#arterial thrombosis treatment
Text
Unveiling the Signs: Recognizing Symptoms of Superficial Venous Reflux Disease
Superficial Venous Reflux Disease (SVRD), commonly associated with varicose veins, is a condition affecting the veins in the legs, causing them to fail in efficiently returning blood back to the heart. This ailment can lead to a range of symptoms that impact daily life and overall health. Recognizing these signs early is crucial for effective management and treatment.

In this series of short blogs, we will explore the key symptoms of SVRD, offering insights into how these manifest and what steps can be taken to mitigate their effects.
The Basics of Varicose Veins and Venous Insufficiency
Varicose veins are not just a cosmetic issue; they are often the most visible sign of SVRD. These enlarged, gnarled veins are more than skin-deep, caused by weakened or damaged vein walls and valves. The condition hampers the normal flow of blood back to the heart, leading to venous insufficiency. Recognizing varicose veins is the first step in identifying underlying venous reflux, characterized by veins that appear bluish, swollen, and can protrude above the skin surface. Understanding that these are possibly the first indicators of SVRD is vital for seeking timely medical advice.
Chronic Leg Pain and Heaviness
One of the most common symptoms experienced by individuals with SVRD is a persistent feeling of heaviness and pain in the legs. This discomfort typically worsens after prolonged periods of standing or sitting and might improve with leg elevation. The sensation of heavy legs can often be mistakenly attributed to fatigue or aging, but it is important to recognize it as a potential sign of deeper venous issues. Prompt attention to these symptoms can lead to early diagnosis and prevent further complications.
Swelling in the Legs and Ankles
Swelling, or edema, in the legs and ankles is another telltale symptom of SVRD. This occurs because of the accumulation of blood and fluid in the lower extremities, a direct consequence of inefficient blood flow caused by faulty valves within the veins. Swelling that tends to increase throughout the day or appears regularly can be a clear indicator of venous reflux, necessitating a consultation with a healthcare professional.
Skin Changes and Ulceration
Over time, SVRD can lead to significant changes in the skin around the affected veins. The skin may become itchy, hardened, and discolored—a condition known as venous eczema or stasis dermatitis. In advanced cases, venous ulcers can form, especially near the ankles. These ulcers are difficult to heal and require medical intervention. Recognizing and addressing skin changes early can prevent progression to ulceration, a severe and often painful complication of SVRD.
Restless Legs Syndrome
While not exclusive to SVRD, Restless Legs Syndrome (RLS) can be exacerbated or triggered by underlying venous insufficiency. Individuals with SVRD might experience uncomfortable sensations in their legs, often described as crawling, throbbing, or an irresistible urge to move the legs. These symptoms typically occur at rest and can severely disrupt sleep patterns. Understanding the link between RLS and SVRD can be crucial in managing both conditions effectively.
Conclusion:
Understanding and recognizing the symptoms of Superficial Venous Reflux Disease is crucial for timely and effective treatment. From visible varicose veins to more debilitating conditions like skin changes and ulcers, awareness is the first step toward preventing progression and improving quality of life. If you experience any of the symptoms discussed, consulting with a healthcare professional can provide you with the necessary interventions to manage this condition effectively. Remember, early detection leads to better outcomes and healthier legs.
#Deep Vein Thrombosis St Augustine#End Stage Renal Disease Treatment St Augustine#Critical Limb is Chemia Symptoms#Genicular Artery Embolization for Knee Pain#Superficial Venous Reflux Disease Symptoms#Uterine Fibroid Treatment St Augustine FL
0 notes
Text
Expert Leg Pain Specialist and Diabetic Foot Ulcer Treatment in Hyderabad
It is essential for your health to get the appropriate medical treatment for your unique needs. We provide specialist treatments for leg discomfort and diabetic foot ulcers at Vascularhyd in Hyderabad. As a premier medical facility in the city, we stand out for our dedication to providing patients with the best care possible.
Leg Pain Specialist Doctor in Hyderabad
You're not the only one who has ongoing leg pain. Our knowledgeable leg pain doctors in Hyderabad are committed to identifying and treating the root reasons of your agony. Our specialists bring a lot of knowledge to the table, providing precise diagnoses and efficient treatment programs customized to your needs for everything from musculoskeletal problems to nerve-related disorders.

Why Choose Our Leg Pain Specialist in Hyderabad?
1. Expertise
Our leg pain specialists have a wealth of experience in identifying and managing a variety of leg pain problems. Their expertise guarantees accurate assessments and successful treatment plans.
2. Personalized Care
We are aware that each patient's condition is distinctive. To help you feel better, our specialists take the time to fully comprehend your worries and provide specialized treatment strategies.
3. Cutting-Edge Technology
Our clinic uses cutting-edge diagnostic equipment to make sure your leg pain problems are handled precisely and successfully.
Diabetic Foot Ulcer Treatment in Hyderabad
Numerous problems, such as diabetic foot ulcers, can result from diabetes. Specialized therapies are available at our clinic to treat and control diabetic foot ulcers. Our team of specialists adopts a multidisciplinary strategy to promote wound healing and stop additional problems.
Why opt for Our Diabetic Foot Ulcer Treatment?
1. Expert Team
Our medical staff is skilled in treating diabetic foot ulcers. They work together to offer thorough treatment that takes into account every element of your disease.
2. Customized Approach
Every case of a diabetic foot ulcer is different. Our staff creates individualized treatment programs for you, taking into account elements like the seriousness of the wound and underlying medical issues.
Best Surgeon for AV Fistula in Hyderabad
Our facility has qualified surgeons on staff who can do AV fistula surgery. Our team is dedicated to achieving the best results for individuals needing this vascular access for dialysis and has a history of successful treatments.
Best Cancer Hospital in Hyderabad
Oncology is a part of our commitment to comprehensive healthcare. Our multidisciplinary team works together to deliver effective cancer treatment options that put both your physical and emotional well-being first. We are one of the finest cancer hospitals in Hyderabad.
Conclusion
In conclusion, Vascularhyd is your dependable partner in Hyderabad for expert leg pain therapy, diabetic foot ulcer care, and more. Our devoted experts are ready to give great care whether you need it for cancer treatment, vascular surgery, diabetic foot ulcers, or leg pain. For additional information about our services and to make an appointment, get in touch with +91 9160903004 or go to https://vascularhyd.com/. With us, your path to greater health begins.
For more info:-
vascular surgeon in hyderabad
varicose veins treatment in hyderabad
deep vein thrombosis treatment in hyderabad
acute limb ischemia treatment in hyderabad
peripheral artery disease treatment in hyderabad
#vascular surgeon in hyderabad#varicose veins treatment in hyderabad#deep vein thrombosis treatment in hyderabad#acute limb ischemia treatment in hyderabad#peripheral artery disease treatment in hyderabad
0 notes
Text
The Importance of Early Detection and Treatment of Vascular Diseases
Conditions that impact the blood vessels are referred to as vascular illnesses, including the arteries, veins, and capillaries. These conditions can be caused by many factors, like, genetics, lifestyle habits and underlying medical conditions. knowing the risk factors for vascular disease is important for preventing and managing these conditions. the Vascular Center, we recognize the importance of early detection and diagnosis of vascular diseases. Many vascular conditions do not cause noticeable symptoms until they have reached an advanced stage. Therefore, routine screenings and checkups are crucial in detecting these conditions early.
There are several different types of vascular diseases, including peripheral artery disease (PAD), deep vein thrombosis (DVT), varicose veins, and aneurysms. Each of these conditions can have its own set of symptoms and complications.
