#Medicare Advantage
Text
Private equity finally delivered Sarah Palin's death panels

Tonight (Apr 26), I’ll be in Burbank, signing Red Team Blues at Dark Delicacies at 6PM.

Remember “death panels”? Sarah Palin promised us that universal healthcare was a prelude to a Stalinist nightmare in which unaccountable bureaucrats decided who lived or died based on a cost-benefit analysis of what it would cost to keep you alive versus how much your life was worth.
If you’d like an essay-formatted version of this post to read or share, here’s a link to it on pluralistic.net, my surveillance-free, ad-free, tracker-free blog:
https://pluralistic.net/2023/04/26/death-panels/#what-the-heck-is-going-on-with-CMS
Palin was right that any kind of healthcare rationing runs the risk of this kind of calculus, where we weight spending $10,000 to extend a young, healthy person’s life by 40 years against $1,000 to extend an elderly, disabled person’s life by a mere two years.
It’s a ghastly, nightmarish prospect — as anyone who uses the private healthcare system knows very well. More than 27m Americans have no health insurance, and millions more have been tricked into buying scam “cost-sharing” systems run by evangelical grifters:
https://www.nytimes.com/2020/01/02/health/christian-health-care-insurance.html
But for the millions of Americans with insurance, death panels are an everyday occurrence, or at least a lurking concern. Anyone who pays attention knows that insurers have entire departments designed to mass-reject legitimate claims and stall patients who demand that the insurer lives up to its claim:
https://kffhealthnews.org/news/article/khn-podcast-an-arm-and-a-leg-how-to-shop-for-health-insurance-november-24-2021/
The private healthcare sector is designed to deny care. Its first duty is to its shareholders, not its patients, and every dollar spent on care is a dollar not available for dividends. The ideal insurance customer pays their premiums without complaint, and then pays cash for all their care on top of it.
All that was true even before private equity started buying up and merging whole swathes of the US healthcare system (or “healthcare” “system”). The PE playbook — slash wages, sell off physical plant, slash wages, reduce quality and raise prices — works in part because of its scale. These aren’t the usual economies of scale. Rather the PE strategy is to buy and merge all the similar businesses in a region, so customers, suppliers and workers have nowhere else to turn.
That’s bad enough when it’s aimed at funeral homes, pet groomers or any of the other sectors that have been bigfooted by PE:
https://pluralistic.net/2022/12/16/schumpeterian-terrorism/#deliberately-broken
But it’s especially grave when applied to hospitals:
https://pluralistic.net/2020/05/21/profitable-butchers/#looted
Or emergency room physicians:
https://pluralistic.net/2022/03/14/unhealthy-finances/#steins-law
And if you think that’s a capitalist hellscape nightmare, just imagine how PE deals with dying, elderly people. Yes, PE has transformed the hospice industry, and it’s even worse than you imagine.
Yesterday, the Center for Economic and Policy Research published “Preying on the Dying: Private Equity Gets Rich in Hospice Care,” written by some of the nation’s most valiant PE slayers: Eileen Appelbaum, Rosemary Batt and Emma Curchin:
https://cepr.net/report/preying-on-the-dying-private-equity-gets-rich-in-hospice-care/
Medicare pays private hospices $203-$1,462 per day to take care of dying old people — seniors that a doctor has certified to have less than six months left. That comes to $22.4b/year in public transfers to private hospices. If hospices that $1,462 day-rate, they have lots of duties, like providing eight hours’ worth of home care. But if the hospice is content to take the $203/day rate, they are not required to do anything. Literally. It’s just free money for whatever the operator feels like doing for a dying elderly person, including doing nothing at all.
As Appelbaum told Maureen Tkacik for her excellent writeup in The American Prospect: “Why anybody commits fraud is a mystery to me, because you can make so much money playing within the guidelines the way the payment scheme operates.”
https://prospect.org/health/2023-04-26-born-to-die-hospice-care/
In California, it’s very, very easy to set up a hospice. Pay $3,000, fill in some paperwork (or don’t — no one checks it, ever), and you’re ready to start caring for beloved parents, grandparents, sisters, brothers, aunts and uncles as they depart this world. You do get a site inspection, but don’t worry — you aren’t required to bring your site up to code until after you’re licensed, and again, they never check — not even if there are multiple complaints. After all, no one at the Centers for Medicare & Medicaid Services (CMS) has the job of tracking complaints.
