#Oligohydramnios
Text

Explore the meaning of high-risk pregnancy. Understand the factors and care needed for a healthy pregnancy journey. Learn about High Risk Pregnancy.
Do Read: https://www.drshubhragoyal.com/welcome/blogs/introduction-to-high-risk-pregnancy--what-does-it-mean
#High Risk Pregnancy#Pregnancy with heart disease#Rh incompatibility#Oligohydramnios#Uterine fibroids pregnancy#Pregestational diabetes#Cervical insufficiency#Pregnancy after 35#Recurrent miscarriages#Intrauterine growth retardation#Placental abruption#VBAC risks (Vaginal Birth After Cesarean)#Perinatal infections#Pregnancy-induced hypertension#Chronic kidney disease pregnancy#Antiphospholipid syndrome pregnancy#Congenital anomalies risk
1 note
·
View note
Text
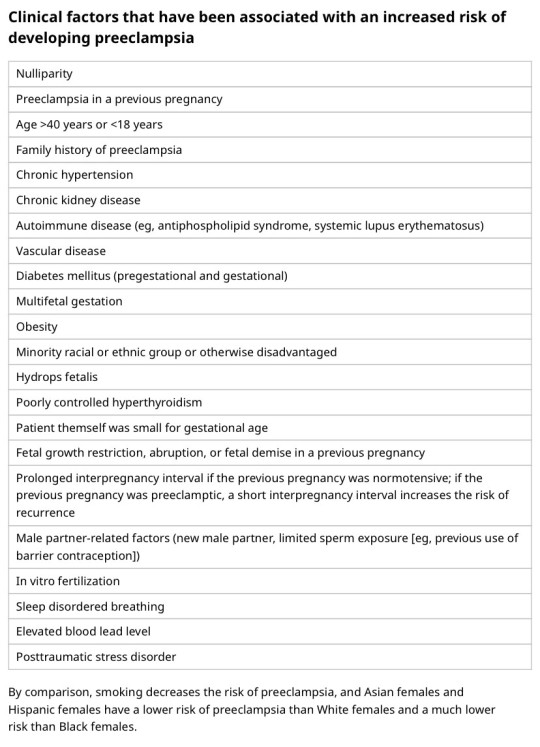
I'm on OB rotation again. I asked the attending what are things the PCP should know about prenatal and postpartum pts. Stuff we discussed:
SSRIs can be continued during pregnancy. I often see patients on Zoloft during pregnancy if they need an antidepressant. In fact, I just started a prenatal patient on Zoloft the other day in clinic. It is safe to continue SSRIs during pregnancy because you should treat the patient's depression. Babies can come out sort of jittery because of the SSRI, but that goes away.
Postpartum patients will have bleeding somewhat similar to a menstrual period right after giving birth. It starts to decrease and becomes like a brownish color and can last up to 6 weeks postpartum. Any bleeding beyond that point is abnormal.
There is some evidence that if you have estrogen-containing birth control, it can decrease milk supply. Actually, I had a patient in clinic recently who was seen by an attending and he started her on a progesterone only birth control so that it would not affect her milk supply. Estrogen decreases the patient's milk supply, so patients who plan to breast-feed should not be started on estrogen-containing birth control. Right after giving birth, your body has increased amounts of estrogen, so you would not start estrogen containing birth control until at least 6 weeks postpartum anyway. Increasing estrogen immediately postpartum increases risk of blood clots. For patients who plan to breastfeed and want to be on an oral contraceptive, use progesterone only oral contraceptives until she stops breastfeeding.
If the mother is breastfeeding at least every 4 hours, then this can be used for contraception. It's about 80% effective. Once baby starts sleeping through the night or once baby starts feeding more than every 4 hours, this method won't work! If you go more than 4 hours without breastfeeding, breastfeeding will not protect you from pregnancy! You can also ovulate before your menstrual period returns, so you can't say you can't get pregnant because your period has not returned yet!
I asked the attending I worked with today about how she goes about prescribing birth control. She said she will usually start with Sprintec. It's usually covered by insurance and if it's not covered, it's pretty affordable. She also said Junel is pretty well tolerated. Certain progestins in certain brands of birth control may work better for certain things like acne control, but she didn't have as much knowledge on that. I'll ask another attending again about that. I usually start people on Sprintec as well.
