#Open windows to ventilate indoor space with outdoor air to prevent virus transmission
Text
From the report by Beth Mole, posted 29 Feb 2024:
In a lengthy background document, the agency laid out its rationale for consolidating COVID-19 guidance into general guidance for respiratory viruses—including influenza, RSV, adenoviruses, rhinoviruses, enteroviruses, and others, though specifically not measles. The agency also noted the guidance does not apply to health care settings and outbreak scenarios.
"COVID-19 remains an important public health threat, but it is no longer the emergency that it once was, and its health impacts increasingly resemble those of other respiratory viral illnesses, including influenza and RSV," the agency wrote.
The most notable change in the new guidance is the previously reported decision to no longer recommend a minimum five-day isolation period for those infected with the pandemic coronavirus, SARS-CoV-2. Instead, the new isolation guidance is based on symptoms, which matches long-standing isolation guidance for other respiratory viruses, including influenza.
"The updated Respiratory Virus Guidance recommends people with respiratory virus symptoms that are not better explained by another cause stay home and away from others until at least 24 hours after both resolution of fever AND overall symptom are getting better," the document states. "This recommendation addresses the period of greatest infectiousness and highest viral load for most people, which is typically in the first few days of illness and when symptoms, including fever, are worst."
The CDC acknowledged that the eased isolation guidance will create "residual risk of SARS-CoV-2 transmission," and that most people are no longer infectious only after 8 to 10 days. As such, the agency urged people to follow additional interventions—including masking, testing, distancing, hygiene, and improving air quality—for five additional days after their isolation period.
"Today’s announcement reflects the progress we have made in protecting against severe illness from COVID-19," CDC Director Dr. Mandy Cohen said in a statement. "However, we still must use the commonsense solutions we know work to protect ourselves and others from serious illness from respiratory viruses—this includes vaccination, treatment, and staying home when we get sick."
Overall, the agency argued that a shorter isolation period would be inconsequential. Other countries and states that have similarly abandoned fixed isolation times did not see jumps in COVID-19 emergency department visits or hospitalizations, the CDC pointed out. And most people who have COVID-19 don't know they have it anyway, making COVID-19-specific guidance moot, the agency argued.
In a recent CDC survey, less than half of people said they would test for SARS-CoV-2 if they had a cough or cold symptoms, and less than 10 percent said they would go to a pharmacy or health care provider to get tested. Meanwhile, "The overall sensitivity of COVID-19 antigen tests is relatively low and even lower in individuals with only mild symptoms," the agency said.
The CDC also raised practical concerns for isolation, including a lack of paid sick leave for many, social isolation, and "societal costs."
The points are likely to land poorly with critics.
“The CDC is again prioritizing short-term business interests over our health by caving to employer pressure on COVID guidelines. This is a pattern we’ve seen throughout the pandemic,” Lara Jirmanus, Clinical Instructor of Medicine at Harvard Medical School, said in a press release last month after the news first broke of the CDC's planned isolation update. Jirmanus is a member of the People's CDC, a group that advocates for more aggressive COVID-19 policies, which put out the press release.
Another member of the group, Sam Friedman, a professor of population health at NYU Grossman School of Medicine, also blasted the CDC's stance last month. The guidance will "make workplaces and public spaces even more unsafe for everyone, particularly for people who are high-risk for COVID complications," he said.
But, the CDC argues that the threat of COVID-19 is fading. Hospitalizations, deaths, prevalence of long COVID, and COVID-19 complications in children (MIS-C) are all down.
COVID-19 vaccines are safe and effective at preventing severe disease, death, and to some extent, long COVID—we just need more people to get them.
Over 95% of adults hospitalized with COVID-19 in the 2023–2024 respiratory season had no record of receiving the seasonal booster dose, the agency noted.
Only 22% of adults got the latest shot, including only 42% of people ages 65 and older. In contrast, 48% of adults got the latest flu shot, including 73% of people ages 65 and older. But even with the crummy vaccination rates for COVID-19, a mix of past infection and shots have led to a substantial protection in the overall population.
The CDC even went as far as arguing that COVID-19 deaths have fallen to a level that is similar to what's seen with flu. "Reported deaths involving COVID-19 are several-fold greater than those reported to involve influenza and RSV. However, influenza and likely RSV are often underreported as causes of death," the CDC said.
In the 2022–2023 respiratory virus season, there were nearly 90,000 reported COVID-19 deaths.
For flu, there were 9,559 reported deaths, but the CDC estimates the true number to be between 18,000 and 97,000.
In the current season, there have been 32,949 reported COVID-19 deaths to date and 5,854 reported flu deaths, but the agency estimates the real flu deaths are between 17,000 and 50,000.
"Total COVID-19 deaths, accounting for underreporting, are likely to be higher than, but of the same order of magnitude as, total influenza deaths," the agency concluded.
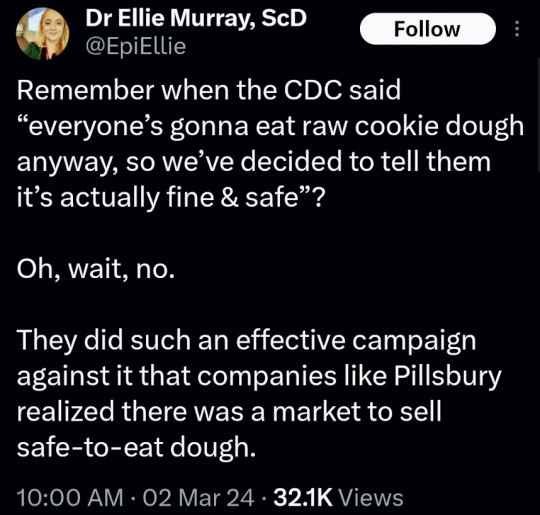
(say no to raw dough: CDC)
#please stay safe#the vaccines are safe#yes the covid shot is safe#covid is not a hoax#covid causes permanent long term damage to your body even if you're healthy#news#scicomm#science#ars technica#covid--19#coronavirus#beth mole#pandemic#the cdc#centers for disease control#5 day covid isolation#yes you should stay home for at least 5 days if you test positive for covid#Open windows to ventilate indoor space with outdoor air to prevent virus transmission#Wear a mask that doesn't touch your lips#keep distance from others
5 notes
·
View notes
Text
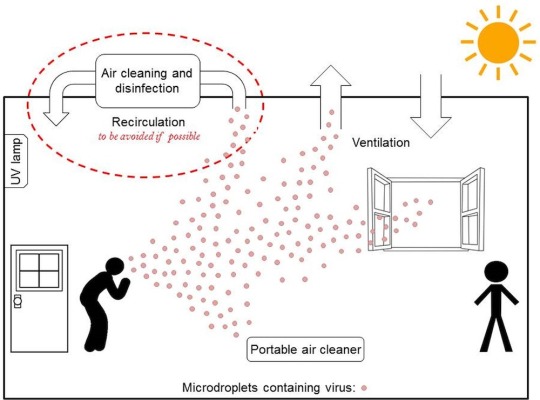
How to to Clean Our Indoor Air Properly Against COVID-19 | Time
*Outdoors is better than indoors
*Indoors requires either greater ventilation or scrubbing of the air (filtration)
*Most buildings have poor ventilation, and cold or hot weather mat require less ventilation
*In those cases, you need to scrub (filter) the air alongside ventilation
*Air duct filtration/UV may have limited value
*Much better to filter "in the room where it happens" using portable filters and Upper-room germicidal UV (GUV) fixtures (not personal UV scrubbers)
*Upper room germicidal is most cost effective for schools and businesses
*Ionization ineffective and causes irritants
TLDR: Mechanical ventilation, upper room UV, and portable room air cleaners
"Outdoors, dilution of any aerosols is infinite—though the time it takes to dilute clouds of aerosol, depends on air movement. Think, for example, of how a cloud of cigarette smoke outdoors lingers or dissipates depending on whether there’s a breeze or not.
Indoors, however, aerosols almost always linger longer than outdoors—often long enough to be inhaled by someone sharing the same space. Put another way, if you breath in an indoor setting where other people are also breathing, you will almost surely breath in some amount of air that has been recently exhaled by someone else. That recycled air—the so-called rebreathed air fraction—estimated by room carbon dioxide measurements, is a good predictor of the risk of infection, given an infectious person generating infectious aerosol in the same room....
Think About Ventilation
Ventilation, natural or mechanical, is the main way that the risk of airborne infection indoors is reduced. For hospital airborne infection isolation and procedure rooms, the U.S. Centers for Disease Control and Prevention (CDC) recommends 6 to 12 room air changes per hour (ACH) with infection-free outdoor air, or air that has been filtered or otherwise decontaminated. One ACH occurs when a volume of air equal to that of the room enters and leaves over a period of one hour. As fresh air enters and mixes with contaminated room air, not all the contaminated air is removed by one air change. Under well-mixed conditions, one air change removes approximately 63% of room air contaminants, and a second air change removes about 63% of what remains, and so on.
But under real world conditions, the protection achieved by ventilation also depends on the amount of contaminant (virus in this case) being added over time, i.e. by an infected person, and on the contagiousness of the infection. The greater the infectiousness of the virus, greater the infection-free ventilation needed to keep concentrations low.
For Omicron, for example, 6-12 ACH ventilation, or equivalent air disinfection, may not be enough to prevent transmission. Unfortunately, not all transmission is preventable by air disinfection—for example, transmission at very close range where there is no time to remove or inactivate viruses generated by one person before they are inhaled by someone else.....
Many residential and older buildings without mechanical ventilation may have about one ACH or less due to air leakage around doors and windows—but when windows are open, depending on building design, orientation, and outside weather conditions, may enjoy significantly higher ACHs. For economical heating and cooling, however, windows are normally closed, especially in larger mechanically ventilated buildings, by design, or closed by occupants in response to outside temperatures. Automated mechanical ventilation systems often bring in a minimum amount of outside air under very cold or hot outside conditions, resulting in most air being recirculated within the building, thereby recirculating air contaminants rather than removing them...
....because mechanical ventilation may not be sufficient to reduce the risk of infection, mechanical ventilation in public buildings should be supplemented by other methods of air disinfection. For current and future viral pathogens like SARS-CoV-19, relatively high levels of “equivalent” ventilation by supplemental air disinfection will be needed.....
....the value of high-efficiency filters or germicidal UV in recirculating ventilation ducts for preventing spread is speculative and limited at best....
A more effective air disinfection strategy is to rapidly decontaminate the air within the room where person-to-person transmission occurs.
“In the room where it happened” is a song from the Hamilton musical, but it could also be a guide to the application of air-disinfection technology....
....a small UV air disinfecting device designed to be worn around the neck cannot possibly move enough air to reduce aerosol transmission. Or, another example, small boxes with UV sources designed to decontaminate cell phones are likely no better than an occasional wipe down with alcohol. Equally irrational are GUV wands because delivering an effective germicidal dose is unpredictable when waving a wand over a surface, and they must be low power to avoid accidental direct over-exposure of eyes or skin. At an even larger scale, GUV portals have been marketed and used in building entrances or exits to “disinfect” people walking through them. This makes no sense not only because no significant decontamination of skin or clothing is possible, but respiratory virus resides in the human respiratory tract, and cannot be eliminated from the outside."
7 notes
·
View notes
Text
5 steps you need to take to protect yourself and prevent the spread of COVID-19

Since March 2020, following the safety protocols of COVID-19 has been part of our daily life. Because this virus is highly contagious and spreads through person-to-person contact, according to the Center for Disease Control and Prevention, the COVID-19 can spread through airborne transmission and mostly occur within enclosed spaces with inadequate ventilation.
Want to be safe from COVID-19: here are tips to protect yourself and others.
So amid the surge of the second wave of the COVID-19 in India, it has become very important to know how to be safe from COVID. Essentially, you can take so many measures to protect yourself from this disease and help break the chain. Most of these measures consist of maintaining social distance and being more cautious about hygiene. Here are some of the simple steps you can take to help prevent the spread of COVID-19 and protect yourself and your family.
5 steps you need to take to protect yourself and prevent the spread of COVID-19:
1. Practice Social Distancing: The best way to protect yourself from COVID is to avoid being exposed to this virus, so social distancing is a must for this. As per the CDC, maintain at least 6 feet (2 meters) of the distance between yourself and people outside your household. Moreover, avoid going to crowded places such as markets, bars, restaurants, gyms, fitness centers, etc. Because at these places, you are at higher risk of being exposed to this virus. And don't be at indoor spaces that do not offer fresh air from the outdoors as much as possible when you are at home; make sure there is enough air or ventilation by opening windows and doors.