This is absolute catnip for private equity — free government money, no obligations, no enforcement, and the people you harm are literally dying and can’t complain. What’s not to like? No wonder PE companies have spent billions “rolling up” hospices across the country. There are 591 hospices in Van Nuys, CA alone — but at least 30 of them share a single medical director:
https://auditor.ca.gov/reports/2021-123/index.html#pg34A
Medicare caps per-patient dispersals at $32,000, which presents an interesting commercial question for remorseless, paperclip-maximizing, grandparent-devouring private equity ghouls: do you take in sick patients (who cost more, but die sooner) or healthy patients (cost less, potentially live longer)?
In Van Nuys, the strategy is to bring in healthy patients and do nothing. 51% of Van Nuys hospice patients are “live discharged” — that is, they don’t die. This figure — triple the national average — is “a reliable sign of fraud.”
There are so many hospice scams and most of them are so stupid that it takes a monumental failure of oversight not to catch and prevent them. Here’s a goodun: hospices bribe doctors to “admit” patients to a hospice without their knowledge. The hospice bills for the patient, but otherwise has no contact with them. This can go on for a long time, until the patient tries to visit the doctor and discovers that their Medicare has been canceled (you lose your Medicare once you go into hospice).
Another scam: offer patients the loosest narcotics policy in town, promising all the opioids they want. Then, once their benefits expire, let them die of an overdose (don’t worry, people who die in hospice don’t get autopsies):
https://www.newyorker.com/magazine/2022/12/05/how-hospice-became-a-for-profit-hustle
You can hire con artists to serve as your sales-force, and have them talk vulnerable, elderly people into enrolling in hospice care by convincing them they have nothing to live for and should just die already and not burden their loved ones any longer.
Hospitals and hospices also collude: hospitals can revive dying patients, ignoring their Do Not Resuscitate orders, so they can be transfered to a hospice and die there, saving the hospital from adding another dead patient to their stats.CMS’s solution is perverse: they’re working with Humana to expand Medicare Advantage (a scam that convinces patients to give up Medicare and enrol in a private insurance program, whose private-sector death panel rejects 13% of claims that Medicare would have paid for). The program will pay private companies $32,000 for every patient who agrees to cease care and die. As our friends on the right like to say, “incentives matter.”
Appelbaum and co have a better idea:
Do more enforcement: increase inspections and audits.
Block mergers and rollups of hospices that make them too big to fail and too big to jail.
Close existing loopholes.
They should know. Appelbaum and her co-authors write the best, most incisive analysis of private equity around. For more of their work, check out their proposal for ending pension-plan ripoffs by Wall Street firms:
https://pluralistic.net/2022/05/05/mego/#A09948

Catch me on tour with Red Team Blues in Burbank, Mountain View, Berkeley, San Francisco, Portland, Vancouver, Calgary, Toronto, DC, Gaithersburg, Oxford, Hay, Manchester, Nottingham, London, and Berlin!

[Image ID: An industrial meat grinder, fed by a conveyor belt. A dead, elderly man is traveling up the conveyor, headed for the grinder's intake. The grinder is labelled 'HOSPICE' in drippy Hallowe'en lettering. It sits in a spreading pool of blood.]

Image:
Seydelmann (modified)
https://commons.wikimedia.org/wiki/File:GW300_1.jpghttps://commons.wikimedia.org/wiki/File:GW300_1.jpg
CC BY-SA 3.0
https://creativecommons.org/licenses/by-sa/3.0/deed.en
#pluralistic#cepr#medicare advantage#medicare#hospice#aca#aging#death panels#fraud#california#preying on the dying
141 notes
·
View notes
Text
Medicare Advantage is a money grab by big insurers - Minnesota Reformer
13 notes
·
View notes
Text
A national physician group this week called for the complete termination of a Medicare privatization scheme that the Biden White House inherited from the Trump administration and later rebranded—while keeping intact its most dangerous components.
Now known as the Accountable Care Organization Realizing Equity, Access, and Community Health (ACO REACH) Model, the experiment inserts a for-profit entity between traditional Medicare beneficiaries and healthcare providers. The federal government pays the ACO REACH middlemen to cover patients' care while allowing them to pocket a significant chunk of the fee as profit.