PCP should know that alkaline phosphatase is high in pregnant patients. It comes from the placenta. So don't be freaked out by that.
You should know HTN in pregnancy and preeclampsia workup. High BP is 140/90. Severely high BP is 160/110. Swelling occurs in many pregnant pts, but that should also alert you to start preeclampsia workup.
[Preeclampsia w/u from UpToDate:
Diagnostic evaluation
•Laboratory – Patients with suspected preeclampsia should have a complete blood count with platelets, creatinine level, liver chemistries, and determination of urinary protein excretion.
•Fetal status – Fetal status is assessed concurrently or postdiagnosis, depending on the degree of concern during maternal evaluation. At a minimum, a nonstress test or biophysical profile is performed if appropriate for gestational age. Ultrasound is used to evaluate amniotic fluid volume and estimate fetal weight, given the increased risk for oligohydramnios and growth restriction.
•Consultation with the neurology service is generally indicated in patients with neurologic deficits/abnormal neurologic examination, which may include ocular symptoms or a severe persistent headache that does not respond to initial routine management of preeclampsia.]
An important thing to review is physiology of pregnancy. Blood volume increases during pregnancy, so there are lots of new RBCs and that will throw off a HgbA1c reading, therefore HgbA1c is not measured during pregnancy and will not be accurate! My attending today told me there was a midwife who offered pts either HgbA1c or oral glucose tolerance tests to screen for gestational DM. The HgbA1c is not accurate in pregnancy, so this should not be done. That would be bad to miss a diagnosis of gestational diabetes. You have to wait until 3 months postpartum to measure HgbA1c to get an accurate reading. Had a pt who did not have a PCP prior to getting pregnant, was on insulin during the pregnancy, and after giving birth, still needs to establish with PCP for diabetes f/u. After you give birth, you insulin needs drastically change, so you don't need as much as you did when you were pregnant. So I stopped her insulin and advised that she f/u with her new PCP for diabetes care.
I still need to review fetal heart tracings. The attending today said the first thing to look at is the baseline (the baseline HR should be about 160 beats/min), then the variability, then look for accelerations and decelerations. If more than 32 weeks GA, accelerations are 15 beats/min above the baseline lasting at least 15 seconds. Early decelerations are representative of compression of the fetal head, which is normal during labor as baby moves down the pelvis/birth canal. Variable decelerations look sharper like a "V" and can represent compression of the umbilical cord. Late decelerations represent placental insufficiency.
ACOG has very helpful practice bulletins.
I can't take screen shots on my work laptop, so I'm just going to summarize gestational HTN w/u from UpToDate:
Gestational HTN: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions 4 hours apart after 20 weeks of gestation in a previously normotensive individual
And:
No proteinuria
No signs/symptoms of preeclampsia-related end-organ dysfunction (eg, thrombocytopenia, renal insufficiency, elevated liver transaminases, pulmonary edema, cerebral or visual symptoms)
Preeclampsia: New onset of systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg on at least 2 occasions at least 4 hours apart after 20 weeks of gestation in a previously normotensive individual. Patients with systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg should have blood pressure confirmed within a short interval (minutes) to facilitate timely administration of antihypertensive therapy.
And:
Proteinuria (≥300 mg per 24-hour urine collection [or this amount extrapolated from a timed collection], or protein:creatinine ratio ≥0.3, or urine dipstick reading ≥2+ [if other quantitative methods are not available]).
In a patient with new-onset hypertension without proteinuria, the diagnosis of preeclampsia can still be made if any features of severe disease are present.
Preeclampsia with severe features: In a patient with preeclampsia, presence of any of the following findings are features of severe disease:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg on 2 occasions at least 4 hours apart (unless antihypertensive therapy is initiated before this time)
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
Progressive renal insufficiency (serum creatinine concentration >1.1 mg/dL [97 micromol/L] or doubling of the serum creatinine concentration in the absence of other renal disease)
Pulmonary edema
Persistent cerebral or visual disturbances
Eclampsia: A generalized seizure in a pt with preeclampsia that cannot be attributed to other causes.
