#retroperitoneal
Text
Brunette Amateur teen dildo ass gaping and farting
Amigo meu de JardimSP(Rec) na brotheragem com outro cara
NARUTO - HAVING SEX WITH SAKURA HINATA AND TSUNADE, SEX SCENES ONLY Part10
Blonde doll experiences hardcore double anal
Moscow Teen Hardcore Rough Ass Fuck
La Vore Girl vs Bumper Humper
Sabrina Ravelli Tanga
CHEATING MOM convinces me to TREAT MY DICK TOO
Lela Star And Friend Have Hot Lesbian Milf Sex On Her Snapchat
Petite blonde teen hd and secretary babe Tender Sex in Jacuzzi
#strongest#douser#phones#favorite#inclavate#epipedometry#ceorls#scoptical#retroperitoneal#cyanoauric#equalling#Chiayi#autosymbolic#lava#self-shelter#wad#sevgili#goldenpert#hafis#neuronal
0 notes
Text
Pool sex with brother and sister
Squelching cunt of a wicked fake cop is drilled without mercy
Girlsway Lesbian Anal With Abella Danger & Angela White
Lovely teen Jessie Rogers cums from lovestick riding
Hairy MILF Pussy Takes Knotted Girthy Dildo - Laszloa the Baddie
big m casino myrtle beach jackpot winners
ho-chunk casino wisconsin dells
Lesbian Tits Worked Hard
yummy finger of young pinay girl
Amateur babe gives the BEST HEAD EVER
#retroperitoneal#cyanoauric#equalling#Chiayi#autosymbolic#lava#self-shelter#wad#sevgili#goldenpert#hafis#neuronal#alkalifies#embitters#earth-mad#tin-whistle#mistion#foret#lath-backed#penicilliform
0 notes
Text
“The water goes under the bridge.”
About the ureter and the gonadal artery.
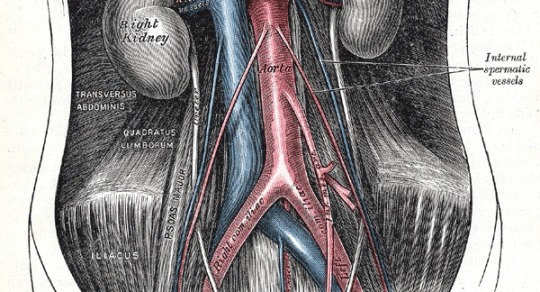
#medicine#med school#medblr#surgery#anatomy#gynecology#urology#colonic surgery#I’ll just say ‘gonadal’ bc it just makes more sense#at least whilr still in the retroperitoneal space
47 notes
·
View notes
Text
The Role for Pre-Polymerized Sucralfate in Management of Erosive and Non-Erosive Gastroesophageal Reflux Disease – High Potency Sucralfate-Mucin Barrier for Enteric Cytoprotection
Abstract
Clinical outcomes from standard sucralfate do not justify a role in the management of erosive and non-erosive gastroesophageal reflux disease. Pre-polymerized sucralfate, sometimes called high potency sucralfate or polymerized cross-linked sucralfate is a new sucralfate formulation recognized by the US FDA in 2005. Positive clinical data from three randomized controlled trials using pre-polymerized sucralfate for GERD and NERD was first reported in 2014 AGA’s Digestive Disease Week (DDW). Gastric refluxate contains protonic acid, dissolved bile acids and proteases each of which cause classic mucosal reactions in the esophageal epithelium. These reactions are symptomatic but may or may not involve erosions. Pre-polymerized sucralfate utilizes biophysical means to exclude all three irritants from epithelial mucosa.
Being non-systemic, the entire clinical effect of any sucralfate rests in the surface concentration of sucralfate achieved. Pre-polymerized sucralfate, presented in 2014 DDW, and discussed here, achieves a surface concentration that is 800% greater than standard sucralfate on normal mucosal lining and 2,400% greater on inflamed or acid-injured mucosa, making it most certainly, a high potency sucralfate. To understand the biomolecular basis of its clinical effect, this review re-introduces the reader to mucosal barrier, discloses the exact site of engagement of sucralfate (mucin within the mucous gel), and how transient sucralfate-mediated biostructural changes in extra-cellular mucin is translated into intra-cellular signaling that modules the mucosal reaction to refluxate. This represents significant enteric cytoprotection.. A broad-based literature review will not only aid understanding of the molecular basis of sucralfate’s clinical effects but will also provide context for an informed impression of whether pre-polymerized sucralfate has a role in the management of GERD and NERD.