For example, PAD can cause pain and cramps in the legs, numbness or weakness in the legs and slow-healing wounds. DVT, on the other hand, can cause swelling and pain in the affected limb and can be life-threatening if the clot breaks free and travels to the lungs. Treatment options for vascular diseases vary according to the type and severity of the disease. Medications, minimally invasive procedures, and surgery can be used to treat vascular disease. Lifestyle changes, such as a healthy diet and regular exercise, can also play an important role in managing blood vessels. At Vascular Center, our team of vascular surgeons, interventional radiologists, cardiologists and other specialists work to provide comprehensive care to patients suffering from vascular diseases. We offer a variety of diagnostic tests to identify and monitor these conditions, including ultrasounds, MRIs, and CT scans. We also inform about technological development and research related to vascular diseases and treatment. For example, we may use minimally invasive procedures such as angioplasty or stenting to treat PAD and other conditions. These procedures usually have a faster recovery time and fewer complications than traditional surgery. One of the most important components of the treatment of vascular diseases is the participation of the patient in the treatment. Quitting smoking and following a healthy lifestyle can significantly improve blood vessels and reduce the risk of complications. At Vascular Center, we have seen many patients successfully control or overcome their vascular disease through a combination of drug therapy, lifestyle changes and regular monitoring. By working with patients, we can help them achieve optimal vascular health and quality of life. conclusion Vascular diseases are serious health problems that can have serious consequences if not treated. However, with early detection, appropriate treatment and lifestyle changes, many patients can manage these conditions effectively. If you are concerned about the health of your blood vessels, contact The Vascular Center and schedule an appointment with one of our experts.
#vascular diseases#early detection#treatment#peripheral artery disease#aortic aneurysm#carotid artery disease#venous insufficiency#deep vein thrombosis#causes#symptoms#complications#lifestyle changes#medication#minimally invasive procedures#surgery#Vascular Center#personalized care
0 notes
Link
Digital subtraction angiogram
Angioplasty/ stenting
Thrombolysis / mechanical thrombectomy for acute vascular thrombosis
Endovascular arterial atherectomy
Endovascular treatment of arterial aneurysm
Endovascular treatment of pseudo aneurysms
Embolisation for vascular malformations.
Endovascular aortic aneurysm repair (EVAR / ESVG)
Haemodialysis access interventions
Inferior Vena Cava filter insertion/retrieval
Endovenous laser/ RFA/ glue ablation for varicose veins
Percutaneous sclerotherapy of spider/ reticular/ perforator veins
Venous access
#Digital subtraction angiogram#Angioplasty/ stenting#Thrombolysis / mechanical thrombectomy for acute vascular thrombosis#Endovascular arterial atherectomy#Endovascular treatment of arterial aneurysm#Endovascular treatment of pseudo aneurysms#Embolisation for vascular malformations.#Endovascular aortic aneurysm repair (EVAR / ESVG)#Haemodialysis access interventions#Inferior Vena Cava filter insertion/retrieval#Endovenous laser/ RFA/ glue ablation for varicose veins#Percutaneous sclerotherapy of spider/ reticular/ perforator veins#nous access
0 notes
Text
Published May 27, 2022
Abstract
The COVID-19 pandemic has led to numerous negative implications for all aspects of society. Although COVID-19 is a predominant lung disease, in 10–30% of cases, it is associated with cardiovascular disease (CVD). The presence of myocardial injury in COVID-19 patients occurs with a frequency between 7–36%. There is growing evidence of the incidence of acute coronary syndrome (ACS) in COVID-19, both due to coronary artery thrombosis and insufficient oxygen supply to the myocardium in conditions of an increased need. The diagnosis and treatment of patients with COVID-19 and acute myocardial infarction (AMI) is a major challenge for physicians. Often the presence of mixed symptoms, due to the combined presence of COVID-19 and ACS, as well as possible other diseases, nonspecific changes in the electrocardiogram (ECG), and often elevated serum troponin (cTn), create dilemmas in diagnosing ACS in COVID-19. Given the often-high ischemic risk, as well as the risk of bleeding, in these patients and analyzing the benefit/risk ratio, the treatment of patients with AMI and COVID-19 is often associated with dilemmas and difficult decisions. Due to delays in the application of the therapeutic regimen, complications of AMI are more common, and the mortality rate is higher.
#mask up#covid#covid 19#covid isn't over#pandemic#covid conscious#cardiovascular health#long covid#covid is airborne#wear a mask#coronavirus
11 notes
·
View notes
Text
Medical Abbreviations on Pharmacy Prescriptions
Here are some common medical abbreviations you may see on pharmacy prescriptions:
qd - once a day
bid - twice a day
tid - three times a day
qid - four times a day
qh - every hour
prn - as needed
pc - after meals
ac - before meals
hs - at bedtime
po - by mouth
IV - intravenous
IM - intramuscular
subQ - subcutaneous
mL - milliliter
mg - milligram
g - gram
mcg - microgram
stat - immediately, right away
NPO - nothing by mouth
cap - capsule
tab - tablet
susp - suspension
sol - solution
amp - ampule
inj - injection
Rx - prescription
C - Celsius
F - Fahrenheit
BP - blood pressure
HR - heart rate
RR - respiratory rate
WBC - white blood cell
RBC - red blood cell
Hgb - hemoglobin
Hct - hematocrit
PT - prothrombin time
INR - international normalized ratio
BUN - blood urea nitrogen
Cr - creatinine
Ca - calcium
K - potassium
Na - sodium
Cl - chloride
Mg - magnesium
PO2 - partial pressure of oxygen
PCO2 - partial pressure of carbon dioxide
ABG - arterial blood gas
CBC - complete blood count
BMP - basic metabolic panel
CMP - comprehensive metabolic panel.
ECG - electrocardiogram
EEG - electroencephalogram
MRI - magnetic resonance imaging
CT - computed tomography
PET - positron emission tomography
CXR - chest x-ray
CTX - chemotherapy
NSAID - nonsteroidal anti-inflammatory drug
DMARD - disease-modifying antirheumatic drug
ACE - angiotensin-converting enzyme
ARB - angiotensin receptor blocker
SSRI - selective serotonin reuptake inhibitor
TCA - tricyclic antidepressant
ADHD - attention deficit hyperactivity disorder
COPD - chronic obstructive pulmonary disease
CAD - coronary artery disease
CHF - congestive heart failure
DVT - deep vein thrombosis
GI - gastrointestinal
UTI - urinary tract infection
OTC - over-the-counter
Rx - prescription
OD - right eye
OS - left eye
OU - both eyes.
TID - thrombosis in dementia
TDS - ter die sumendum (three times a day)
BOM - bilaterally otitis media (infection in both ears)
BT - body temperature
C&S - culture and sensitivity
D/C - discontinue or discharge
D/W - dextrose in water
ETOH - ethyl alcohol
FUO - fever of unknown origin
H&P - history and physical examination
I&D - incision and drainage
I&O - intake and output
KVO - keep vein open
N&V - nausea and vomiting
PERRLA - pupils equal, round, reactive to light and accommodation
PR - per rectum
QAM - every morning
QHS - every bedtime
QOD - every other day
S/P - status post (after)
TPN - total parenteral nutrition
UA - urinalysis
URI - upper respiratory infection
UTI - urinary tract infection
VO - verbal order.
XRT - radiation therapy
YOB - year of birth
BRBPR - bright red blood per rectum
CX - cervix
DVT - deep vein thrombosis
GB - gallbladder
GU - genitourinary
HCV - hepatitis C virus
HPI - history of present illness
ICP - intracranial pressure
IVP - intravenous pyelogram
LMP - last menstrual period
MRSA - methicillin-resistant Staphylococcus aureus
MVA - motor vehicle accident
NKA - no known allergies
PEG - percutaneous endoscopic gastrostomy
PRN - pro re nata (as needed)
ROS - review of systems
SOB - shortness of breath
TAH - total abdominal hysterectomy.