2. Wash your hands and keep them clean: Washing hands often with soap and alcohol-based sanitizers kill the virus on your hand. We touch so many objects every hour and catch so many viruses and bacteria; so to rub them off, wash your hands frequently and keep practicing hand hygiene. Additionally, at your place, clean high-touch surfaces daily such as tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets, and sinks.
Due to the higher importance of washing hands and social distancing to prevent the spread of covid-19, then be careful of these measures:
Without washing hands, don't eat food, fruits, and drink.
When you are in a public place, make sure that you touch minimal objects and sanitize your hand more frequently.
Don't touch your eyes, nose, and mouth unnecessarily and with unwashed hands.
Further, it is vital to wash hands or sanitize, before or after these daily activities:
Before and after eating food
Before preparing food
Before touching your face
After using the restroom
After removing your mask
After touching animals or pets

3. Wear a mask or face mask: Wearing a mask has become the most basic requirement for protection against COVID- 19. Masks essentially act as barriers and filters to capture the droplets and particles we expel. When it is not possible to maintain social distancing, you can wear a mask to protect yourself. By wearing a mask that covers your mouth and nose, you will reduce the risk of serving as the source of disease spread by trapping your droplets in the mask and reducing the risk of getting sick via droplets containing the coronavirus by blocking access to your airways.

4. Get tested if you have any symptoms: The symptoms of COVID-19 are similar to that of other respiratory diseases such as influenza, flu. If you have any of these symptoms like cold, fever, headache, cough, loss of taste and smell, sore throat, etc., make sure you get tested for COVID-19. Further, isolate yourself and check the coronavirus symptoms day by day.
Here are some of the COVID-19 tips for staying home:
Isolate yourself and maintain distance from others as much as possible.
When you cough and sneeze, use a tissue, or cover your mouth with the elbow or hands. After that, wash your hands.
Eat healthy food and use separate dishes, cups, glasses, spoons, etc.
Make sure there is enough ventilation in your room.

5. Get inoculated with COVID-19 Vaccine: Walk into your nearest COVID vaccination center and get inoculated. Millions of people are taking vaccines as they are highly effective to prevent COVID. At the beginning of the COVID in 2020, scientists had very little knowledge about this disease, but today we have a weapon to fight this battle against the coronavirus- which is the corona vaccine. Most of the countries all across the world are inoculating their people and with very positive results. However, don't forget that a COVID vaccine is only for preventing this disease and not necessarily a coronavirus cure. So after getting vaccinated, don't be complacent and lenient in following the safety protocols of COVID-19.

Conclusion:
Covid 19 can have serious, life-threatening complications, and amid the surge of the second wave, be mindful of all the guidelines of COVID-19. As you know that how does coronavirus spreads, so maintain social distancing, wash your hand, keep hygiene, wear a face covering or mask, and above, get vaccinated now. Further, if you develop any symptoms of the COVID-19, then immediately isolate yourself and follow CDC guidelines.
#How to fight the battle against the coronavirus#how to protect yourself from covid-19#5 ways to prevent covid-19#10 precautions of covid-19#covid-19#prevent the spread of covid-19#covid-19 protocol#social distancing guidelines#cdc guidelines for covid-19
2 notes
·
View notes
Text
My New Ventilated Social-Distancing Movie Theatre
(or, how I bought a 2020-proof social life for less than $100)
So the USA is (still) a hot mess in terms of pandemic response. Because both my father and I are at increased risk for complications from COVID-19, and my sister and I have to work together in person to run our workshops, my entire family has been in a state of self-quarantine for six months straight (with no end in sight). But it’s hard being in constant isolation, so the four households that comprise my local family have been doing weekly outdoor gatherings -- with plenty of hand sanitizer and safely-spaced tables -- so we can see each other and socialize at a distance. However, that’s only feasible when the weather cooperates.
I’ve also really missed watching movies with friends, which prior to the pandemic had been a regular activity. I have a 70-year-old tripod screen I inherited from my grandfather and a projector I use for running panels at conventions, so we’ve watched occasional DVDs outdoors, but we could only do that on evenings without wind (which could tear the brittle screen) or rain (which would damage the projector), and we have to be careful not to have the sound too loud because it might disturb the neighbors.
A couple weeks ago, when our city delayed reopening again due to rising COVID-19 case numbers, I decided to convert half of my garage into an outdoor movie theatre. It turned out pretty well, and it only cost about what I would spend on movie tickets in an average year (and since I’m not going to any movies in 2020, it’s pretty much a wash). I’m sharing the details in case it gives anyone else ideas for making a health-conscious social hangout!
Obviously YMMV, and in areas with higher case numbers (hi, FL & AZ), this still might be too much contact. Be safe and follow official recommendations to prevent viral spread, folks!

The Space
Before I settled on the garage, I considered building a movie space under a tent canopy (nixed because they’re almost impossible to anchor through Midwest storm winds) or carport kit (too expensive and high-maintenance for me), so there are definitely other options depending on where you live, your typical weather, and what space you have available!
My garage has an unusual layout that allows for better-than-average ventilation. When it was first built, it was a 2 1/2-car garage with the doors facing the street and windows on the side. About 40 years later, the owners decided to move the driveway to the other side of the house, so they built a second garage attached to the drive-door side and knocked out an end wall to put in a new overhead door. This means that by square footage, the garage could hold four cars, but the way the drive doors are situated, it’s a divided two-car garage with a bunch of extra space at the far end. The two sides are connected by one of the original overhead doors, which means that three of the four walls have openings that allow for air movement. (More on that below.)
Normally there’s a car in each side of the garage, but I decided I was willing to park outside all summer for the sake of having a social life. Over the course of a week, I emptied and thoroughly cleaned the half of the garage that has the windows.

Air Flow
Constant fresh air flow is critical to flushing aerosolized particles that can spread the virus, so in order to make a safe indoor space, I had to simulate outdoor air movement. I opened all three overhead doors and both windows, then placed several fans to draw air through the building: One in each window, one along the side wall, and a box fan in the connecting door between the two sides of the garage to pull more air in from the outside. To make sure air was actually moving through the building and not just circulating within it, I turned on all the fans while I was sweeping the (very dusty) floor and walls, and adjusted the fan angles until the dust blew straight out the overhead door, rather hanging in the air or gathering in the corners. (Experts recommend that to prevent virus transmission, indoor spaces should have 100% air turnover every 10 minutes; obviously I have no way of testing that in a garage, but there is a constant light breeze through the building and stuff seems to be blowing out, so I feel pretty good about it.)

Projection Setup
I already had the projector and DVD player (I took the one out of my living room, since I usually just watch DVDs on my game console anyway), but I wanted a larger wall-mounted screen, since my grandfather’s 1950s screen was designed for showing vacation slides in a living room, not wide-screen films. Hanging fabric screens are very cheap, but I opted for a 120″ retractable screen so it would stay clean in the dusty garage. I also have an old set of monitor speakers that provide nice stereo sound.

Seating
The beauty of setting up in a garage is that it’s basically outdoors, so you can use lawn furniture or bean bags or old chairs you pulled out of someone’s trash (I do this regularly; it’s how I got my entire patio set). Measuring out at least 6 feet between each table and staggering their positions so nobody was directly downwind of another table, I set up all the card tables and folding tables I owned, and put a pair of chairs by each one so that couples from the same household could share a table but not be in close contact with any other groups. I put my largest folding table (which was also salvaged from the trash -- seriously, it’s the best way to get stuff!) against the wall right by the open door to serve as a snack table, so it’s on the opposite wall from the seating and nobody would be breathing on the food. I covered all the tables with decorative heavy-duty vinyl tablecloths (mostly for sanitation purposes, because those tables have been sitting out in my garage and I know I’ve had raccoons and opossums out there -- not to mention the colony of bats that lives in the loft off the back of the garage).
This setup can seat up to eight people, and even provides a place for serving food. (I put pump bottles of hand sanitizer on each table and on the food table, and people wear face masks when they’re loading up their plates, so there’s minimal contamination risk there.)
Total Cost
My out-of-pocket cost for this whole project was only about $83, though that’s because I already had a lot of stuff lying around. Here’s a more complete breakdown:
Fans: I already owned the box fan ($25 new) and a couple other fans that I’d picked up super cheap at garage sales ($5 or so), because my house is old and the HVAC is not very efficient. The only new fan I bought for this project was a refurbished air circulator from Amazon ($14), because I needed a small but high-velocity fan to fit in a window.
Projection setup: The only new thing I bought was the screen, which was $65 including shipping (though non-retractable fabric screens start around $10-15, so if you’re on a budget you can get one very cheap). I bought the projector used on eBay about eight years ago. I think I paid around $40 for it then, but prices have come down since; I’ve seen discount projectors for as low as $20. The DVD player is a cheapo region free model, which I got a decade ago for maybe $30. The speakers were secondhand; I’ve also used an old set of external PC speakers ($10 from Goodwill) when running video off my laptop, and they worked well enough in the indoor space.
Seating: Almost all the outdoor furniture I own came from other people’s trash, so I didn’t pay anything for it! Any kind of seating or tables will work, though. I did invest about $4 for new tablecloths, which I got on seasonal clearance.
Bonus Perks
I’ve discovered that the garage walls block a LOT of light and sound unless you’re standing directly outside the drive doors, so we can watch movies for half the night or stay up late chatting and we aren’t disturbing the neighbors! We couldn’t run movies out on the patio late at night because the sound would carry to neighboring houses.
Also, when we’re watching a film in the evening, we get to watch my bats fly through the garage on their way to and from dinner! (Which might be an annoyance to the bats if we were out there all the time, but we try to keep our volume low and we’re only out there about once a week, so I don’t think we’re disturbing them too much.) Bats are protected in my state, as some of the native species are critically endangered, and we try to encourage nesting as they’re essential to pest insect control. I love watching them fly around!
The setup also works well for video games. A local friend and I had been playing online, late at night because it was the only time we could get enough bandwidth to maintain connection (the ISP in my area is not super reliable), but now we can sit on opposite sides of the garage and play local co-op with no lag:

