#Types of urinary retention
Text
youtube
Urinary Retention: Types, Causes, Diagnosis & Treatment - Expert Insights by Dr. Soumyan Dey
0 notes
Text



From last fall: One of the reddest reds on the landscape, associates with ericaceous heath belts with minimal light competition. So mainly dry sandstone with shallow nutrient poor soils and good drainage or sandstone barrens. Due to slow growth and an acidic weathering effect associated with the bark cortex and the water retention these species also tend to have incredible lichen diversity.
Citheronia regalis horn devil larva are associated as the primary moth that eats these leaves.
Oxydendrum arboreum
Sourwood, or some call it sour bark tree, chewing on the bark and active phloem was once common practice to alleviate the nerve pain associated with toothaches. The leaves themselves are an anti-gas, anti-inflammatory laxative(strong one at that). In some cases a tea can be made of the leaves that also aids in other issues and have been used to treat urinary infections by native people and early settlers to the Appalachian mountains and ilp.
Right now at llanfair permaculture we have an interesting soil dynamic that may be accessible for species like this due to good drainage and high organic comp as well as good lighting, the other thing is that these seeds don't seem to require any specialized treatment to germinate.
https://www.jstor.org/stable/3799771
76 notes
·
View notes
Text
What is Functional Neurological Disorder
What is Functional Neurological Disorder??
Functional Neurological Disorder (FND) describes a Problem with how the brain Receives and sends information to the rest of the body.
It's often helpful to think of your brain as a computer. In someone who has FND, there's no damage to the hardware, or structure, of the brain. It's the software, or program running on the computer, that isn't working properly.
The problems in FND are going on in a level of the brain that you cannot control. It includes symptoms like arm and leg weakness and seizures. Other symptoms like fatigue or pain are not directly caused by FND but are often found alongside it.
Symptoms of FND
FND can have many symptoms that can vary from person to person. Some people may have few symptoms, and some people may have many.
Functional Limb Weakness
Functional Seizures
Functional Tremor
Functional Dystonia
Functional Gait Disorder
Functional Facial Spasm
Functional Tics
Functional Jerks and Twitches
Functional Drop Attacks
Functional Sensory Symptoms
Functional Cognitive Symptoms
Functional Speech and Swallowing Difficulties
Persistent Postural Perceptual Dizziness (PPPD)
Functional Visual Symptoms
Dissociative Symptoms
Common associated symptoms or conditions??
There are other symptoms or conditions that are commonly associated with FND. These include:
· Chronic Pain, Including Fibromyalgia, Back and Neck Pain, And Complex Regional Pain Syndrome
· Persistent Fatigue
· Sleep Problems including Insomnia (Not sleeping Enough) and Hypersomnia (Sleeping too much)
· Migraines and other Types of Headaches and Facial Pain
· Irritable Bowel Syndrome and other Problems with the Function of your Stomach and Bowel
· Anxiety and Panic Attacks
· Depression
· Post-Traumatic Stress Disorder
· Chronic Urinary Retention
· Dysfunctional Breathing
What causes FND?
· We know that the symptoms of FND happen because there's a problem with how the brain is sending and receiving messages to itself and other parts of the body. Using research tools, scientists can see that certain circuits in the brain are not working properly in people with FND.
· However, there's still a lot of research to be done to understand how and why FND happens.
Why does FND happen?
FND can happen for a wide range of reasons. There's often more than one reason, and the reasons can vary hugely from person to person.
Some of the reasons why the brain stops working properly in FND include:
the brain trying to get rid of a painful sensation.
a migraine or other neurological symptom
the brain shutting down a part or all of the body in response to a situation it thinks is threatening
In some people, stressful events in the past or present can be relevant to FND. In others, stress is not relevant.
The risk of developing FND increases if you have another neurological condition.
Diagnosing FND
When diagnosing FND, your healthcare provider will carry out an assessment to see if there are typical clinical features of FND.
Your healthcare provider may still choose to test for other diseases and conditions before diagnosing FND. This is because many conditions share the same symptoms and, in around a quarter of cases, FND is present alongside another neurological condition. Someone can have both FND and conditions like sciatica, carpal tunnel syndrome, epilepsy, or multiple sclerosis (MS).
The diagnosis of FND, however, should be given because you have the clinical features of FND. It shouldn't be given just because there's no evidence of other conditions or illnesses.
Because the symptoms of FND are not always there, your healthcare provider may ask you to video your symptoms when they are bad so they can see what's happening to you.
Treatments
FND is a variable condition. Some people have quite short-lived symptoms. Others can have them for many years.
There are treatments available that can manage and improve FND. These treatments are all forms of rehabilitation therapy, which aims to improve your ability to carry out every day activities. Many of these treatments are designed to "retrain the brain". Some people with FND benefit a lot from treatment and may go into remission. Other people continue to have FND symptoms despite treatment.
Treatments are:
· Physiotherapy
· Occupational Therapy
· Psychological Therapy
· Speech, Language and Swallowing Therapy
· Medication (Antidepressants, Neuropathic Painkillers)
Who is at risk of FND?
No single process has been identified as being sufficient to explain the onset of FND. Several interacting factors biologically, psychologically, and socially can cause vulnerabilities, triggers and maintaining factors that contribute to FND.
Why is this happening to me?
There are usually several underlying biopsychosocial factors which play a role in the development of FND. Some of these factors contribute to making the brain vulnerable, trigger FND episodes and prevent people from getting better. Injury and pain can be a common trigger. Anxiety, depression, and traumatic life experiences can also contribute to making brains vulnerable to FND.
4 notes
·
View notes
Text
Can Hernia Surgery Cause Prostate Problems?

Hernia surgery is a common procedure, but many people worry about potential complications, particularly whether it can cause prostate problems. Understanding the relationship between hernia surgery in Jabalpur and prostate health requires a look at the anatomy and the nature of the surgeries involved.