TIA - transient ischemic attack
Tx - treatment
UC - ulcerative colitis
URI - upper respiratory infection
VSD - ventricular septal defect
VTE - venous thromboembolism
XR - x-ray
w/c - wheelchair
XRT - radiation therapy
ASD - atrial septal defect
Bx - biopsy
CAD - coronary artery disease
CKD - chronic kidney disease
CPAP - continuous positive airway pressure
DKA - diabetic ketoacidosis
DNR - do not resuscitate
ED - emergency department
ESRD - end-stage renal disease
FFP - fresh frozen plasma
FSH - follicle-stimulating hormone.
GCS - Glasgow Coma Scale
Hct - hematocrit
Hgb - hemoglobin
ICU - intensive care unit
IV - intravenous
JVD - jugular venous distension
K - potassium
L - liter
MCH - mean corpuscular hemoglobin
MI - myocardial infarction
Na - sodium
NGT - nasogastric tube
NPO - nothing by mouth
OR - operating room
PCN - penicillin
PRBC - packed red blood cells
PTT - partial thromboplastin time
RBC - red blood cells
RT - respiratory therapy
SOA - short of air.
SCD - sequential compression device
SIRS - systemic inflammatory response syndrome
STAT - immediately
T - temperature
TPN - total parenteral nutrition
WBC - white blood cells
ABG - arterial blood gas
A fib - atrial fibrillation
BPH - benign prostatic hypertrophy
CBC - complete blood count
CO2 - carbon dioxide
COPD - chronic obstructive pulmonary disease
CPR - cardiopulmonary resuscitation
CT - computed tomography
CXR - chest x-ray
D5W - dextrose 5% in water
Dx - diagnosis
ECG or EKG - electrocardiogram
EEG - electroencephalogram
ETO - early termination of pregnancy.
FHR - fetal heart rate
GSW - gunshot wound
H&P - history and physical exam
HCG - human chorionic gonadotropin
I&D - incision and drainage
IBS - irritable bowel syndrome
ICP - intracranial pressure
IM - intramuscular
INR - international normalized ratio
IOP - intraocular pressure
LFT - liver function test
LOC - level of consciousness
LP - lumbar puncture
NG - nasogastric
OA - osteoarthritis
OCD - obsessive-compulsive disorder
OTC - over-the-counter
P - pulse
PCA - patient-controlled analgesia
PERRLA - pupils equal, round, reactive to light and accommodation.
PFT - pulmonary function test
PICC - peripherally inserted central catheter
PO - by mouth
PRN - as needed
PT - physical therapy
PT - prothrombin time
PTSD - post-traumatic stress disorder
PVC - premature ventricular contraction
QD - once a day
QID - four times a day
RA - rheumatoid arthritis
RICE - rest, ice, compression, elevation
RSI - rapid sequence intubation
RSV - respiratory syncytial virus
SBP - systolic blood pressure
SLE - systemic lupus erythematosus
SSRI - selective serotonin reuptake inhibitor
STAT - immediately
TB - tuberculosis
TIA - transient ischemic attack.
TID - three times a day
TKO - to keep open
TNTC - too numerous to count
TPN - total parenteral nutrition
URI - upper respiratory infection
UTI - urinary tract infection
V-fib - ventricular fibrillation
V-tach - ventricular tachycardia
VA - visual acuity
WNL - within normal limits
AED - automated external defibrillator
ARDS - acute respiratory distress syndrome
BID - twice a day
BP - blood pressure
BUN - blood urea nitrogen
CAD - coronary artery disease
CHF - congestive heart failure
CVA - cerebrovascular accident
D/C - discontinue
DKA - diabetic ketoacidosis.
DM - diabetes mellitus
DVT - deep vein thrombosis
EGD - esophagogastroduodenoscopy
ER - emergency room
F - Fahrenheit
Fx - fracture
GI - gastrointestinal
GTT - glucose tolerance test
HCT - hematocrit
Hgb - hemoglobin
HRT - hormone replacement therapy
ICP - intracranial pressure
IDDM - insulin-dependent diabetes mellitus
IBS - irritable bowel syndrome
IM - intramuscular
IV - intravenous
K - potassium
KVO - keep vein open
L&D - labor and delivery
LASIK - laser-assisted in situ keratomileusis.
ROM - range of motion
RT - radiation therapy
Rx - prescription
SCD - sequential compression device
SOB - shortness of breath
STD - sexually transmitted disease
TENS - transcutaneous electrical nerve stimulation
TIA - transient ischemic attack
TSH - thyroid-stimulating hormone
UA - urinalysis
US - ultrasound
UTI - urinary tract infection
VD - venereal disease
VF - ventricular fibrillation
VT - ventricular tachycardia
WBC - white blood cell
XRT - radiation therapy
XR - x-ray
Zn - zinc
Z-pak - azithromycin (antibiotic).
AAA - abdominal aortic aneurysm
ABG - arterial blood gas
ACS - acute coronary syndrome
ADL - activities of daily living
AED - automated external defibrillator
AIDS - acquired immunodeficiency syndrome
ALS - amyotrophic lateral sclerosis
AMA - against medical advice
AML - acute myeloid leukemia
APAP - acetaminophen
ARDS - acute respiratory distress syndrome
ASCVD - atherosclerotic cardiovascular disease
BPH - benign prostatic hyperplasia
BUN - blood urea nitrogen
CABG - coronary artery bypass graft
CBC - complete blood count
CHF - congestive heart failure
COPD - chronic obstructive pulmonary disease
CPAP - continuous positive airway pressure
CRF - chronic renal failure.
CT - computed tomography
CVA - cerebrovascular accident
D&C - dilation and curettage
DVT - deep vein thrombosis
ECG/EKG - electrocardiogram
EEG - electroencephalogram
ESRD - end-stage renal disease
FSH - follicle-stimulating hormone
GERD - gastroesophageal reflux disease
GFR - glomerular filtration rate
HbA1c - glycated hemoglobin
Hct - hematocrit
HIV - human immunodeficiency virus
HPV - human papillomavirus
HTN - hypertension
IBD - inflammatory bowel disease
IBS - irritable bowel syndrome
ICU - intensive care unit
IDDM - insulin-dependent diabetes mellitus
IM - intramuscular.
IV - intravenous
LFT - liver function test
MI - myocardial infarction
MRI - magnetic resonance imaging
MS - multiple sclerosis
NPO - nothing by mouth
NS - normal saline
OCD - obsessive-compulsive disorder
OSA - obstructive sleep apnea
PCOS - polycystic ovary syndrome
PMS - premenstrual syndrome
PPD - purified protein derivative
PSA - prostate-specific antigen
PT - prothrombin time
PTT - partial thromboplastin time
RA - rheumatoid arthritis
RBC - red blood cell
RSV - respiratory syncytial virus
SLE - systemic lupus erythematosus
TB - tuberculosis.
It is important to remember that medical abbreviations can vary based on location and specialty.
Healthcare professionals should use medical abbreviations with caution and only when they are familiar with their meanings.
Patients should always communicate any questions or concerns they have about their medications or medical care to their healthcare provider or pharmacist to ensure they receive safe and accurate medical care.

7 notes
·
View notes
Text
Best Cardiologist in Singapore: A Comprehensive Guide, Top Tips, and Recommendations
Introduction
Looking for the best cardiologist in Singapore to address your cardiovascular concerns and receive top-notch medical care? Then this article is for you. Cardiovascular disease (CVD), refers to a disease of the heart or within your blood vessels. When it comes to cardiovascular disease, you will of course want the best cardiologist in Singapore. After all, cardiovascular disease accounted for 7762 deaths (32.0%) in Singapore alone in 2021. Cardiovascular diseases are highly serious and can be the result of:
A blood clot (thrombosis)
A buildup of fatty deposits inside your arteries. As a result, the artery hardens and narrows (atherosclerosis)
To help you with choosing the best cardiologist or heart doctor for your situation, we’ve put together this guide. Throughout the guide we will cover the role a cardiologist fulfills, the specializations of cardiologists and what to look for in a cardiologist. We will also provide some information on how to prepare for your first appointment, the documents you need to provide and questions you can ask your cardiologist at your appointments.