So, in summary, my “movie theatre” is by no means a luxurious setup, but it was cheap :) and it’s a great way for my small pandemic social bubble to get together and chat, have a movie night, or play games without risking being in a closed room together.
13 notes
·
View notes
Text
Ventilating complaints about air standards
The world has finally accepted that the COVID-19 virus is spread on the air, and mainly indoors. So why haven’t ventilation standards been updated for buildings?
This article first appeared in Cosmos Weekly on 30 July 2021. For more stories like this, subscribe to Cosmos Weekly.
Australia is in the grips of another COVID-19 outbreak. This time, the highly transmissible Delta variant of SARS-CoV-2 has plunged many into lockdown and put the nation on high alert.
Epidemiologists say the Delta variant, which has spread to 104 countries and counting, may be about 90% more infectious than the original – Alpha – strain of SARS-CoV-2. But one thing remains the same: this virus is airborne. It spreads in the air we breathe. In lab studies, SARS-CoV-2 has been shown to linger in the air for up to 16 hours, carried aloft on microscopic particles called aerosols.
World-leading aerosol scientist Professor Lidia Morawska, of Queensland University of Technology (QUT), in Brisbane, says the latest outbreak has once again exposed the gaps in our hotel quarantine system and highlighted flaws in building design and ventilation systems – which should flush out contaminated air, without affecting other occupants, if designed correctly and operating well.
“Well over a year into the pandemic, there hasn’t seen any progress whatsoever [in Australia] to tackle this,” Morawska says. “No one mentions the word ventilation.”
The latest outbreak has once again exposed the gaps in our hotel quarantine system and highlighted flaws in building design and ventilation system.
Morawska is not alone in her frustration. Architects and building engineers are also calling for stronger recognition of respiratory viruses that spread via aerosols and improvements to ventilation in public spaces.
“We knew in July last year that SARS-CoV-2 was airborne,” says architect Geoff Hanmer, an adjunct professor of architecture at the University of Adelaide. “And yet it’s taken ISIAQ [the International Society of Indoor Air Quality and Climate] and the World Health Organization almost a year to admit that that’s the case.”
These experts’ exasperation is exacerbated because the engineering solutions to rid indoor spaces of airborne pathogens already exist – they just need to be installed or upgraded.
What needs to be done?
There are three key ingredients in the cocktail that is infection risk, Morawska explains. The first is the concentration of airborne particles that are emitted when an infected person talks, sings, coughs or sneezes. Second, a lack of ventilation, which lets aerosols linger in the air. And thirdly, some exposure time for people to inhale the virus-laden particles.
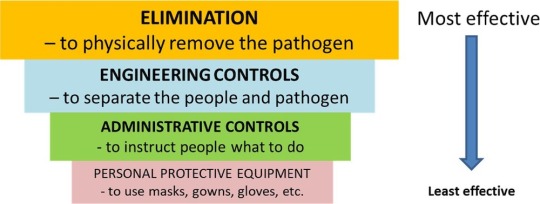
Traditional infection control pyramid adapted from the US Centers for Disease Control. Credit: Morawska et al/CDC/Environment International
Changing how buildings operate can address two out of those three factors. Improved ventilation increases airflow, diluting airborne particles; incorporating high-grade filtration systems can remove microscopic contaminants from the air.
However, the current standards for ventilating indoor public spaces (excluding hospitals) are not designed for infection control.
Public buildings from hospitals to schools and aged care facilities are “naturally” ventilated, meaning they rely on open windows to let fresh air in. They often have inadequate or poor ventilation, particularly in colder months.
“Very few countries have any regulations about indoor air quality. Infection transmission – which occurs mainly in indoor public spaces – is not specifically mentioned in any national regulations,” says Morawska.
“We must do something about the [building industry] standards.”
Hanmer says revising construction codes to improve ventilation standards to control for airborne infections would be a good start.
“But the problem is that new buildings are only a very small fraction of the total population of buildings,” he says.
Public buildings from hospitals to schools and aged care facilities are “naturally” ventilated, meaning they rely on open windows to let fresh air in. They often have inadequate or poor ventilation, particularly in colder months.
Many commercial buildings, such as shopping centres, hotels and universities, are also poorly ventilated, Hanmer says, because the performance of their mechanical ventilation systems – which pump in fresh air to replace stale indoor air – is too often substandard.
“It’s a bit of a lottery at the moment – certainly we need to get to a state where we’ve got better data and better regulation on air quality, generally,” says Hanmer, who recently surveyed the air quality in a number of public buildings.
“Clearly, the application of [national construction] codes in mechanically ventilated buildings hasn’t been as good as it should be.”
How can it be done?
Increasing ventilation rates to create greater airflow through rooms and buildings is one way to minimise infection risk indoors.
In 2009, WHO compiled 65 studies showing that poor ventilation is “associated with increased infection rates or outbreaks of airborne diseases”, concluding that “higher ventilation rates could decrease the risk of infection”.
But hard evidence linking improved ventilation with reduced infection rates directly is scarce. A 2019 study from the Taiwan Centres of Disease Control is a rare example. It found that increasing ventilation in stuffy university buildings controlled an outbreak of tuberculosis, an airborne bacterial disease. The outbreak, which lasted three years and involved 27 active cases and 1,665 contacts, was snuffed out after ventilation specialists reconfigured the building’s ventilation systems to improve airflow.

Portable air purifiers may help. Credit: Onurdongel/Getty
Fast forward to 2021, and both the WHO and US Centres for Disease Control and Prevention (CDC) now recommend that the total indoor air volume in healthcare facilities should be replaced with fresh outdoor air a minimum of 6 to 12 times per hour to prevent the spread of COVID-19.
Epidemiologist Mary-Louise McLaws, of UNSW Sydney, says this is the gold standard for ventilation for “hot zones” in hospitals – equivalent to 80 litres of air per second per person – and that these ventilation rates can be hard to achieve. In other settings, such as confined spaces and offices, airflow rates of 3 litres of air per second per person are needed, McLaws says.
While experts deliberate over exactly how much ventilation is needed to reduce infection rates, Morawska says there is no magic number because it depends on how the building is used.
This includes the number of people in each room (“The more sources, the higher the [required] ventilation rate,” she says) and their usual activities such as exercising, singing or talking loudly, all of which expel large amounts of viral particles.
Occupancy, though, can vary from one hour to the next, so ventilation systems need to be flexible. But ramping up ventilation is not just a matter of a simple flick of a switch; airflow direction and distribution are also important.
Engineering level controls to reduce the environmental risks for airborne transmission. Credit: Morawska et al/Environment International
Adding pathogen-proof filters to existing ventilation systems is not always possible either, if the airflow is too weak. Engineers also need to design ventilation systems with energy conservation in mind, Morawska says.
“It’s not just about increasing ventilation rates,” she says. We need smarter systems that remove the virus or any other contaminants but do not increase energy use.”
“We need to make sure that naturally ventilated buildings with high use have some fallback ventilation,” he says.
Demand-controlled systems could be used in schools to increase ventilation during predictably busy periods and dial airflow down when rooms are not in use. Another option is installing ventilation systems that detect rising levels of CO2 levels and kick in when air quality deteriorates, says Hanmer.
Ramping up ventilation is not just a matter of a simple flick of a switch; airflow direction and distribution are also important.
A fallback ventilated system comes into operation when the detected levels of CO2 in the air rise above about 800 parts per million, so it could reliably improve air quality, Hanmer says. Aged-care facilities would be the “absolute first priority” and schools a close second.
Building systems engineer Professor John Zhai, of the University of Colorado Boulder, suggests a simpler solution: portable air purifiers could be installed to filter air in crowded public spaces such as supermarket checkouts. These systems could be deployed quickly to reduce infection risk, provided they are the right size for the space.
Researchers are also designing smart systems that can detect mobile phone signals or use cameras (with image-processing algorithms) to determine when an indoor space gets too crowded and needs more ventilation, adjusting flow rates accordingly.
What would it cost?
Few economic analyses have been done to estimate the cost of improving ventilation because no one has been asking the question, says Morawska. However, available estimates suggest that necessary investments in building systems may be less than 1% of the construction cost of a typical building for new builds.
Hanmer estimates it would cost a few thousand dollars per room to install fallback ventilation systems in aged-care facilities. “I don’t think that’s an unreasonable burden given the seriousness of the disease,” he says. “And it’s whole lot less than a lockdown in a major capital city.”
But on top of the price tag for installations and upgrades, Zhai says that building engineers also have to consider the energy costs of running souped-up ventilation systems. Installing high-grade filters capable of trapping and removing microscopic airborne particles means greater fan power is needed to push the air through the filter – and that uses more energy, he says.
Around 40% of the total electricity used in buildings already goes into powering ventilation fans and it would take tremendous amounts of energy to increase airflow rates to recommended levels, Zhai says: “To double the flow rate, you basically need eight times the energy use.
The cost of improving ventilation system would be far less than the billions of dollars spent each year on influenza and other respiratory diseases.
“It can work for most emergency situations. You can supply a lot of air for a short period of time, to reduce infection risk. But for regular times, it’s not economically wise to do that.”
Morawska says, however, that the cost of improving ventilation system would be far less than the billions of dollars spent each year on influenza and other respiratory diseases. It could also help curb the costs of COVID-19, which currently has a global financial toll to the tune of $1 trillion each month.
But if countries continue to dismiss the airborne transmission of COVID-19 and other infectious diseases, as they have done for decades, then we will suffer the cost of this denial, Morawska says.
“Unless we start putting steps in place now to fix things on the longer term, once the pandemic passes – and it will eventually pass – no one will want to do anything about this,” she says.
“We’ll be left in exactly in the same situation when the next pandemic comes and still dealing with respiratory infections like the cold and flu.”
This article first appeared in Cosmos Weekly on 30 July 2021. To see more in-depth stories like this, subscribe today and get access to our weekly e-publication, plus access to all back issues of Cosmos Weekly.
Subscribe now
Ventilating complaints about air standards published first on https://triviaqaweb.weebly.com/
0 notes
Link
Scientists Urge Air Quality Changes in the Workplace, in Wake of Pandemic Clean water in 1842, food safety in 1906, a ban on lead-based paint in 1971. These sweeping public health reforms transformed not just our environment but expectations for what governments can do. Now it’s time to do the same for indoor air quality, according to a group of 39 scientists. In a manifesto of sorts published on Thursday in the journal Science, the researchers called for a “paradigm shift” in how citizens and government officials think about the quality of the air we breathe indoors. The timing of the scientists’ call to action coincides with the nation’s large-scale reopening as coronavirus cases steeply decline: Americans are anxiously facing a return to offices, schools, restaurants and theaters — exactly the type of crowded indoor spaces in which the coronavirus is thought to thrive. There is little doubt now that the coronavirus can linger in the air indoors, floating far beyond the recommended six feet of distance, the experts declared. The accumulating research puts the onus on policymakers and building engineers to provide clean air in public buildings and to minimize the risk of respiratory infections, they said. “We expect to have clean water from the taps., said Lidia Morawska, the group’s leader and an aerosol physicist at Queensland University of Technology in Australia. “We expect to have clean, safe food when we buy it in the supermarket. In the same way, we should expect clean air in our buildings and any shared spaces.” Meeting the group’s recommendations would require new workplace standards for air quality, but the scientists maintained that the remedies do not have to be onerous. Air quality in buildings can be improved with a few simple fixes, they said: adding filters to existing ventilation systems, using portable air cleaners and ultraviolet lights — or even just opening the windows where possible. Dr. Morawska led a group of 239 scientists who last year called on the World Health Organization to acknowledge that the coronavirus can spread in tiny droplets, or aerosols, that drift through the air. The W.H.O. had insisted that the virus spreads only in larger, heavier droplets and by touching contaminated surfaces, contradicting its own 2014 rule to assume all new viruses are airborne. The W.H.O. conceded on July 9 that transmission of the virus by aerosols could be responsible for “outbreaks of Covid-19 reported in some closed settings, such as restaurants, nightclubs, places of worship or places of work where people may be shouting, talking or singing,” but only at short range. The pressure to act on preventing airborne spread has recently been escalating. In February, more than a dozen experts petitioned the Biden administration to update workplace standards for high-risk settings like meatpacking plants and prisons, where Covid outbreaks have been rampant. Last month, a separate group of scientists detailed 10 lines of evidence that support the importance of airborne transmission indoors. On April 30, the W.H.O. inched forward and allowed that in poorly ventilated spaces, aerosols “may remain suspended in the air or travel farther than 1 meter (long-range).” The Centers for Disease Control and Prevention, which had also been slow to update its guidelines, recognized last week that the virus can be inhaled indoors, even when a person is more than six feet away from an infected individual. “They have ended up in a much better, more scientifically defensible place,” said Linsey Marr, an expert in airborne viruses at Virginia Tech, and a signatory to the letter. Updated May 13, 2021, 2:00 p.m. ET “It would be helpful if they were to undertake a public service messaging campaign to publicize this change more broadly,” especially in parts of the world where the virus is surging, she said. For example, in some East Asian countries, stacked toilet systems could transport the virus between floors of a multistory building, she noted. More research is also needed on how the virus moves indoors. Researchers at the Department of Energy’s Pacific Northwest National Laboratory modeled the flow of aerosol-sized particles after a person has had a five-minute coughing bout in one room of a three-room office with a central ventilation system. Clean outdoor air and air filters both cut down the flow of particles in that room, the scientists reported in April. But rapid air exchanges — more than 12 in an hour — can propel particles into connected rooms, much as secondhand smoke can waft into lower levels or nearby rooms. “For the source room, clearly more ventilation is a good thing,” said Leonard Pease, a chemical engineer and lead author of the study. “But that air goes somewhere. Maybe more ventilation is not always the solution.” In the United States, the C.D.C.’s concession may prompt the Occupational Safety and Health Association to change its regulations on air quality. Air is harder to contain and clean than food or water. But OSHA already mandates air-quality standards for certain chemicals. Its guidance for Covid does not require improvements to ventilation, except for health care settings. “Ventilation is really built into the approach that OSHA takes to all airborne hazards,” said Peg Seminario, who served as director of occupational safety and health for the A.F.L.-C.I.O. from 1990 until her retirement in 2019. “With Covid being recognized as an airborne hazard, those approaches should apply.” In January, President Biden directed OSHA to issue emergency temporary guidelines for Covid by March 15. But OSHA missed the deadline: Its draft is reportedly being reviewed by the White House’s regulatory office. In the meantime, businesses can do as much or as little as they wish to protect their workers. Citing concerns of continued shortages of protective gear, the American Hospital Association, an industry trade group, endorsed N95 respirators for health care workers only during medical procedures known to produce aerosols, or if they have close contact with an infected patient. Those are the same guidelines the W.H.O. and the C.D.C. offered early in the pandemic. Face masks and plexiglass barriers would protect the rest, the association said in March in a statement to the House Committee on Education and Labor. “They’re still stuck in the old paradigm, they have not accepted the fact that talking and coughing often generate more aerosols than do these so-called aerosol-generating procedures,” Dr. Marr said of the hospital group. “We know that Plexiglas barriers do not work,” she said, and may in fact increase the risk, perhaps because they inhibit proper airflow in a room. The improvements do not have to be expensive: In-room air filters are reasonably priced at less than 50 cents per square foot, although a shortage of supply has raised prices, said William Bahnfleth, professor of architectural engineering at Penn State University, and head of the Epidemic Task Force at Ashrae (the American Society of Heating, Refrigerating and Air-Conditioning Engineers), which sets standards for such devices. UV lights that are incorporated into a building’s ventilation system can cost up to roughly $1 per square foot; those installed room by room perform better but could be 10 times as expensive, he said. If OSHA rules do change, demand could inspire innovation and slash prices. There is precedent to believe that may happen, according to David Michaels, a professor at George Washington University who served as OSHA director under President Barack Obama. When OSHA moved to control exposure to a carcinogen called vinyl chloride, the building block of vinyl, the plastics industry warned it would threaten 2.1 million jobs. In fact, within months, companies “actually saved money and not a single job was lost,” Dr. Michaels recalled. In any case, absent employees and health care costs can prove to be more costly than updates to ventilation systems, the experts said. Better ventilation will help thwart not just the coronavirus, but other respiratory viruses that cause influenza and common colds, as well as pollutants. Before people realized the importance of clean water, cholera and other waterborne pathogens claimed millions of lives worldwide every year. “We live with colds and flus and just accept them as a way of life,” Dr. Marr said. “Maybe we don’t really have to.” Source link Orbem News #Air #Pandemic #quality #Scientists #Urge #Wake #workplace
0 notes
Photo