Read More About This Article : https://irispublishers.com/ajgh/fulltext/the-role-for-pre-polymerized-sucralfate.ID.000531.php
Read More Iris Publishers Google Scholar Article: https://scholar.google.com/citations?view_op=view_citation&hl=en&user=Wws4PocAAAAJ&cstart=20&pagesize=80&citation_for_view=Wws4PocAAAAJ:4TOpqqG69KYC
0 notes
Text
Okay, so semi-serious anatomy and physiology analysis!
At this point, with how big Bad's back wound is, you could probably reach in and touch his kidneys where they sit in the retroperitoneal space! You could probably also touch most of his other internal organs!
Please say a prayer for his immune system. If the soul vulture infection doesn't get him, I know wound infection fucking will!!
Once again, Ghosties, rip in peace!!!
#qsmp#qsmp analysis#qsmp badboyhalo#tw body horror#cw gore#<- hopefully these work feel free to tell me to tag further if necessary
64 notes
·
View notes
Note
So this is for writing, how fast do you bleed out from a ruptured organ? Is it seconds or minutes or hours or even days? What do you feel and what should someone do in said situation
Oh honey, that depends entirely on the organ.
Ruptured lung? Depends on the amount of damage, but a pneumothorax is more likely than a hemothorax. And that’ll crush your organs and asphyxiate you depending on severity.
Ruptured heart? Yeah, uh, bye bye. Ask me about cardiac tamponade.
Ruptured spleen? You’ll bleed out fairly quickly, but not immediately. Also spleens tear like tissue paper. 😒 I have a beef with them.
Ruptured liver? Please no. They’re such vascular organs. Please no.
Ruptured bowel? You won’t die immediately but boy will you get an infection. And probably lead to sepsis and massive organ dysfunction and eventually dying.
Ruptured kidneys? Not the beans! They do so much for you, a retroperitoneal bleed might take a few days to catch or kill.
So yeah. It depends. :) But any injury can be minor and just kind of… leak. Until it becomes a bigger problem.
#you ask skye answers#lovely anon#Skye talks medical stuff#the amount of times I’ve had trauma patients with ruptured spleens I swear#It’s a dumb organ#Such a drama queen organ#You sneeze on it and it squeaks and explodes
41 notes
·
View notes
Text
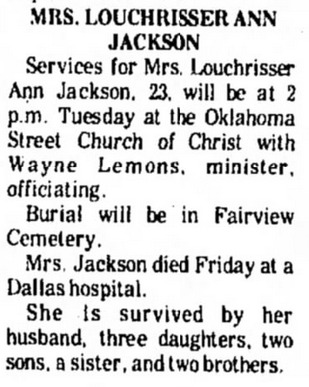
Louchrisser Jackson, 23 (USA 1977)
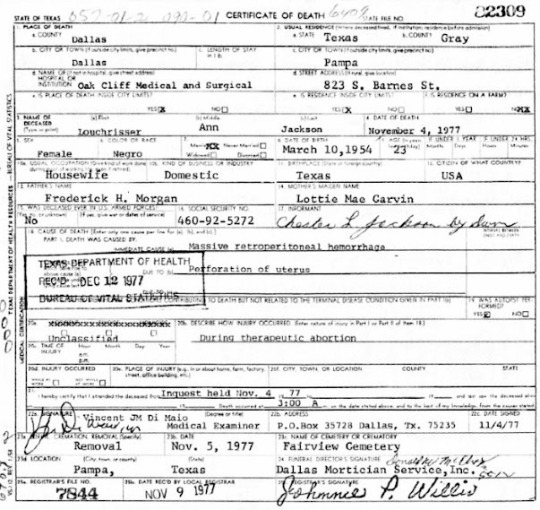
Louchrisser Jackson was 23, married and in the first trimester. At 12 weeks pregnant she went to get an abortion at Reproductive Services in Dallas on November 4, 1977. The abortionist was Robert L. Gardner.