The rebranded pilot program, which was launched without congressional approval and is set to run through at least 2026, officially began this month, and progressive healthcare advocates fear the experiment could be allowed to engulf traditional Medicare.
In a Tuesday letter to Health and Human Services Secretary Xavier Becerra and Centers for Medicare and Medicaid Services Administrator Chiquita Brooks-LaSure, Physicians for a National Health Program (PNHP) argued that ACO REACH "presents a threat to the integrity of traditional Medicare, and an opportunity for corporations to take money from taxpayers while denying care to beneficiaries."
The group, which advocates for a single-payer healthcare system, voiced alarm over the Biden administration's decision to let companies with records of fraud and other abuses take part in the ACO REACH pilot, which automatically assigns traditional Medicare patients to private entities without their consent.
CMS said in a press release Tuesday that "the ACO REACH Model has 132 ACOs with 131,772 healthcare providers and organizations providing care to an estimated 2.1 million beneficiaries" for 2023.
"As we have stated, PNHP believes that the REACH program threatens the integrity of traditional Medicare and should be permanently ended," Dr. Philip Verhoef, the physician group's president, wrote in the new letter. "Whether or not one agrees with this statement, we should all be able to agree that companies found to have violated the rules have no place managing the care of our Medicare beneficiaries."
Among the concerning examples PNHP cited was Clover Health, which has operated so-called Direct Contracting Entities (DCEs)—the name of private middlemen under the Trump-era version of the Medicare pilot—in more than a dozen states, including Arizona, Florida, Georgia, and New York.
PNHP noted that in 2016, CMS fined Clover—a large Medicare Advantage provider—for "using 'marketing and advertising materials that contained inaccurate statements' about coverage for out-of-network providers, after a high volume of complaints from patients who were denied coverage by its MA plan. Clover had failed to correct the materials after repeated requests by CMS."
Humana, another large insurer with its teeth in the Medicare privatization pilot, "improperly collected almost $200 million from Medicare by overstating the sickness of patients," PNHP observed, citing a recent federal audit.
"It appears that in its selection process [for ACO REACH], CMS did not prevent the inclusion of companies with histories of such behavior," Verhoef wrote. "Given these findings, we are concerned that CMS is inappropriately allowing these DCEs to continue unimpeded into ACO REACH in 2023."

While the Medicare pilot garnered little attention from lawmakers when the Trump administration first launched it during its final months in power, progressive members of Congress have recently ramped up scrutiny of the program.
Last month, Sen. Elizabeth Warren (D-Mass.) and Rep. Pramila Jayapal (D-Wash.) led a group of lawmakers in warning that ACO REACH "provides an opportunity for healthcare insurers with a history of defrauding and abusing Medicare and ripping off taxpayers to further encroach on the Medicare system."
"We have long been concerned about ensuring this model does not give corporate profiteers yet another opportunity to take a chunk out of traditional Medicare," the lawmakers wrote, echoing PNHP's concerns. "The continued participation of corporate actors with a history of fraud and abuse threatens the integrity of the program."
#us politics#news#2023#common dreams#medicare#trump administration#biden administration#Accountable Care Organization Realizing Equity Access and Community Health model#department of health and human services#Xavier Becerra#Chiquita Brooks-LaSure#Physicians for a National Health Program#Centers for Medicare and Medicaid Services#Dr. Philip Verhoef#Direct Contracting Entities#Medicare Advantage#sen. elizabeth warren#Rep. Pramila Jayapal#medicare for all#us healthcare#us health insurance
95 notes
·
View notes
Text
New rules for selling Medicare so-called "Advantage"
Federal regulations go into effect September 30 prohibiting those sneaky misleading Part C ads made by the for-profit health insurance middlemen.
Excerpt:
Starting Sept. 30, if Joe Namath, William Shatner or Jimmy Walker wants to sell you on Medicare Advantage (MA), they are going to have to disclose what insurance plan they are advertising. And these television pitches can’t misuse the Medicare logo or card to lead consumers to believe the celebrity endorsers represent the federal government.
It’s all part of a regulation the Centers for Medicare & Medicaid Services (CMS) finalized in April that is designed to crack down on what Health and Human Services Secretary Xavier Becerra has called “misleading marketing schemes by health insurance companies that offer Medicare Advantage plans.”
__________
Hmm. It's a start.