Understanding Hernias and Prostate Health:
A hernia occurs when an internal part of the body pushes through a weakness in the muscle or surrounding tissue wall. Common types include inguinal (groin) hernias, which are most relevant when discussing proximity to the prostate.
The prostate is a small gland located just below the bladder in men and surrounds part of the urethra. It plays a crucial role in male reproductive health by producing seminal fluid. Because of its location, there is concern that procedures in the nearby inguinal region might affect it.
The Nature of Hernia Surgery:
Hernia repair, especially inguinal hernia repair, involves returning the displaced tissue to its proper position and reinforcing the muscle wall, often with mesh. There are two main types of hernia surgery:
1. Open Surgery: A single incision is made near the hernia site.
2. Laparoscopic hernia surgery in Jabalpur: Several small incisions are made for a camera and surgical instruments.
Both methods aim to minimize trauma to surrounding tissues, but the proximity of the inguinal area to the prostate raises valid concerns.
Potential Risks and Complications:
While hernia surgery in Jabalpur is generally safe, potential complications can arise, though prostate problems are not typically among them. Possible complications include:
• Infection: Post-operative infections can occur but are generally related to the surgical site rather than the prostate.
• Nerve Damage: This can cause pain or numbness in the groin area, but it usually doesn’t affect the prostate directly.
• Bladder and Urinary Issues: Rarely, patients might experience urinary retention or difficulty, which can be mistaken for prostate problems. However, these are typically short-term and resolve with time.
Prostate Problems and Hernia Surgery:
There is no direct evidence that hernia surgery in Jabalpur causes prostate problems. However, certain symptoms can overlap or be mistaken for each other. For instance, urinary difficulties post-surgery might be confused with prostate issues.
Pre-existing Conditions: Men with pre-existing prostate conditions, such as benign prostatic hyperplasia (BPH), might notice increased symptoms post-surgery due to the stress of surgery and recovery. This is not because the surgery caused prostate issues but because the body is dealing with multiple stresses simultaneously.
Mitigating Risks:
To minimize potential complications:
• Discuss Thoroughly: Patients should discuss their full medical history with their surgeon, including any prostate issues.
• Choose Experienced Surgeons: Opt for a hernia surgeon in Jabalpur with extensive experience in hernia repair.
• Follow Post-Op Care: Adhere strictly to post-operative care instructions to avoid complications.
While hernia operation in Jabalpur, especially inguinal hernia repair, is close to the prostate, there is no direct evidence linking it to causing prostate problems. The symptoms that might arise post-surgery are usually temporary and related to the body's overall response to surgery rather than the prostate itself. As always, discussing concerns with the best hernia surgeon in Jabalpur provider is crucial for personalized advice and peace of mind.
#laparoscopicherniaspecialistinjabalpur#herniaoperationinjabalpur#bestherniasurgeoninjabalpur#laparoscopicherniasurgeryinjabalpur
0 notes
Text
Prostate Cancer Treatment in India for Foreign Patients
Prostate cancer is one of the most common cancers in men. It develops in the prostate gland. It is a small walnut-shaped gland that produces seminal fluid. The prostate is placed under the bladder. It is a blank hollow organ that manages to store urine. It is positioned in front of the rectum which is the end of the intestines. Prostate cancer begins when uncontrollable cells grow in the prostate gland that makes a lump or a tumor.
Prostate Cancer Treatment in India
Prostate cancer is a very serious disease. It is treatable in the early stages before cancer spreads to the prostate gland. Some of the symptoms of prostate cancer as like; Trouble urinating, the urge to urinate frequently at night, blood in the semen, Pain or burning during urination, reduced force in the stream of urine, pain when sitting caused by an enlarged prostate, losing weight without trying, blood in the urine, etc. There are many types of Prostate cancer. Types are the following;
Adenocarcinoma. It is the most common type of prostate cancer.
Small Cell Carcinomas
Transitional Cell Carcinomas
Neuroendocrine Tumors
Sarcomas. These are some rare types of prostate cancer.
Prostate cancer treatment depends on the stage of cancer in the prostate gland. The size of the tumor, patient condition & different therapies are given as required. Some of the prostate cancer treatment options are as particle therapy, radiation therapy, laparoscopic radical prostatectomy, radiosurgery, radical retropubic prostatectomy, chemotherapy, hormone & urinary retention medications, etc.
Prostate Cancer Treatment Cost in India
Prostate cancer treatment cost in India is based on various factors such as techniques, doctor’s expertise, equipment, patient medical conditions, city, and hospitals. This treatment starts from INR 1Lks up to 4.5Lks.
Best Prostate Cancer Treatment Hospitals in India
India has many best quality hospitals for prostate cancer treatment that offer excellent cancer care. These hospitals are very well known for their best care, equipment, medical oncology, and other specialists.
Fortis Memorial Research Institute (New Delhi)
Narayana Superspeciality Hospital (Gurgaon)
Indraprastha Apollo Hospitals (New Delhi)
Medanta- The Medicity (Gurgaon)
Kokilaben Dhirubhai Ambani Hospital (Mumbai)
Tata Memorial Hospital (Mumbai)
Top Prostate Cancer Treatment Doctors in India
There are many best oncology surgeons in India for treating against prostate cancer treatment. They have many years of knowledge, experience & expertise. Some of the doctor’s names are given below:
Dr. Keshavamurthy Mohan (Uro-oncologist)
Prof. Dr. Raj Nagarkar (Surgical oncologist)
Dr. Madhav Sanzgiri (Urology/Genito-urinary Surgery)
Dr. Kapil Kumar (Director& HOD of Surgical Oncology)
Dr. Lakshman Bellamkonda (Urologist, Andrologist & transplant surgeon)
Dr. Vadhiraja B.M (HOD & Consultant Radiation Oncologist)
Al Afiya Medi Tour is a leading medical tourism company in India. We offer medical tourism services such as finding the right doctor, the right hospital, and cost estimation etc. Some of the main countries are Bangladesh, South Africa, Egypt, Uganda, Zambia, Sudan, Dubai, Namibia, Iraq, Kenya, Saudi Arabia, Ethiopia, Nigeria, and so on. We provide free medical assistance for TURP surgery cost, lung cancer treatment, cancer treatment cost, lung transplant, liver transplant cost, top knee replacement surgeons, knee replacement surgery cost, top shoulder replacement surgeons, etc.
