#Breast cancer overdiagnosis
Text
Unveiling the Truth: Breast Cancer Overdiagnosis Among Women Over
Understanding Breast Cancer Overdiagnosis: A Comprehensive Insight
Breast cancer stands as a significant concern for women across all age groups, with increased prominence as women reach their 70s and beyond. Recent years have witnessed mounting evidence of breast cancer overdiagnosis within this demographic, sparking critical debates about the efficacy and appropriateness of screening…

View On WordPress
#Age-specific screening#Breast cancer overdiagnosis#Cancer awareness#Elderly breast health#Health disparities#Healthcare decisions#Medical interventions#Screening guidelines#Shared decision-making#Women over 70
0 notes
Text
The Treatment-Prevalence Paradox
More widely available treatment ought to abate the rate (and severity) of disease.
Take breast cancer, pitiless killer of over forty thousand American women each year. As early detection and treatment for breast cancer improved since 1989, rates of death from breast cancer plummeted. Or maternal mortality: as antibiotics became more readily available, rates of maternal death in childbirth collapsed. Better and more widely available dental care has meant fewer toothless Americans. And as we developed immunizations and cures for childhood illness, child mortality rates nose-dived.
And yet as treatments for anxiety and depression have become more sophisticated and more readily available, adolescent anxiety and depression have ballooned.
I’m not the only one to have found something fishy in the fact that more treatment has not resulted in less depression. A group of academic researchers recently noticed the same. They published a peer-reviewed paper titled “More Treatment but No Less Depression: The Treatment-Prevalence Paradox.” The authors note that treatment for major depression has become much more widely available (and, in their view, improved) since the 1980s worldwide. And yet in not a single Western country has this treatment made a dent in the incidence of major depressive disorder. Many countries saw an increase.
“The increased availability of effective treatments should shorten depressive episodes, reduce relapses, and curtail recurrences. Combined, these treatment advances unequivocally should result in lower point-prevalence estimates of depression,” they write. “Have these reductions occurred? The empirical answer clearly is NO.”
I checked with several of the paper’s authors. Two confirmed that the same might be said for anxiety. As treatment has become more widely available and dispersed, point-prevalence rates should go down. They have not. And while the authors admit that there was likely more depression in the past than we realized, they argue that there is at least as much, and probably more, depression now.
After generations of increased intervention, that shouldn’t be the case. More access to antibiotics should spell fewer deaths from infection. And more generally available therapy should spell less depression.
Instead, adolescent mental health has been in steady decline since the 1950s. Between 1990 and 2007 (before any teens had smartphones), the number of mentally ill children rose thirty-five-fold. And while overdiagnosis or the expansion of definitions of mental illness may partially account for this rapid change, it is hard to dismiss or contextualize away the startling rise in teen suicide: “Between 1950 and 1988, the proportion of adolescents aged between fifteen and nineteen who killed themselves quadrupled,” The New Yorker reported. Mental illness became the leading cause of disability in children.
Yes, the coincidence of these two trends—deteriorating mental health in an era of vastly expanded awareness, detection, diagnosis, and treatment of psychological disorders—may be just that: coincidence. It does not unveil a causal arrow. But it is peculiar. At the very least, it may provide a clue that many of the treatments and many of the helpers aren’t actually helping.
-- Abigail Shrier, Bad Therapy
4 notes
·
View notes
Text
General health screenings

Health Screenings
General health screenings are a fundamental aspect of preventive healthcare, serving as an early detection tool for various diseases and health conditions. They are designed to identify risk factors and early signs of illness, ideally before symptoms become apparent. This approach aims to improve outcomes by starting treatments early, possibly before a disease progresses to a more severe stage.
Importance of Health Screenings
Health screenings are critical because they can detect potential health issues when they are most treatable. Early detection of diseases such as cancer, diabetes, and heart disease can significantly increase the chances of successful treatment and reduce the risk of serious complications or death. For instance, screenings like mammograms for breast cancer and colonoscopies for colorectal cancer can catch these diseases in their early stages when they are most responsive to treatment.
Types of Health Screenings
Health screenings vary based on age, sex, and medical history. Common types include:
Blood Pressure Screening: High blood pressure (hypertension) is a major risk factor for heart disease and stroke. Regular screenings help manage this silent condition before it causes significant harm.
Cholesterol Checks: High cholesterol is associated with an increased risk of coronary artery disease. A lipid panel is used to check the level of cholesterol and triglycerides in the blood.
Cancer Screenings: Various tests are used to detect different types of cancer. Pap smears for cervical cancer, mammograms for breast cancer, and PSA tests for prostate cancer are some examples. These screenings are recommended based on guidelines that consider age and risk factors.
Diabetes Screening: Blood tests measure blood sugar levels to detect diabetes and prediabetes, conditions that are often asymptomatic in their early stages but can lead to serious health issues.
Bone Density Screening: This screening is recommended for postmenopausal women and older adults at increased risk of osteoporosis. It measures bone strength and helps prevent fractures.
Body Mass Index (BMI) and Obesity Screening: Obesity is a significant risk factor for several diseases, including diabetes, heart disease, and certain cancers. BMI screenings help identify individuals who are at risk due to their weight.
Benefits of Regular Health Screenings
The primary benefit of regular health screenings is the potential to save lives by preventing serious diseases or detecting them early enough for effective treatment. Screenings can also prevent complications by managing conditions like diabetes and hypertension early on. Furthermore, they provide an opportunity for individuals to discuss lifestyle changes with healthcare providers to improve their overall health and wellness.
Challenges and Considerations
While the benefits of health screenings are significant, there are also challenges and considerations to keep in mind:
Overdiagnosis and Overtreatment: Some screenings can lead to overdiagnosis, detecting conditions that may never cause symptoms or death. This can lead to unnecessary anxiety and treatment, which might have its own risks.
Access and Inequality: Access to health screening services can vary greatly depending on geographical location, socioeconomic status, and healthcare infrastructure. This disparity can lead to uneven health outcomes across different populations.
Personalized Screening Schedules: Not everyone needs the same screenings at the same intervals. Personal factors such as family history, genetic predisposition, and lifestyle choices should influence the frequency and type of screenings one undergoes.
General health screenings are a vital part of maintaining good health. They offer a proactive approach to managing health risks and detecting diseases early. Regular engagement with healthcare providers for screenings can lead to early interventions, which are often less invasive and more effective, thereby improving the quality of life and reducing healthcare costs over time. However, it's crucial to tailor health screenings to individual needs and consider both the benefits and potential drawbacks. This balanced approach ensures that screenings contribute positively to public health without causing undue harm or anxiety.
0 notes
Text
Overdiagnosis of Breast Cancer in Older Women—and Unnecessary Treatment—Is Widespread: Study
August 20, 2023
BREAST CANCER
Overdiagnosis of Breast Cancer in Older Women—and Unnecessary Treatment—Is Widespread: Study
SHARE* READ MORE
FRONTLINE HEALTH
Doctor Explains Eastern Idea of Energy in Western Terms
SHARE* READ MORE
ADVERTISEMENT:
EDUCATION & FAMILY NEWS
EXCLUSIVE: Transgender Coach Changes in Locker Room With Shocked Pennsylvania High School Students
SHARE* READ…
View On WordPress
0 notes
Text
The Unintended Consequences Of Unnecessary CT Scan Applications
Medical imaging plays a crucial role in diagnosing and treating various health conditions, with CT scans being one of the most common imaging techniques.