7 notes
·
View notes
Link
"Unlike ads for prescription drugs, insurance companies are not required by law to mention the side effects on patients, but Americans deserve to know about the many disadvantages of Medicare Advantage..." (for seniors AND tax payers).
Read and heed. Tell the people you love.
5 notes
·
View notes
Text
My OTC Medicare Advantage Benefit Saga:
I'm writing thins in case any of you have Medicare. (Do you have medicare advantage? if not! Get some when it reopens next fall, because medicare part C is amazeballs).
They switched up providers and the entire system of Over the counter Meds benefits at the new year. They increased the benefit and made it monthly instead of quarterly and added a $50.00 food voucher. They were late sending cards out to let people actually use the benefit and out right lied to social services, medicare advantage social workers etc., that they mailed the catalog/directions/etc. packet in December when as of 1/10/22 they hadn't mailed them at all. This is a serious asshole maneuver as if you do not spend your benefit by month's end it doesn't roll over. My card only got here end of last week and as of last Tuesday very few had them yet. I suspect preventing most people using their benefit this month is an illicit cost saving measure.
Anyway, the old system, you had a catalog full of OTC stuff you could order four times a year. You couldn't go over the limit, and any change left after the order was lost. It was all at cost so big bang for your buck, but they lacked all kinds of things one would think should be in there like surgical masks or better, but they had no masks at all at the start of the pandemic, and a year in they only added the crappy white cloth ones that never fit properly. You'd think masks would have been standard for elderly and disabled people even before the pandemic, but... Yeah. Still it was way better than not having it. You could get things like antacid and first aid supplies and toothbrushes, but it was missing stuff that logic dictates made sense.
The new system is a give away to pharmacies. You get more to spend, but it's at price gougey pharmacy prices instead of at cost. You can only use certain chain pharmacies and grocery stores. The two cheapest grocery stores in my small city/town are not on the list. The second and third most expensive are.
So my social worker and the person in charge of several things including OTC benefit in my state were on a conference call with me Tuesday as we tried to work out WTF. Why me? I'm a squeaky wheel who kept asking how I was meant to use the benefit and so is my nurse/social worker. The lady from OTC was super nice and helpful, it's just the office in Washington and third party administrator were not communicating about stuff at all in a useful way. So they asked if I'd guinea pig for them using only information that came with the card which was sketchy at best. I agreed to go to the Rite AID, ask them if they had any info sheets sent to them, and try to buy an experimental month's worth of OTC. (I'm doing the grocery run next week, I think. I was exhausted from errands and treatment.)
NOTE: If you get your card make sure to activate it and definitely save the mailer it's attached to as it lists participating chain stores and the monthly benefit amounts. Do remember to account for state tax if any and have extra money with you in case you go over.
No one at Rite AID on that shift knew what an OTC benefit was and they took my benefit card for something else when I went to pay. They had definitely not been informed this roll out was happening nor had they been sent a what people could buy with it list any more than we had.
My purchase set was deliberately experimental. I mostly selected things I knew were on the old list, but tried brands they didn't carry for a bunch of things. Oral B toothbrush heads instead of Phillips. I got tums, but also the store brand equivalent, that kind of thing. I also grabbed a big box of the previously forbidden masks. They fit under the vague guidelines on the card mailer, but I knew they were off list last year.
I explained to the cashier about not knowing what was covered and that we may have to put things back. Everything went through. Even the masks. I was so caught up in the experiment, I forgot to factor in state tax, so I went a little over, which is fine, as that too is useful data. If the only thing over is tax, you can't remove items from the tally, which is good to know. I have reported back, so the medicare advantage people for my state can use the results to help all the others.
Next month I will branch out a little more and see if I can push it a little further from the old catalog of we don't get our items list in time.
All in all, as annoying as it is that pharmacies are profiting off this instead of people getting full value, being able to buy the toothbrush head brand I need and to purchase things off book like masks is a huge help. I just wish some things weren't jacked up 3-4 times the price from the old catalog. With the benefit increase it balances out though. Not having to spend thirty bucks on masks is worth it by itself. It also means not spending an hour or two planning my purchase so as to lose as little as possible.
The old catalog let us buy soap, but not shampoo. I am wondering if soap is still allowed under the new guidelines. I supose it's a question for next month.