What Is A Cardiologist?
When looking for the best cardiologist in Singapore, it’s important to first know what a cardiologist is. Cardiologists are doctors who focus on diseases and defects of the heart and blood vessels, often referred to as the cardiovascular system. It is the role of a cardiologist to diagnose, assess and treat patients, staying with them through the whole process. As such, it’s crucial that you find a cardiologist who you trust and are confident in working with.
What To Look For In A Cardiologist?
When looking for a cardiologist to treat your body, you want the best cardiologist in Singapore. Our goal today is to help you find just that. With cardiologists, you often see the same doctor from the diagnosis and assessment stage through to treatment, procedures and finally aftercare. As such, you want to be sure that the cardiologist you choose is the best for you. With that in mind, you should be looking for a cardiologist you trust, one with a great reputation and one who cares about your health.
How To Find The Best Cardiologist In Singapore?
You’ve most likely already begun your search for a cardiologist, here are some useful tips and advice on finding the best cardiologist in Singapore. Online search engines and directories are a great place to get an idea of who is available in your area. Often these come with comparisons and patient reviews so you can really get a sense for who the cardiologist is and how they work. Furthermore, you may want to consider reaching out to friends, family and other healthcare professionals for recommendations. In fact, the Harley Street has many good patient reviews and testimonials as a testament to having some of the best cardiologists in Singapore.
The Harley Street Heart And Vascular Centre
At the Harley Street we have the top cardiologists in Singapore across our three branches.
Gleneagles Hospital, Singapore
Mount Elizabeth Novena, Singapore
Mount Elizabeth Medical Centre, Singapore
In each of our locations we have state of the art facilities, highly trained caring and professional staff and the best cardiologists in Singapore.
Conclusion
To keep your body healthy, it is essential that you maintain regular cardiac checkups with your cardiologist. Go to this page to read even more information covering the topic on our website. The cardiologists at The Harley Street are highly experienced and have helped many patients manage their conditions. So, if you’re looking for the best cardiologist in Singapore, get in touch with us today.
2 notes
·
View notes
Text
When to worry about thrombosis — Rarely, patients with thrombocytopenia are at risk for thrombosis rather than, or in addition to, bleeding. While most of the implicated disorders are rare, it is important to consider them because urgent treatment may be needed to prevent life-threatening thrombotic events.
Examples include the following:
●Heparin-induced thrombocytopenia – A small percentage of patients exposed to heparin (less than 5 percent) will develop heparin-induced thrombocytopenia (HIT) in which antibodies to a platelet factor 4 epitope induced by heparin can cause thrombocytopenia and platelet activation, leading to life-threatening venous and/or arterial thrombosis. This diagnosis should be considered in a patient recently exposed to heparin who develops thrombocytopenia, thrombosis, anaphylaxis, or skin reactions. Treatment involves immediate discontinuation of heparin and administration of a non-heparin anticoagulant (e.g., dabigatran or bivalirudin).
●Vaccine-induced immune thrombotic thrombocytopenia (VITT) – VITT is a rare syndrome that occurs after vaccination with coronavirus disease 2019 (COVID-19) adenoviral vector vaccines (AstraZeneca and Janssen [Johnson & Johnson]). It resembles spontaneous HIT in that there is no prior heparin exposure, and it is associated with life-threatening venous and/or arterial thrombosis. Individuals with thrombosis and/or thrombocytopenia should be evaluated for recent administration of a COVID-19 vaccine within the preceding 5 to 30 days, and for which specific type of vaccine they received.
●Antiphospholipid syndrome – The antiphospholipid syndrome (APS) can develop in individuals with systemic lupus erythematosus, other medical conditions (eg, infection, medications, cancer), or in individuals without an underlying condition. Patients may have venous and/or arterial thrombosis. Treatment involves anticoagulation or aspirin, and treatment of any underlying condition.
●Disseminated intravascular coagulation – Patients with disseminated intravascular coagulation (DIC) are at risk of bleeding or thrombosis, usually venous. DIC is commonly seen in acutely ill patients with sepsis or malignancy, but it can also be seen in a variety of other conditions.
●Thrombotic microangiopathy – Thrombotic microangiopathies (TMAs) such as thrombocytopenic purpura (TTP), hemolytic uremic syndrome (HUS), or drug-induced TMA (DITMA) are associated with small-vessel platelet-rich thrombi. These microthrombi can occur in any organ and can be life-threatening. Plasma exchange for TTP may be life-saving and should be initiated immediately when TTP is suspected.
●Paroxysmal nocturnal hemoglobinuria – Paroxysmal nocturnal hemoglobinuria (PNH) is a rare condition caused by loss of glycosyl phosphatidylinositol from cell membranes. Thrombosis (often involving unusual locations such as intraabdominal or cerebral veins) can occur, along with hemolytic anemia and/or bone marrow failure. Treatment depends on the degree of cytopenias and the presence of thrombosis.
●ITP with a concomitant thrombotic disorder – Certain conditions can occur in patients with ITP increasing their risk of thrombosis such as atrial fibrillation or recent or previous deep vein thrombosis. Management of anticoagulation in that population can be challenging; however, it is important to note that the low platelet count is not protective against thrombosis, and anticoagulation is often indicated.
Work up:
Peripheral blood smear — Review of the peripheral blood smear is used to exclude pseudothrombocytopenia (eg, falsely low platelet count due to platelet clumping) and to evaluate morphologic abnormalities of blood cells that could be useful in determining the cause of thrombocytopenia. As an example, giant platelets may suggest a congenital platelet disorder (eg, MYH-9-related disorders, Bernard Soulier syndrome [BSS]); these may be counted as red blood cells by some automated counters.
Pseudothrombocytopenia — The possibility of pseudothrombocytopenia (ie, falsely low platelet count) should be eliminated before any further evaluation is undertaken. Pseudothrombocytopenia can occur in a number of settings, all of which can be identified by review of the peripheral blood smear and/or repeating the CBC using a non-EDTA anticoagulant:
●Incompletely mixed or inadequately anticoagulated samples may form a clot that traps platelets in the collection tube and prevents them from being counted.
●In approximately 0.1 percent of individuals, exposure of patient samples to the EDTA anticoagulant in the collection tube can induce platelet clumps or platelet rosettes around white blood cells (WBCs). These may be counted by automated counters as leukocytes rather than platelets. The mechanism is "naturally occurring" platelet autoantibodies directed against a concealed epitope on platelet membrane glycoprotein (GP) IIb/IIIa that becomes exposed by EDTA-induced dissociation of GPIIb/IIIa [45-52].
If platelet clumping is observed, the platelet count is repeated using heparin or sodium citrate as an anticoagulant in the collection tube. If citrate is used, the platelet count should be corrected for dilution caused by the amount of citrate solution; no such correction is needed for heparin. Alternatively, fresh, non-anticoagulated blood can be pipetted directly into platelet-counting diluent fluid.
RBC and WBC abnormalities — Abnormal RBC and WBC morphologies may suggest a specific condition.
Examples include the following:
●Schistocytes suggest a microangiopathic process (eg, DIC, TTP, HUS, DITMA).
●Nucleated RBCs, and Howell-Jolly bodies, may be seen post-splenectomy or occasionally in patients with poor splenic function.
●Spherocytes suggest immune-mediated hemolytic anemia or hereditary spherocytosis.
●Leukoerythroblastic findings, teardrop cells, nucleated RBCs, or immature granulocytes suggest an infiltrative process in the bone marrow.
●Leukocytosis with a predominance of bands and/or toxic granulations suggests infection.
●Immature WBCs (eg, myeloblasts) or dysplastic WBCs suggest leukemia or myelodysplasia.
●Multi-lobed/hypersegmented neutrophils (ie, more than 5 lobes) suggest a megaloblastic process (eg, B12/folate/copper deficiency).