Source: https://alafiyameditour1.blogspot.com/2024/05/prostate-cancer-treatment-in-india-for_9.html
0 notes
Text
What Are Common Urological Conditions in Seniors?
Navigating Urological Health in Older Adults
As individuals journey through the golden years of life, prioritizing urological health becomes increasingly essential. Aging brings about changes in the body, and the urinary tract system and male reproductive organs are not exempt from this process. Understanding the common urological conditions that affect older adults empowers both individuals and caregivers to take proactive steps towards maintaining optimal health and well-being. Exploring the services of the best urologists in Jamaica can provide invaluable support and guidance in managing and treating these conditions effectively.
Prostate Enlargement (BPH):
One of the most prevalent urological issues faced by older men is benign prostatic hyperplasia (BPH). This condition involves the non-cancerous enlargement of the prostate gland, leading to urinary symptoms such as frequent urination, urgency, weak urine stream, and incomplete emptying of the bladder. While BPH is not life-threatening, its symptoms can significantly impact quality of life. Treatment options range from medications to surgical interventions, tailored to the severity of symptoms and individual preferences.
Urinary Incontinence:
Urinary incontinence, the involuntary leakage of urine, becomes more common with age, particularly among older women. This condition can manifest as stress incontinence (leakage with physical activity), urge incontinence (sudden, intense urge to urinate), or overflow incontinence (inability to empty the bladder completely). Effective management strategies include pelvic floor exercises, behavioral therapies, medications, and in some cases, surgical procedures.
Urinary Retention:
Older adults may also experience urinary retention, the inability to empty the bladder fully. This can result from various factors, including BPH, nerve damage, medications, or structural abnormalities. Chronic urinary retention increases the risk of urinary tract infections (UTIs) and bladder damage. Treatment often involves catheterization to drain the bladder and addressing the underlying cause.
Urinary Tract Infections (UTIs):
UTIs are common among older adults and can present with vague symptoms such as confusion, agitation, or generalized weakness, rather than the typical urinary symptoms seen in younger individuals. UTIs in older adults may be associated with factors such as bladder dysfunction, urinary catheterization, or underlying medical conditions. Prompt diagnosis and appropriate antibiotic therapy are crucial to prevent complications such as urosepsis.
Kidney Stones:
While kidney stones can occur at any age, their incidence tends to increase with age. Older adults may be more prone to dehydration, reduced kidney function, and changes in urinary composition, predisposing them to stone formation. Management of kidney stones may involve pain management, hydration, and in some cases, procedures such as lithotripsy or surgical intervention to remove larger stones.
Urological Cancers:
Aging is a significant risk factor for urological cancers, including prostate cancer, bladder cancer, and kidney cancer. Regular screenings and early detection are paramount for favourable outcomes. Treatment options vary depending on the type and stage of cancer but may include surgery, radiation therapy, chemotherapy, or targeted therapies. In conclusion, navigating urological health in older adults requires a multifaceted approach encompassing preventive measures, timely screenings, and tailored interventions. By prioritizing urological wellness and addressing any emerging concerns promptly, older adults can enjoy a fulfilling and vibrant quality of life in their later years.
#online urologists consultation#best urologists in jamaica#best urologists online consultation#diabetes
0 notes
Text
0 notes
Text
What is Urinary Incontinence?
Urinary incontinence is a condition characterized by the unintentional loss of urine, leading to leakage from the bladder. It can vary in severity, from occasionally leaking urine when coughing or sneezing to having a sudden, strong urge to urinate and being unable to reach the toilet in time.
There are several types of urinary incontinence:
Stress incontinence: This occurs when physical movement or activity puts pressure on the bladder, causing leakage. It's commonly associated with activities such as coughing, sneezing, laughing, or exercising. It's often due to weakened pelvic floor muscles, which can be caused by factors such as childbirth, pregnancy, aging, or obesity.
Urge incontinence: Also known as overactive bladder, this type involves a sudden and intense urge to urinate, followed by an involuntary loss of urine. It can be caused by overactivity of the bladder muscles or neurological conditions that affect bladder control.
Overflow incontinence: This occurs when the bladder doesn't empty completely, causing it to overflow and leak urine. It can be caused by conditions that obstruct the flow of urine, such as an enlarged prostate in men or urinary retention.
Functional incontinence: This type occurs when physical or cognitive impairments prevent a person from reaching the toilet in time, even though the bladder function itself may be normal. It can be caused by conditions such as arthritis, dementia, or mobility issues.
Mixed incontinence: Some individuals may experience a combination of different types of urinary incontinence.
Treatment for urinary incontinence depends on the underlying cause and severity of symptoms. It may include lifestyle changes (such as bladder training, pelvic floor exercises, dietary modifications), medications, medical devices (such as pessaries), or surgery in some cases. It's essential for individuals experiencing urinary incontinence to consult a healthcare professional for proper diagnosis and treatment.
0 notes
Text
Vesicoureteric Reflux

What Is Vesicoureteric Reflux?
Vesicoureteric reflux is the condition in which the urine flows back from the bladder to the ureter. This condition is also known as vesicoureteral reflux. There is a progressive flow of urine from the kidney to the bladder through ureters. The uni-directional flow of urine from kidney to urinary bladder is ensured by the flaps situated between the ureter and urinary bladder (vesico-ureteric junction). This condition is commonly diagnosed in infants and young children.
In this condition, the urine may flow back form one or both the ureters. Based on the severity of symptoms and extent of disease, the urologist generally grades this condition from Grade 1 to Grade 5 with Grade 1 mildest form and Grade 5, a severe form. Fortunately, most children recover from this condition as they get older. The vesicoureteric reflux is divided into primary and secondary.