2 notes
·
View notes
Text

Things you need to know about Medicare
Medicare offers free access to crucial screenings and preventative care, which aids people to stay healthy. A complimentary annual wellness exam is provided under Medicare Part B, along with yearly and recurrent tests for cardiovascular disease, diabetes, depression, cervical, and prostate cancer, in men and breast cancer in women. Also included are flu vaccines. Additionally, the Part D program might assist in defraying the expense of expensive prescription medications.
Read more: https://www.evernote.com/shard/s482/sh/2bbe12b3-7734-7f83-bfb8-b9a9b1c8ce30/6114fb1cb9f701c2b37eace823b1751c
2 notes
·
View notes
Text
Both Medicare Advantage and Medigap plans are, in layman’s terms, an extension of the Original Medicare offered by private insurers, but they differ significantly.
1 note
·
View note
Text
How And When To Apply For Medicare?

Applying for Medicare is a crucial step for individuals nearing the age of 65 or those qualifying due to disability or specific medical conditions. Understanding how and when to apply for Medicare ensures seamless access to essential healthcare benefits. Below, we'll explore the process of applying for Medicare, including important timelines and considerations.
When to Apply for Medicare:
Initial Enrollment Period (IEP): The Initial Enrollment Period for Medicare begins three months before an individual's 65th birthday and lasts for seven months. It includes the month of their birthday, the three months before, and the three months after. Applying for Medicare during this period is crucial to ensure coverage starts promptly, without incurring any late enrollment penalties.
Special Enrollment Period (SEP): Some individuals may qualify for a Special Enrollment Period, allowing them to enroll in Medicare outside of the Initial Enrollment Period without facing penalties. Qualifying events for SEP include having coverage through an employer or union, losing other health coverage, or moving outside of your plan's service area. It's essential to apply for Medicare during the SEP if eligible to avoid gaps in coverage and potential penalties.
General Enrollment Period (GEP): If someone misses their Initial Enrollment Period and doesn't qualify for a Special Enrollment Period, they can enroll during the General Enrollment Period, which runs from January 1 to March 31 each year. However, late enrollment penalties may apply. Applying for Medicare during the GEP provides another opportunity to secure healthcare coverage, albeit with potential financial consequences for delayed enrollment.
How to Apply for Medicare:
Online Application: One of the most convenient ways to apply for Medicare is through the Social Security Administration (SSA) website. The online application process is straightforward and allows individuals to apply for Medicare Part A and/or Part B from the comfort of their homes. Applicants can visit the SSA website and follow the instructions to complete the application form securely.
In-Person Application: Individuals who prefer in-person assistance or have specific questions about the Medicare application process can visit their local Social Security office. Trained staff at SSA offices can provide personalized assistance, answer questions, and guide applicants through the Medicare enrollment process. It's advisable to schedule an appointment to ensure efficient service and minimize wait times.
Phone Application: Alternatively, individuals can apply for Medicare by calling the Social Security Administration's toll-free number. By contacting SSA over the phone, applicants can speak with a representative who will assist them in completing the Medicare application. Phone applications are suitable for individuals who prefer verbal assistance or have limited access to online resources.
Important Considerations:
Gather Necessary Information: Before applying for Medicare, it's essential to gather all necessary information and documentation. This may include personal identification documents, proof of age, proof of citizenship or legal residency, and details about current health insurance coverage. Having this information readily available streamlines the application process and ensures accurate enrollment.
Understand Coverage Options: When applying for Medicare, individuals should understand their coverage options and consider additional plans that may supplement their healthcare benefits. This includes Medicare Advantage (Part C), Medicare Prescription Drug Plans (Part D), and supplemental Medigap policies. Researching and comparing different coverage options can help individuals make informed decisions about their healthcare needs.
Be Aware of Enrollment Deadlines: Missing enrollment deadlines can result in delays in healthcare coverage and potential penalties. It's crucial to be aware of Medicare enrollment periods and submit applications in a timely manner to avoid gaps in coverage and financial consequences. Planning ahead and understanding enrollment deadlines ensures smooth transitions and uninterrupted access to healthcare benefits.
Applying for Medicare is a critical step for individuals approaching the age of 65 or those qualifying due to disability or specific medical conditions. By understanding medicare eligibility requirements individuals can ensure seamless access to essential healthcare benefits without facing penalties.