However, the increasing prevalence of unnecessary CT scan requests raises concerns about potential risks and consequences.
While CT scans offer valuable insights into the human body, subjecting patients to this imaging procedure without a valid medical indication can lead to a range of unfavorable outcomes.
This article explores the potential consequences of an unnecessary request for a CT scan and emphasizes the importance of judicious and evidence-based use of medical imaging technology.
Radiation Exposure And Cancer Risk:
One of the primary concerns associated with unnecessary CT scans is the exposure to ionizing radiation.
CT scans use X-rays to produce detailed cross-sectional images of the body, and although the radiation doses are relatively low, repeated, or unnecessary exposure can accumulate over time.
Ionizing radiation has been linked to an increased risk of developing cancer, including leukemia, thyroid cancer, and breast cancer.
While the risk of developing cancer from a single CT scan is relatively small, the cumulative effect of unnecessary scans can significantly raise this risk.
Overdiagnosis And Overtreatment:
Unnecessary CT scans can lead to overdiagnosis, which refers to the detection of abnormalities that may never progress or cause harm.
This can result in unnecessary treatments and interventions, subjecting patients to potential risks and increasing healthcare costs.
For example, detecting incidental findings during a CT scan that are unrelated to the initial concern can lead to unnecessary biopsies, surgeries, or further diagnostic tests, causing physical and emotional distress to patients.
Moreover, overdiagnosis can also contribute to overtreatment, where patients receive unnecessary medications or therapies for conditions that may not require intervention.
This can result in adverse effects, unnecessary healthcare expenses, and the diversion of resources from patients who genuinely need them.
Financial Implications:
Unnecessary CT scans not only pose risks to patients' health but also have significant financial implications.
Medical imaging procedures, including CT scans, can be costly, and when performed without a valid medical indication, they contribute to escalating healthcare expenses.
Unwarranted scans strain healthcare systems, increase insurance premiums, and potentially limit access to necessary care for those who cannot afford it.
By avoiding unnecessary imaging requests, healthcare providers can allocate resources effectively, ensuring that patients receive appropriate and timely care while minimizing financial burdens.
Psychological Impact:
Undergoing medical tests, including CT scans, can be a source of anxiety and stress for patients. When a scan is performed unnecessarily, it can heighten patients' concerns and contribute to psychological distress.
False-positive results or incidental findings during unnecessary scans can lead to unnecessary worry, anxiety, and emotional burden.
This can adversely affect patients' mental well-being, leading to sleep disturbances, decreased quality of life, and even unnecessary lifestyle changes prompted by unfounded health concerns.
Conclusion:
The consequences of an unnecessary request for a CT scan extend beyond the immediate health risks.
Unwarranted exposure to ionizing radiation, overdiagnosis, overtreatment, financial implications, and psychological impact highlight the importance of avoiding unnecessary scans.
Healthcare providers and patients should engage in informed decision-making, weighing the potential benefits and risks of medical imaging procedures.
By adopting evidence-based guidelines and ensuring appropriate utilization of CT scans, we can protect patients from unnecessary harm, optimize healthcare resources, and foster a more efficient and patient-centered approach to medical imaging.
Exploring the Outcome of Unjustified CT Scan Requests: Connect with Australia's Leading Diagnostic Imaging Centers for Expert Insights and Information.
0 notes
Text
Google partners with a med-tech company to develop AI breast cancer screening tools
Google has licensed its AI research model for breast cancer screening to medical technology company iCAD
The hope is that AI might become a tool to help radiologists and their patients
Commercial deployment, however, still depends on how successful continued research and testing are
Google aims to eventually deploy the technology in real-world clinical settings - targeting a "2024 release"
Generally, medical experts are approaching AI with caution
Relying too heavily on AI without bringing doctors in to assess all the nuances of a patient's health could heighten the risk of overdiagnosis
Information Source: The Verge
0 notes
Text
Blood tests for cancer offer a 'new frontier'—and big challenges
New Post has been published on https://petnews2day.com/small-pets/blood-tests-for-cancer-offer-a-new-frontier-and-big-challenges/
Blood tests for cancer offer a 'new frontier'—and big challenges
New, experimental blood tests may be a “new frontier” in cancer screening, detecting dozens of cancers typically overlooked by standard tests—but some experts worry these tests may ultimately lead to unnecessary treatments, Gina Kolata writes for the New York Times.
A ‘new frontier’ in cancer screenings
Currently, standard cancer screening tests are used to detect breast, colon, cervix, and prostate cancers, but 73% of people who die of cancer have cancers that are not detected by these standard tests.
Experimental blood tests, which look for minuscule pieces of cancer proteins or DNA, may be a “new frontier” in cancer screenings, Kolata writes, and they are being prioritized as part of President Joe Biden’s Cancer Moonshot program. According to the companies developing these tests, including GRAIL and Exact Sciences, the tests can detect dozens of cancers and could reduce cancer death rates by detecting tumors when they’re still small and curable.
In one study, 10,000 female patients ages 65 to 75 in the Geisinger health system were screened using Exact Sciences’ test. In total, the blood test identified 26 patients who had different cancers, including lymphoma, breast cancer, lung cancer, and ovarian cancer. Of these patients, 65% had early-stage disease.
In a separate trial of GRAIL’s test, which involved 6,629 patients, interim data showed the test detected cancer signals in 92 participants. Of these participants, 29 had cancers that were detected by additional tests, such as CT/PET scans and biopsies. Twenty-three of these participants had new cancers, nine of which were early stage, while six participants previously had cancer and were experiencing a recurrence.
According to Tomasz Beer, a cancer researcher at Oregon Health & Science University who is directing GRAIL’s study, a 12-month follow-up of the study participants is forthcoming. “The goal here is to reduce the morbidity and mortality from cancer,” he said. “That is a noble and important effort.”
“I think there’s promise for a real impact,” he added.
Does early detection really result in better survival?
Some researchers and cancer experts have been skeptical of the tests’ benefits, arguing that early detection of cancer may not necessarily mean better survival outcomes for patients.
“Paradoxical as it may sound, finding cancers earlier could mean just as many deaths, with the same timing as without early diagnosis,” Kolata writes. “That is because — at least with current treatments — cancers destined to kill are not necessarily cured if found early.”
In addition, some patients may test positive for cancer, but doctors will be unable to locate any tumors. For example, Susan Bell, a 73-year-old nurse who was part of the Geisinger study, initially tested positive for alpha-fetoprotein, which could indicate liver or ovarian cancer. However, a subsequent PET scan and abdominal MRI failed to find a tumor. Currently, it’s not clear whether Bell’s test was a false positive or if she has a tumor that is too small to detect.
According to Daniel Hayes, a breast cancer researcher at the University of Michigan, situations like Bell’s lead to what he calls “Damocles syndrome,” since “[y]ou’ve got this thing hanging over your head, but you don’t know what to do about it.”
In addition, Susan Domchek, a breast cancer researcher at the University of Pennsylvania, said false positives will become “a real problem” once large numbers of people are being tested. “[W]e need to know what to do with those results and what they mean,” she added.
Patients may be at risk of overtreatment with these tests
Another concern with these blood tests is the potential for overdiagnosis, or “finding small tumors that would never have been noticed and may not have caused any harm,” Kolata writes.
“Some cancers simply fail to grow or are destroyed by the body’s immune system,” Kolata writes. “But without knowing if the cancer is dangerous, it will be treated as though it is, subjecting people to therapies that are often difficult or debilitating and may be unnecessary.”