What Are The Causes Of Vesicoureteric Reflux?
The causes of vesicoureteric reflux are different for primary vesicoureteric reflux and secondary vesicoureteric reflux.
Primary vesicoureteric reflux: In this type of vesicoureteric reflux, the valve between the ureter and urinary bladder does not work properly. This results in backflow of urine. This is the most common cause of this condition in children. However, as the age increases, the ureter and bladder become mature, and the valve regains functioning. If the urine flows back from only one ureter, it is termed as vesicoureteric unilateral reflux, and if both the ureters are involved in the backflow of urine, the condition is termed as vesicoureteric bilateral reflux.
Secondary vesicoureteric reflux:There are various causes of secondary vesicoureteric reflux. In some cases, there is a blockage of urine due to abnormal tissue fold in the urethra (posterior urethral valve) and in conditions like neurogenic bladder . Obstruction in bladder outlet prevents the voiding of complete urine from the bladder. In cases of neurogenic bladder, the child may also have damaged nerves that control contraction and relaxation of the bladder resulting in reflux.
What Are The Symptoms Of Vesicoureteric Reflux?
Symptoms of vesicoureteric reflux depend upon the severity and complications of the disease. The patients with vesicoureteric reflux may experience the following symptoms:
Recurrent urinary tract infection
The excessive urge to urinate
Fever
Cloudy urine
Frequent urination
Pain during urination
Bedwetting
Urinary retention
Loss of appetite
Irritability
Presence of protein in the urine
High blood pressure
How Vesicoureteric Reflux Is Diagnosed?
The vesicoureteric reflux can be diagnosed both before and after birth. Before birth, the condition can be diagnosed through the ultrasound, which reveals swelling in kidneys (hydronephrosis). Various techniques that are used to diagnose the condition are:
Laboratory workup: Many children have the recurrent urinary infection as the primary symptom of this condition. Thus, urinalysis is done to determine the presence of urinary tract infection.
Imaging techniques: Kidney, bladder, and ureter ultrasound is done to determine the presence of any structural abnormalities.
Micturating cystourethrogram (MCUG):It is a specialized X-ray of the urinary tract. During this procedure, the doctor places a small catheter in the bladder and fill the bladder with a special dye. The X-ray is taken before and after urination. The doctor, by evaluating the flow of dye, determines if the urine flows back in the ureter.
Nuclear scan:During this procedure, the doctor uses a radioisotope. The detector detects the isotope and determines any damages in kidney.
How Vesicoureteric Reflux Is Treated?
The following are the management options available for vesicoureteric reflux:
Medications: Low dose of antibiotics is provided to the children to prevent urinary tract infection. However, regular monitoring is required to determine the presence of urinary tract infection. Further, doctors should implement imagining techniques to monitor the progression of the disease. Besides various precautions are to be taken like avoiding constipation, perineal hygine and frequent voiding to reduce the risk of infection.
Surgery: Various types of surgeries are available for treating vesicoureteric reflux. Open surgery is done to repair the larger problem in the urinary tract and involves anesthesia. Robotic-and laparoscopic surgery is done to repair the valve between the ureter and urinary bladder. Endoscopic surgery is performed to strengthen the valve with the use of a bulking agent. Ureteric reimplantation is surgery in which the doctor disconnects the ureter and urinary bladder and reattaches them at an angle to create a valve.
What Are The Preventive Measures For Vesicoureteric Reflux?
Although there are no measures to prevent the vesicoureteric reflux, certain measures may improve the health of the urinary tract. These are:
Regular urination and cleaning from front to back.
Drinking enough fluids.
Eat plenty of fiber-rich food to avoid constipation.
Change the diaper frequently or as soon as it gets dirty.
Get proper treatment for urinary and fecal incontinence.
What Is The Prognosis Of Vesicoureteric Reflux?
Most children with this condition recover on their own. Surgery has a high rate of success, with a 97%-99% positive outcome. Early diagnosis and monitoring of the condition reduces complications.
#Vesicoureteral Reflux Treatment In India#causes of Vesicoureteral Reflux#symptoms of Vesicoureteral Reflux
0 notes
Text
Everything You Need to Know About Kidney Failure

Kidney failure, a serious health condition, affects millions globally. It is also known as renal failure and is a serious medical condition that can have life-altering implications. This blog will provide an in-depth understanding of its types, symptoms, early signs, how do you know kidney problems, and treatment options. Let’s explore this critical issue together.
Understanding kidney failure
Before we explore kidney failure specifics, it’s imperative to understand the role of the kidneys in our bodies. The kidneys filter out waste products, excess nutrients, and fluids from the bloodstream. These are then excreted from the body in urine. When the kidneys cannot perform this function effectively, kidney failure results.
It occurs when the kidneys, two bean-shaped organs located on either side of the spine, lose their ability to filter out waste and excess fluids from the blood. If this occurs, harmful waste can build up in the body, resulting in health problems.
Types of kidney failure
Kidney failure can be classified into two main types:
Acute kidney injury (AKI).
AKI is characterized by a rapid loss of kidney function over a short period — usually within a few hours or days. This type of kidney failure is often reversible if treated promptly and appropriately. Causes of AKI can include severe infections, certain medications, or a blockage in the urinary tract.
Chronic kidney disease (CKD).
CKD is a long-term condition in which the kidneys gradually lose their ability to function. Unlike AKI, CKD damage is often permanent and can lead to end-stage renal disease (ESRD), where dialysis or a kidney transplant is necessary to sustain life. CKD causes include high blood pressure and diabetes.
The symptoms of kidney failure
A variety of conditions can cause kidney failure symptoms, which vary greatly from person to person. Among them are:
General fatigue and illness
Confused or having difficulty concentrating
Weight loss and loss of appetite
The problem of insomnia and other sleep disorders
An increase in swelling in the legs, ankles, and feet as a result of fluid retention
Itching and dry skin that persists
Breathing difficulties
If fluid builds up around the heart lining, it can cause chest pain
Signs of kidney failure at an early stage
Changes in urination: This can include an increase or decrease in frequency, the presence of blood in the urine, or a change in the color or consistency of the urine.