Whether applying online, in-person, or over the phone, it's essential to gather necessary information, understand coverage options, and be aware of enrollment deadlines. By taking proactive steps to enroll in Medicare, individuals can safeguard their health and well-being while navigating the complexities of the healthcare system.
0 notes
Text
MedPAC Report to Congress: A Wrap with Monday?
Yesterday I wrote a post on President Biden’s healthcare budget. Today, I thought a quick visit back to March and MedPAC’s Annual Report to Congress on payment and program adequacy would be a good “wrapper” – for now.
Every year, MedPAC (the Medicare Payment Advisory Commission) reports to the Congress in March on the Medicare fee-for-service (FFS) payment systems, the Medicare (MA) program, and…

View On WordPress
#Budgets#CMS#Congress#Economics#Industry Outlook#Management#Medicare#Medicare Advantage#MedPac#Money#Payment#Policy#Rates#Reimbursement#Repot to Congress 2024#Strategy#sustainability#Trends#Washington
0 notes
Text
By Jake Johnson
Common Dreams
Oct. 4, 2023
"Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare," says a new report from Physicians for a National Health Program.
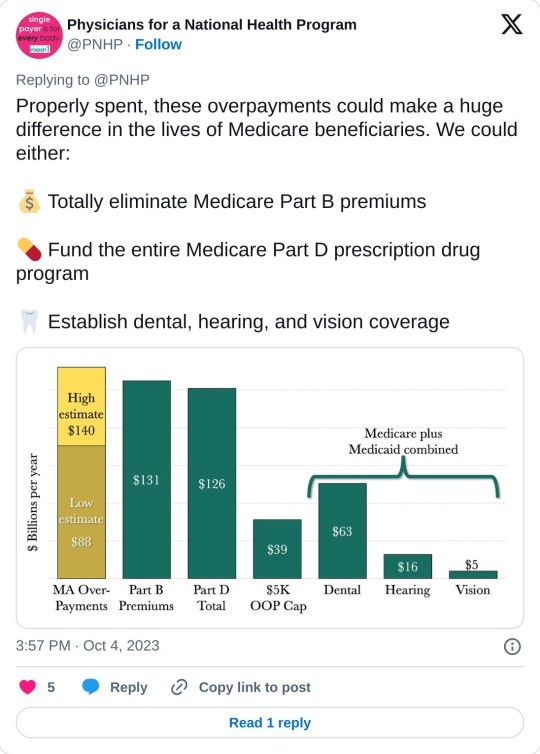
A report published Wednesday estimates that privately run, government-funded Medicare Advantage plans are overcharging U.S. taxpayers by up to $140 billion per year, a sum that could be used to completely eliminate Medicare Part B premiums or fully fund Medicare's prescription drug program.
Physicians for a National Health Program (PNHP), an advocacy group that supports transitioning to a single-payer health insurance system, found that Medicare Advantage (MA) overbills the federal government by at least $88 billion per year, based on 2022 spending.
That lower-end estimate accounts for common MA practices such as upcoding, whereby diagnoses are piled onto a patient's risk assessment to make them appear sicker than they actually are, resulting in a larger payment from the federal government.
But when accounting for induced utilization—"the idea that people with supplemental coverage are likely to use more health care because their insurance pays for more of their cost"—PNHP estimated that the annual overbilling total could be as high as $140 billion.
"This is unconscionable, unsustainable, and in our current healthcare system, unremarkable," says the new report. "Medicare Advantage is just another example of the endless greed of the insurance industry poisoning American healthcare, siphoning money from vulnerable patients while delaying and denying necessary and often lifesaving treatment."
Even if the more conservative figure is accurate, PNHP noted, the excess funding that MA plans are receiving each year would be more than enough to expand traditional Medicare to cover dental, hearing, and vision. Traditional Medicare does not currently cover those benefits, which often leads patients to seek out supplemental coverage—or switch to an MA plan.
The Congressional Budget Office has estimated that adding dental, vision, and hearing to Medicare and Medicaid would cost just under $84 billion in the most costly year of the expansion.
"While there is obvious reason to fix these issues in MA and to expand traditional Medicare for the sake of all beneficiaries," the new report states, "the deep structural problems with our healthcare system will only be fixed when we achieve improved Medicare for All."
Bolstered by taxpayer subsidies, Medicare Advantage has seen explosive growth since its creation in 2003 even as it has come under fire for fraud, denying necessary care, and other abuses. Today, nearly 32 million people are enrolled in MA plans—more than half of all eligible Medicare beneficiaries.