HELLP syndrome: hemolysis, elevated liver enzymes, low platelets. Hypertension may be present (HELLP in such cases is often considered a variant of preeclampsia).
Chronic (pre-existing) hypertension: hypertension diagnosed or present before pregnancy or on at least 2 occasions before 20 weeks of gestation. Hypertension that is first diagnosed during pregnancy and persists for at least 12 weeks postpartum is also consider chronic hypertension.
Blood pressure criteria during pregnancy are:
Systolic ≥140 mmHg and/or diastolic ≥90 mmHg
Prepregnancy and 12 weeks postpartum blood pressure criteria are:
Stage 1 – Systolic 130 to 139 mmHg or diastolic 80 to 89 mmHg
Stage 2 – Systolic ≥140 mmHg or diastolic ≥90 mmHg
Chronic HTN with superimposed preeclampsia*:
Any of these findings in a patient with chronic hypertension:
A sudden increase in blood pressure that was previously well-controlled or an escalation of antihypertensive therapy to control blood pressure
New onset of proteinuria or a sudden increase in proteinuria in a patient with known proteinuria before or early in pregnancy
Significant new end-organ dysfunction consistent with preeclampsia after 20 weeks of gestation or postpartum
*Precise diagnosis is often challenging. High clinical suspicion is warranted given the increase in maternal and fetal-neonatal risks associated with superimposed preeclampsia.
Chronic hypertension with superimposed preeclampsia with severe features:
Any of these findings in a patient with chronic hypertension and superimposed preeclampsia:
Systolic blood pressure ≥160 mmHg and/or diastolic blood pressure ≥110 mmHg despite escalation of antihypertensive therapy
Thrombocytopenia (platelet count <100,000/microL)
Impaired liver function as indicated by liver transaminase levels at least twice the normal concentration or severe persistent right upper quadrant or epigastric pain unresponsive to medication and not accounted for by alternative diagnoses, or both
New-onset or worsening renal insufficiency
Pulmonary edema
Persistent cerebral or visual disturbances
A reduction in blood pressure early in pregnancy is a normal physiologic occurrence. For this reason, women with chronic hypertension may be normotensive at their first few prenatal visits. Later in pregnancy, when their blood pressure returns to its prepregnancy baseline, they may appear to be developing preeclampsia or gestational hypertension if there are no documented prepregnancy blood pressure measurements.
BP: blood pressure.
* Blood pressure should be elevated on at least two occasions at least four hours apart. However, if systolic pressure is ≥160 mmHg or diastolic pressure is ≥110 mmHg, confirmation after a short interval, even within a few minutes, is acceptable to facilitate timely initiation of antihypertensive therapy.
¶ The onset of preeclampsia and gestational hypertension is almost always after 20 weeks of gestation. Preeclampsia before 20 weeks of gestation may be associated with a complete or partial molar pregnancy or fetal hydrops. Postpartum preeclampsia usually presents within two days of delivery. The term "delayed postpartum preeclampsia" is used for signs and symptoms of the disease leading to readmission more than two days but less than six weeks after delivery.
Δ Significant proteinuria is defined as ≥0.3 g in a 24-hour urine specimen or protein/creatinine ratio ≥0.3 (mg/mg) (34 mg/mmol) in a random urine specimen or dipstick ≥1+ if a quantitative measurement is unavailable.
◊ Almost all women with the new onset of hypertension and proteinuria at this gestational age or postpartum have preeclampsia, but a rare patient may have occult renal disease exacerbated by the physiologic changes of pregnancy. An active urine sediment (red and white cells and/or cellular casts) is consistent with a proliferative glomerular disorder but not a feature of preeclampsia. Women with chronic hypertension who had proteinuria prior to or in early pregnancy may develop superimposed preeclampsia. This can be difficult to diagnose definitively, but should be suspected when blood pressure increases significantly (especially acutely) in the last half of pregnancy/postpartum or signs/symptoms associated with the severe end of the disease spectrum develop.