Swelling in the legs, ankles, and feet: This is caused by the kidneys’ inability to remove excess fluid from the body.
High blood pressure: The kidneys regulate blood pressure. Damage to the kidneys can result in high blood pressure, which in turn can cause further damage to the kidneys.
Fatigue and weakness: Healthy kidneys produce a hormone called erythropoietin, which signals the body to make red blood cells. When the kidneys are damaged, they may not make enough of this hormone. This may lead to a decrease in red blood cells and result in fatigue and weakness.
Loss of appetite: This can be due to a build-up of toxins in the body that are normally removed by the kidneys.
Kidney Failure: Urine color
One of the earliest and most noticeable signs of kidney failure is changes in the color and consistency of urine. Healthy urine is pale yellow and clear. In kidney failure, the urine may become dark yellow, brown, or even red if blood is present. It may also appear foamy or bubbly due to excess protein.
Chronic kidney disease stages
Chronic kidney disease progresses through five stages, each representing a different kidney function level. These stages are determined by the glomerular filtration rate (GFR), which measures how well the kidneys filter waste from the blood.
Stage 1: Kidney damage with a normal or high GFR (90 or above). Kidney function is considered normal, but kidney damage has been detected.
Stage 2: Kidney damage with mildly decreased GFR (60 to 89). At this stage, some minor loss of kidney function has occurred.
Stage 3: Moderately decreased GFR (30 to 59). This stage indicates moderate to severe kidney damage.
Stage 4: Severely decreased GFR (15 to 29). Kidney function has declined to the point where kidney disease complications are likely to occur.
Stage 5: Kidney failure, also known as end-stage renal disease (ESRD), with a GFR less than 15. At this stage, dialysis or kidney transplants are necessary to sustain life.
Treatment Options for Kidney Failure
Kidney failure treatment depends on the cause, the individual’s overall health, and the severity of the disease. Treatment options include:
Lifestyle changes: This can include dietary modifications, regular exercise, and quitting smoking.
Medications: These can help manage symptoms and slow disease progression.
Dialysis: This treatment filters and purifies the blood using a machine. This helps to keep your body in balance when the kidneys can’t work.
Kidney transplant: This involves replacing the diseased kidney with a healthy one from a donor.
Conclusion
Kidney failure is a serious medical condition that requires prompt attention and treatment. If you or a loved one are experiencing any symptoms or signs of kidney problems, it’s imperative to seek medical help right away. With early detection and appropriate treatments, you should consult the Best Urologist In Jaipur. Dr Sandeep Nunia is the best Urology doctor in Jaipur. He has years of experience and is the highest-ranking Urologist in Jaipur for treating ailments such as Laparoscopic treatment, Female Urology, Sexology treatment, Uro Oncology, and Kidney stone treatment.
0 notes
Text
All facts about Benign Prostatic Hyperplasia/Enlargement (BPH/BPE), its diagnosis and available treatments
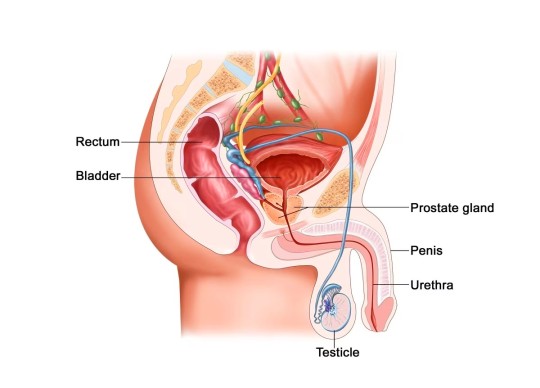
What is prostate gland?
• A prostate gland is an accessory gland of male reproductive system that wraps around the male urethra near the bladder.
• Prostate gland developed at age of 12 years, and it starts growing in middle age.
• The prostate surrounds the urethra, the tube that carries urine from the bladder through the penis and outside the body.
• Prostate gland contains crucial enzyme, 5-alpha-reductace which converts the hormones testosterone in the body to DHT.
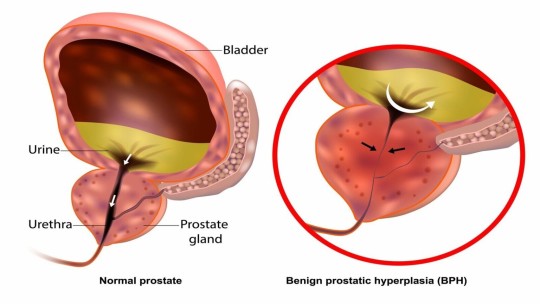
What is Benign prostatic hyperplasia/enlargement (BPH/BPE)?
• BPH/BPE is a condition that occurs when the prostate gland enlarges, potentially slowing or blocking the urinary stream.
• Other names for benign prostatic hyperplasia include benign prostatic hypertrophy and an enlarged prostate.
• The prostate normally enlarges to some degree in all men with advancing age, although not all men require treatment.
• As the prostate gets bigger, it may press on the urethra and cause the flow of urine to be slower and less forceful.
• "Benign" means the enlargement isn't caused by cancer or infection.
• "Hyperplasia" means enlargement.
What are symptoms of BPH?
The symptoms of BPH can likely begin after an age between 40 to 50 years and only in men. The most common symptoms of BPH include:
• Frequent urination (able to hold less than 2 hours)
• Getting up in the night for urination (Nocturia)
• Sudden desire to pass urine (Urgency) or leakage of urine (Urgency incontinence)
• A hesitant, interrupted, or weak stream of urine
• Failure to pass urine (urinary retention)
• Dribbling of urine
• Incomplete emptying of the bladder
• Blood in Urine
• Frequent urinary tract infection
• Straining during urination
How to diagnose BPH and types of investigations required?