According to Barnett Kramer, a member of Lisa Schwartz Foundation for Truth in Medicine and a former director of the National Cancer Institute‘s division of cancer prevention, overdiagnosis already occurs with standard screening tests, which can lead to thyroid glands, breasts, or prostates being removed for small tumors that end up being harmless.
And with blood tests looking for dozens of cancers, overdiagnosis, and potentially overtreatment, is likely to get even worse. “We will dip more and more deeply into the iceberg of disease” and find “lesions that look like a cancer to the pathologist but may not have the same natural history at all,” Kramer said.
Overall, if these blood tests become commonplace without concrete evidence to show they are beneficial to patients, it will be “difficult to unring the bell,” Kramer said.
“Everybody loves early detection, but it comes with harms,” said Donald Berry, a statistician at MD Anderson Cancer Center. “The harms, we know. The benefits are very uncertain.” (Kolata, New York Times, 6/10)
!function(f,b,e,v,n,t,s) if(f.fbq)return;n=f.fbq=function()n.callMethod? n.callMethod.apply(n,arguments):n.queue.push(arguments); if(!f._fbq)f._fbq=n;n.push=n;n.loaded=!0;n.version='2.0'; n.queue=[];t=b.createElement(e);t.async=!0; t.src=v;s=b.getElementsByTagName(e)[0]; s.parentNode.insertBefore(t,s)(window,document,'script', 'https://connect.facebook.net/en_US/fbevents.js'); fbq('init', '992099241263762'); fbq('track', 'PageView');
Source link
0 notes
Text
https://youtu.be/ZygnC81LUGQ
youtube
October is Breast Cancer Awareness Month!
So.. I thought I should do this video because, according to the research, the majority of women still don’t know what their personal breast cancer risk is.
According to the research; they also have an inaccurate perception of the benefits/risks that come with regular breast cancer screening.
This video aims to address this because, personally, I believe that patients who are better educated are also patients who are more empowered and can make better decisions regarding their personal health.
In this video, I discuss why breast cancer screening programmes have proved so controversial and why there is so much debate about when to start receiving mammograms and how frequent those mammograms should be.
I'll also explain why overdiagnosis and false positives are two things that worry a whole lot of people and why (in my humble opinion) I think we should aim for a more individualised approach when it comes to breast cancer screening.
Happy Viewing!
#breast cancer awareness month#breast cancer awareness#breast cancer#breast cancer screening#women’s health#know your breasts#breast care#mammogram#mammography#health#science#research#cancer#medicine#Youtube
4 notes
·
View notes
Text
my childhood friend who still lives in our hometown and who i should really unfollow on fb bc she allows local men to comment on her posts about reproductive rights lol shared this super fearmongering meme about breast cancer that listed all these symptoms that “could be breast cancer” and it’s literally every experience one could have with a breast, like the odds of any of these things being cancer are extremely low, but instead of acknowledging that fact or aiming in any way for accuracy the meme was like “everyone needs to see this, share to save a life, etc.” this is a kind of violence aimed at women and other ppl w breasts, feeding the fear of our own bodies and causing us to misspend resources on the breast cancer industry when in fact there is a serious overdiagnosis and overtreatment problem in the bc world, and a HUGE disparity in access to treatment along racial lines
absolutely, do your due diligence as you get older, and be aware of your approximate risk level. but also know that almost all of the sensations we have in our breasts are other things than cancer and don’t live your life anticipating death by boob
58 notes
·
View notes
Link
Screening mammograms have not been found to reduce deaths from breast cancer. Instead, they result in overdiagnosis, which leads to unnecessary anxiety and overtreatment (including mammograms and chemotherapy).
1 note
·
View note
Text
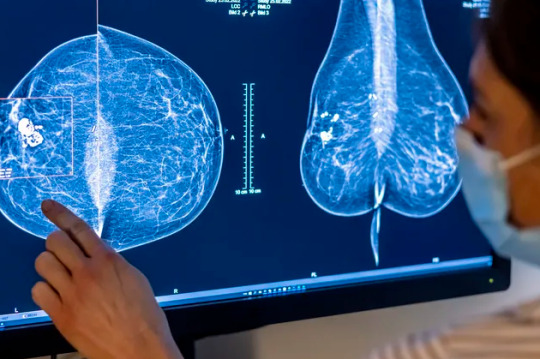
50% of Women Had a False-Positive Mammogram After 10 Years

STORY AT-A-GLANCE
- Data once again show mammograms don't deliver on the promise of effective breast cancer screening as more than half of women in one study had a false positive after 10 years of testing
- In addition to the added risk from radiation in mammograms that triggers fatal cancer in up to 25 of 100,000 women, the screening does not efficiently identify all cancers, especially in women with dense breasts
- Women have choices for screening that do not involve radiation, including thermography, ultrasound and clinical breast examination
- They can also practice healthy lifestyle choices to reduce risk and maintain optimal levels of omega-3 fatty acid and vitamin D
By Dr. Joseph Mercola (Mercola)
The effectiveness of consistent early screening mammograms has been studied for many years with mixed results. Current research published by the University of California in March 2022, showed half of all women who got annual mammograms will experience at least one false-positive test after 10 years.1
False-positive testing from mammography as a screening tool can lead to overdiagnosis and overtreatment, including unnecessary biopsies.2 A past study3 from the John Wayne Cancer Institute revealed needle biopsy can increase the spread of cancer compared to patients who received excisional biopsy, also known as lumpectomies.
After a false-positive mammography, needle biopsies are widely used to diagnose breast cancer. But this can accidentally cause malignant cells to spread from the tumor site and encourage metastasis to form in other areas of your body. The researchers from John Wayne Cancer Institute concluded:4
"Manipulation of an intact tumor by FNA or large-gauge needle core biopsy is associated with an increase in the incidence of SN metastases, perhaps due in part to the mechanical disruption of the tumor by the needle."
There's also a significant financial cost to annual mammogram screenings. According to the American Cancer Society,5 73% of women over 45 had a screening mammogram within the past 2 years. In the U.S., these percentages add up to an overwhelming number of women. As of July 1, 2020, there were 62.03 million women from 40 to 70 years in the U.S.6
Assuming the average out-of-pocket cost for a mammogram in the U.S. is roughly $100,7 the total revenue generated is in the billions of dollars. But the financial cost is not the only downside to annual mammogram testing, and women do have other choices for effective screening.
False-Positive Mammograms Are Not Uncommon
The featured study8 was published in JAMA Oncology in March 2022. The researchers asked the question if there was a difference between screening for breast cancer using traditional digital mammography or 3D mammography, also called digital breast tomosynthesis.
Data were collected between January 1, 2005, and December 31, 2018, at 126 facilities. It included 903,495 women aged 40 to 79 years. The results showed there were 2,969,055 nonbaseline screening mammograms interpreted by 699 radiologists; 58% of those mammograms were performed in women younger than 60 years.
Importantly, it was also noted that 46% of these mammograms were on women who had dense breast tissue. Michael Bissell, epidemiologist in the UC Davis Department of Public Health Sciences and researcher in the study, said in a press release:9
"The screening technology did not have the largest impact on reducing false positives. Findings from our study highlight the importance of patient-provider discussions around personalized health. It is important to consider a patient's preferences and risk factors when deciding on screening interval and modality."