HIV and HCV testing — Thrombocytopenia has been identified as an important "indicator condition" for HIV infection. Thus, adults with new thrombocytopenia should have HIV testing if not done recently.
Thrombocytopenia may also be seen with hepatitis C virus (HCV) infection; testing is appropriate for adults with thrombocytopenia if not done recently. Other laboratory testing — Aside from the testing mentioned above (CBC, review of peripheral smear, HIV and HCV testing), no additional laboratory testing is absolutely required in a patient with isolated thrombocytopenia. However, additional testing may be warranted in patients with other findings.
Examples of findings that may trigger other laboratory testing include the following:
●Symptoms or findings of systemic autoimmune disorders (eg, systemic lupus erythematosus [SLE], anti-phospholipid syndrome [APS]) may prompt testing for anti-nuclear antibodies or anti-phospholipid antibodies, respectively. We do not test for these in patients with isolated thrombocytopenia and no signs or symptoms suggestive of SLE or APS.
●Findings of liver disease should prompt measurements of hepatic enzymes and possibly tests of liver synthetic function (eg, albumin, coagulation testing), depending on the severity of the liver disease.
●Thrombosis should prompt consideration of DIC, heparin-induced thrombocytopenia (HIT) and related syndromes, and APS. Depending on the site of thrombosis and other hematologic findings, paroxysmal nocturnal hemoglobinuria (PNH) may also be a consideration.
●Microangiopathic changes on the peripheral smear should prompt coagulation testing (eg, PT, aPTT, fibrinogen) and measurement of serum lactate dehydrogenase (LDH) and renal function to evaluate for DIC, TTP, or HUS; with subsequent evaluation based on the results.
ADDITIONAL EVALUATION
Hematologist referral/consultation — Referral to a hematologist is appropriate to confirm any new diagnosis of a thrombocytopenic condition or to determine the cause of any unexplained thrombocytopenia. The urgency of referral depends on the degree of thrombocytopenia and other abnormalities, and the stability of the findings.
In hospitalized patients, some conditions are medical emergencies that require immediate action. Immediate hematologist involvement in diagnosis and management is appropriate for the following:
●Suspected thrombotic thrombocytopenic purpura (TTP) or hemolytic uremic syndrome (HUS).
●Suspected heparin-induced thrombocytopenia (HIT).
●Suspected COVID-19 vaccine-induced immune thrombotic thrombocytopenia (VITT).
●Suspected hematologic malignancy (eg, acute leukemia), aplastic anemia, or other bone marrow failure syndrome.
The consulting hematologist can also assist in diagnosis and management of patients with severe thrombocytopenia (ie, platelet count less than 50,000/microL) who have serious bleeding or require an urgent invasive procedure, and in pregnant women with severe thrombocytopenia, regardless of the cause.
Bone marrow evaluation — Bone marrow evaluation (aspirate and biopsy) is not required in all patients with thrombocytopenia. However, it may be helpful in some patients if the cause of thrombocytopenia is unclear, or if a primary hematologic disorder is suspected. A possible exception may be a clinical picture consistent with a nutrient deficiency in which a bone marrow would only be needed if a deficiency could not be documented, or if the hematologic findings did not resolve upon nutrient repletion.
The following bone marrow findings may be helpful:
●Normal or increased numbers of megakaryocytes suggests that the thrombocytopenia is due, at least in part, to a condition associated with platelet destruction (eg, ITP, drug-induced immune thrombocytopenia).
●Decreased megakaryocyte numbers, along with overall decreased or absent cellularity (picture 18 and picture 19), is consistent with decreased bone marrow production of platelets, as in aplastic anemia.
●In rare cases, severe reduction or absence of megakaryocytes with no other abnormalities (also called acquired amegakaryocytic thrombocytopenia or acquired pure megakaryocytic aplasia) may occur. This finding is most often reported in patients with SLE, and is typically due to an autoantibody directed against the thrombopoietin receptor.
●Megaloblastic changes in the RBC and granulocytic series suggest a nutrient deficiency (eg, vitamin B12, folate, copper) (picture 20), while dysplastic changes suggest a myelodysplastic disorder (picture 21 and picture 22).
●Granulomata, increased reticulin or collagen fibrosis (picture 23 and picture 24), or infiltration with malignant cells (picture 25) establishes the diagnosis of bone marrow invasion, especially when a leukoerythroblastic blood picture is also present.
GENERAL MANAGEMENT PRINCIPLES
There are some general management principles that apply to all patients with thrombocytopenia regardless of the cause, and for which questions may arise before a diagnosis has been established.
●Activity restrictions – Patients who are otherwise healthy and have no manifestations of petechiae or purpura may not require activity restrictions.
Individual considerations apply to participation in certain activities. As an example, individuals with severe thrombocytopenia (less than 50,000/microL) generally should not participate in extreme athletics such as boxing, rugby, and martial arts. However, no restrictions are necessary for usual activities or low-impact exercise.
●Anticoagulant and anti-platelet medications – For anticoagulant and anti-platelet medications, the clinical indications and risks associated with discontinuation (eg, thrombosis) are balanced against the bleeding risk associated with the degree of thrombocytopenia and of continuing the anticoagulant and/or anti-platelet medication [7]. Input from the consulting specialist who prescribed the medication and/or the hematologist may be sought. A discussion of anticoagulation in adults with thrombocytopenia is presented separately.
It is also important to note that thrombocytopenia by itself does not protect against venous or arterial thrombosis, and appropriate use of thromboprophylaxis or anticoagulants should not be withheld from a patient with mild to moderate thrombocytopenia (eg, greater than 50,000/microL) if it is indicated (eg, postoperatively). For patients with more severe thrombocytopenia, decisions are made on a case-by-case basis regarding the risks of bleeding and benefits of anticoagulation.
●Over-the-counter remedies – Patients should be educated about which non-prescription remedies interfere with platelet function (eg, aspirin, nonsteroidal anti-inflammatory drugs, ginkgo biloba). In general, these agents are avoided unless there is a specific indication for which equivalent alternatives are lacking.
●Safe platelet count for invasive procedures – Most platelet count thresholds for invasive procedures are based on weak observational evidence at best. In general, procedures with a greater risk of bleeding are performed at higher platelet counts. While there is some flexibility in individual circumstances, anesthesiologists and surgeons performing these procedures will have the last word. A listing of general guidelines used for different procedures is presented separately.
Optimal methods for raising the platelet count in preparation for an invasive procedure depend on the underlying condition (eg, corticosteroids or intravenous immune globulin (IVIG) for presumptive ITP; platelet transfusion for myelodysplastic syndromes). These approaches are discussed in detail in separate topic reviews.
Individuals with impaired platelet function may require platelet transfusions despite adequate platelet counts, depending on the procedure. Attention should also be paid to correcting coagulation abnormalities if present.
●Emergency management of bleeding – Urgent management of critical bleeding in the setting of severe thrombocytopenia requires immediate platelet transfusion, regardless of the underlying cause.
6 notes
·
View notes
Text
What Is Cerebrovascular ?

Cerebrovascular Best Treatment In Homeopathy
Cerebrovascular disease refers to a group of conditions that affect blood flow and the blood vessels in the brain. Problems with blood flow may occur from blood vessels narrowing (stenosis), clot formation (thrombosis), artery blockage (embolism), or blood vessel rupture (haemorrhage). Lack of sufficient blood flow (also referred to as ischemia) affects brain tissue and may cause a stroke.