Gardner severely tore Louchrisser’s uterus and she started bleeding badly. The abortion facility didn’t have blood for emergency transfusions on hand, so Gardner administered his own blood— which did not match Louchrisser’s blood type and just made everything even worse.
A private ambulance was called but was not told what was happening. In that jurisdiction, private ambulances were only permitted to transport stable patients and were actually not allowed to respond to emergency calls. Because the ambulance service had no reason to expect an emergency, they did not respond promptly or refer the transport to the fire department's ambulance service, which was actually equipped for emergencies.
When the ambulance crew arrived, Louchrisser was in cardiac arrest. The crew, upon discovering that they'd secretly been called for an emergency transport, rushed Louchrisser to the hospital immediately.
On that same day, Louchrisser died. Gardner tried to cover up what he’d done to her by requesting that the body be released without an inquiry. A doctor at the hospital became suspicious about the request and requested an inquiry. It was a good thing that somebody caught the cover-up before the chance for an autopsy was lost.
The autopsy found massive hemmorage of at least two liters of blood, and a "1.8 x 2 cm. ragged perforation in the right lateral wall just above the internal os of the cervical canal. This perforation communicates freely with the retroperitoneal space on the right side. The endometrial surface of the uterus is ragged and hemorrhagic." Death was attributed to "massive retroperitoneal hemorrhage due to perforation of the uterus during a therapeutic abortion." How a medically unnecessary operation that killed Louchrisser could have possibly qualified as “therapeutic” was not explained.
Later another client (21-year-old Claudia L.) petitioned the state to close the facility and it was discovered that the facility allowed employees with no medical degree to give medical advice and perform medical procedures, clients were not informed of the risks of their abortions and there was still no emergency equipment on hand.
Gardner himself confessed that Reproductive Services ran "an assembly-line operation." He admitted the facility took only one or two minutes between operations, used black-tarnished surgical instruments and 'switched sterile gloves between operations but never scrubbed down.'
Louchrisser left behind a husband and her 5 surviving children.
Dallas Times Herald June 20, 1978
Dallas Morning News June 20, 1978, June 23, 1978, and July 28, 1978
Texas Autopsy Report No. 2262-77-1103
#tw ab*rtion#tw abortion#tw blo0d#tw murder#tw death#pro life#pro choice#abortion#abortion debate#unsafe yet legal#black lives matter#unsafe but legal#abortion is not healthcare
5 notes
·
View notes
Text

PSMA PET can also help DOWNSTAGE some patients. This is an example of a patient who had an enlarged retroperitoneal lymph node (red arrow). Based on CT alone, this is highly suspicious for metastasis, however, on the PET scan this is not PSMA-positive and as such is not a metastasis (note the primary tumor is PSMA-positive - blue arrow). The patient was thus staged as N0M0. Image credit: Novartis.
#TeachingRounds#FOAMed#FOAMRad#Radiology#NuclearMedicine#nucmed#PETCT#PSMA#prostatecancer#theranostics#oncology#urology
3 notes
·
View notes
Text
“Hey. How are you holding up?” Petra - Dr. Allison, her anesthesiologist 2 years out of residency but would also ignore her if she addressed her like an attending - asked as she sidled up right next to her on the bench she sat on. In the other girl’s hands was a can of Coke, which she then passed over to her.
She calmly accepted the can with shaking hands before resting it against her head. Only then did she noticed it was warm.
“Sorry, Lab wouldn’t let me sneak it in the blood bank fridges,” the dark-haired girl grinned, seeing the clear disappointment on her face, “Cold drinks are a bit of a luxury anyway. How are you holding up?”
She stared at the can of soda, passing it from one to another.
“No one’s ever done a surgery like that before, ” Euridice sighed as she cracked open the can of warm soda, “ and me not having completed even my first year in surgery thought I could do it.”
She pressed her hand over her face and then tilted her head towards the starry sky above.
“Believed all the hype my mentors heaped on me - the next best thing since the scalpel,” she chuckled painfully, “And now I feel like I just killed my patient with my hubris.”
Petra didn’t reply. She simply stared at her with calm brown eyes as if inviting her to continue.