After data collection, the researchers analyzed the type of mammography used, screening interval, age of the woman and breast density. From this data, they estimated that a woman would have a cumulative risk of at least one false positive after receiving mammograms each year or every other year for 10 years.10
The analysis also showed a false positive resulted in repeated imaging within six months or a biopsy recommendation. The scientists then separated the data for 2D and 3D digital mammography, theorizing that 3D may have a lower risk of a false positive test.
While the theory was proved by the data, the reduction in risk was minimal. They estimated that over 10 years of 3D screening, 50% of women had at least one false-positive test while 56% of those receiving traditional digital mammography had at least one false positive. The comparison between those who had short interval follow-up recommendations and biopsy recommendations differed by only 1%.
Mammograms May Not Work for Women With Dense Breasts
The researchers also found that regardless of whether women had 2D or 3D mammography, the false-positive results were higher in women who had extremely dense breasts.11
The difference between false positives in women who had entirely fatty breasts and those with dense breasts was significant. Using 3D mammography, women with entirely fatty breasts had a 31% probability of a false positive test, while those with dense breasts had a 67.3% probability of a false positive test.12
The researchers also found that, in general, between both types of mammography, women who had almost entirely fatty breasts had a lower probability of a false positive test as compared to women with extremely dense breasts. Additionally, women with dense breasts did not benefit from cancer detection with tomosynthesis.
In addition to the problem with overdiagnosis is the reality that mammograms do not detect all breast cancer. The documentary, “Boobs: The War on Women’s Breasts” available on DVD or Vimeo digital,13 tells the story of Nancy Cappello. Capello was diagnosed with breast cancer after receiving two normal mammograms.
Capello's cancer was missed because she had dense breast tissue. It was only found when her doctor felt the ridge in her breast and prescribed an ultrasound in addition to a mammogram. Capello became a pioneer in the movement to teach women about dense breast tissue and how using a mammogram is "like finding a polar bear in a snowstorm." She said:14
"So I went on a quest — for research — and I discovered for nearly a decade BEFORE my diagnosis, six major studies with over 42,000 women concluded that by supplementing a mammogram with an ultrasound increases detection from 48% to 97% for women with dense tissue.
I also learned that women with extremely dense tissue are 5x more likely to have breast cancer when compared with women with fatty breasts and that research on dense breast tissue as an independent risk factor for breast cancer has been studied since the mid 70s.
… I endured a mastectomy, reconstruction, 8 chemotherapy treatments and 24 radiation treatments. The pathology report confirmed — stage 3c cancer because the cancer had traveled outside of the breast to my lymph nodes. Eighteen lymph nodes were removed and thirteen contained cancer — AND REMEMBER — a "normal" mammogram just weeks before. Is that early detection?"
Cappello succumbed to her breast cancer in 2018 and died after a 15-year fight to beat her cancer,15 but as a result of her efforts, 38 states have passed mandatory breast density reporting laws. The film states that up to 90% of women may have some degree of dense breast tissue that may affect a mammogram's outcome and could benefit from whole breast ultrasound — a procedure that's generally used as an adjunct to a mammogram, rather than a primary test.16
Mammography Radiation Is Not Without Risk
There's also the issue that mammograms use ionizing radiation in a relatively high dose. This, in and of itself, can contribute to the development of breast cancer. A 2016 study concluded:17 "… ionizing radiation as used in low-dose X-ray mammography may be associated with a risk of radiation-induced carcinogenesis."
The researchers pointed out that women who carry a genetic variation or have an inherited disposition of breast cancer should avoid radiation as much as possible. Unfortunately, conventional medicine often recommends routine or even extra mammography for those who have an inherited disposition for breast cancer18 or a genetic mutation.19
The next generation of mammography, 3D tomosynthesis, is basically a CT scan for the breast. Radiation exposure from this is even greater than standard mammograms by a significant margin. According to one study,20 annual screening using digital or film mammography on women aged 40 to 80 years is associated with an induced cancer incidence and fatal breast cancer rate of 20 to 25 cases per 100,000 mammograms.
This means an annual mammogram could cause 20 to 25 cases of fatal cancer for every 100,000 women who got the test. A 3D mammography requires multiple views to get the three-dimensionality. It stands to reason your total radiation exposure is considerably higher than from a standard 2D mammogram.
Additionally, data do not support screening asymptomatic women as it is not saving extra lives. A response published in The BMJ21 to research published in The Lancet22 was written by Hazel Thornton, an honorary visiting fellow in the department of health sciences at the University of Leicester. She included reports on her testimony before the House of Commons Health Committee on breast cancer services.
She was asked why she thought the NHS Breast Screening Programme was “a costly trawl of an asymptomatic public group … creating huge costly psychological and physical morbidity,” to which part of her answer was that it:23
“… focuses on the women who benefit, in other words, the one life that is saved, and it overlooks the hundreds of women that go through the process and in some cases suffer psychological harm for that one. It is unbalanced and disproportionate and should be reviewed, in my opinion, at the moment.”
In a Cochrane review of the literature24 they discovered — as Thornton testified — for every 2,000 women screened over 10 years, one avoids dying of breast cancer, and 10 will be treated unnecessarily. Additionally, over 200 women will undergo psychological distress and uncertainty for years after receiving false-positive findings.
One cohort study25 engaged participants in Denmark from 1980 to 2010. They also found screening did not lower the incidence of advanced tumors and concluded “that 1 in every 3 invasive tumors and cases of DCIS diagnosed in women offered screening represent overdiagnosis (incidence increase of 48.3%).”26
You Have Choices
Although mammography is the most frequently recommended breast cancer screening tool, you have choices for diagnostic testing that do not involve radiation. Women should be provided enough information to make an informed decision and allowed to use their choice. When you know the options, you can ask to have the test that best suits your situation.
Other potentially safer options for breast examination include clinical breast exams, thermography and ultrasound. Thermography and ultrasound don't use radiation and can detect abnormalities that mammograms can miss, especially in women with dense breasts.
While it’s also claimed that mammography can catch cancers that an ultrasound misses; according to the National Institutes of Health, “… researchers do not know with full certainty whether 3D mammography is better or worse than standard mammography at avoiding false-positive results and identifying early cancers in all types of patients.”27
Not only that, the U.S. Preventive Services Task Force (USPSTF) on breast cancer screening admits that “… the current evidence is insufficient to assess the benefits and harms of digital breast tomosynthesis (DBT) as a primary screening method for breast cancer.”28
Although they are effective, alternative tests can be difficult to access in the U.S. due to federal guidelines and the influence of the billion-dollar mammography industry. To deny women the use of these screening programs, the USPSTF claims:
“… current evidence is insufficient to assess the balance of benefits and harms of adjunctive screening for breast cancer using breast ultrasonography, magnetic resonance imaging, DBT, or other methods in women identified to have dense breasts on an otherwise negative screening mammogram.”
It's also important to recognize that screening does not prevent breast cancer. Instead, prevention requires healthy lifestyle choices, paying attention to nutritional factors and avoiding toxins.
For example, vitamin D is of vital nutritional factor that can reduce your risk of all cancer,29 including breast cancer.30 Animal and human studies have also demonstrated that omega-3 fatty acids can help prevent breast cancer and have a positive effect during breast cancer treatment.31
To understand your potential risk, it's crucial that you know your vitamin D level and omega-3 index. Conventional medicine has led many women to believe that simply getting an annual test will protect them from breast cancer. Leading a healthy lifestyle and being informed of your screening options can help you avoid this potentially deadly pitfall.