Earlier this year, the Biden administration took steps to crack down on MA overbilling, prompting howls of protest and a furious lobbying campaign by the industry's major players, including UnitedHealth Group and Humana. Relenting to industry pressure, the Biden administration ultimately agreed to phase in its rule changes over a three-year period.
Leading MA providers have also faced backlash from lawmakers for handing their top executives massive pay packages while cutting corners on patient care and fighting reforms aimed at rooting out overbilling.
As PNHP's new report explains, MA plans are paid by the federal government as if "their enrollees have the same health needs and require the same levels of spending as their traditional Medicare counterparts," even though people who enroll in MA plans tend to be healthier—and thus have less expensive medical needs.
"There are several factors that potentially contribute to this phenomenon," PNHP's report notes. "Patients who are sicker and thus have more complicated care needs may be turned off by limited networks, the use of prior authorizations, and other care denial strategies in MA plans. By contrast, healthier patients may feel less concerned about restrictions on care and more attracted to common features of MA plans like $0 premiums and additional benefits (e.g. dental and vision coverage, gym memberships, etc.). Insurers can also use strategies such as targeted advertising to reach the patients most favorable to their profit margins."
A KFF investigation published last month found that television ads for Medicare Advantage "comprised more than 85% of all airings for the open enrollment period for 2023."
"TV ads for Medicare Advantage often showed images of a government-issued Medicare card or urged viewers to call a 'Medicare' hotline other than the official 1-800-Medicare hotline," KFF noted, a practice that has previously drawn scrutiny from the U.S. Senate and federal regulators.
PNHP's report comes days after Cigna, a major MA provider, agreed to pay $172 million to settle allegations that it submitted false patient diagnosis data to the federal government in an attempt to receive a larger payment.
Dr. Ed Weisbart, PNHP's national board secretary, toldThe Lever on Wednesday that such overpayments are "going directly into the profit lines of the Medicare Advantage companies without any additional health value."
"If seniors understood that the $165 coming out of their monthly Social Security checks was going essentially dollar for dollar into profiteering of Medicare Advantage, they would and should be angry about that," said Weisbart. "We think that we pay premiums to fund Medicare. The only reason we have to do that is because we're letting Medicare Advantage take that money from us."
13 notes
·
View notes
Text
4 Things Medicare Covers That May Surprise You

0 notes
Text
Part D plans to ramp up restrictions on medications. The biggest change has been the growing number of drugs that are completely excluded from insurers’ lists of covered medications.
0 notes
Text
AN OPEN LETTER to THE U.S. HOUSE OF REPRESENTATIVES
Co-sponsor H.R. 732, the Save Medicare Act.
802 so far! Help us get to 1,000 signers!
As a constituent, I'm emailing to ask you to co-sponsor H.R. 732, the Save Medicare Act.
Medicare Advantage plans use deceptive marketing to oversell and overcharge for their private health care plans, and then under deliver on care. These private insurers are using government funding to increase their own profits, at the expense of their patients. And they take so much from the Medicare trust fund, that it’s threatening the solvency and future of traditional Medicare.
Congress must act to rein in Medicare Advantage, and should start by giving it a more accurate name. It is not Medicare and should not be advertised as such. The Save Medicare Act would force these plans to stop using “Medicare” in their name and would establish penalties for private insurers who don’t comply. Seniors and people with disabilities deserve to have this level of transparency when choosing their health care.
Please protect traditional Medicare by cosponsoring this bill.
▶ Created on April 4 by Jess Craven · 801 signers in the past 7 days
📱 Text SIGN PWAYKR to 50409
🤯 Liked it? Text FOLLOW JESSCRAVEN101 to 50409
#AN OPEN LETTER to THE U.S. HOUSE OF REPRESENTATIVES#Co-sponsor H.R. 732#the Save Medicare Act.#802 so far! Help us get to 1000 signers!#co-sponsor#H.R. 732#Medicare Advantage#deceptive#marketing#oversell#overcharge#private health care plans#under deliver#care#private insurers#government funding#increase#profits#expense#patients#Medicare trust fund#solvency#future#Medicare#Congress#must act#rein in Medicare Advantage#bill#The Save Medicare Act#noncompliance
0 notes