Is COVID-19 Airborne?

For months, the Centers for Disease Control and Prevention (CDC) has said that the novel coronavirus mainly spreads when someone comes into close contact with another person who has the virus. In October, the CDC acknowledged another way that COVID-19 spreads: Through airborne transmission.
To lower your risk of getting infected by this newly recognized method of transmission, you may need to adopt some new habits.
“Mask-wearing, hand-washing and practicing social distancing are still among the most important ways to stop the spread of COVID-19, but there are additional steps that you can take to help protect yourself from airborne spread of the virus,” says Nazar Raoof, M.D., division director of infectious disease at Raritan Bay Medical Center. “However, the most common way to get COVID-19 is still through close contact with others, not airborne transmission.”
The role of respiratory droplets in COVID-19 transmission
For both forms of COVID-19 disease transmission – close contact and airborne – it’s respiratory droplets containing the virus that spread illness.
Everyone produces respiratory droplets, which are tiny, moist particles that are expelled from the nose or mouth when you cough, sneeze, talk, shout, sing or exhale deeply. Respiratory droplets typically travel a few feet through the air before they fall to the ground. They may carry bacteria or viruses if you’re sick.
When people are very close together, these small, largely invisible, droplets may travel from one person to another without either person realizing it, spreading disease. This is why social-distancing guidelines recommend that people stay six feet apart; larger respiratory droplets have trouble traveling that far before gravity pulls them to the ground. Masks also help prevent droplets from spreading between people.
Why airborne transmission is different
Some respiratory droplets are so small, they may hang in the air for minutes or hours, rather than falling to the ground. These droplets, which are sometimes called aerosols, are typically found in indoor spaces with poor ventilation. When outdoors, fresh air and breezes help dissipate these particles.
Aerosols may move through the air within an enclosed space, infecting people who are farther away than six feet. They may also hang in the air after someone with COVID-19 has moved on, infecting others who breathe the tiny particles in.
The more time that you spend in a poorly ventilated indoor space and the more crowded it is, the greater your risk is of contracting COVID-19. For these reasons, experts recommend against spending extended periods in indoor spaces with other people, especially if you aren’t wearing a mask.
Opening windows in indoor spaces can allow for better air circulation and may lower the risk of airborne transmission.
How to protect yourself from airborne COVID-19
To lower your risk of COVID-19, continue to follow the habits that health experts have recommended, and add some new practices to your repertoire:
stay six feet away from people outside of your household
wear a mask in public
wash your hands often
don’t touch your face unless you have clean hands
avoid indoor spaces with poor air circulation, especially crowded spots
plan to meet people in outdoor settings, rather than indoor locations
If you must visit a poorly ventilated indoor space:
keep your mask over your nose and mouth at all times
try to stay at least six feet away from others
open a window to increase air circulation, if possible
spend as little time as possible there, then leave
advice of your physician. Always consult your physician for individual care.
Read full article: https://expatimes.com/?p=18965&feed_id=37069
0 notes
Link
What You Can Do to Avoid the New Coronavirus Variant Right Now
It’s more contagious than the original and spreading quickly. Upgrade your mask and double down on precautions to protect yourself.
By Tara Parker-Pope Jan. 28, 2021
New variants of the coronavirus continue to emerge. A few have caused concern in the United States because they are so contagious and spreading fast. To avoid them, you’ll need to double down on the same pandemic precautions that have kept you safe so far.
The variant known as B.1.1.7., which was first identified in Britain has the potential to infect an estimated 50 percent more people, and researchers have begun to think that it may also be slightly more deadly. The Centers for Disease Control and Prevention has predicted that this variant could become the dominant source of infection in the United States by March. A variant first reported in South Africa has found it’s way to South Carolina. And scientists are studying whether a variant with a different mutation, and first found in Denmark, along with one identified in California, have caused a surge of cases in California.
The new variants appear to latch onto our cells more efficiently. (You can find a detailed look inside one of the variants here.) The change suggests it could take less virus and less time in the same room with an infected person for someone to become ill. People infected with the variant may also shed larger quantities of virus, which increases the risk to people around them.
“The exact mechanism in which it’s more transmissible isn’t entirely known,” said Nathan D. Grubaugh, assistant professor and epidemiologist at the Yale School of Public Health. “It might just be that when you’re infected, you’re exhaling more infectious virus.”
So how do you avoid a more contagious version of the coronavirus? I spoke with some of the leading virus and infectious disease experts about what makes the new variant so worrisome and what we can do about it. Here’s what they had to say.
How can I protect myself from the new coronavirus variant?
The variants spread the same way the coronavirus has always spread. You’re most likely to contract the virus if you spend time in an enclosed space breathing the air of an infected person. The same things that have protected you from the original strain should help protect you from a variant, although you may need to be more rigorous. Wear a two- or three-layer mask. Don’t spend time indoors with people not from your household. Avoid crowds, and keep your distance. Wash your hands often, and avoid touching your face.
Your Coronavirus Tracker: We'll send you the latest data for places you care about each day.
“The first thing I say to people is that it’s not a different virus. All the things we have learned about this virus still apply,” said Dr. Ashish K. Jha, dean of the Brown University School of Public Health. “It’s not like this variant is somehow magically spreading through other means. Anything risky under the normal strain just becomes riskier with the variant.”
And let’s face it, after months of pandemic living, many of us have become lax about our Covid safety precautions. Maybe you’ve let down your guard, and you’re spending time indoors and unmasked with trusted friends. Or perhaps you’ve been dining in restaurants or making more trips to the grocery store each week than you did at the start of lockdowns. The arrival of the variant means you should try to cut back on potential exposures where you can and double down on basic precautions for the next few months until you and the people around you get vaccinated.
“The more I hear about the new variants, the more concerned I am,” said Linsey Marr, professor of civil and environmental engineering at Virginia Tech and one of the world’s leading aerosol scientists. “I think there is no room for error or sloppiness in following precautions, whereas before, we might have been able to get away with letting one slide.”
Should I upgrade my mask?
You should be wearing a high-quality mask when you run errands, go shopping or find yourself in a situation where you’re spending time indoors with people who don’t live with you, Dr. Marr said. “I am now wearing my best mask when I go to the grocery store,” she said. “The last thing I want to do is get Covid-19 in the month before I get vaccinated.”
Dr. Marr’s lab recently tested 11 mask materials and found that the right cloth mask, properly fitted, does a good job of filtering viral particles of the size most likely to cause infection. The best mask has three layers — two cloth layers with a filter sandwiched in between. Masks should be fitted around the bridge of the nose and made of flexible material to reduce gaps. Head ties create a better fit than ear loops.
If you don’t want to buy a new mask, a simple solution is to wear an additional mask when you find yourself in closer proximity to strangers. I wear a single mask when I walk my dog or exercise outdoors. But if I’m going to a store, taking a taxi or getting in the subway, I double mask by using a disposable surgical mask and covering it with my cloth mask.
Do I need an N95 medical mask?
While medical workers who come into close contact with sick patients rely on the gold-standard N95 masks, you don’t need that level of protection if you’re avoiding group gatherings, limiting shopping trips and keeping your distance from others.
“N95s are hard to get,” said Dr. Jha. “I don’t think people should think that’s what they need. Certainly there are a lot of masks out in the marketplace that are pretty good.”
If you’re working in an office or grocery store, or find yourself in a situation where you want added mask protection, you can get an alternative to the N95. Dr. Jha suggested using a KF94 mask, a type of mask made in South Korea that can be purchased easily online. It resembles an N95, with some differences. It’s made of a similar nonwoven material that blocks 94 percent of the hardest-to-trap viral particles. But the KF94 has ear loops, instead of elastic head bands, so it won’t fit as snugly as an N95.
The KF94 is also disposable — you can buy a pack of 20 for about $40 on Amazon. While you can let a KF94 mask air dry and reuse it a few times, it can’t be laundered and won’t last as long as a cloth mask. One solution is to save your KF94 mask for higher-risk situations — like riding a subway, spending time in a store or going to a doctor’s appointment. Use your cloth mask for outdoor errands, exercise or walking the dog.
Are there additional ways to reduce my risk?
Getting the vaccine is the ultimate way to reduce risk. But until then, take a look at your activities and try reducing the time and number of exposures to other people.
For instance, if you now go to the store two or three times a week, cut back to just once a week. If you’ve been spending 30 to 45 minutes in the grocery store, cut your time down to 15 or 20 minutes. If the store is crowded, come back later. If you’re waiting in line, be mindful of staying at least six feet apart from the people ahead of you and behind you. Try delivery or curbside pickup, if that’s an option for you.
If you’ve been spending time indoors with other people who aren’t from your household, consider skipping those events until you and your friends get vaccinated. If you must spend time with others, wear your best mask, make sure the space is well ventilated (open windows and doors) and keep the visit as short as possible. It’s still safest to take your social plans outdoors. And if you are thinking about air travel, it’s a good idea to reschedule given the high number of cases around the country and the emergence of the more contagious variant.
“The new variants are making me think twice about my plan to teach in-person, which would have been with masks and with good ventilation anyway,” Dr. Marr said. “They’re making me think twice about getting on an airplane.”
Will the current Covid vaccines work against the new variants?
Experts are cautiously optimistic that the current generation of vaccines will be mostly effective against the emerging coronavirus variants. Earlier this month, Pfizer and BioNTech announced that their Covid vaccine works against one of the key mutations present in some of the variants. That’s good news, but some data also suggest that variants with certain mutations, particularly the one first seen in South Africa, may be more resistant to the vaccines. While the data are concerning, experts said the current vaccines generate extremely high levels of antibodies, and they are likely to at least prevent serious illness in people who are immunized and get infected.