- 1 JAMA Network, 2022; 5(3)
- 2 Current Oncology, 2015;22(5)
- 3, 4 JAMA Surgery, 2004;139(6)
- 5 American Cancer Society, Breast Cancer Facts and Figures 2019-2020 Table 5
- 6 Statistica, Resident Population of the United States by Sex and Age, July 1, 2020
- 7 Cost Helper Health, How Much Does a Mammogram Cost?
- 8 JAMA Oncology, 2022;5(3) Question and Findings
- 9, 11 Science Daily, March 25, 2022
- 10 Science Daily, March 25, 2022 subhead 2 para 2 and all subhead 3
- 12 JAMA Oncology, 2022;5(3) Results, False positive recall
- 13 Vimeo, August 29, 2020
- 14 AreYouDense.org, Nancy’s Story
- 15 New York Times November 28, 2018
- 16 Johns Hopkins Medicine
- 17 Medical Principles and Practice 2016;25(2)
- 18 Journal of the American College of Radiation, 2018; 15(supp 3)
- 19 BreastCancer.org, April 15, 2020, Guideline Recommendations
- 20 Radiology, 2010; doi.org/10.1148/radiol.10100570
- 21, 23 The BMJ, 2020;370:m3191
- 22 The Lancet Oncology, 2020; doi.org/10.1016/S1470-20245(20)30398-3
- 24 Cochrane Library, 2013; doi.org/10.1002/14651858.CD001877.pub5
- 25, 26 Annals of Internal Medicine, 2017; doi.org/10.7326/M16-0270
- 27 NIH. Mammography
- 28 U.S. Preventive Services Task Force. Breast Cancer: Screeening. January 11, 2016
- 29 National Cancer Institute, Vitamin D and Cancer Prevention
- 30 The Oncologist, 2012;17(1)
- 31 Breast Cancer Research, 2015;17(1) starting 40% down the page with subhead How might EPA and DHA act to prevent breast cancer?
Read the full article
0 notes
Text

After reading this, you’ll know more than an estimated 97 percent of doctors about a critical concept called lead-time bias.
While running for president of the United States, former New York mayor Rudy Giuliani ran a campaign ad contrasting his 82 percent chance of surviving prostate cancer in the United States with the 44 percent chance of surviving it in England “under socialized medicine” where routine PSA testing for prostate cancer is not done. “To Giuliani, this meant that he was lucky to be living in New York and not in York because his chances of surviving prostate cancer seemed to be twice as high in New York. Yet despite this impressive difference in the five-year survival rate, the mortality rate”—the rate at which men were dying of prostate cancer—“was about the same in the US and the UK.” How could that be? PSA testing increased survival from 44 to 82 percent, so how is that “no evidence that screening saves lives? For two reasons: The first is lead-time bias…The second is overdiagnosis.”
As I illustrate at 1:05 in my video Breast Cancer and the Five Year Survival Rate Myth, overdiagnosis is when cancer that otherwise would have never caused a problem is detected. Consider this: Let’s say that, without screening, only 400 people out of a thousand with progressive cancer are alive five years later. That means that without screening, the five-year survival rate is only 40 percent. But, let’s say that with screening, an additional two thousand cancers are overdiagnosed, meaning cancers that would have never caused a problem or may have disappeared on their own are picked up. So, because those cancers are harmless, those overdiagnosed patients are all still alive five years later, assuming their unnecessary cancer treatment didn’t kill them. In this way, the five-year survival rate has just doubled, even though in either case, the same number of people died from cancer. If that’s confusing, watch the video. That’s one way the changes in survival rates with screening may not correlate with changes in actual cancer death rates.
The other way is lead-time bias. Imagine a group of patients who were diagnosed with cancer because of symptoms at age 67 and all died at age 70. Each patient survived only three years. So, the five-year survival rate for the group is 0 percent. Now, imagine that the same group underwent screening. By definition, screening tests lead to earlier diagnosis. Suppose that with screening, the cancers were diagnosed in all patients at age 60 instead of 67, but, nevertheless, they all still died at age 70. In this screening scenario, each patient survived ten years, which makes the five-year survival rate for this group 100 percent. Survival just went from 0 to 100 percent! You can imagine the headlines: “ Cancer patients live three times longer with a new screening test, ten years instead of three.” All that really happened in this screening scenario, though, is that the people were treated as cancer patients for an additional seven years. If anything, that would likely just diminish their quality of life.
So, that’s the second way that changes in survival rates with screening may not correlate with changes in actual cancer death rates. In fact, the correlation is zero, as you can see at 3:14 in my video. There is no correlation at all between increases in survival rates and decreases in mortality rates. That’s why “[i]f there was an Oscar for misleading statistics, using survival statistics to judge the benefit of screening would win a lifetime achievement award hands down. There is no way to disentangle lead time and overdiagnosis biases from screening survival data.” That’s why, “in the context of screening, these statistics are meaningless: there is no correlation between changes in survival and what really matters, changes in how many people die.” Yet, that’s what you see in the ads and leaflets from most of the cancer charities and what you hear from the government. Even prestigious cancer centers, like M.D. Anderson, have tried to hoodwink the public this way, as you can see at 3:57 in my video.
If you’ve never heard of lead-time bias, don’t worry, you’re not alone. Your doctor may not have heard of it either. “Fifty-four of the 65 physicians [surveyed] did not know what the lead-time bias was. Of the remaining 11 physicians who indicated they did know, only 2 explained the bias correctly.” So, just by having read to this point in this blog post, you may already know more about this than 97 percent of doctors.
To be fair, though, is it possible the doctors don’t recognize the term but understand the concept? No. “The majority of primary care physicians did not know which screening statistics provide reliable evidence on whether screening works.” In fact, they “were also 3 times more likely to say they would ‘definitely recommend’ a [cancer screening] test” based on “irrelevant evidence,” compared to a test that actually decreased cancer mortality by 20 percent.
If physicians don’t even understand key cancer statistics, how are they going to effectively counsel their patients? “Statistically illiterate physicians are doomed to rely on their statistically illiterate conclusions, on local custom, and on the (mostly) inaccurate promises of pharmaceutical sales representatives and their leaflets.”
KEY TAKEAWAYS
Overdiagnosis, the detection of cancer that otherwise would never have caused a problem, can result in unnecessary cancer treatments and affect survival rates of breast cancer patients.
For example, without screening, the five-year survival rate is 40 percent. With screening, however, overdiagnosis results in more cancer patients, despite the likelihood that their cancers are harmless or may disappear on their own. And, those overdiagnosed patients should be alive after five years, which doubles the five-year survival rate, even though the same number of patients died from cancer.
Lead-time bias is also an issue. Symptomatic patients may be diagnosed at a later age than had they been with screening, which, by definition, leads to earlier diagnosis. In this case, imagine patients were diagnosed without screening at age 67 and died three years later, so the five-year survival rate is 0 percent. Now imagine the group underwent screening and the cancers were diagnosed at age 60, so they were alive for ten years before dying at 70. In the screening scenario, the five-year survival rate for the group is 100 percent.
In fact, there is no correlation between increases in survival rates and decreases in mortality rates.
It is not possible to disentangle the biases of lead time and overdiagnosis from screening survival data.
The overwhelming majority of doctors—54 out of 65 physicians surveyed—are unfamiliar with lead-time bias, and of the 11 who indicated they did know, only 2 explained the bias accurately.