To know if BPH or any another problem is causing symptoms, a urologist will ask you questions, perform an examination and will order few tests as below:
• Rectal examination – Your urologist will need to perform a rectal examination to feel the size and shape of the prostate gland.
• Urinalysis – You might be asked for a urine sample to see if you have a urinary tract infection, diabetes, or certain kidney disorder.
• Blood tests – A blood test to check the prostate-specific antigen (PSA) level is often recommended.
• Ultrasound test – A USG test to know the size of prostate, thickness of bladder and structure of kidneys and post void residual urine.
• Uroflowmetry Test – This is a special kind of test to know how much prostate gland is obstructing the urethra.

Mention role of Prostate specific antigen (PSA) in evaluation?
• PSA, or prostate-specific antigen, plays a role as one of the diagnostic markers though it is non-specific.
• Elevated PSA levels may indicate BPH or Prostate gland infection or Prostate cancer and needs to be evaluated further.
• Regular PSA screenings can aid in monitoring prostate health and detecting potential issues like prostate cancer in their early stages.
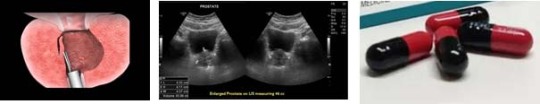
What are the treatments available for BPH?
• Watchful waiting – If symptoms are mild and not bothersome, then regular monitoring is what all is needed and don't need the treatment right away.
• Medicines – There are 2 types of medicine commonly used to treat BPH. One type relaxes the muscles that surround the urethra, and another reduces the size of prostate.
• Surgery – There are several ways to treat BPH with surgery. They can involve removing obstructing prostate and making the urethra wider so that more urine can flow through easily.
Explain LASER surgery of prostate?
• It is also known as Holmium LASER enucleation of prostate (HoLEP)/ Thulium fibre LASER enucleation of prostate (ThuLEP)?
• There are different types of laser prostate surgeries, but they all involve the use of laser energy to remove or vaporize excess prostate tissue that is causing urinary issues.
• Best approach is LASER enucleation, which involves removing the inner part of the prostate to alleviate urinary symptoms.
• Laser prostate surgery is often considered as a minimally invasive option compared to traditional surgical methods, and it may result in less bleeding and a faster recovery.
How is LASER prostate surgery (HoLEP/ThuLEP) performed?
• LASER prostate surgery is performed by endoscopy method, that means a tiny camera will insert in urethra along with an energy source used which is a LASER fiber.
• It doesn’t involve any surgical cut over the body and performed through urethra.
Mention Post operative care after LASER surgery of prostate.
• Try to avoid constipation. Eat foods that have a lot of fiber.
• Drink plenty of water, especially if your urine looks red or you pass small blood clots. It is normal for your urine to have a small amount of blood in it right after surgery.
• Avoid lifting weighted things for some time.
• Avoid smoking and alcohol intake.
• Increase your activity slowly – Start with short walks around your home and walk a little more each day.
• Take prescribed medication as advised.

1 note
·
View note
Text
Urinary Catheters: An Essential Medical Device

Urinary catheters are thin tube-like medical devices that are inserted into the bladder through the urethra to drain urine from the bladder. These catheters play a vital role in healthcare, especially for patients dealing with urinary problems or undergoing certain medical procedures. This article explores various aspects of urinary catheters, including their usage, types, insertion procedures and safety considerations.
What are Urinary Catheters Used For?
Urinary catheters have several important clinical applications:
- Draining urine during and after surgery: Catheters are commonly used during surgical procedures involving the bladder, urethra or surrounding areas to empty the bladder and prevent urine accumulation. They are also used post-operatively until the patient regains bladder control.
- Managing urinary retention: Some medical conditions like enlarged prostate can cause urinary retention where the bladder cannot empty itself fully. Catheters assist in complete drainage in such cases.
- Monitoring urine output: For patients in ICU or those undergoing certain treatments, catheters help doctors and nurses closely monitor urine volume to assess kidney function and fluid status.
- Pain management: For patients with urinary tract infections or other painful conditions, catheters provide comfort by preventing uncomfortable bladder filling until the underlying issue is addressed.
With such diverse and essential uses, urinary catheters remain vitally important for supportive care in various clinical settings.
- Keeping the catheter tubing free from kinks or loops which can block flow.
- Regularly inflating and securing Foley balloons to their intended size.
- Changing the collection bag regularly or as needed to avoid backflow.
- Monitoring for symptoms like fever, pain or cloudy urine which could indicate an infection.
With proper insertion, care and routine checks by healthcare workers, urinary catheters when absolutely needed can help patients comfortably while minimizing risks to their well-being.
Alternative to Catheterization
While catheters offer major clinical benefits, they are also associated with certain risks. As such, alternate options are preferred wherever feasible:
- Behavioral techniques like scheduled toileting, pelvic floor exercises and prompted voiding help prevent need for long-term catheters.
- In select patients, alpha-blockers or 5-alpha-reductase inhibitors can help reduce prostate size and relive urinary retention stemming from an enlarged prostate.
- Percutaneous suprapubic catheter avoids urethral insertion and associated problems but still ensures bladder drainage if needed long-term.
- For end-of-life care, external collection devices or absorbing pads are better quality-of-life options compared to invasive indwelling catheters.
With continued advancements, minimally invasive procedures like urethral stents, bulking agents and nerve stimulation are also reducing overdependence on urinary catheters in suitable clinical contexts.
0 notes
Text
Comprehensive Catheterization Training: Navigating the Essentials for Healthcare Professionals
Catheterization is a crucial medical procedure that requires precision and expertise. Training healthcare professionals in this skill is essential to ensure patient comfort, safety, and the prevention of complications. Here's a comprehensive guide to catheterization training:
1. Understanding Catheterization:
Begin with a thorough understanding of the anatomy and physiology related to catheterization. Explore the different types of catheters, their uses, and the specific patient populations for whom catheterization may be necessary.
