#PGY
Text
I just started a patient on HRT for the first time ever in our residency clinic!!
After ~2.5 years of residency, 1.5 years of building a LGBTQIA+ curriculum, 4 months of advocacy seminars, and a whole lot of barriers, we have finally gotten the okay to start initiating hormone therapy for the purpose of gender affirming care.
This patient is one of two who I had already started the evaluation and informed consent process. We had actually already decided on a plan to start estrogen, but this week the administration approved our official informed consent form so she came in, signed it with my colleague, and got to start estrogen tonight!!
This is a huge milestone for our clinic, residency, and community but also for me, my colleague (who has been a huge champion for all of this change), and of course my patient. I'm honestly a little bummed that I wasn't the one in clinic today to have the visit after doing all the evaluation and informed consent, but the excitement and progress is definitely worth it and I'm thankful for that.
#osteoblr#residency#family medicine#clinic#lgbtqia#pgy-3#medblr#gender affirming care#gender affirming healthcare#estrogen#testosterone#transgender#trans
28 notes
·
View notes
Text
Man. Nothing quite gets me pissed like medical misinformation from residents on tiktok.
#biggest pet peeve of my life.#stop filming shit in the or.#if i catch a pgy doing that its over. youre gone.#no practicing medicine for you.#god i want to scream
13 notes
·
View notes
Text
Residency…
Even my eyebag’s eyebags have eyebags at this point.
#oh the drama#residency#medicine#surgery#eyebags#please#and i’m doing double work right now since my co-res decided to milk the parental leave system#love that (/s)#and right when the new interns started#so they’re going to be on easy street when they come back since the interns will be prepped and ready to go when they come back#i mean eight weeks off…#and they aren’t even the ones who gave birth#and i’m on call as much as the interns are at this point#i didn’t even get a chance to breathe between PGY-1 and PGY-2 i feel like an extended intern right now tbh#and that isn’t right#sorry but all the extra work getting dumped on me isn’t fair#when they come back they better be ready to WORK#sorry if that’s bitchy and insensitive but what about MY well-being?#i needed to rant this out my therapist wasn’t enough i needed tumblr lol#and i did all this while recovering from a leg injury#if this dude gets the chief position over me i am going to lose it#personal#update: thanks for the hugs and hearts guys 💜💜💜💜
10 notes
·
View notes
Text
Lessons as a new attending:
#1: Your nurse will absolutely make or break your outpatient practice. Be exceedingly picky. Knowledge of your specialty is secondary and can be taught. Having initiative, clinical reasoning skills, organizational skills, follow-up and follow-through, and the humility to be taught are paramount. The moment you lose trust in your nurse is the minute you should cut them loose. It’s not going to work. I’m three months in and had to fire my nurse. I felt horrible about it. Now my only regret is not doing it sooner. Everyone except me knew it wasn’t working out after a month. There are some things that cannot be taught or fixed.
#2: NEVER give your email or phone number to a medical sales rep. Just don’t do it. You will regret it because some of them quite literally do not have boundaries or pick up in subtleties.
#3: Similar to intern year, organization is key. Check boxes have made a return to my life. This past weekend was my first weekend call shift as an attending and it was an absolute hot mess where I completely lost track of who I had billed for and who I had not. It’s a mess that my billers are still trying to sort out.
#4: You know more than you think, and you aren’t expected to know everything. Talk to your partners. Most people are more than happy to help.
48 notes
·
View notes
Text
what's new in pdtn land
became a dad last month

had to fight tooth and nail to get 8 weeks of unpaid leave for child care though, because I have < 1 year in service and HR/admin in my hospital system is a fucking disaster. my wife has similar rules about her maternity leave but her admin waived them without any pushback. she works for a different hospital system and gets 12 weeks fully paid. guess who's more likely to retain their physician?
2. had my teaching titles/roles stripped back in January, rather suddenly. I admittedly let myself get into an unhealthy cycle over the winter and wasn't doing a lot of teaching, but I'm surprised they took me off the schedule entirely for a year. I'm not sure how I'm supposed to get better without actually getting reps on service. I talked to the PD about it, who acquiesced but when the new teaching schedule came out I wasn't on it. yet we share the same vision for the program and its residents.
3. moved into a new house to accommodate #1, which unfortunately meant moving out of the city. the housing market is total insanity still, houses were impossible to find without an HOA and even then, flying off the market within 48 hours.
