Tavistock a few years ago.
As a result, the review recommended a heightened focus on the adult services, and the NHS has responded by announcing an investigation into the adult NHS gender clinics.
Call for the development of new treatments and clear clinical targets.
The review recognizes the the evidence base for psychotherapeutic approaches to the management of gender dysphoria in youth is very low quality. At the same time, the report pointed out that standard therapeutic interventions for distress are the standard of care in medicine, and that no studies of the application of this approach to gender dysphoria have shown harm.
The review stated unambiguously that the “ultimate goal of any intervention is to help the child or young person to function and thrive, they need to be provided with tools and strategies to give them the best opportunity to do so.” The review called for the development of an “explicit clinical pathway for non-medical interventions, as well as a research strategy for evaluating their effectiveness.”
With this recommendation, the Cass report has redirected the clinical community towards the development and study of non-invasive clinical interventions with a focus on long-term outcomes, with the goal of helping young people achieve the best quality of life.
SEGM Take-Aways
The single most salient take-away is that the so-called “gender-affirming” model of care, which treats young people’s declarations of transgender identity as an indication that any physical body modification desired by the young person is medically necessary, is over in England. So is the era of the “gender-clinic model of care,” which exists to operationalize the highly medicalized “gender-affirming” care model.
We end our take-away by pointing the readers to a powerful editorial by the BMJ Editor in Chief. The entirety of this short editorial is worth reading, but we will highlight the more salient quotes below:
“Offering treatments without an adequate understanding of benefits and harms is unethical. All of this matters even more when the treatments are not trivial; puberty blockers and hormone therapies are major, life altering interventions.”
“Without doubt, the advocacy and clinical practice for medical treatment of gender dysphoria had moved ahead of the evidence—a recipe for harm.”
“...Families, carers, advocates, and clinicians—acting in the best interests of children and adolescents—face a clear choice whether to allow the Cass review to deepen division or use it as a driver of better care.”
This analysis, published by the Editor-in-Chief of one of the most prestigious medical journals in the world, signals that the implications of the Cass Review will likely reverberate worldwide. It now appears inevitable that the arc of history has bent in the direction of reversal of gender-affirming care worldwide, although in some countries it will take considerably longer to change medical practice.
The Cass Review is a historic document the significance of which cannot be overstated. It is also multi-faceted, and no single analysis can do it justice. We have done our best to synthesize the most salient aspects of the review after a single reading. We have no doubt that we missed other important aspects and we trust that others will point them out.
#SEGM#Society for Evidence Based Gender Medicine#Cass report#Cass review#Dr. Hilary Cass#Hilary Cass#NHS England#National Health Service#gender affirming care#gender affirming healthcare#gender affirmation#medical scandal#medical malpractice#medical corruption#religion is a mental illness
11 notes
·
View notes
Text
This is really different from my usual posts, but I really don't care. I currently live in a region of the UK, and the NHS England review has a very bad implication for my future. I might head out early, if you catch my drift. When I go quiet for a while, you'll know why
#trans rights#Gabriel talks#fuck the nhs#nhs england#cass review#cass report#trans rights are human rights
19 notes
·
View notes
Text
Nurses are not heroes.
That was a dangerous narrative perpetuated by the government and media at the height of Covid. It prevents them from being seen as human with human needs. Now it’s being used by the same media and government to justify the horrendous working conditions and pressure they are being put under.
Nurses stay unpaid after every shift to help their patients and colleagues. That’s great! Nurses are heroes ❤️
Nurses working through their breaks to help their patients. That’s great! Nurses are heroes. ❤️
Nurses are dealing with unalive and traumatic situations every day. Nurses are heroes ❤️
Nurses get beaten and abused on shift by patients and relatives but it’s ‘part of the job’. Nurses are heroes ❤️
There is nothing heroic about a person not getting adequate rest between shifts. An exhausted nurse should not be looking after anybody other than themselves. They are human.
There’s nothing heroic about a person not being able to provide themselves with adequate nutrition or hydration. They are human.
There is nothing heroic about not receiving proper support or acknowledgment of the trauma they go through every day. Same with assistants and paramedics. They’re still human.
There is nothing heroic about being black and blue by a patient or stalked by a relative and having to see them the next day. Not being able to do anything about it because it’s seen as ‘part of the role’.
There is a massive difference between ‘knowing what you’re getting into’ as a newly qualified nurse and treating them with disrespect, running them into the ground and expecting them to be ok with not having their basic needs met for the needs of the general public.
The nurses wages do not reflect their working conditions or the trauma they experience and have to heal from. They are human and grieve for their patients too. They don’t reflect that this a vocation requiring a degree. That nurses don’t just ‘make beds’, they insert tubes down peoples throats to breathe for them, take chest drains out, keep people alive with complex concoctions of medications they’ve mixed. And so much more.