2. Infection Control Measures:
Emphasize the importance of stringent infection control practices. Proper hand hygiene, aseptic techniques, and the use of sterile equipment are critical aspects of catheterization training to prevent infections.
3. Patient Communication and Consent:
Train healthcare professionals in effective communication with patients. Obtaining informed consent is crucial, and practitioners should be adept at explaining the procedure, addressing patient concerns, and respecting their dignity and privacy.
4. Equipment Familiarization:
Ensure thorough familiarity with catheterization equipment. This includes understanding the various types of catheters, drainage bags, lubricants, and securing devices. Training should cover proper handling and disposal of these materials.
5. Procedure Simulation:
Incorporate hands-on simulation exercises using anatomical models or virtual reality technology. Allow healthcare professionals to practice the catheterization procedure in a controlled environment, providing a safe space for skill development.
6. Complication Management:
Educate practitioners on potential complications associated with catheterization, such as infection, blockages, or discomfort. Training should include techniques for recognizing and addressing these issues promptly.
7. Urinary System Assessment:
Train healthcare professionals to conduct a comprehensive assessment of the urinary system. This includes understanding indications for catheterization, recognizing signs of urinary retention, and determining the appropriate catheter size and type.
8. Documentation Practices:
Emphasize the importance of accurate and timely documentation. Healthcare professionals should be trained to record relevant patient information, details of the catheterization procedure, and any observations or complications.
9. Cultural Competency:
Recognize the cultural and individual variations in patient responses to catheterization. Training should address sensitivity to diverse cultural practices and beliefs related to personal care and bodily functions.
10. Continued Professional Development:
Catheterization training should not be a one-time event. Encourage healthcare professionals to engage in ongoing education, stay updated on best practices, and participate in refresher courses to maintain proficiency and stay abreast of advancements in catheterization technology and procedures.
By incorporating these elements into catheterization training programs, healthcare professionals can develop the necessary skills, knowledge, and attitudes to perform catheterization safely and effectively, ensuring the best possible outcomes for patients.
0 notes
Text
Urinary Tract Infection
A urinary tract infection (UTI) is an infection that affects any part of the urinary system, which includes the kidneys, bladder, ureters (tubes that connect the kidneys to the bladder), and the urethra (the tube through which urine exits the body). UTIs are a common medical issue, with the majority of cases involving the lower urinary tract (bladder and urethra) and referred to as cystitis. More severe infections that reach the kidneys are known as pyelonephritis.
Urinary tract infection, commonly called UTI, is a bacterial infection that affects the urinary system. It is a common condition affecting millions worldwide, particularly women. UTI is caused when bacteria, usually from the digestive tract, enter the urethra and infect the urinary tract.
The immune system plays a crucial role in the body’s ability to fight off UTI. The immune system is responsible for protecting the body from harmful bacteria, viruses, and other pathogens that can cause infections. When bacteria enter the urinary tract and cause an infection, the immune system responds by sending white blood cells to fight off the bacteria. The white blood cells target the bacteria and release chemicals that help to destroy them.
However, sometimes the immune system cannot fight off the bacteria on its own, especially if the person has a weakened immune system due to illness or medication. In such cases, antibiotics may be required to treat the infection. Antibiotics work by killing or stopping the growth of bacteria, thereby allowing the immune system to take over and clear the infection.
Here are some of the common causes of UTIs:
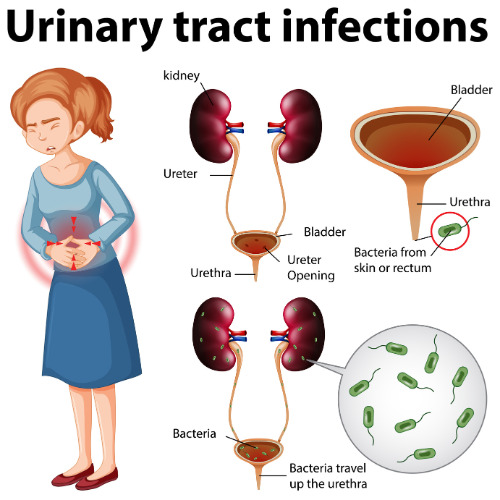
Sexual Activity: Sexual intercourse can introduce bacteria into the urethra, increasing the risk of UTIs. This is sometimes referred to as “honeymoon cystitis.”
Anatomy: Certain anatomical factors, such as a shorter urethra in women, make it easier for bacteria to enter the urinary tract, making women more susceptible to UTIs.
Urinary Retention: Incomplete emptying of the bladder can leave residual urine, creating a conducive environment for bacterial growth.
Urinary Catheters: People who require urinary catheters are at a higher risk of UTIs because the catheter can introduce bacteria directly into the urinary tract.
Diaphragm and Spermicides: The use of diaphragms for contraception, as well as certain spermicides, may increase the risk of UTIs in some women.
Dehydration: Insufficient fluid intake can lead to concentrated urine, which can irritate the urinary tract and increase the risk of infection.
Hormonal Changes: Hormonal changes, such as those occurring during pregnancy and menopause, can affect the urinary tract’s natural defenses, making women more vulnerable to UTIs.
Immune System Compromises: Conditions or medications that weaken the immune system, such as diabetes or immune suppressive drugs, can increase susceptibility to infections, including UTIs.
Obstruction: Anything that obstructs or hinders the flow of urine, such as kidney stones or an enlarged prostate in men, can lead to UTIs.
Sexually Transmitted Infections: Certain sexually transmitted infections (STIs) can cause urethritis, an infection of the urethra, which is considered a type of lower UTI.
Symptoms:
Painful or burning urination
Cloudy or bloody urine
Strong-smelling urine
Pelvic pain
And sometimes a low-grade fever
Diagnosis:
UTIs are diagnosed through a medical history, physical examination, and a urinalysis.
Sometimes, a urine culture may be necessary to identify the specific bacteria causing the infection.
Complications:
If left untreated, UTIs can lead to more severe infections, kidney damage, or even sepsis, a life-threatening condition.
Recurrent UTIs may require further evaluation to identify underlying causes.