“The reason why I’m cautiously optimistic is that from what we know about how vaccines work, it’s not just one antibody that provides all the protection,” said Dr. Adam Lauring, associate professor of infectious disease at the University of Michigan. “When you get vaccinated you generate antibodies all over the spike protein. That makes it less likely that one mutation here or there is going to leave you completely unprotected. That’s what gives me reason for optimism that this is going to be OK in terms of the vaccine, but there’s more work to be done.”
If I catch Covid-19, will I know if I have the new variant?
Probably not. If you test positive for the coronavirus, the standard PCR test can’t definitively determine if you have the variant or the original strain. While some PCR test results can signal if a person is likely to be infected with a variant, that information probably won’t be shared with patients. The only way to know for sure which variant is circulating is to use gene sequencing technology, but that technology is not used to alert individuals of their status. While some public health and university laboratories are using genomic surveillance to track the prevalence of variants in a community, the United States doesn’t yet have a large-scale, nationwide system for checking coronavirus genomes for new mutations.
Treatment for Covid-19 is the same whether you have the original strain or the variant. You can read more about what to do if you get infected here.
Are children more at risk from the new variant?
Children appear to get infected with the variant at about the same rate as the original strain. A large study by health officials in Britain found that young children are only about half as likely as adults to transmit the variant to others. While that’s good news, the highly contagious nature of the variant means more children will get the virus, even if they are still proportionately less contagious and less prone to getting infected than adults. You can learn more here.
If I’ve already had Covid-19, am I likely to have the same level of immunity to the new strain?
Most experts agree that once you’ve had Covid-19, your body has some level of natural immunity to help fight off a second infection — although it’s not known how long the protection lasts. The variants circulating in Brazil and South Africa appear to have mutations that allow the virus to evade natural antibodies and reinfect someone who has already had the virus. The concern is based on lab tests using antibodies of people with a previous infection, so whether that translates to more reinfections in the real world isn’t known. The effect of the vaccine against these variants isn’t known yet either. While all of this sounds frightening, scientists are hopeful that even if the vaccines don’t fully protect against new variations of the virus, the antibodies generated by the vaccine still will protect people from more serious illness.
https://www.nytimes.com/2021/01/19/well/live/covid-b117-variant-advice.html?utm_source=pocket-newtab
0 notes
Text
Covid19 enables people to recognize the value of fresh air system
A sudden covid19 touched everyone's heart,
People want to have a safe and comfortable indoor air!
Novel coronavirus pneumonia may spread through aerosol
At present, the main transmission routes of new coronavirus are respiratory droplets transmission and contact transmission, aerosol and fecal oral transmission. In order to prevent the air leakage of bacteria contained in the ward and discharge to the adjacent room or environment outside the ward, and to further protect the medical staff or other patients in the ward (non single ward), in addition to wearing masks, they should also isolate the ward and its patients through negative pressure Purification air conditioning system, buffer facilities and other dilution, reduce indoor bacteria concentration, achieve secondary isolation.
Should windows be opened for ventilation?
In order to reduce the influence of suspended aerosols, proper ventilation measures are necessary. However, it should be noted that aerosols are relative. When other improper air flow is involved, the original settled particles (especially the dried droplet cores) can be resuspended under the effect of turbulence, or the original polluted aerosols can flow to the non polluted areas and expand the propagation range.
This is particularly important for people living at home. For example, patients must be isolated in a single room at home. When natural ventilation is carried out in public areas or other rooms, the doors and windows of the patient's room must be closed, and devices with high velocity such as fans should not be used to avoid turbulence and resuspension of particles.
Nowadays, almost every household has installed air conditioning. Whether it is central air conditioning or split air conditioning, all the air is recycled in a closed environment. Once someone is infected, will more people be infected due to virus transmission?
It is said that the air can be disinfected. Yes, but pay special attention to the fact that when disinfecting the air with disinfectant, it must be operated in an unattended environment. If a person inhales disinfectant or repeatedly sprays disinfectant on the body, there is a potential risk, which may stimulate the respiratory tract and increase the possibility of triggering respiratory diseases.
I believe we all know that it's easy to get dizzy, chest tightness and fatigue if you stay in a closed space with central air conditioning on all day long. This is precisely because the air is not circulating, the human body exhaled a large amount of carbon dioxide in the indoor circulation, unable to discharge, resulting in the reduction of oxygen content. Excessive carbon dioxide concentration will cause mild headache, slow reaction, and even individual dyspnea and other symptoms!
As we all know, ventilation is only through opening windows or using special ventilation equipment to circulate indoor and outdoor air. However, the fresh air equipment is a kind of device that can help indoor ventilation. It introduces the outdoor fresh air into the room after treatment, and discharges the indoor polluted air to the outdoor, so as to ensure the indoor air circulation and ensure the indoor fresh air at all times. The working principle of the system is to connect the outdoor air and form the indoor and outdoor air circulation by using the fan power and the pipe induced and exhaust air technology.
Start up 24-hour fresh air system
Provide fresh and clean air for the family
Suzhou Mia intelligent Technology Co.,Ltd
0 notes
Text
Ventilating complaints about air standards
The world has finally accepted that the COVID-19 virus is spread on the air, and mainly indoors. So why haven’t ventilation standards been updated for buildings?
This article first appeared in Cosmos Weekly on 30 July 2021. For more stories like this, subscribe to Cosmos Weekly.
Australia is in the grips of another COVID-19 outbreak. This time, the highly transmissible Delta variant of SARS-CoV-2 has plunged many into lockdown and put the nation on high alert.
Epidemiologists say the Delta variant, which has spread to 104 countries and counting, may be about 90% more infectious than the original – Alpha – strain of SARS-CoV-2. But one thing remains the same: this virus is airborne. It spreads in the air we breathe. In lab studies, SARS-CoV-2 has been shown to linger in the air for up to 16 hours, carried aloft on microscopic particles called aerosols.
World-leading aerosol scientist Professor Lidia Morawska, of Queensland University of Technology (QUT), in Brisbane, says the latest outbreak has once again exposed the gaps in our hotel quarantine system and highlighted flaws in building design and ventilation systems – which should flush out contaminated air, without affecting other occupants, if designed correctly and operating well.
“Well over a year into the pandemic, there hasn’t seen any progress whatsoever [in Australia] to tackle this,” Morawska says. “No one mentions the word ventilation.”
The latest outbreak has once again exposed the gaps in our hotel quarantine system and highlighted flaws in building design and ventilation system.
Morawska is not alone in her frustration. Architects and building engineers are also calling for stronger recognition of respiratory viruses that spread via aerosols and improvements to ventilation in public spaces.
“We knew in July last year that SARS-CoV-2 was airborne,” says architect Geoff Hanmer, an adjunct professor of architecture at the University of Adelaide. “And yet it’s taken ISIAQ [the International Society of Indoor Air Quality and Climate] and the World Health Organization almost a year to admit that that’s the case.”
These experts’ exasperation is exacerbated because the engineering solutions to rid indoor spaces of airborne pathogens already exist – they just need to be installed or upgraded.
What needs to be done?
There are three key ingredients in the cocktail that is infection risk, Morawska explains. The first is the concentration of airborne particles that are emitted when an infected person talks, sings, coughs or sneezes. Second, a lack of ventilation, which lets aerosols linger in the air. And thirdly, some exposure time for people to inhale the virus-laden particles.
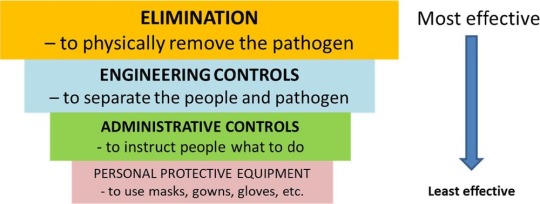
Traditional infection control pyramid adapted from the US Centers for Disease Control. Credit: Morawska et al/CDC/Environment International
Changing how buildings operate can address two out of those three factors. Improved ventilation increases airflow, diluting airborne particles; incorporating high-grade filtration systems can remove microscopic contaminants from the air.
However, the current standards for ventilating indoor public spaces (excluding hospitals) are not designed for infection control.
Public buildings from hospitals to schools and aged care facilities are “naturally” ventilated, meaning they rely on open windows to let fresh air in. They often have inadequate or poor ventilation, particularly in colder months.
“Very few countries have any regulations about indoor air quality. Infection transmission – which occurs mainly in indoor public spaces – is not specifically mentioned in any national regulations,” says Morawska.
“We must do something about the [building industry] standards.”
Hanmer says revising construction codes to improve ventilation standards to control for airborne infections would be a good start.
“But the problem is that new buildings are only a very small fraction of the total population of buildings,” he says.
Public buildings from hospitals to schools and aged care facilities are “naturally” ventilated, meaning they rely on open windows to let fresh air in. They often have inadequate or poor ventilation, particularly in colder months.
Many commercial buildings, such as shopping centres, hotels and universities, are also poorly ventilated, Hanmer says, because the performance of their mechanical ventilation systems – which pump in fresh air to replace stale indoor air – is too often substandard.
“It’s a bit of a lottery at the moment – certainly we need to get to a state where we’ve got better data and better regulation on air quality, generally,” says Hanmer, who recently surveyed the air quality in a number of public buildings.
“Clearly, the application of [national construction] codes in mechanically ventilated buildings hasn’t been as good as it should be.”
How can it be done?
Increasing ventilation rates to create greater airflow through rooms and buildings is one way to minimise infection risk indoors.
In 2009, WHO compiled 65 studies showing that poor ventilation is “associated with increased infection rates or outbreaks of airborne diseases”, concluding that “higher ventilation rates could decrease the risk of infection”.
But hard evidence linking improved ventilation with reduced infection rates directly is scarce. A 2019 study from the Taiwan Centres of Disease Control is a rare example. It found that increasing ventilation in stuffy university buildings controlled an outbreak of tuberculosis, an airborne bacterial disease. The outbreak, which lasted three years and involved 27 active cases and 1,665 contacts, was snuffed out after ventilation specialists reconfigured the building’s ventilation systems to improve airflow.