4. given #1 and #2, I have limited prospects on staying at my current job. the pay is good and the day-to-day work on non-teaching is pretty manageable. but it's not what I want out of my career long-term. I'm toying with the idea of going part time or PRN here, and putting that time into being a mercenary. locums pays well and requires fewer hours--there aren't any benefits but since I'm on my wife's plan that doesn't matter to me. so I can use that time to be at home more, and expand on my private practice hybrid concept. the locums gigs also offer me a chance to get a diversity of references instead of being tied to one employer. if I'm not back on teaching with some frequency by next January, I'll probably scale down to PRN by the subsequent summer or walk.
16 notes
·
View notes
Text
One more week and I’m done with residency!
I’ve learned so much, I’m more self assured, a better clinician, better rooted in my knowledge and my morals.
I feel broken.
After a few glasses of wine and the celebrations of graduation, I came home and the tears started flowing. It was overwhelming, the relief that this experience is over. Because there is a poorly defined seldom spoken collective trauma that we as residents go through.
It’s in the impossibly long hours, the massive amounts of clinical knowledge, the fear of making a mistake, in the scorn of colleagues and superiors when we do, and don’t forget about the global pandemic. We push through aday at a time. Counting down until the next vacation, the next day off, until the block ends, the shift is over. We cry in empty patient rooms, in supply closets, in showers, on our kitchen floors, in our cars- If we cry at all. Eventually you get good at seldom feeling, we push all tenderness aside, if we can.
As I finish these most grueling years, I feel splintered. There are other things too; the doll in lace, listening to the agonized cries of a mother losing a child, telling a four year old’s father that he has leukemia, watching a forgotten toddler suffer for weeks in agony that we can’t stifle with medications as the family struggles with code status, the young adults who suffer alone as visitors are forbidden in the height of the pandemic, doing a neurological exam on an infant in a trauma bay only to discover fixed and dilated pupils and learn later that he was shaken...
We all have dozens of stories like this. Most of them pushed aside, shuttered somewhere for later. Hidden.
There are good stories too- the thirty week preemie who went home as a healthy baby, the first words uttered after weeks of therapy following a TBI, bringing a pool into the PICU to grant a final wish, joking with a boy who got a fishhook stuck in his nose, the crayon drawn cards and pictures that decorate my workspace, games of candyland and monopoly in hospital rooms, summer camp for cancer kids, countless hugs from patients and a few from grateful parents as well.
I am so immensely grateful to my mentors, to the kind attendings, to the patients and the families for all that they have taught me. I’m hoping to become a better person and continue to refine by skills as a general pediatrician and pediatric hospitalist as this next phase of life begins. I also plan on being unashamedly selfish and spending time and effort on myself.
It’s going to take a lot healing before I’m well again.
25 notes
·
View notes
Text
Ultimate Sunday Scaries today in which I start my first attending job tomorrow!
Lots of feels. Can’t believe it’s already been three months since I finished residency (can’t believe it’s only been three months since I finished residency). Mostly hoping I don’t get lost in the hospital. Grateful that the first three days is just orientation and I don’t really have to see patients until next week.
12 notes
·
View notes
Text
Sitting at the airport in Greece, attending our mandatory residency program orientation, thinking about how life is going to change so drastically in a few short days. Everything I've worked so hard for: it's within reach. There's so much paperwork, so much to be done, and I feel overwhelmed -- but at the same time, I'm cautiously excited.
18 notes
·
View notes
Text

Enjoy the best products deals on halfpe.com
#https://halfpe.com/products/petgains-pgy-soft-plush-cushion-shark-shape-cave-bed-blue-medium#Join our whatsapp link for more collections#https://whatsapp.com/channel/0029VaNGuLm1iUxfTNlxzK1w
0 notes
Text
eek im also afraid of dogs do they have to show them running towards the camera 🙈 when is park gyuyoung gonna come and help me with my trauma huh
#purple.mp3#this is exactly why i didn't watch this show when it aired#but i can't resist pgy and she's adooooorable in this role#anyway ml and i should share a beer
0 notes
Text
Hi friends! It's been a while... Or is two years more than a while?
Anyway, I've continued to not only survive residency but also grow as a person and physician. Over the past two years, I have found my niche in family medicine moreso than just my OMT and behavioral health focus (which are both still going strong by the way). I have become one of the only providers of gender affirming care in my area and a fierce advocate for the LGBTQIA+ community.