Prevention:
You can reduce the risk of UTIs
By staying hydrated,
Practicing good hygiene,
Wiping from front to back after using the toilet,
Urinating before and after sexual intercourse,
Avoid irritants like strong soaps or feminine hygiene sprays.
Prevention is key to avoid UTIs. Drinking plenty of water and urinating frequently can help flush out bacteria from the urinary tract. Women should also wipe from front to back after using the bathroom and avoid using irritants such as douches or feminine hygiene sprays. Wearing loose-fitting clothing and cotton underwear can also help prevent UTI.
It’s important to seek prompt medical attention if you suspect a UTI, especially if symptoms are severe or if you have a history of kidney problems. Early treatment can help prevent the infection from spreading to the kidneys or causing other complications.
Consult our health expert.
0 notes
Text
0 notes
Text
How Soft Drinks May Affect Your Kidneys - Hiranandani Hospital Kidney

In a world dominated by convenience and indulgence, soft drinks have become a ubiquitous part of our daily lives. From cola to lemon-lime sodas, these sugary beverages are enjoyed by people of all ages. However, as we revel in the fizzy sweetness, it's crucial to consider the potential impact of soft drinks on our health, particularly on vital organs like the kidneys. In this blog post, we'll delve into the intricate relationship between soft drink consumption and kidney health, exploring the mechanisms that may lead to adverse effects.
The Sugar Dilemma
One of the primary concerns associated with soft drinks is their high sugar content. Most carbonated beverages are laden with fructose corn syrup, a type of sugar that has been linked to various health issues. Excessive sugar intake has long been associated with conditions like obesity and type 2 diabetes, but its impact on kidney health is less widely known, says Hiranandani Hospital Kidney transplant department.
When we consume large amounts of sugar, the body must work overtime to process it. The kidneys, responsible for filtering blood and eliminating waste, play a crucial role in this process. High sugar intake can lead to an increased workload for the kidneys, potentially contributing to kidney damage over time.
Furthermore, the consumption of sugary beverages has been linked to insulin resistance, a condition where the body's cells become less responsive to the hormone insulin. This resistance can trigger a cascade of metabolic changes that may have implications for kidney function.
Read more :- Does Consuming Soft Drinks Affect Your Kidney
The Role of Phosphoric Acid
Apart from sugar, another key ingredient in many soft drinks is phosphoric acid. This chemical compound is responsible for the tangy taste in colas, but its effects on the kidneys are less appetizing. Phosphoric acid has been studied for its potential to promote the formation of kidney stones.
Kidney stones are solid deposits that form in the kidneys when certain substances, such as calcium and oxalate, concentrate in the urine. The acidic nature of phosphoric acid may contribute to the formation of these stones by altering the pH balance in the urine, making it more conducive to stone formation. While more research is needed to establish a definitive link between phosphoric acid and kidney stones, the existing evidence raises concerns about the impact of this common soda ingredient on renal health.
Dehydration and Kidney Function
As per Hiranandani Hospital Kidney, Soft drinks, particularly those containing caffeine, can contribute to dehydration. Caffeine is a diuretic, meaning it increases urine production and can lead to fluid loss from the body. Dehydration can have a direct impact on kidney function.
The kidneys require an adequate supply of fluid to effectively filter waste from the blood and produce urine. When the body is dehydrated, the kidneys may struggle to perform these functions efficiently. Prolonged or chronic dehydration can potentially contribute to the development of kidney problems, including the formation of kidney stones and the risk of urinary tract infections.
The Link to Hypertension
Soft drink consumption has also been associated with an increased risk of hypertension, or high blood pressure. Hypertension is a known risk factor for kidney disease, as it can damage the blood vessels in the kidneys over time.
The excessive intake of sugary beverages may contribute to hypertension through multiple mechanisms. High sugar consumption has been linked to insulin resistance and inflammation, both of which can contribute to elevated blood pressure. Additionally, the high sodium content in many soft drinks can further contribute to hypertension, as excess sodium can lead to water retention and increased blood volume.
Reducing the Risk
While the potential negative impact of soft drinks on kidney health is a cause for concern, there are steps individuals can take to mitigate these risks and promote overall kidney health.
Moderation is Key: The key to a healthy lifestyle often lies in moderation. Occasional indulgence in soft drinks may not pose a significant risk, but regular, excessive consumption should be avoided.
Choose Healthier Alternatives: Opting for healthier beverage alternatives can significantly reduce the risks associated with soft drinks. Water is the best choice for staying hydrated, and herbal teas or infused water can add flavor without the negative health effects.
Read Labels: Being aware of the ingredients in soft drinks is essential. Reading labels can help you make informed choices about the products you consume and avoid those with excessive sugar or additives.
Stay Hydrated: Drinking an adequate amount of water is crucial for kidney health. Ensuring proper hydration can help the kidneys function optimally and reduce the risk of complications.
Maintain a Balanced Diet: A diet rich in fruits, vegetables, and whole grains can contribute to overall health, including kidney health. These foods provide essential nutrients and antioxidants that support the body's natural detoxification processes.
Conclusion
While the allure of a cold, fizzy soft drink may be tempting, it's essential to consider the potential impact on kidney health. The high sugar content, combined with additives like phosphoric acid and caffeine, can pose risks to the kidneys over time. By being mindful of our beverage choices, opting for moderation, and prioritizing hydration through healthier alternatives, we can take proactive steps to safeguard our kidneys and promote overall well-being, says Hiranandani Hospital Kidney Care. As with any health-related concerns, consulting with healthcare professionals and staying informed about the latest research is crucial for making informed decisions about our dietary choices and lifestyle.
#hiranandani hospital kidney transplant#hiranandani hospital kidney#hiranandani hospital powai news#hiranandani hospital reviews#hiranandani hospital powai covid#hiranandani powai hospital#hiranandani hospital kidney care#hiranandani hospital powai#hiranandani hospital kidney tranplant#hiranandani hospital
0 notes