Portable air purifiers may help. Credit: Onurdongel/Getty
Fast forward to 2021, and both the WHO and US Centres for Disease Control and Prevention (CDC) now recommend that the total indoor air volume in healthcare facilities should be replaced with fresh outdoor air a minimum of 6 to 12 times per hour to prevent the spread of COVID-19.
Epidemiologist Mary-Louise McLaws, of UNSW Sydney, says this is the gold standard for ventilation for “hot zones” in hospitals – equivalent to 80 litres of air per second per person – and that these ventilation rates can be hard to achieve. In other settings, such as confined spaces and offices, airflow rates of 3 litres of air per second per person are needed, McLaws says.
While experts deliberate over exactly how much ventilation is needed to reduce infection rates, Morawska says there is no magic number because it depends on how the building is used.
This includes the number of people in each room (“The more sources, the higher the [required] ventilation rate,” she says) and their usual activities such as exercising, singing or talking loudly, all of which expel large amounts of viral particles.
Occupancy, though, can vary from one hour to the next, so ventilation systems need to be flexible. But ramping up ventilation is not just a matter of a simple flick of a switch; airflow direction and distribution are also important.

Engineering level controls to reduce the environmental risks for airborne transmission. Credit: Morawska et al/Environment International
Adding pathogen-proof filters to existing ventilation systems is not always possible either, if the airflow is too weak. Engineers also need to design ventilation systems with energy conservation in mind, Morawska says.
“It’s not just about increasing ventilation rates,” she says. We need smarter systems that remove the virus or any other contaminants but do not increase energy use.”
“We need to make sure that naturally ventilated buildings with high use have some fallback ventilation,” he says.
Demand-controlled systems could be used in schools to increase ventilation during predictably busy periods and dial airflow down when rooms are not in use. Another option is installing ventilation systems that detect rising levels of CO2 levels and kick in when air quality deteriorates, says Hanmer.
Ramping up ventilation is not just a matter of a simple flick of a switch; airflow direction and distribution are also important.
A fallback ventilated system comes into operation when the detected levels of CO2 in the air rise above about 800 parts per million, so it could reliably improve air quality, Hanmer says. Aged-care facilities would be the “absolute first priority” and schools a close second.
Building systems engineer Professor John Zhai, of the University of Colorado Boulder, suggests a simpler solution: portable air purifiers could be installed to filter air in crowded public spaces such as supermarket checkouts. These systems could be deployed quickly to reduce infection risk, provided they are the right size for the space.
Researchers are also designing smart systems that can detect mobile phone signals or use cameras (with image-processing algorithms) to determine when an indoor space gets too crowded and needs more ventilation, adjusting flow rates accordingly.
What would it cost?
Few economic analyses have been done to estimate the cost of improving ventilation because no one has been asking the question, says Morawska. However, available estimates suggest that necessary investments in building systems may be less than 1% of the construction cost of a typical building for new builds.
Hanmer estimates it would cost a few thousand dollars per room to install fallback ventilation systems in aged-care facilities. “I don’t think that’s an unreasonable burden given the seriousness of the disease,” he says. “And it’s whole lot less than a lockdown in a major capital city.”
But on top of the price tag for installations and upgrades, Zhai says that building engineers also have to consider the energy costs of running souped-up ventilation systems. Installing high-grade filters capable of trapping and removing microscopic airborne particles means greater fan power is needed to push the air through the filter – and that uses more energy, he says.
Around 40% of the total electricity used in buildings already goes into powering ventilation fans and it would take tremendous amounts of energy to increase airflow rates to recommended levels, Zhai says: “To double the flow rate, you basically need eight times the energy use.
The cost of improving ventilation system would be far less than the billions of dollars spent each year on influenza and other respiratory diseases.
“It can work for most emergency situations. You can supply a lot of air for a short period of time, to reduce infection risk. But for regular times, it’s not economically wise to do that.”
Morawska says, however, that the cost of improving ventilation system would be far less than the billions of dollars spent each year on influenza and other respiratory diseases. It could also help curb the costs of COVID-19, which currently has a global financial toll to the tune of $1 trillion each month.
But if countries continue to dismiss the airborne transmission of COVID-19 and other infectious diseases, as they have done for decades, then we will suffer the cost of this denial, Morawska says.
“Unless we start putting steps in place now to fix things on the longer term, once the pandemic passes – and it will eventually pass – no one will want to do anything about this,” she says.
“We’ll be left in exactly in the same situation when the next pandemic comes and still dealing with respiratory infections like the cold and flu.”
This article first appeared in Cosmos Weekly on 30 July 2021. To see more in-depth stories like this, subscribe today and get access to our weekly e-publication, plus access to all back issues of Cosmos Weekly.
Subscribe now
Ventilating complaints about air standards published first on https://triviaqaweb.weebly.com/
0 notes
Text
DOH suggests holding of activities in open spaces amid pandemic
#PHnews: DOH suggests holding of activities in open spaces amid pandemic
MANILA – The Department of Health (DOH) on Monday advised the public to conduct activities in open air spaces, install exhaust fans in comfort rooms and avoid usage of recirculated air option for vehicles to prevent possibility of contracting the coronavirus disease 2019 (Covid-19) through airborne transmission.
Health Undersecretary Maria Rosario Vergeire, in a virtual press briefing on Monday, said that while health experts are still studying the possibility of airborne infection, the DOH has issued Department Memorandum 2020-0429 which provides administrative and engineering controls for the improvement of ventilation and air quality in enclosed, indoor spaces and lessen the transmission of the virus.
“When an activity cannot be moved into an open air setting, opening windows and doors should be put into practice to facilitate the flow of outdoor air into the space, when possible,” the memorandum read.
The DOH advised individuals not to stay where air coming from fans and air-conditioning units flow directly as these may facilitate the transmission of the coronavirus "by directing air from infected individuals to others in the room".
“In non-hospital settings where ventilation is greatly recirculated or access to outside air is not feasible, filters such as high-efficiency particulate air filtration air purifiers can be used to clean recirculated air provided that the unit is adequate for the size of the room in which it is installed in,” it added.
The DOH also suggested the installation of exhaust fans in comfort rooms and closing of the toilet seat lid while flushing to “minimize the release of droplets into air flows after flushing".
“Utilize the car’s vents to bring in fresh outside air and/or lower the vehicle windows,” the DOH said, adding that recirculated air option for the vehicle’s ventilation during passenger transport must be avoided.
Earlier, the US Centers for Disease Control and Prevention said people with Covid-19 seem to have infected others who were more than six feet away in enclosed spaces and inadequate ventilation. (PNA)
***
References:
* Philippine News Agency. "DOH suggests holding of activities in open spaces amid pandemic." Philippine News Agency. https://www.pna.gov.ph/articles/1118297 (accessed October 13, 2020 at 05:39AM UTC+14).
* Philippine News Agency. "DOH suggests holding of activities in open spaces amid pandemic." Archive Today. https://archive.ph/?run=1&url=https://www.pna.gov.ph/articles/1118297 (archived).
0 notes
Text
How to use ventilation and air filtration to prevent the spread of coronavirus indoors
#thevastmajority💸 👨👨👦 👨👩👧👦
more news https://northdenvernews.com
The vast majority of SARS-CoV-2 transmission occurs indoors, most of it from the inhalation of airborne particles that contain the coronavirus. The best way to prevent the virus from spreading in a home or business would be to simply keep infected people away. But this is hard to do when an estimated 40% of cases are asymptomatic and asymptomatic people can still spread the coronavirus to others.
Masks do a decent job at keeping the virus from spreading into the environment, but if an infected person is inside a building, inevitably some virus will escape into the air.
Shelly Miller
I am a professor of mechanical engineering at the University of Colorado Boulder. Much of my work has focused on how to control the transmission of airborne infectious diseases indoors, and I’ve been asked by my own university, my kids’ schools and even the Alaska State Legislature for advice on how to make indoor spaces safe during this pandemic.
Once the virus escapes into the air inside a building, you have two options: bring in fresh air from outside or remove the virus from the air inside the building.
It’s all about fresh, outside air
The safest indoor space is one that constantly has lots of outside air replacing the stale air inside.
In commercial buildings, outside air is usually pumped in through heating, ventilating and air-conditioning (HVAC) systems. In homes, outside air gets in through open windows and doors, in addition to seeping in through various nooks and crannies.
COVID-19 IN COLORADO
The latest from the coronavirus outbreak in Colorado:
MAP: Known cases in Colorado.
TESTING: Here’s where to find a community testing site. The state is now encouraging anyone with symptoms to get tested.
STORY: Is your throat scratchy from Colorado’s wildfire smoke or coronavirus? Here’s how to tell.
>> FULL COVERAGE
Simply put, the more fresh, outside air inside a building, the better. Bringing in this air dilutes any contaminant in a building, whether a virus or a something else, and reduces the exposure of anyone inside. Environmental engineers like me quantify how much outside air is getting into a building using a measure called the air exchange rate. This number quantifies the number of times the air inside a building gets replaced with air from outside in an hour.
While the exact rate depends on the number of people and size of the room, most experts consider roughly six air changes an hour to be good for a 10-foot-by-10-foot room with three to four people in it. In a pandemic this should be higher, with one study from 2016 suggesting that an exchange rate of nine times per hour reduced the spread of SARS, MERS and H1N1 in a Hong Kong hospital.
Many buildings in the U.S., especially schools, do not meet recommended ventilation rates. Thankfully, it can be pretty easy to get more outside air into a building. Keeping windows and doors open is a good start. Putting a box fan in a window blowing out can greatly increase air exchange too. In buildings that don’t have operable windows, you can change the mechanical ventilation system to increase how much air it is pumping. But in any room, the more people inside, the faster the air should be replaced.
Using CO2 to measure air circulation
So how do you know if the room you’re in has enough air exchange? It’s actually a pretty hard number to calculate. But there’s an easy-to-measure proxy that can help. Every time you exhale, you release CO2 into the air. Since the coronavirus is most often spread by breathing, coughing or talking, you can use CO2 levels to see if the room is filling up with potentially infectious exhalations. The CO2 level lets you estimate if enough fresh outside air is getting in.