How can doctors who don’t even understand key cancer statistics effectively counsel their patients?
There is just so much confusion when it comes to mammography, combined with the corrupting commercial interests of a billion-dollar industry. As with any important health decision, everyone should be fully informed of the risks and benefits, and make up their own mind about their own bodies. This is one installment in my 14-part series on mammograms, which includes:
Nine out of Ten Women Misinformed About Mammograms
Mammogram Recommendations: Why the Conflicting Guidelines?
Flashback Friday: Should Women Get Mammograms Starting at Age 40?
Do Mammograms Save Live?
Consequences of False-Positive Mammogram Results
Do Mammograms Hurt?
Can Mammogram Radiation Cause Breast Cancer?
Understanding the Mammogram Paradox
Overtreatment of Stage 0 Breast Cancer DCIS
Women Deserve to Know the Truth About Mammograms
Why Mammograms Don’t Appear to Save Lives
Why Patients Aren’t Informed About Mammograms
The Pros and Cons of Mammograms
For more on breast cancer, see my videos Oxidized Cholesterol 27HC May Explain Three Breast Cancer Mysteries, Eggs and Breast Cancer and Flashback Friday: Can Flax Seeds Help Prevent Breast Cancer?
I was able to cover colon cancer screening in just one video. If you missed it, see Should We All Get Colonoscopies Starting at Age 50?.
Also on the topic of medical screenings, check out Flashback Friday: Worth Getting an Annual Health Check-Up and Physical Exam? Is It Worth Getting Annual Health Check-Ups? and Is It Worth Getting an Annual Physical Exam?.
In health,
Michael Greger, M.D.
0 notes
Text
What’s the future benefits of machine learning in the medical sector
Today, technology-based healthcare is a reality as smart medical devices become mainstream. The healthcare industry welcomes innovation; that is why the future of AI in healthcare is very bright. Google has already launched an algorithm that successfully identifies cancer in mammograms, while scientists at Stanford University can identify skin cancer thanks to Deep Learning. Artificial Intelligence Development in New York is responsible for processing thousands of different data points, accurately predicting risks and outcomes, as well as many other functions.
Benefits of machine learning in the medical sector
Drug discovery:
Drug discovery and development is very expensive and time-consuming work. Typically, the development of a new drug takes more than 10 years to enter the market and costs approximately $ 2.6 billion, according to the Tufts Center for the Study of Drug Development. A drug discovery initiative aims to find a compound that reacts with specific molecules in the body, causing the disease to be cured. But there is a strong possibility that the nucleus or the supporting drug compound will react adversely to undirected molecules in the body, potentially causing dangerous and threatening side effects.
Since pharmaceutical companies cannot predict a potential effect of a drug compound on targeted and nondirected molecules using traditional computational technologies, the chances of drug failure are higher in clinical trials. This scenario makes drug discovery a very expensive and time-consuming process. In this case, better predictive methods that use machine learning can save a lot of resources. The machine learning-based approach (considering the large volume of clinical data for approved and failed drugs) to identify a toxic compound that can cause side effects can save a lot of resources before starting clinical trials.
About 90% of drugs cannot go through the testing process. By automating compound molecule reaction processes using machine learning development, pharmaceuticals can improve the drug discovery, development process and reduce time to market. According to a Machine learning company, automating the drug discovery process can reduce costs by approximately 70%.
Machine learning-based behavior modification:
Behavioral modification is an important part of medicine, and since machine practice has expanded in healthcare, countless startups have grown in areas such as cancer prevention and recognition, patient treatment, and more. Somatics, a B2B2C-based data analysis company, has released an ML-based app to identify the gestures we make in our daily lives, allowing us to understand our unconscious behavior and make necessary changes.

Identification and diagnosis of diseases:
By analyzing hundreds of health care records and other patient data, machine learning algorithms can find patterns related to diseases and health conditions.
Recent developments in machine learning can help increase access to healthcare in developing countries and innovate in cancer diagnosis and treatment. Entrepreneur reports that a deep learning-based prediction model developed at the Massachusetts Institute of Technology can predict the development of breast cancer years in advance.
In addition, according to a Data science development company in USA research, applications of AI in healthcare "can now diagnose skin cancer more accurately than a certified dermatologist." The article points out the additional benefits of machine learning, including the speed and efficiency of diagnostics, and a shorter period of time to train an algorithm compared to a human.
Patient safety and results:
The quality of the data input in the Artificial Intelligence services determines the reliability of the output. Bad or faulty data can undermine the reliability of the system, which then calls into question whether decisions based on the data are right or wrong.
Another concern with faulty data is that it can lead to a lack of cultural competence. For example, since the data generally does not represent minority populations, it can put people at risk of overdiagnosis or underdiagnosis.
The bottom line is that concerns about system stability and a lack of cultural competence can lead to erroneous results when machine learning algorithms are used on incorrect data to ill-informed medical decision making, and ultimately affect patient safety and outcomes.
Improved radiotherapy:
One of the most popular applications of and machine learning in healthcare is in the field of radiology. There are many unique variables in medical image analysis that can arise at any given time. There are many lesions, cancer foci, etc. that simply cannot be modeled using complex equations. Learning from the various models of ML-based algorithms available will make it easier to identify and find variables. One of the most popular uses of machine learning in medical image analysis is to classify objects such as injuries as general or abnormal, ulcer or non-lesion. Researchers at UCLH can help Google's Deepmind Health actively develop algorithms to identify the difference between healthy and cancerous tissue and improve radiation therapy.
Conclusion:
Summarizing the importance of the applications of deep learning and machine learning in healthcare, the highest score corresponds to its powerful abilities to sort and classify health data, as well as to accelerate the clinical decisions of doctors and any type of prediction that can save lives. or make surgery less complicated (for example, preventing hypoxemia during surgery). Isn't it already a lot? Human life is without a doubt the most valuable thing. Today, machine learning in healthcare provides technologies that directly contribute to the future of advanced medical diagnostics and medicine as a whole. Other alternatives, such as AI in nutrition, will be discussed in future articles!

Witten By
Yamuna mannepalli
I am working as a Marketing Associate at USM Business Systems. I completed a B.Tech. in Computer Science from JNTUK. I spend most of my time observing social behavior for brand spanking new shopper trends. I'm curious about technology, market behavior, new media, the surroundings, property, artistic movement, eventualities and corporations.
#machine learning#machine learning development#machine learning in healthcare#machine learning services#machine learning solutions
1 note
·
View note
Text
What are Cancer Screening tests?
Screening serves as a cancer detector before the symptoms appear. The screening will help find cancer at an early stage when it might lead to treatment. However, as soon as symptoms appear, cancer may have already spread. This can make it harder to cure.
The benefits of these tests are as follows:
They reduce the chance of dying by screening for cancer.
They have more benefits than harms. For example, possible harms of screening include bleeding, inaccurate test results, physical damage, and overdiagnosis(which is the diagnosis of cancers that do not need treatment.)
Bear in mind that it doesn’t necessarily mean they have diagnosed cancer when your doctor suggests a screening test. Screenings are done when the patient has no symptoms.