Symtoms
a severe and sudden headache
paralysis of one side of the body, or hemiplegia
weakness on one side, also known as hemiparesis
confusion
difficulty communicating, including slurred speech
losing vision on one side
loss of balance
becoming unconscious
Causes
Diabetes
High blood cholesterol
High blood pressure
Physical inactivity and obesity
Smoking
#brahmhomeo#homeopathy#health#patient#medicine#disease#treatment#carebearcousins#ahmedabad#drpradeepkushwaha
3 notes
·
View notes
Text
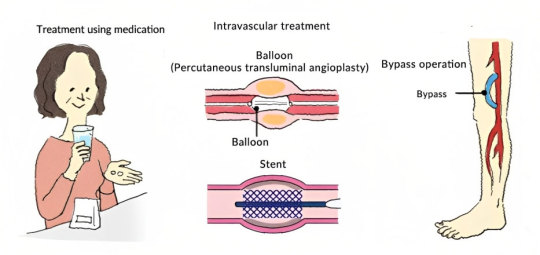
How can peripheral arterial disease be treated ?
The goals of treatment for peripheral artery disease is:
Manage symptoms, such as leg pain, blackening, or ulcer, so as to improve your quality of life.
Improve artery health to reduce the risk of heart attack and stroke.
Depending on the severity of the peripheral arterial disease (PAD) and diagnostic testing results, medical treatment, minimally invasive endovascular treatment or surgical treatment option may be offered.
Lifestyle changes:
For mild PAD sufferers, lifestyle changes may be enough to slow or even halt the progression of your disease. Commonly prescribed lifestyle changes include:
Stop smoking
Exercise regularly
Eat a healthy diet that’s low in fats and cholesterol
Manage underlying conditions like diabetes or high blood pressure
1- Medications: PAD patients may receive medications to prevent blood clots(blood thinners), improve blood flow, and reduce pain from claudication. In addition, medications may be used to control your high cholesterol, high blood pressure, or diabetes.
If your leg pain is so severe that it prevents you from carrying out everyday activities, or if your symptoms have failed to respond to lifestyle changes and medical treatment, revascularization may be recommended.
2- Endovascular (Interventional Radiology) treatment: Minimally invasive procedures such as angioplasty, stenting and thrombolysis may be offered to restore the flow in blocked arteries of your legs.
3- Surgical treatment: This involves inserting a graft bypass to move blood around the blocked or narrowed artery. The graft may be made from a vessel taken from another part of your body or using synthetic materials.
Successful PAD (peripheral artery disease) management often involves a combination of lifestyle changes, medications, and, when necessary, medical procedures or surgery. Tailoring the treatment plan to individual needs is crucial for optimal outcomes. If you suspect PAD or are at risk, seeking prompt medical attention ensures an accurate diagnosis and the development of a personalized treatment strategy.
For more information, consult Dr. Kunal Arora One the Best Interventional Radiologist in Mumbai or you can contact us on 9892288400.
#dr. kunal arora#best varicose treatment#endovascular care centre#interventional radiologist in mumbai#vascularhealth#veintreatment#deep vein thrombosis#healthcare#varicoseveintreatment#best interventional radiologist in mumbai#peripheral artery disease#endovascular treatment#Interventional Radiologist#Intravascular Treatment
0 notes
Text
When Should You See A Vascular Specialist?

Vascular health is a critical aspect of overall well-being, yet it often goes unnoticed until symptoms become severe.
However, various factors can compromise vascular health, leading to potentially serious complications. Knowing when to seek the expertise of a vascular specialist can make a significant difference in preventing or managing vascular conditions.
In this blog, we'll explore the signs and symptoms, as explained by the specialist at the best polyclinic in Kolkata, that indicate the need for a consultation with a vascular specialist.

You should consider seeing a vascular specialist if you're experiencing:
1. Continuous Leg Pain:
One common indicator of vascular issues is continuous leg pain.
This pain may show as cramping, throbbing, or aching in the calves, thighs, or buttocks, especially during physical activity.
A vascular specialist can conduct diagnostic tests such as ankle-brachial index (ABI) testing or Doppler ultrasound to assess circulation and determine the appropriate course of treatment.
2. Swelling And Discoloration:
Swelling and discoloration in the legs or feet are potential signs of venous insufficiency or deep vein thrombosis (DVT).
Venous insufficiency occurs when the veins fail to adequately return blood to the heart, leading to pooling and swelling.
DVT, on the other hand, is a blood clot that forms in a deep vein, often causing swelling, warmth, and redness in the affected area.

3. Non-Healing Wounds:
Wounds that fail to heal or show slow healing progress, particularly in the lower extremities, may indicate poor circulation due to arterial or venous disease.
Inadequate blood flow deprives tissues of essential nutrients and oxygen, impairing the body's ability to repair itself.
A vascular specialist can assess the wound, identify underlying vascular issues, and recommend appropriate interventions, which may include vascular surgery or minimally invasive procedures to restore blood flow.

4. Varicose Veins And Spider Veins:
While varicose veins and spider veins are often considered cosmetic concerns, they can also signal underlying venous insufficiency.
Varicose veins appear as enlarged, twisted veins that protrude from the skin's surface, while spider veins are smaller, web-like clusters of veins.
These conditions may cause discomfort, heaviness, or itching, especially after prolonged standing or sitting.
For more information, you need to consult the best vascular surgeon in Kolkata.
Wrap-Up The vascular system plays a pivotal role in maintaining our health and well-being.
Recognizing the signs and symptoms of vascular conditions and knowing when to seek help from a vascular specialist is crucial for timely diagnosis and appropriate management.
You should remember that early detection and treatment of vascular issues can help prevent serious complications.
So don't hesitate to see a specialist at the top diagnostic centre in Kolkata if you have any concerns.
#best multispeciality clinic kolkata#top diagnostic centre kolkata#best healthcare in kokata#health clinic kolkata#best polyclinic kolkata#best healthcare service kolkata
0 notes
Text
Discovering Excellence in Vascular Health Vein and Artery Clinic Near You
In the realm of healthcare, the intricate network of veins and arteries plays a vital role in maintaining overall wellness. When issues arise within this system, seeking specialized care becomes essential. Fortunately, for those in need, there's a beacon of hope in the form of vein and artery clinics, dedicated to addressing vascular health concerns with precision and expertise.

One such clinic stands out, nestled conveniently within reach, offering comprehensive care and advanced treatments tailored to individual needs.
At the vein and artery clinic near me, a team of highly skilled vascular specialists stands ready to tackle a range of conditions affecting the circulatory system. From varicose veins and peripheral artery disease to deep vein thrombosis and beyond, their expertise covers a broad spectrum of vascular disorders.
What sets this clinic apart is its commitment to utilizing cutting-edge technology and evidence-based practices to deliver optimal outcomes. From state-of-the-art diagnostic tools to minimally invasive procedures, patients can expect nothing less than the highest standard of care.
Upon stepping into the clinic, patients are greeted by a warm and inviting atmosphere designed to alleviate any apprehensions they may have. The staff, comprising friendly faces and compassionate professionals, ensures that each patient feels heard, understood, and valued throughout their journey to vascular wellness.
One of the clinic's primary focuses is on education and empowerment. Patients are not only treated for their conditions but also equipped with the knowledge and resources needed to actively participate in their own care. Whether it's understanding the underlying causes of their symptoms or learning preventive measures to maintain vascular health, patients are empowered to make informed decisions about their well-being.
The clinic's array of services covers the entire spectrum of vascular care. For those troubled by unsightly varicose veins, innovative treatments such as endovenous laser therapy and sclerotherapy offer effective solutions with minimal downtime. Similarly, individuals suffering from peripheral artery disease can benefit from interventions like angioplasty and stenting to restore proper blood flow to their limbs.
Moreover, the clinic's dedication to ongoing research and development ensures that patients have access to the latest advancements in vascular medicine. Clinical trials and collaborations with leading institutions enable them to offer innovative therapies that may not be available elsewhere, giving patients hope where traditional treatments may have fallen short.
Accessibility is another hallmark of this esteemed clinic. Situated conveniently within reach, it aims to make quality vascular care accessible to all who need it. Whether you're in the heart of the city or nestled in the suburbs, expert help is never too far away.