Outdoors, CO2 levels are just above 400 parts per million (ppm). A well ventilated room will have around 800 ppm of CO2. Any higher than that and it is a sign the room might need more ventilation.
READ: Colorado Sun opinion columnists.
Last year, researchers in Taiwan reported on the effect of ventilation on a tuberculosis outbreak at Taipei University. Many of the rooms in the school were underventilated and had CO2 levels above 3,000 ppm. When engineers improved air circulation and got CO2 levels under 600 ppm, the outbreak completely stopped. According to the research, the increase in ventilation was responsible for 97% of the decrease in transmission.
Since the coronavirus is spread through the air, higher CO2 levels in a room likely mean there is a higher chance of transmission if an infected person is inside. Based on the study above, I recommend trying to keep the CO2 levels below 600 ppm. You can buy good CO2 meters for around $100 online; just make sure that they are accurate to within 50 ppm.
Air cleaners
If you are in a room that can’t get enough outside air for dilution, consider an air cleaner, also commonly called air purifiers. These machines remove particles from the air, usually using a filter made of tightly woven fibers. They can capture particles containing bacteria and viruses and can help reduce disease transmission.
The U.S. Environmental Protection Agency says that air cleaners can do this for the coronavirus, but not all air cleaners are equal. Before you go out and buy one, there are few things to keep in mind.
The first thing to consider is how effective an air cleaner’s filter is. Your best option is a cleaner that uses a high-efficiency particulate air (HEPA) filter, as these remove more than 99.97% of all particle sizes.
The second thing to consider is how powerful the cleaner is. The bigger the room – or the more people in it – the more air needs to be cleaned. I worked with some colleagues at Harvard to put together a tool to help teachers and schools determine how powerful of an air cleaner you need for different classroom sizes.
The last thing to consider is the validity of the claims made by the company producing the air cleaner.
The Association of Home Appliance Manufacturers certifies air cleaners, so the AHAM Verifide seal is a good place to start. Additionally, the California Air Resources Board has a list of air cleaners that are certified as safe and effective, though not all of them use HEPA filters.
Keep air fresh or get outside
Both the World Health Organization and U.S. Centers for Disease Control and Prevention say that poor ventilation increases the risk of transmitting the coronavirus.
If you are in control of your indoor environment, make sure you are getting enough fresh air from outside circulating into the building. A CO2 monitor can help give you a clue if there is enough ventilation, and if CO2 levels start going up, open some windows and take a break outside. If you can’t get enough fresh air into a room, an air cleaner might be a good idea. If you do get an air cleaner, be aware that they don’t remove CO2, so even though the air might be safer, CO2 levels could still be high in the room.
If you walk into a building and it feels hot, stuffy and crowded, chances are that there is not enough ventilation. Turn around and leave.
By paying attention to air circulation and filtration, improving them where you can and staying away from places where you can’t, you can add another powerful tool to your anti-coronavirus toolkit.
Shelly Miller is professor of Mechanical Engineering, University of Colorado Boulder. This article is republished from The Conversation under a Creative Commons license. Read the original article.
The Colorado Sun is a nonpartisan news organization, and the opinions of columnists and editorial writers do not reflect the opinions of the newsroom. Read our ethics policy for more on The Sun’s opinion policy and submit columns, suggested writers and more to [email protected].
Our articles are free to read, but not free to report
Support local journalism around the state.
Become a member of The Colorado Sun today!
$5/month
$20/month
$100/month
One-time Contribution
The latest from The Sun
What’s Working: Spanish-speaking virtual agents, extra $300 weeks approved and a new small business fund
How to use ventilation and air filtration to prevent the spread of coronavirus indoors
How a Charlie Sheen news story ushered Colorado author into the world of cryptids and adventure
Colorado lists 20 coronavirus cases tied to Sturgis motorcycle rally
Colorado Supreme Court declines to hear Republican challenge to Gov. Jared Polis’ mask mandate
from https://ift.tt/34PA0AF https://ift.tt/34EHuX0
0 notes
Text
COVID-19 case clusters offer lessons and warnings for reopening
Several months into the COVID-19 pandemic, countries are looking for ways to restart their economies, public health officials are looking to guide safe reopening and people are eagerly looking to escape cabin fever. But tough lessons have surfaced from countries that were hit early in the pandemic and have already reopened.
Consider South Korea: In April, after new cases had steadily declined to single digits, the country began easing lockdown restrictions. But that respite was short-lived. On May 6, a 29-year-old man tested positive for SARS-CoV-2, just a few days after visiting five dance clubs in one night in Seoul’s Itaewon district. On May 8, South Korea responded quickly, postponing plans to reopen schools and urging bars and clubs to shut down again for a month. As of June 8, the Korean Centers for Disease Control had linked the sick man to 96 other clubgoers who got COVID-19, plus 178 people with whom those clubgoers came into contact.
That wasn’t the only cluster that put the brakes on South Korea’s reopening plans. Soon more clusters popped up in an online retail center, a theme park, a table tennis club and a handful of churches.
Other countries should expect similar starts and stops upon relaxing stay-at-home rules. “Reopening is not a one-way street, and we may need to make a U-turn,” says Andrew Noymer, an epidemiologist at the University of California, Irvine.
Studying these kinds of transmission clusters as well as common environments where COVID-19 moves easily from person to person provides a glimpse of how to avoid the U-turns. To that end, epidemiologist Gwenan Knight and her colleagues at the London School of Hygiene and Tropical Medicine compiled a massive database of worldwide COVID-19 case clusters based on media accounts, published scientific studies and government health department reports.
As of June 10, their database included 231 cluster events, or groups of cases tied to the same place. The data are limited to known clusters and to what the patients involved could recall and what they told investigators.
Where does COVID-19 spread?
A team at the London School of Hygiene and Tropical Medicine has compiled a database of 231 known COVID-19 case clusters, represented in the graphic here. The settings are color-coded based on whether the virus spread in an indoor vs. outdoor setting, and each bubble’s size represents the number of cases in the cluster. As much as possible, the team looked at the first round of transmission, in hopes of getting an accurate snapshot of the risks different types of settings pose. When data were available, the team also calculated a cluster’s attack rate, or the percentage of people who got sick out of the total number of people present.
The most prevalent setting among reported clusters is in households, and the largest clusters occurred aboard ships. The London team’s database includes some entries that represent more than one cluster; in this chart, those have been separated out so each bubble shown represents a single cluster.
Some interesting trends have emerged. Indoor settings dominate, partly because the virus hit during winter, when people spend most of their time indoors, and partly because in outdoor settings an abundant flow of fresh air helps dissipate virus particles exhaled by an infected person. Ultraviolet rays from the sun might also help kill virus particles.
Households were the most common place for transmission, accounting for 15 percent, or 38 of 231, cluster events. And mealtime was prime time. “It’s not the eating. It’s the sitting around and talking,” Noymer suspects. SARS-CoV-2 primarily spreads via respiratory droplets and direct contact. While sharing food or utensils could theoretically pose a risk for infection, no clusters have been linked to eating itself. A study published June 3 in Emerging Infectious Diseases found traces of SARS-CoV-2 genetic material on chopsticks used by patients in Hong Kong, but whether virus particles could survive on a chopstick and actually infect someone remains unknown.
The largest known clusters occurred in settings that are by now well publicized: ships (the Diamond Princess cruise ship and the USS Teddy Roosevelt aircraft carrier), food packing plants and prisons. Dormitories in Singapore, where migrant workers live in cramped conditions, also saw large numbers of infections. In all of these places, people live or work in close quarters over long periods of time.

Worker dormitories have had several outbreaks of COVID-19. Singapore’s Minister for Manpower Josephine Teo visited a foreign worker dormitory in May called Westlite Papan, where health officials are carrying out daily testing for COVID-19.WALLACE WOON/EPA-EFE/Shutterstock
The dataset also points to settings where one activity may be riskier than another, says Quentin Leclerc, an epidemiologist on Knight’s team who manages the database. “For example, why have we found clusters associated with one type of indoor sport, but not another?” In a cluster of 112 cases stemming from Zumba classes in Cheonan, South Korea, a pilates and yoga instructor from the same gym was among those infected. But that instructor did not subsequently pass the virus on to any students. High intensity sports that involve a lot of heavy breathing in confined spaces could be prime spots for transmission, while lower intensity activities, like yoga, might not be as risky (SN: 5/19/20).
Only one transportation cluster — three cases on a bus — appears in the database, but that doesn’t mean the virus doesn’t spread on buses or trains. “Transport outbreaks are very difficult to identify,” says Yuguo Li, an engineer at the University of Hong Kong who studies infectious disease transmission.
Of course there could be other possible transmission settings that researchers don’t know about or haven’t been able to study. But the case clusters below might offer some useful insights.
A restaurant with poor ventilation
A cautionary tale of poor ventilation comes from Guangzhou, China, on the eve of Lunar New Year. A 63-year-old woman and her family walked into a crowded restaurant for lunch, after returning from Wuhan the day before. That same day she developed a fever and cough; she later tested positive for the coronavirus.
Of the 89 other customers who visited the restaurant that day, 10 fell ill with COVID-19, including the woman and four members of her family. Patients are most contagious around the time their symptoms emerge, so this woman was most likely the index case — the first person in the cluster to become infected.
The five other infections occurred in families seated at the tables on either side of hers, less than three feet away. Security footage shows that the three families didn’t interact or touch the same objects. The droplets the woman produced as she chatted with her family were unlikely to reach the other tables on their own. So the virus probably got some help from the air conditioning unit blowing directly over the row of three tables, researchers from the Guangzhou Center for Disease Control and Prevention report in the July Emerging Infectious Diseases.
The restaurant had no windows. The only source of outside air was an exhaust fan in a bathroom. The air conditioning unit only recirculated indoor air, blowing the woman’s respiratory droplets to the nearby tables. With very little fresh air coming in, the concentration of droplets would get higher and higher, says Yan Chen, an engineer at Purdue University in West Lafayette, Ind.
In the zone