What we do
We offer a vast range of cancer screening tests to diagnose your condition best, using high-tech equipment. Some examples of our professional services are as follows:
Colonoscopy, sigmoidoscopy, and stool tests
Transvaginal ultrasound
Low-dose helical computed tomography
PSA test
Skin exams
Mammography
Pap test and human papillomavirus (HPV) testing
Breast MRI
Virtual colonoscopy
Source: Snfamilymedicine
0 notes
Text
April 2021 Learning Network Resources
Trust in Healthcare
Quinn SC, et alt. Addressing Vaccine Hesitancy in BIPOC Communities — Toward Trustworthiness, Partnership, and Reciprocity. NEJM. March 2021
“A primary path toward trust and confidence is relationship building. In too many situations and circumstances, BIPOC communities are asked to ‘help us solve the problems in your community.’ Long-standing and reciprocal relationships between medical and research institutions and BIPOC communities are largely nonexistent. The relationships that do exist are generally short-lived, often enduring only as long as grant funding lasts. For health care and public health institutions to build a reputation of trustworthiness, partnerships rooted in bidirectional communication, capacity building, and reciprocity are required.”
Beach MC, et alt. Testimonial Injustice: Linguistic Bias in the Medical Records of Black Patients and Women. Journal of General Internal Medicine. March 2021
“Black patients may be subject to systematic bias in physicians’ perceptions of their credibility, a form of testimonial injustice. This is another potential mechanism for racial disparities in healthcare quality that should be further investigated and addressed.”
Pollard MS, et alt. Decline in Trust in the Centers for Disease Control and Prevention During the COVID-19 Pandemic. RAND Corporation. March 2021
“As part of a nationally representative RAND American Life Panel (ALP) survey fielded in early May 2020 that assessed how Americans are coping with COVID-19, we asked more than 2,000 individuals to report their levels of trust in a variety of federal institutions, including the CDC, the United States Postal Service (USPS), and the Federal Emergency Management Agency (FEMA). In October 2020, we resurveyed a random sample of 1,892 of the original respondents and asked them to report their levels of trust again. In this report, we compare individual-level changes in trust in the CDC, USPS, and FEMA between May and October 2020. Responses are weighted to match a range of population distributions in the Current Population Survey and voting behavior.”
Carolla B, et alt. Are Health Centers Facilitating Equitable Access to COVID-19 Vaccinations? Kaiser Family Foundation. March 2021
“These early data show that health centers appear to be reaching people of color at a higher rate than overall vaccination efforts. While vaccinations at health centers represent a relatively small share of total vaccinations administered nationally to date, further ramping up health centers’ involvement in vaccination efforts at the federal, state, and local levels will likely be a meaningful step in reaching people of color and advancing equity on a larger scale.”
Tharakan S, et alt. The impact of the globalization of cancer clinical trials on the enrollment of Black patients. American Cancer Society. March 2021
“The globalization of cancer clinical trials is associated with a widening racial enrollment disparity gap in the United States. The impact of global trials on domestic clinical trial generalizability warrants further consideration from a regulatory and policy standpoint.”
Bleich SN, et alt. Addressing Racial Discrimination in US Health Care Today. JAMA Health Forum. March 2021
“From the public statements and initial actions of the Biden administration, it is clear that addressing racial discrimination will be a high policy priority. This comes alongside a growing national awareness of the seriousness of this problem by leadership groups in health care and medicine. This article addresses 2 central issues related to racial discrimination in health care: the extent of reported discrimination in various health care settings among Black and Latinx households and recommended policies to hold health care institutions accountable for addressing racial discrimination.”
Bogart LM, et alt. What Contributes to COVID-19 Vaccine Hesitancy in Black Communities, and How Can It Be Addressed? RAND Corporation. March 2021
“Recent polls show that Black Americans are less willing than Americans of other races or ethnicities to be vaccinated for COVID-19. These lower vaccination rates among Black Americans would further widen COVID-19 inequities in diagnosis, hospitalization, and mortality. A main driver of hesitancy among Black Americans is thought to be general mistrust of health care systems and providers. Such mistrust has arisen in Black communities as an understandable, rational, and self-protective reaction to history, knowledge, and continuous and repeated discrimination, racism, and harmful experiences toward Black Americans by the health care system, health care providers, and the U.S. government.”
Blogs, Issue Briefs, Opinion Pieces and More…
Hyun D, et alt. Many hospitalized Covid-19 patients are given antibiotics. That’s a problem. STAT. March 2021.
“As the Covid-19 pandemic continues into its second year, public health experts are increasingly concerned that the response to this global crisis may be accelerating another one: the development and persistence of the antibiotic-resistant bacteria known as superbugs. Why? All antibiotic use hastens the emergence of resistance. And although antibiotics aren’t used to treat Covid-19, which is a viral illness, they’re often prescribed to Covid-19 patients who are at risk for bacterial infection.”
Khullar D, et alt. Imagining a World Without Low-Value Services: Progress, Barriers, and the Path Forward. AJMC. March 2021
“Low-value services are a major problem in the US health care system. We believe that the coronavirus disease 2019 pandemic’s unprecedented impact on the health system, and society writ large, offers an opportunity to reshape the conversation and incentives around low-value services. This article explores current barriers to and opportunities for accelerating progress toward high-value care delivery.”
Brownlee SM, et alt. Better understanding the downsides of low value healthcare could reduce harm. BMJ. March 2021
“Today, efforts to quantify and tackle gaps in patient safety have expanded far beyond anaesthesia. A distinct discipline with its own emerging scientific framework, patient safety has been declared ‘one of the most important components of healthcare delivery’ by the World Health Organization. Yet there is one area of healthcare that remains sorely in need of similar data on harm and an equally sustained worldwide effort to reduce it. That area is overuse of low value healthcare services.”
For Cancer Screening, COVID-19 Pandemic Creates Obstacles, Opportunities. National Cancer Institute. March 2021
“The pandemic may lead to other potential innovations in cancer screening. Some physicians are already using video conferencing tools to educate people about screening tests, while others are discussing ways to focus screening resources on those most at risk of developing cancer.”
Journals
Maust DT, et alt. Prevalence of Central Nervous System-Active Polypharmacy Among Older Adults With Dementia in the US. JAMA. March 2021
“In this cross-sectional analysis of Medicare claims data, 13.9% of older adults with dementia in 2018 filled prescriptions consistent with CNS-active polypharmacy. The lack of information on prescribing indications limits judgments about clinical appropriateness of medication combinations for individual patients.”
Park S, et alt. Trends in Use of Low-Value Care in Traditional Fee-for-Service Medicare and Medicare Advantage. JAMA. March 2021
“This cross-sectional study found that use of low-value care was similarly prevalent in MA and TM, suggesting that MA enrollment was not associated with decreased provision of low-value care compared with TM.”
Soong C, et alt. Advise non-pharmacological therapy as first line treatment for chronic insomnia. BMJ. March 2021
“Guidelines recommend non-pharmacological approaches, including cognitive behavioural therapy, as first line treatment for chronic insomnia in adults (box 1).12345 Yet, sedatives are commonly prescribed to treat insomnia.”
Habib AR, et alt. Recommendations From Breast Cancer Centers for Frequent Screening Mammography in Younger Women May Do More Harm Than Good. JAMA Internal Medicine. March 2021
“The most recent (2016) US Preventive Services Task Force (USPSTF) breast cancer screening recommendations for women with average risk advise biennial screening in women aged 50 to 74 years. Among younger women (aged 40-49 years), the estimates of reduced breast cancer mortality are smaller and have more uncertainty, and the rates of potential harm are higher. Thus, the USPSTF does not recommend routine screening but suggests individualization based on shared decision-making.”