“I don’t know what I could’ve done differently,” she continued, “But is that because there was nothing else that could’ve been done or is it because I just don’t have the experience to think of it?”
“Maybe start out by thinking about what you did do?” Petra said with a small smile, “Talking out loud usually helps me think.”
Euridice drank another mouthful of warm soda as she recalled the surgery an hour prior.
“...We managed to get an IO line in with minimal bleeding from the drill. The man’s tough tissues which made things difficult at first helped with the tamponade afterwards,” Euri said, “and then we started transfusion as intended. While that was running, I attempted to cut through the exposed portions of abdomen with the scalpel to no avail, hence why I went for the bone saw.”
“It worked, and I was able to open up the surgical field. And I didn’t nick anything important,” she said with a frown, “Maybe I was too cautious at the time. I felt like I could’ve done it faster...but at the same time, the skin and fascia could’ve just given way like a piece of plastic, and I could’ve end up cutting the bowel and vessels underneath.”
“So you probably couldn’t have opened up the surgical field faster then. What else?”
“I had to get to the suspected bleed,” she continued on, feeling more calm than distressed as she continued, “there was definitely injured small bowel throughout the abdomen, but it was the bleed that was going to kill him first.”
“Given the trajectory of whatever pierced him, I suspected he nicked something retroperitoneally, likely his aorta. Blood was leaking from the abdomen as I dissected the mesentery and eventually the IVC away using a scalpel. A lycan’s innards seem to be far less resistant to trauma than his skin and muscle.”
“I saw the blood spurting out of the aorta. I tried to start preparations for the repair...” she gritted her teeth.
“But that’s when he started crashing.”
“I don’t get why he had to start crashing then,” Euridice closed her eyes before standing straight up, anger boiling in her chest as she screamed at the sky. “You idiot! You’ve endured for so long! You were so close! Just ten minutes more! Ten minutes...”
She could feel something hot on her face, which she wiped with her sleeve. And then a soft touch on her shoulder.
Petra sighed, having stood up with her and a hand on her shoulder, “You know that’s a lie. Just setting up the bypass as well as clamping of the aorta would’ve needed more time than that.”
“I could’ve accessed endovascularly through the iliac artery from the star-.”
“Blindly? When you didn’t even know where the aortic injury was or that there was one?” Petra sarcastically countered, “Didn’t realize you were a psychic, Euri, or had such a reckless streak in you.” Petra flicked her in the cheek.
“Hey. Watch it,” she frowned as she rubbed the spot. Petra stepped back, expression serious.
“Look. I’ve seen surgeons - attending-level surgeons - make stupid mistakes in cases far simpler than the one you just performed - outpatient cases where they had infinite time to mull over what they would do. And still blow it,” Petra said with the confidence of experience. “There was nothing more you could’ve done. And we just went over the reasons why.”
“Not to mention,” Petra continued, “At least you gave this person a fighting chance. I guarantee if it was anyone else on call tonight, they would’ve just let him die, even before seeing those intraosseous needles fail to go through.”
“So stop moping,” Petra finished, voice all business now, “We still have a job to do, and I can’t have the surgeon on call off her A-game.”
She’s right. There’s still work to do.
“There we go. That’s a better look on you, Dr. Ariston,” Petra nodded with a smile as she stood up, “Well, you know where to find me if there’s a case to do. See ya around, Euri.”
“Umm yeah. Bye. And thanks.”
The other woman hummed in reply as she walked towards the rest tents.
She looked at the warm can of soda in her hands and chugged the rest down.
“Right... Still got a job to do, Euri.”
3 notes
·
View notes
Text
Cancer Treatment: Types and Treatments awareness
Cancer is a serious illness that affects many people around the world. There are different types of cancer, and each one needs its own kind of treatment. In this blog, we will talk about cancer and the surgeries used to treat it by taking reference from blogs of Dr. Harshit Srivastava — best surgical oncologist in Lucknow. Whether you’re someone with cancer, taking care of someone with cancer, or just interested in learning about cancer treatment, this blog is for you.
Oncoplastic Surgery
There are surgeries now that can help treat breast cancer without removing the whole breast. These surgeries focus on removing the cancer while still keeping the breast looking as normal as possible. This gives hope to people who have had breast cancer.