Y. Li et al/medRxiv 2020
In the Guangzhou restaurant illustrated here, one sick patron infected nine others. Air conditioning units cooled different zones, and one unit blew directly over the three tables where COVID-19 cases arose. The woman believed to be the index case (magenta, just left of center at top of image) was seated with her family at the middle table. Air flowing from the air conditioning unit may have blown her respiratory droplets over to the table farthest from the AC unit. The air then bounced off the wall and brought those droplets back in the direction of the table on the other side, next to the AC unit.
In this computer simulation based on trace gas tests conducted at the restaurant, droplets (turquoise) congregate in the air around the three tables due to the airflow from the air conditioning unit and poor ventilation in the room. The red figures represent the other people who fell ill with COVID-19 after eating at the restaurant at the same time.
When the restaurant was empty during lockdown, Li and his colleagues tested the theory with a few human volunteers, some mannequins and harmless gas droplets to trace and simulate the spread. Their preliminary simulations, posted online April 22 at medRxiv.org, show that the air conditioning flow in the room could have created a bubble of small droplets around the three tables, and that there was an exceptionally low amount of fresh air in the room. That’s where the blame for infection lies, Li’s team argues. With more fresh air in the mix, droplet concentration would probably have been lower.
Long work shifts at close proximity
A case cluster in a South Korean call center provides an example of how COVID-19 can emerge in a bustling open-office setting — and how to intervene and stop transmission.
The call center in downtown Seoul occupies four floors in a 19-story building that has commercial offices and residences. When almost all of building users — 1,143 people — were tested, 97 were positive for SARS-CoV-2; 94 of them worked in call center offices on the 11th floor, researchers report in the August Emerging Infectious Diseases.
Employees sat side by side, talking on the phone for long shifts. Because a striking majority of cases were concentrated in a single open work area on one side of the building, researchers suspect that prolonged proximity, rather than, say, touching the same elevator button drove the spread.
Crowded call center
Most of the 97 COVID-19 cases in a mixed residential and commercial building in downtown Seoul, South Korea, were concentrated on the 11th floor. There, 94 call center employees tested positive for COVID-19 (workstations of people who got infected shown in blue), most of them concentrated on one side of the building.

S. Park et al/Emerging Infectious Diseases 2020
At the call center, the Korean CDC was extremely thorough in its attempts to find cases and stop their spread, testing 99.8 percent of the people who had any contact with the building and quickly isolating all positive cases. Beyond the building, investigators tracked 225 household contacts of those positive cases, and 34 tested positive. Through this intense screening process, the agency cut transmission chains and prevent new cases from emerging. “It shows how intervention can work,” says Werner Bischoff, an epidemiologist at Wake Forest University in Winston-Salem, N.C.
Sharing more than memories
A sobering warning about the importance of social distancing comes from a family in Irbid, Jordan, about 60 miles north of Amman. Defying a local ban on large gatherings, the family held a wedding celebration in March. Of the roughly 360 people who attended, 76 tested positive for the coronavirus in the four weeks that followed, researchers report in the September Emerging Infectious Diseases.
Sign up for e-mail updates on the latest coronavirus news and research
Two days before the ceremony the bride’s 58-year-old father, who had traveled from Spain, felt feverish and developed a runny nose and cough. He tested positive for the coronavirus two days after the wedding.
Though he did not recall having contact with anyone who had COVID-19 in Spain, scientists believe he sparked the cluster. In Jordan, it’s common for the bride’s family to greet all of the guests at the reception entrance, usually with a hug or a kiss. “These factors, in addition to crowded dancing and close face-to-face communication, likely contributed to the large number of infections from this wedding,” the researchers write.
Lockdown exit strategies
Some unknown variables — like the effectiveness of fabric masks and the degree to which infected people without symptoms spread the virus — could influence the risk equation for coronavirus in any of these and other settings.
As restrictions lift, people will have to make tough choices about in-person interactions. Social distancing is still important. You might limit your contacts, but other people you encounter might not. As restrictions ease, some public health officials suggest creating COVID-19 “bubbles,” or expanding social circles to people who agree to observe the same precautionary measures.

In South Korea, some restaurants like this food hall have erected plexiglass barriers between diners, in hopes of reducing the spread of COVID-19.Chung Sung-Jun/Getty Image
Restaurants and workplaces can take steps when they reopen to try to limit transmission, as some have already done. Installing plexiglass barriers between tables and improving ventilation by opening windows, serving customers outside, turning on exhaust fans and using HEPA filters could help lower transmission risk. Keeping tables or desks at least six feet apart is also a good idea. The CDC has released reopening guidelines for everything from restaurants to water parks.
Whether more outdoor cases will emerge as temperatures rise and people spend more time outside is an open question. Fresh air and sunlight could limit cases in outdoor settings, or clusters could emerge in newly opened outdoor settings, such as swimming pools or summer camps. Data on how the virus behaves in summer just don’t exist yet.
If South Korea’s thwarted first attempt at loosening restrictions has taught us anything, it’s that reopening and lifting social distancing practices comes with one certainty: New COVID-19 infections will happen. Hugs and high-fives are still a long way off. “This isn’t a marathon,” Noymer says. “It’s a 26.2-mile sprint.”
.image-mobile {display: none;} .image-tablet {display: none;} @media (max-width: 650px) { .image-mobile {display: none;} .image-desktop {display: none;} .image-tablet {display: block;} } @media (max-width: 420px) { .image-mobile {display: block;} .image-desktop {display: none;} .image-tablet {display: none;} }
from Tips By Frank https://www.sciencenews.org/article/coronavirus-covid-19-case-clusters-lessons-warnings-reopening
0 notes
Text
The best ways to reduce the risk of COVID-19 indoors
Many factors play into the effectiveness of ventilation systems on COVID-19. (Meritt Thomas/Unsplash/)
Shelly Miller is a professor of mechanical engineering at the University of Colorado Boulder. This story originally featured on The Conversation.
The vast majority of SARS-CoV-2 transmission occurs indoors, most of it from the inhalation of airborne particles that contain the coronavirus. The best way to prevent the virus from spreading in a home or business would be to simply keep infected people away. But this is hard to do when an estimated 40 percent of cases are asymptomatic and asymptomatic people can still spread the coronavirus to others.
Masks do a decent job at keeping the virus from spreading into the environment, but if an infected person is inside a building, inevitably some virus will escape into the air.
I’m a professor of mechanical engineering at the University of Colorado Boulder. Much of my work has focused on how to control the transmission of airborne infectious diseases indoors, and I’ve been asked by my own university, my kids’ schools and even the Alaska State Legislature for advice on how to make indoor spaces safe during this pandemic.
Once the virus escapes into the air inside a building, you have two options: bring in fresh air from outside or remove the virus from the air inside the building.
It’s all about fresh, outside air
The safest indoor space is one that constantly has lots of outside air replacing the stale air inside.
In commercial buildings, outside air is usually pumped in through heating, ventilating, and air-conditioning (HVAC) systems. In homes, outside air gets in through open windows and doors, in addition to seeping in through various nooks and crannies.
Simply put, the more fresh, outside air inside a building, the better. Bringing in this air dilutes any contaminant in a building, whether a virus or a something else, and reduces the exposure of anyone inside. Environmental engineers like me quantify how much outside air is getting into a building using a measure called the air exchange rate. This number quantifies the number of times the air inside a building gets replaced with air from outside in an hour.
While the exact rate depends on the number of people and size of the room, most experts consider roughly six air changes an hour to be good for a 10-foot-by-10-foot room with three to four people in it. In a pandemic this should be higher, with one study from 2016 suggesting that an exchange rate of nine times per hour reduced the spread of SARS, MERS, and H1N1 in a Hong Kong hospital.
Many buildings in the US, especially schools, do not meet recommended ventilation rates. Thankfully, it can be pretty easy to get more outside air into a building. Keeping windows and doors open is a good start. Putting a box fan in a window blowing out can greatly increase air exchange too. In buildings that don’t have operable windows, you can change the mechanical ventilation system to increase how much air it is pumping. But in any room, the more people inside, the faster the air should be replaced.
Using CO2 to measure air circulation
So how do you know if the room you’re in has enough air exchange? It’s actually a pretty hard number to calculate. But there’s an easy-to-measure proxy that can help. Every time you exhale, you release CO2 into the air. Since the coronavirus is most often spread by breathing, coughing or talking, you can use CO2 levels to see if the room is filling up with potentially infectious exhalations. The CO2 level lets you estimate if enough fresh outside air is getting in.
Outdoors, CO2 levels are just above 400 parts per million (ppm). A well ventilated room will have around 800 ppm of CO2. Any higher than that and it is a sign the room might need more ventilation.
Last year, researchers in Taiwan reported on the effect of ventilation on a tuberculosis outbreak at Taipei University. Many of the rooms in the school were underventilated and had CO2 levels above 3,000 ppm. When engineers improved air circulation and got CO2 levels under 600 ppm, the outbreak completely stopped. According to the research, the increase in ventilation was responsible for 97 percent of the decrease in transmission.
Since the coronavirus is spread through the air, higher CO2 levels in a room likely mean there is a higher chance of transmission if an infected person is inside. Based on the study above, I recommend trying to keep the CO2 levels below 600 ppm. You can buy good CO2 meters for around $100 online; just make sure that they are accurate to within 50 ppm.
The word on air cleaners
If you are in a room that can’t get enough outside air for dilution, consider an air cleaner, also commonly called air purifiers. These machines remove particles from the air, usually using a filter made of tightly woven fibers. They can capture particles containing bacteria and viruses and can help reduce disease transmission.
The U.S. Environmental Protection Agency says that air cleaners can do this for the coronavirus, but not all air cleaners are equal. Before you go out and buy one, there are few things to keep in mind.
The first thing to consider is how effective an air cleaner’s filter is. Your best option is a cleaner that uses a high-efficiency particulate air (HEPA) filter, as these remove more than 99.97 percent of all particle sizes.
The second thing to consider is how powerful the cleaner is. The bigger the room–or the more people in it–the more air needs to be cleaned. I worked with some colleagues at Harvard to put together a tool to help teachers and schools determine how powerful of an air cleaner you need for different classroom sizes.
The last thing to consider is the validity of the claims made by the company producing the air cleaner.
The Association of Home Appliance Manufacturers certifies air cleaners, so the AHAM Verifide seal is a good place to start. Additionally, the California Air Resources Board has a list of air cleaners that are certified as safe and effective, though not all of them use HEPA filters.
Keep air fresh or get outside
Both the World Health Organization and U.S. Centers for Disease Control and Prevention say that poor ventilation increases the risk of transmitting the coronavirus.
If you are in control of your indoor environment, make sure you are getting enough fresh air from outside circulating into the building. A CO2 monitor can help give you a clue if there is enough ventilation, and if CO2 levels start going up, open some windows and take a break outside. If you can’t get enough fresh air into a room, an air cleaner might be a good idea. If you do get an air cleaner, be aware that they don’t remove CO2, so even though the air might be safer, CO2 levels could still be high in the room.
If you walk into a building and it feels hot, stuffy, and crowded, chances are that there is not enough ventilation. Turn around and leave.
By paying attention to air circulation and filtration, improving them where you can and staying away from places where you can’t, you can add another powerful tool to your anti-coronavirus toolkit.
0 notes