The NHS has relied on the generosity of its nurses and assistant staff for too long. That generosity is wearing out. What we are being put through isn’t worth our wages anymore.
Stop advertising nurses as heroes and force the public and parliament to see us as the humans we are.
#healthcare#medicine#nurses#strikes#uk government#uk politics#registered nurse#fair pay for nursing#rcn strike#rcn#nhs england#news#uk media#uk nurses#nhs#national health service
97 notes
·
View notes
Text
In December 2023, Jordan Smitheman collapsed and died from an asthma attack. Now his mum Donna and the rest of Jordan’s family are campaigning to make inhalers free in England and you can sign their petition here:
In case you didn’t know, asthma medication such as inhalers are not free in England. I, like many others diagnosed with chronic asthma in this country, have to pay to breathe. Sounds inhumane because it is.
“Asthma accounts for 2-3% of primary care consultations. It impacts on everyday life such as education and work and leads to 60,000 hospital admissions and 200,000 bed days per year in the UK (NICE). Asthma attacks kill three people in the UK each day and every 10 seconds someone has a potentially life-threatening asthma attack.” Source: NHS England
In England, if you take diabetes medicine, you're entitled to free prescriptions for all your medicines, including medicines for other conditions. In England, if you have epilepsy and take epilepsy medicines, you are entitled to a medical exemption certificate which lets you get free prescriptions. Yet the same is not true for asthma, a lifelong respiratory disease with no cure that requires medication and regular checkups.
If I didn’t have my inhalers, I would die, and people can still die from asthma even when they’re taking medication. So why should anyone have to pay to breathe, to live?
Currently, I pay £111.60 for a 12 month prepayment certificate, which works out cheaper in the long-run for the cost of my monthly medications. If I didn’t have this, I would be paying £9.65 per item, and I currently have prescriptions for 2 asthma inhalers as well as a separate medication. If I need 2 inhalers a month, I’d be almost £20 out of pocket, and that’s without taking my other medication into account. If I use my reliever a lot that month and need an emergency inhaler - which has happened many times - that’s another £9.65 on top. It’s not cheap. Not everyone can afford it.
Jordan’s mum Donna says it best on the petition page:
“We believe that access to life-saving medication should be a right, not a privilege determined by one's ability to pay. We call upon the NHS and the government of England to make all asthma treatments free of charge. This will ensure that everyone suffering from this condition has equal access to necessary care and can manage their symptoms effectively without fear of cost.”
Please sign and share the petition. ❤️
7 notes
·
View notes
Video
Nurses in England, Wales and Northern Ireland started a nationwide strike on Thursday, in the largest action of its kind in NHS history. Staff continued to provide "life-preserving" and urgent care. Laura is one of those Nurses and she was on strike in the UK city of Liverpool.
The Royal College of Nursing said staff had been given no choice after Government ministers refused to reopen pay talks. RCN general secretary Pat Cullen has called on the Government to "do the decent thing" and resolve the dispute.
"We need to stand up for our health service, we need to find a way of addressing those over seven million people that are sitting on waiting lists, and how are we going to do that? By making sure we have got the nurses to look after our patients."
#liverpool#trade unions#royal college of nursing#nursing#uk government#manchester#nhs england#NHS#wales#northern ireland#student#protest#politics#government#economics#Labour Party#keir starmer#rishi sunak#conservative party#Healthcare#london#newcastle#scotland
56 notes
·
View notes
Text
#guilty feminist#the guilty feminist#feminism#feminist#women’s rights#deborah frances white#human rights#instagram#uk politics#woman’s rights#uk news#fuck the tories#nurses strike#nhs england#jan 2023
46 notes
·
View notes
Text




#Prince William#Prince of Wales#British Royal Family#Suicide Bereavement UK#At Your Side#Armed Forces Suicide Bereavement Study #NHS England#Armed Forces#suicide bereavement research #military veterans#mental health#support#military families#suicide#military service
4 notes
·
View notes
Text
To my fellow brethren in the UK facing a difficult winter this year on top of a medical system shattering under the weight of incompetent political interference just remember: the possessions of Tories make for excellent kindling, and in a pinch so do their clothes. Whether they’re wearing them or not at the time is of no consequence.
I know we like to rally behind the slogan “eat the rich” but just remember, these vermin are poisonous and of no value, nutritional or otherwise.
55 notes
·
View notes
Text
Post surgery update (+)
I managed to get out of pyjamas and into my cat onesie today. I very much consider this progress 🥰

My bowels are starting to get back into a rhythm, my pain is reducing, and I'm noticeably getting stronger each day.
I'm currently fortunate enough to have a community nurse come by daily each morning to clean and change the packing and dressing over my former stoma site.
Recovery is still a pain, but it's much more preferable to having a stoma 🥰
6 notes
·
View notes