Gastrointestinal Cancers: The Silent Threats
Cancers in the stomach and intestines can be hard to find early because they don’t always show clear signs. But with new tests and treatments, there’s hope for people with these cancers. Finding them early and using different treatments together can help people live better.
Liver, Pancreas, and Bile Duct Cancers: Hepato-Pancreatico-Biliary Malignancies
Cancers in the liver, pancreas, and bile ducts can be very dangerous because these organs are important for digestion. Surgery is often needed, but there are also new treatments that can help fight these cancers. By working together, doctors can give people with these cancers better chances of getting well.
Gynecological Cancers: What Every Woman Should Know
Cancers like ovarian, cervical, and uterine cancers affect women in different ways. But with more knowledge about the signs and tests, women can get help earlier. New treatments are also being studied to help women with these cancers live longer and better lives.
Genito-Urinary Cancer: Cancers in the Reproductive System
Cancers in the reproductive system, like prostate and ovarian cancers, can be tricky to treat. But there are many ways to help, like surgery and new kinds of treatments. Doctors are always learning more about how to help people with these cancers.
Retroperitoneal Tumors: Understanding Rare Tumors
Some tumors are in places that are hard to reach, like behind the stomach. These tumors are rare and can be tough to treat. But with doctors from different specialties working together, people can have a better chance of beating these tumors.
Fighting Cancers in the Head and Neck
Cancers in the head and neck can be caused by smoking, drinking, or certain viruses. But there are many ways to treat these cancers, like surgery, radiation, and special medicines. People with these cancers can now have more hope for getting better.
Lung and Thoracic Cancer
Lung and chest cancersare some of the most common cancers. But with new tests and treatments, more people are surviving these cancers. Doctors now have many tools to help people with lung and chest cancers live longer.
Dealing with Bone and Soft Tissue Tumors
Tumors in bones and soft tissues can be scary, but there are treatments that can help. Surgery is often needed, but there are also other treatments like chemotherapy and radiation. Doctors are also studying new ways to help people with these tumors.
Conclusion
The landscape of cancer care is constantly evolving, driven by advances in technology, research, and clinical practice. From oncoplastic surgery to targeted therapies and immunotherapies, patients with cancer now have more treatment options than ever before. However, challenges remain, and the fight against cancer requires a collaborative effort involving patients, caregivers, healthcare providers, and researchers. Together, we can continue to make strides in the prevention, detection, and treatment of cancer, offering hope and healing to individuals and families affected by this formidable disease.
0 notes
Text
Marinha resgata mulher inglesa de 87 anos a bordo de navio de passageiros ao largo dos Açores
A Marinha resgatou uma mulher inglesa, de 87 anos, que se encontrava a bordo de um navio de passageiros, a sudoeste da ilha de São Miguel, nos Açores, que necessitava de cuidados médicos hospitalares imediatos.

De acordo com um comunicado da Marinha, o resgate, iniciado pelas 17h30 locais (18h30 em Portugal Continental) de quarta-feira e concluído pelas 01h50 locais (02h50 em Portugal Continental) de sexta-feira, foi efetuado através do Centro de Coordenação de Busca e Salvamento Marítimo de Ponta Delgada (MRCC Delgada), em articulação com o Centro de Orientação de Doentes Urgentes - Marítimos (CODU-MAR) e com o Centro de Coordenação de Busca e Salvamento Aéreo das Lajes (RCC Lajes).
Segundo a nota, tratou-se do resgate médico de uma mulher que se encontrava a bordo do navio de passageiros "AMBITION", com bandeira das Bahamas, que estava a navegar a cerca de 850 milhas náuticas (o equivalente a cerca de 1.600 quilómetros), a sudoeste da ilha de São Miguel.
"A passageira, de nacionalidade inglesa, apresentava um quadro clínico de dor aguda no abdómen e hemorragia retroperitoneal, necessitando de cuidados médicos hospitalares imediatos", lê-se.
A Marinha explicou que o resgate foi efetuado pelo helicóptero EH-101 da Força Aérea Portuguesa (FAP), que transportou a paciente para o aeroporto das Lajes, na ilha Terceira, tendo sido posteriormente transferida para uma unidade hospitalar.