Because of this, I have started to further my learning through a year-long LGBTQIA+ health fellowship seminar series. This program has requested I post a reflection on a blog after each seminar, and since I already have a blog, I figured why not post here and spread the knowledge to the medblr community.
Anyway, I just wanted to make an intro post explaining the posts to come so it's less weird when I start posting very specific/niche blog posts. As I stated before, I am a fierce advocate for the LGBTQIA+ community and I will literally just be posting my homework, so any anti-LGBTQIA+ comments will be deleted and the user will be blocked. I don't have time to debate strangers on the internet as to why human beings should be allowed to exist.
19 notes
·
View notes
Text
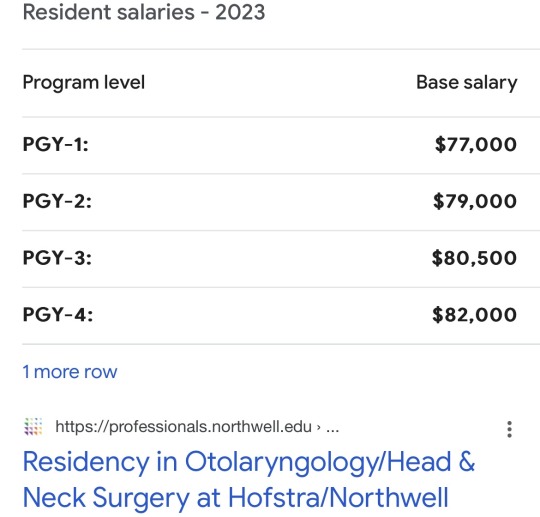
How much ENT surgical residents make in a year
0 notes
Text
i appreciate all those posts about how scientists see the beauty in the things they research, maybe just in a different way than artists and poets or whatever
but i currently am not seeing the beauty in a single thing about research
0 notes
Text
Big Sib, Big Sib!
When I started child neurology, I never expected to gain an older sibling.

View On WordPress
0 notes
Text
Got into an argument with the GI NP about a consult I placed. they said "happy to see the patient but not sure why the consult is needed"
So I explain that the patient's ileus is nonsurgical (passing gas, already seen by surgery) but after his NG tube was removed his presenting symptoms (severe bloating) started rapidly accumulating. Etiology remains unclear. I'd like to blow out his colon and see if that helps reduce the bloating.
She goes on to say that well, surgery said he's still passing gas and he's improving so I'm not sure what else we would offer. We can see him in the office.
I say yes, I know what they said but what I see/hear from the patient is different. I understand if you don't think a full consult is needed but I would like to know your thoughts on doing an aggressive bowel regimen, as it's evident he has quite a bit of stool regardless. A curbside/your off-the-record input is fine.
She then says I don't know if I would do an aggressive bowel regimen, miralax is fine. and mainly, please save inpatient consults for acute inpatient issues. Surgery says he is improving.
...
My headspace: I WILL DESTROY YOU, I WILL COME TO YOUR HOUSE, STEAL YOUR PLANTS, AND PISS ON YOUR DRYWALL.
I take a deep breath.
"I realize that's what surgery said, but he wasn't improving when I saw him yesterday. Though passing gas his symptoms were ramping back up. This was shortly after the NG came out. I was looking for additional guidance, you gave it. I am pretty judicious with my consults coming from a program where I was expected to discuss my rationale over the phone."
Don't you talk down to me, motherfucker. I don't have to chug dongs the way I did for the previous five years.
An hour or so later, I get a message saying she saw the patient and would discuss with the GI attending.
I love that I have the support of my division in pushing back on petty shit like this. I usually just give my chief a heads up in case anything gets back to him.
9 notes
·
View notes
Text
Why does there have to be a rampant surge in RSV, just as I’m getting my feet wet into attendinghood?
Like yes RSV is bread and butter with a (typically) predictable clinical course and well defined treatment algorithm.
But I’d be lying to tell you I’m not already dreading my next call because of all of the midnight and small hour RSV hypoxia admissions. I also had to transfer a kid over five hours away because that was the closest available ICU bed, it’s a mess!
The clinic nurses and my medical assistant were joking about me being a black cloud this morning, because I admitted like three kids to myself last time I was on. No. I have always been a staunchly grey cloud, and I refuse to believe I am a respiratory distress magnet...
Also I have been exposed to so much RSV, influenza, and adenovirus this week I’m amazed I haven’t caught something yet (good job immune system!)
5 notes
·
View notes