The Vein and Artery Clinic near you stands as a beacon of excellence in vascular health. With its skilled professionals, advanced treatments, patient-centered approach, and commitment to innovation, it offers a comprehensive solution to a wide range of vascular conditions. For anyone seeking specialized care for their veins and arteries, this clinic promises not just treatment, but a path towards lasting wellness and peace of mind.
For more info:-
san antonio peripheral artery disease treatments
phlebectomy services in san antonio tx
0 notes
Text
Unraveling Possibilities: Fibrinolytic Therapy Market Outlook
Fibrinolytic therapy, also known as thrombolysis, is a medical procedure involving the administration of medication called fibrinolytics to dissolve dangerous blood clots (thrombi) that develop in blood vessels. These blood clots can cause serious medical conditions like heart attacks and strokes if they block arteries supplying blood to vital organs like the heart or brain. Fibrinolytic therapy works by breaking down fibrin, a key component of blood clots, through the use of medications like recombinant tissue plasminogen activator, streptokinase, tenecteplase, and desmoteplase. They are used to treat conditions like pulmonary embolism, deep vein thrombosis, myocardial infarction, and ischemic strokes. The Global fibrinolytic therapy market is estimated to be valued at US$ 34.96 Bn in 2024 and is expected to exhibit a CAGR of 3.7% over the forecast period 2023 to 2030.
Key Takeaways
Key players operating in the Fibrinolytic Therapy are Genentech, Inc. (Roche), Bayer AG, Boehringer Ingelheim International GmbH, Pfizer Inc., Bristol Myers Squibb Company, Novartis AG, AstraZeneca PLC, Johnson & Johnson, Daiichi Sankyo Company, Limited, Merck & Co., Inc., Sanofi S.A., Takeda Pharmaceutical Company Limited, Abbott Laboratories, and Mallinckrodt Pharmaceuticals, Mitsubishi Tanabe Pharma Corporation. Genentech holds a significant share due to its blockbuster drug Activase (Alteplase) for ischemic strokes.
The key opportunities in the fibrinolytic therapy market include rising demand for long-acting agents like tenecteplase to replace streptokinase and development of drugs suitable for genetic variations associated with differential fibrinolysis responses. There is significant potential for market expansion in developing economies due to increasing healthcare investments and disease burden of cardiovascular diseases.
Market drivers and restrain:
Rising prevalence of cardiovascular diseases is one of the key drivers of the fibrinolytic therapy market. According to WHO, cardiovascular diseases are the leading cause of deaths globally, taking an estimated 17.9 million lives each year. Growing geriatric population is also fueling the market since risk of CVDs increases with age. However, high costs of treatment, risk of bleeding complications, and requirement of specialized care are some factors inhibiting wider adoption of fibrinolytic drugs in some countries.
Market drivers:
- Growing prevalence of cardiovascular diseases
- Increasing geriatric population
Market restrain:
- High costs of treatment
- Bleeding risks associated with fibrinolytic drugs
- Requirement of specialized care
Segment Analysis
The Fibrinolytic Therapy market is dominating sub-segmented into Plasminogen Activators, tenecteplase, urokinase, alteplase, lanoteplase and streptokinase. The plasminogen activators sub-segment is dominating currently due to improvement in cardiovascular disease treatment methods. Plasminogen activators helps in dissolving of blood clots by activating plasminogen into plasmin. Its effectiveness makes it suitable for treating conditions like pulmonary embolism (PE), deep vein thrombosis (DVT).
Global Analysis
In terms of regional analysis, North America is the fastest growing and dominating region currently in the Fibrinolytic Therapy market due to rising number of heart diseases patients, improved healthcare infrastructure and higher spending on research and development activities in the region. Asia Pacific is expected to witness the highest CAGR over the forecast period. This is attributable to increasing burden of cardiovascular diseases, growing geriatric population and health awareness in emerging economies like China and India.
0 notes
Text
D-dimer Testing Market to hit USD 2 Bn by 2032, says Global Market Insights Inc.

D-Dimer Testing Market size is predicted to register over USD 2 billion by 2032. The increasing prevalence of conditions, such as deep vein thrombosis (DVT), pulmonary embolism (PE), and disseminated intravascular coagulation (DIC) will drive the industry progression.
Request for a sample of this research report @ https://www.gminsights.com/request-sample/detail/5972
As per the Centre of Disease Control and Prevention (CDC), the number of individuals annually impacted by deep vein thrombosis (DVT) or pulmonary embolism (PE) reached 900,000 people in the U.S. These conditions often necessitate D-Dimer testing as part of the diagnostic process to assess the likelihood of thrombotic events. The rising aging population, associated with obesity and sedentary habits, is also contributing to the growing incidence of thrombotic disorders.
Rising advancements in healthcare infrastructure, particularly in emerging economies, are boosting accessibility to diagnostic services, including D-Dimer testing. There is a growing awareness among healthcare professionals about the utility of this testing in diagnosing thrombotic disorders at an early stage. The integration of novel technologies, such as point-of-care testing and automation in laboratory settings to enhance the efficiency and accuracy of D-Dimer assays will add to the market gains.
Rising usage to treat pulmonary embolism
D-Dimer testing market from the pulmonary embolism (PE) application segment is slated to record high demand by 2032, as it represents a life-threatening condition characterized by the blockage of arteries in the lungs, often resulting from blood clots originating in other body parts. D-Dimer testing helps in the assessment of suspected cases of pulmonary embolism, aiding clinicians in ruling out or confirming the presence of thrombotic events. The rising incidence of prolonged immobility, surgery, and certain medical conditions will also contribute to the increased demand for PE diagnosis.
Growing presence in hospitals
The hospitals segment in the D-dimer testing market is poised to generate notable revenues during 2024 and 2032, due to their higher popularity as primary hubs for patient care, diagnosis, and treatment. With rising burden of thrombotic disorders globally, hospitals witness a steady influx of patients with symptoms like deep vein thrombosis (DVT) and pulmonary embolism. Hospitals also often house advanced laboratory facilities equipped with automated testing platforms and skilled personnel for facilitating efficient and high-throughput D-Dimer testing.
Asia Pacific to emerge as a lucrative market
The Asia Pacific D-dimer testing market is touted to surge at a rapid pace from 2024 to 2032, attributed to the increasing adoption of western lifestyle habits coupled with rising urbanization and sedentary lifestyles. The expanding geriatric population across Asia Pacific countries, particularly in Japan, China, and India, is predisposed to a higher incidence of thrombotic events. The improving healthcare infrastructure and growing investments in medical R&D activities in countries like South Korea and Singapore are facilitating greater accessibility to advanced diagnostic technologies.
Request for Report Customization @ https://www.gminsights.com/roc/5972
D-Dimer Testing Industry Participants
Some major companies in the global D-Dimer testing market include Siemens Healthcare GmbH, Abbott Laboratories, Thermo Fisher Scientific Inc., BioMedica Diagnostics, Unbound Medicine Inc biomérieux SA, Quidel Corporation, Diazyme Laboratories Inc. (General Atomics), FHoffmann-La Roche Ltd., HORIBA Ltd., Sekisui Diagnostics LLC (Sekisui Chemical Co. Ltd.), and Werfen.
These firms are focusing on partnership ventures to widen their global presence and customer base. For instance, in May 2022, the assay, developed by Horiba Medical, successfully detected venous thromboembolism (VTE) with excellent accuracy, reliability, and turnaround time on the manufacturer's Yumizen G800 fully automated hemostasis analyzer.
#Ddimer#BloodClotTesting#Thrombosis#CoagulationTesting#CardiovascularHealth#MedicalDiagnosis#Hemostasis#DiagnosticTesting#ClotDetection#LaboratoryMedicine
1 note
·
View note
Text
Genetic Factors and Single Subsegmental Pulmonary Embolism Risk
Pulmonary embolism (PE) is a potentially life-threatening condition characterized by the obstruction of pulmonary arteries by blood clots. While PE can affect various segments of the pulmonary vasculature, single subsegmental pulmonary embolism (SSPE) has garnered increasing attention due to its unique clinical features and management challenges. In this blog post, we delve into the genetic factors influencing SSPE risk and their implications for patient care and management.