Estiveram envolvidos na operação o MRCC Delgada, o RCC Lajes, a FAP, o Serviço Regional de Proteção Civil e Bombeiros dos Açores (SRPCBA) e o Centro de Comando Operacional da Unidade de Controlo Costeiro e de Fronteiras da GNR.
0 notes
Text
Dr. Tapan Singh Chauhan - Surgical Oncologist in India

Dr. Tapan Singh Chauhan is a distinguished MCh Surgical Oncologist renowned for his expertise in gastrointestinal (GI), hepatopancreaticobiliary oncology, and peritoneal surface malignancy, particularly Hyperthermic Intraperitoneal Chemotherapy (HIPEC). With a stellar academic background and extensive training from premier oncology institutes, Dr. Chauhan has emerged as a leader in the field, known for his proficiency in complex surgical procedures and minimally invasive techniques.
Educational Background and Training
Dr. Chauhan's academic journey began with an MS in General Surgery from Pt. B.D. Sharma PGIMS Rohtak, followed by specialized training in Surgical Oncology from renowned institutions such as Dr.B.R.A.IRCH, AIIMS, New Delhi, and Gujarat Cancer Research Institute, Ahmedabad. Driven by his passion for GI oncology and minimally invasive surgery, he pursued further fellowship positions under distinguished mentors, including Prof. Marcus Buechler in Heidelberg (HPB oncology) and Dr. T. Subramaneshwar Rao at Indo–American Cancer Institute, Hyderabad, focusing on MIS techniques.
Clinical Expertise and Specializations
Dr. Chauhan's expertise spans a wide range of complex surgical procedures, including but not limited to:
Esophagectomy (open and laparoscopic)
Radical Gastrectomy with D2 Dissection
Radical Cholecystectomy
Whipple's Surgery
Distal pancreatosplenectomy
Hepatectomy
Hemicolectomy, subtotal, total colectomy (open and laparoscopic)
Anterior resection, Low anterior resection, ULAR, APR (open and laparoscopic)
Retroperitoneal Lymph Node Dissection (RPLND) and Retroperitoneal Sarcoma Excision
Radical Cystectomy and Radical total and partial Nephrectomy
Cytoreductive surgeries (CRS) and HIPEC for various cancers, including ovarian, colorectal, mesothelioma, pseudomyxoma, and gastric cancer
Gynecological surgeries for uterine cancer, carcinoma cervix, and ovarian cancer, including fertility-preserving surgeries.
Professional Achievements
Dr. Chauhan's contributions to the field of surgical oncology extend beyond clinical practice, with numerous publications in esteemed journals and paper presentations at national and international conferences. His dedication to advancing the field through research and innovation, coupled with his commitment to providing optimal patient care, has earned him recognition as a leading authority in GI oncology and complex surgical interventions.
Current Practice
As a leading surgical oncologist, Dr. Tapan Singh Chauhan continues to push the boundaries of excellence in cancer care, offering advanced treatment options and compassionate care to his patients. His unwavering commitment to improving outcomes and enhancing the quality of life for individuals battling cancer underscores his status as a true leader and innovator in the field of surgical oncology.
0 notes
Text
Exploring the Enigma Where is the Pancreas Located
The pancreas is a vital organ in the human body, playing a crucial role in both the endocrine and digestive systems. Nestled deep within the abdomen, this organ remains relatively inconspicuous despite its essential functions. In this article, where is pancreas located we will unravel the mystery and delve into the question: Where is the pancreas located?
Anatomy of the Pancreas:
The pancreas is a glandular organ situated behind the stomach, adjacent to the small intestine. It has a unique dual function, serving as both an endocrine and exocrine organ. The majority of the pancreas is composed of exocrine tissue, responsible for producing digestive enzymes that aid in the breakdown of food in the small intestine. Additionally, the pancreas houses clusters of cells known as the islets of Langerhans, which function as endocrine cells and secrete hormones such as insulin and glucagon into the bloodstream to regulate blood sugar levels.
Location in the Abdomen:
To pinpoint the precise location of the pancreas, one must explore the upper abdominal region. Specifically, the pancreas is situated horizontally behind the stomach and extends from the duodenum, the first part of the small intestine, to the spleen. The head of the pancreas is nestled within the curvature of the duodenum, while the tail extends towards the spleen on the left side of the abdomen.