Jonas DE, et alt. Screening for Lung Cancer With Low-Dose Computed Tomography Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. March 2021
“Screening high-risk persons with LDCT can reduce lung cancer mortality but also causes false-positive results leading to unnecessary tests and invasive procedures, overdiagnosis, incidental findings, increases in distress, and, rarely, radiation-induced cancers. Most studies reviewed did not use current nodule evaluation protocols, which might reduce false-positive results and invasive procedures for false-positive results.”
Maust DT, et alt. Prevalence of Central Nervous System–Active Polypharmacy Among Older Adults With Dementia in the US. JAMA. March 2021
“In this cross-sectional analysis of Medicare claims data, 13.9% of older adults with dementia in 2018 filled prescriptions consistent with CNS-active polypharmacy. The lack of information on prescribing indications limits judgments about clinical appropriateness of medication combinations for individual patients.”
Krist AH. Screening for Lung Cancer US Preventive Services Task Force Recommendation Statement. JAMA. March 2021
“To update its 2013 recommendation, the US Preventive Services Task Force (USPSTF) commissioned a systematic review on the accuracy of screening for lung cancer with low-dose computed tomography (LDCT) and on the benefits and harms of screening for lung cancer and commissioned a collaborative modeling study to provide information about the optimum age at which to begin and end screening, the optimal screening interval, and the relative benefits and harms of different screening strategies compared with modified versions of multivariate risk prediction models.”
Bai F, et alt. Stroke Risk Factor Status and Use of Stroke Prevention Medications Among Hispanic/Latino Adults in HCHS/SOL. Stroke. March 2021
“Hispanic/Latino adults in the United States have high prevalence and awareness of VRFs but low adherence to secondary stroke prevention strategies. Older adults, women, and uninsured people are vulnerable groups that may benefit from targeted interventions.”
Media
Moloney S. NYC Health + Hospitals Adopt COVID-19 Care Recommendations of Board of Internal Medicine. Norwood News. March 2021
“NYC Health + Hospitals announced on March 16, that it has adopted the American Board of Internal Medicine (ABIM) Foundation guidelines, system-wide, to further reduce the potential spread of COVID-19, and keep staff and patients safe during the pandemic. The COVID-19 ‘Choosing Wisely’ guidelines advise healthcare providers on eliminating unnecessary testing and treatment in an effort to reduce exposure to COVID-19. The guidelines also incorporate specific, evidence-based recommendations clinicians should consider to utilize limited resources wisely, such as blood transfusions.”
Harris R. Antibiotic Use Ran High In Early Days Of COVID-19, Despite Viral Cause. NPR. March 2021
“Doctors treating COVID-19 patients early in the pandemic often reached for antibiotics. But those drugs were not helpful in most cases, and overuse of antibiotics is a serious concern.”
Davenport L. Swallowable Capsule-Camera Instead of Endoscopy for Use at Home. Medscape. March 2021
“A miniature camera the size of a capsule that is swallowed and that then transmits images of the inside of the gut can reveal cancer and gastrointestinal diseases. The device, which will be studied in a trial conducted by the National Health Service (NHS) in England, is used by patients at home instead of having to visit a clinic for an endoscopy.”
Marchione M, et alt. Researchers study impact of pandemic cancer screening pause. Associated Press. March 2021
“Millions of colonoscopies, mammograms, lung scans, Pap tests and other cancer screenings were suspended for several months last spring in the United States and elsewhere as COVID-19 swamped medical care. Now researchers are studying the impact, looking to see how many cancers were missed and whether tumors found since then are more advanced.”
The post April 2021 Learning Network Resources first appeared on Choosing Wisely.





https://feeds.feedblitz.com/~/649515080/0/catherinemccracken~April-Learning-Network-Resources/
0 notes
Text
Big Pharma EXPOSED: Study of 3 top medical journals reveals that many medications, medical products and services are completely INEFFECTIVE
If you’ve ever suspected that a medication you’re taking isn’t really doing much to improve your symptoms, it might not just be your imagination: A comprehensive study has shown that a concerning number of medications, medical products and services are simply not effective.
A study that was recently published by eLife showed just how poor Big Pharma’s record is when it comes to producing effective medications. They carried out an analysis of more than 3,000 randomized controlled trials from 2003 to 2017 that were published in three top medical journals: the New England Journal of Medicine, the Lancet, and the Journal of the American Medical Association.
The researchers were looking at the effectiveness of the current “best practices” across different medical disciplines, populations and interventions. They found 396 medical reversals – in other words, practices and treatments that turned out not to be effective and were essentially de-adopted. Medications were the most common intervention, followed by procedures, vitamins/supplements, devices, and system intervention across varied fields such as ophthalmology, rheumatology, allergies, urology, infectious diseases, pediatrics, cardiovascular medicine and anesthesiology.
For example, one study looked at the antidepressants mirtazapine and sertraline, which are recommended as first-line treatments for clinical depression regardless of age. The studies showed that the two drugs did not make any significant difference in depressive symptoms in older adults with Alzheimer’s disease.
In addition to medication, the study identified useless interventions like wearable step tracking technology for promoting weight loss. They also discussed dangerous medical recommendations like annual or bi-annual mammograms for women at a low risk of breast cancer under the age of 50. These recommendations prey on women’s very understandable fear of breast cancer when the truth is that the radiation from excessive mammograms is actually a breast cancer risk itself.
They quoted a Cochrane review that said: “The chance that a woman will benefit from attending screening is small at best, and — if based on the randomized trials — ten times smaller than the risk that she may experience serious harm in terms of overdiagnosis.”
Profits over people
Incredibly, even though hundreds of medications and medical products have been shown not to work, many are still being used and paid for with taxpayer dollars through Medicaid and Medicare. The researchers wrote that after a practice has been found to be ineffective, it is hard to convince doctors to stop using it.
The truth is that so many of these interventions are highly profitable for those in the medical industry, and it doesn’t matter much to them if it isn’t helping people. In fact, sick people who depend on medications are actually more profitable to the medical industry. Big Pharma’s profits have been projected to reach $1.5 trillion in 2023, so there is a lot of money at stake.
Since you can’t depend on doctors and drug companies to always act in your best interest, it is important to do all you can to prevent health problems. A healthy diet is one of the best ways to stack the odds in your favor. Eliminating sugar and processed foods and focusing on organic fruits and vegetables can go a long way toward enhancing your health, as can getting regular exercise – at least 30 minutes of moderate movement a few times a week is enough.
You should also try to keep your exposure to toxins as low as possible. This means choosing organic food, fighting indoor air pollution with an air purifier, ensuring your drinking water is free of fluoride and other toxins, and avoiding chemical-laden personal hygiene and cleaning products.
You are the person who is ultimately responsible for your health, so make sure any medications or other medical interventions your doctor suggests are truly safe and necessary. Ask questions, do your research, and seek a second or even third opinion if you have any doubts.
Isabelle Z.
Sources for this article include:
NaturalHealth365.com
ELifeSciences.org
Related Posts
Use N-acetylcysteine? The FDA is trying to make it illegal because it could help treat COVID-19
Doctor who cured 350 coronavirus patients with 100% success rate speaks out passionately in Washington D.C.
You are what you eat: 3 foods that look eerily similar to the organs they heal
CBD oil: A miracle oil that relieves anxiety without causing a high
from WordPress https://ift.tt/2CTGQJN
via IFTTT
0 notes