Understanding Single Subsegmental Pulmonary Embolism (SSPE)
SSPE refers to the presence of a blood clot in a single subsegmental branch of the pulmonary artery, typically detected through imaging studies such as computed tomography pulmonary angiography (CTPA). Unlike larger pulmonary emboli that may cause significant hemodynamic compromise, SSPEs are often smaller and may exhibit varying clinical presentations, ranging from asymptomatic to mild respiratory symptoms.
Genetic Factors and SSPE Risk
Recent research has shed light on the role of genetic factors in predisposing individuals to venous thromboembolism (VTE), including pulmonary embolism. VTE encompasses deep vein thrombosis (DVT) and PE, with genetic predispositions contributing to thrombus formation and propagation. Several key genetic factors are implicated in SSPE risk:
Factor V Leiden Mutation
The Factor V Leiden mutation is one of the most well-known genetic risk factors for VTE, including PE. This mutation involves a change in the Factor V protein, leading to increased resistance to inactivation by protein C, a natural anticoagulant. Individuals carrying one or two copies of the Factor V Leiden mutation have a higher risk of developing thrombotic events, including SSPE.
Prothrombin Gene Mutation (G20210A)
The prothrombin gene mutation, specifically the G20210A variant, is another genetic factor associated with increased VTE risk. This mutation results in elevated levels of prothrombin, a key protein in the coagulation cascade. The combination of Factor V Leiden and prothrombin gene mutations further amplifies the thrombotic risk, including SSPE occurrence.
MTHFR Gene Polymorphisms
Methylenetetrahydrofolate reductase (MTHFR) gene polymorphisms, particularly the C677T and A1298C variants, have been linked to altered homocysteine levels and thrombotic events. Elevated homocysteine levels are associated with endothelial dysfunction and increased clotting tendency, contributing to VTE risk, including SSPE.
Clinical Implications and Management Strategies
Understanding the genetic factors influencing SSPE risk is crucial for risk stratification, diagnosis, and management of affected individuals. Genetic testing may be considered in patients with unprovoked or recurrent VTE events, especially in younger individuals or those with a family history of thrombotic disorders. Identifying specific genetic mutations allows for personalized risk assessment and tailored anticoagulation strategies.
Anticoagulation Therapy
Anticoagulation remains the cornerstone of SSPE management, aimed at preventing clot propagation and recurrent thrombotic events. The choice of anticoagulant agents, such as direct oral anticoagulants (DOACs) or vitamin K antagonists (VKAs), depends on individual patient factors, including genetic profile, comorbidities, and bleeding risk.
Lifestyle Modifications and Follow-Up
In addition to pharmacological therapy, lifestyle modifications such as maintaining a healthy weight, regular physical activity, and smoking cessation are essential in reducing VTE recurrence risk. Regular follow-up evaluations, including imaging studies and laboratory monitoring, help assess treatment efficacy and identify potential complications.
Genetic Insights for SSPE Management with PatientSelfTesting
In conclusion, genetic factors play a significant role in single subsegmental pulmonary embolism risk, influencing thrombotic propensity and treatment outcomes. Incorporating genetic testing into clinical practice allows for personalized risk assessment and optimized management strategies for SSPE patients.
At PatientSelfTesting, we recognize the importance of genetic insights in pulmonary embolism management, offering advanced genetic testing solutions to healthcare providers and patients. Partner with PatientSelfTesting to leverage genetic knowledge and improve outcomes in SSPE and venous thromboembolism care.
0 notes
Text
The Rise of Tech-Driven Therapies: Reshaping the Global Intravascular Imaging Market
The global intravascular imaging market is expected to reach a value of more than US$ 656.29 million by 2033, indicating that it will continue to grow. Based on industry estimates, this upswing implies a Compound Annual Growth Rate (CAGR) of 5.4%, expanding upon an estimated market size of US$ 387.8 million in 2023.
Claim Your Exclusive Report Sample Preview:
https://www.futuremarketinsights.com/reports/sample/rep-gb-9926
For the diagnosis and management of cardiovascular disease, intravascular imaging is essential. These sophisticated imaging methods give medical professionals a thorough understanding of the blood vessel inside, enabling them to:
Diagnose blockages and abnormalities in coronary arteries.
Guide minimally invasive procedures like stent placement.
Monitor treatment effectiveness.
Market Growth Driven by Multiple Factors:
Several key trends are propelling the intravascular imaging market forward:
Rising Cardiovascular Disease Rates: The increasing prevalence of conditions like deep vein thrombosis and coronary artery disease is driving the demand for accurate diagnostic tools.
Improved Image Quality: Advancements in imaging technology are leading to the development of intravascular imaging systems with superior image resolution and clarity.
Growing Adoption of Minimally Invasive Procedures: The minimally invasive nature of intravascular imaging techniques is fostering their adoption in clinical settings.
Focus on Enhanced Patient Care: Intravascular imaging empowers physicians to make more informed decisions, ultimately improving patient outcomes.
In an effort to cut healthcare expenses, physician offices and institutions are driving up demand for intravascular imaging. The need for cost-effectiveness, flexibility, and downsizing has contributed to the growing use of intravascular imaging systems.
It is anticipated that firms will continue to push the boundaries of technology in their diagnostic equipment manufacturing, driving intravascular imaging sales and expanding the intravascular imaging market share. Globally increasing rates of heart disease with coronary occlusion, deep vein thrombosis, and other illnesses are predicted to drive up patient traffic in diagnostic centers and propel the growth of the intravascular imaging market.
Key Takeaways:
The United States is predicted to reach US$ 700 million by 2033.
The United States is predicted to increase at a 5.6% annual rate.
The intravascular imaging market in the United Kingdom is expected to reach US$400 million by the end of the forecast period.
China’s intravascular imaging industry is anticipated to be worthUS$850 million.
The intravascular imaging market in Japan is expected to develop significantly, reaching US$ 700 million by 2033.
“Due to the increased effectiveness of intravascular imaging methods for the diagnosis of blood vessel disease, broad adoption of intravascular imaging is expected to significantly increase the popularity of intravascular imaging while accelerating intravascular imaging revenue growth,” says an FMI analyst.
Competitive Landscape:
In order to boost their chances of making sales abroad, the top companies in the intravascular imaging market are working to expand the reach of their products. Interregional and international market companies working together, merging and acquiring, and forming partnerships are also anticipated to encourage the growth of the intravascular imaging market share.
Some of the top key players in the intravascular imaging market include Acqiris, NIDEK CO. LTD., AGFA Healthcare, Aculight Carl Zeiss AG, Heidelberg Engineering Inc., Optopol, Sonostar Technologies Co.Ltd., OPKO Health, AlazarTech and others.
Siemens Healthineers implemented Luminos Impulse in September 2021, a fluoroscopy technology with an innovative layout and features shared by high-end fluoroscopy systems such as a seamless imaging chain, complete dose optimization, cybersecurity features, and detector-sharing capabilities for radiography.
Siemens Healthineers unveiled Somatom X.ceed in May 2021, a unique high-resolution, rapid speeds CT (computed tomography) scanner designed specifically for extremely demanding clinical applications where time and precision are critical.
Avinger Inc. announced the entire business launch of their TigereyeTM image-guided chronic total occlusion (CTO) crossing system in January 2021.
Segmentation Analysis of the intravascular imaging Market
By Product Type:
Instruments
Software
By Modality:
Handheld
Trolley Mounted
By End User:
Hospitals
Diagnostic Imaging Centers
Ambulatory Surgical Centers
Long Term Care Centers
Others
By Region:
North America
Latin America
Western Europe
Eastern Europe
South Asia & Pacific
East Asia
The Middle East & Africa
0 notes