For a more accurate understanding, envision the pancreas lying deep within the retroperitoneal space, which is located behind the peritoneum – the membranous sac that lines the abdominal cavity. The retroperitoneal position of the pancreas provides stability, protecting it from external forces and allowing it to fulfill its vital functions without interference.
Surrounded by neighboring organs such as the liver, gallbladder, and spleen, the pancreas establishes intricate connections with the digestive and circulatory systems. Its proximity to the stomach and small intestine facilitates the efficient release of digestive enzymes, while its endocrine role ensures the regulation of blood glucose levels in coordination with the insulin-producing islets.
Clinical Significance:
Understanding the location of the pancreas is essential for medical professionals, as it aids in the diagnosis and treatment of various pancreatic disorders. Conditions such as pancreatitis, pancreatic cancer, and diabetes mellitus can affect the functionality of this organ, emphasizing the importance of accurate anatomical knowledge.
Conclusion:
In conclusion, the pancreas is a remarkable organ tucked away in the depths of the abdomen, playing a multifaceted role in maintaining the body's homeostasis. Its dual function as an exocrine and endocrine organ underscores its significance in both digestion and metabolic regulation. As we unravel the enigma of where the pancreas is located, we gain a deeper appreciation for this organ's intricate contributions to our overall health and well-being.
0 notes
Text
Life as a Senior NCO for a Head of Household that can't Provide.
No...... Brainer.
Now, settle the term "ill-gotten" in its power to claw back.
If you can't, you still have the power as a U.S. Citizen to relinquish your assets to a Fiduciary Institution.
Otherwise, you need to be aware of what people are responsible for when they make the calls that guide our economy.
But, you balk. And that's clear enough for me.
Sergeant Major Nathan Marksmith, North Wales Militia/ Joint Militia Detachment
------
0 notes
Text
“Hannah Roe,” 29 (USA 1978)
A medical journal published two cases of death by uterine rupture after legal saline-oxytocin abortion. The authors noted that although the association between oxytocin administration and uterine rupture in pregnancy was well-established, it was common for abortionists to administer oxytocin in combination with saline for abortions.
One of the women killed is “Hannah Roe”. She was 29 and pregnant for the 4th time. She was approximately 20 weeks pregnant when she underwent a saline-oxytocin abortion in a hospital. She had never had any uterine surgery in her life. Hannah was obese, which made abortion in general riskier for her.
The abortion was started by removing 40 ccs of amniotic fluid and injecting 200 ccs of saline. The following events show a timeline of Hannah’s decline and death. All timeframes are counting from the start of the abortion. Please note that amounts of time are approximate.
4 hours: Hannah was given IV oxytocin, which was intended to speed up the abortion.
24 hours: Even though she had already had 60u of oxytocin, Hannah was given another 40u through IV.
27 hours: Hannah was very pale and her blood pressure was registered at 70/30. A pelvic exam showed mild bleeding. An additional 60u of oxytocin was administered.
27 hours and >10 minutes: Hannah suffers from profuse vaginal bleeding.
After her bleeding became severe, Hannah was rushed to the operating room. Her dead child and the placenta were manually removed and the uterus was examined, but no defect was found at the time. Hannah was given 2 units of whole blood and fibrinogen to treat the bleeding. Then she was transferred to another hospital that had a better blood bank.
At the second hospital, Hannah’s blood pressure was only 40/0 and her hematocrit level was 20%. Her abdomen was full of blood. Doctors administered more blood transfusions, but Hannah’s condition was too critical for surgery. 5 hours and multiple cardiopulmonary arrests later, Hannah was declared dead.
The autopsy revealed a transverse rupture of Hannah’s right lower uterine segment. The rupture was half as long as the entire wall. In addition to the intraperitoneal hemorrhage, an estimated 1,500 ccs of blood was found retroperitoneally.
The case report also noted that similar uterine ruptures had been caused by prostaglandin abortions augmented with oxytocin.
(Hannah Roe is Patient 2)
#pro life#tw abortion#abortion#pro choice#tw murder#abortion debate#tw ab*rtion#unidentified victim#unsafe yet legal
3 notes
·
View notes