§ Photopsia (flashes of light), scotomata (dark areas or gaps in the visual field), blurred vision, or temporary blindness (rare); severe headache (ie, incapacitating, "the worst headache I've ever had") or headache that persists and progresses despite analgesic therapy; altered mental status. Seizure occurrence upgrades the diagnosis to eclampsia.¥ The differential diagnosis of preeclampsia with severe features includes but is not limited to:
Antiphospholipid syndrome
Acute fatty liver of pregnancy
Thrombotic thrombocytopenic purpura (TTP)
Hemolytic uremic syndrome (HUS)
The laboratory findings in these disorders overlap with those in preeclampsia with severe features. (Refer to table in the UpToDate topic on the clinical manifestations and diagnosis of preeclampsia.) The prepregnancy history, magnitude and spectrum of laboratory abnormalities, and additional presence of signs and symptoms not typically associated with preeclampsia help in making the correct diagnosis, which is not always possible during pregnancy.
In addition, a variety of medical disorders may be associated with hypertension and one or more of the signs and symptoms that occur in women with preeclampsia with severe features. These patients can usually be distinguished from patients with preeclampsia by taking a detailed history, performing a thorough physical examination, and obtaining relevant laboratory studies.‡ In contrast to preeclampsia, gestational hypertension is not associated with end-organ involvement, so neither proteinuria nor the symptoms or laboratory findings of preeclampsia are present.
#OB#OBGYN#birth control#gestational HTN#preeclampsia#eclampsia#breastfeeding#gestational diabetes#fetal heart tracing#FHT
2 notes
·
View notes
Text
i think about the 42 babies born in no man's land so much. like, i totally buy that babies were being born in the restricted zone but when i think of those babies, i think of the following at minimum (that the writers definitely did not)
of those 42, 12 need formula !!! if the formula crisis of last summer taught us anything, it's that this is probably not good, to need formula in no man's land
and needing formula is kind of broad. what kind of formula did these babies need? god forbid they need a hypoallergenic formula due to an allergy
all of the babies shown in detective comics #741 are, like, sitting without support or crawling and man. sitting independently is a 6 month milestone. crawling is, like, 8-9 months.
so most of the women had to have been pregnant before no man's land. assuming ovulation on 1/1, the first day of no man's land, the babies would be due on 9/23 at the earliest. so they'd be at most, like, 3 months old. obviously leslie was joking about nights in no man's land getting cold, but also does chuck dixon not know anything about how long women are pregnant for? (answer: yes).
potential for premature babies without a nicu =/
did the joker kidnap 42 <3 month old babies? was he feeding the newborns every two hours? did joker's experience with newborns in no man's land prepare him for the fourth trimester after he had his clayface baby.
anyways, what happens to pregnant peeps who go overdue and there's no pitocin to induce labor? that generally doesn't lead to good outcomes due to the deterioration of the placenta past 40 weeks
also, some of these women had to have developed gestational diabetes. with no way of knowing.
also, ~maybe pre-eclampsia is caught if a woman's blood pressure runs high, but there's no way to check for protein in the urine. what happens when it turns into eclampsia? again, no way to induce labor. what if someone develops hellp syndrome.
none of these women got rhogam.
even in low risk pregnancies, 1 in 4 women need a c-section. was leslie performing c-sections? i know her speciality is apparently "anything we need her to be able to do" but, c'mon. really?
what if someone developed postpartum preeclampsia.
were these mothers more likely to develop puerperal fever due to high infection risk and limited medical supplies?
25-30% of people are positive for group-b strep. obviously they couldn't test for that. so potentially positive women were giving birth without antibiotics.
none of these babies got vitamin k or their first hep-b vaccine within the first 12 hours.
what happens to pregnant people who have, like, a missed miscarriage. if the body isn't expelling the tissue, you need a d&c or you're at risk for infection
ectopic pregnancies??? did women die from those in there??
plancenta previa or placental abruption???
hyperemesis gravidarum????
oligohydramnios or polyhydramnios?
were all 42 of these pregnancies just. complication-free?
chuck. i have questions. chuck. chuck. bat editoral of the 90s. help.
23 notes
·
View notes
Text
Congenital Clubfoot: Symptoms And Causes

Clubfoot is one of the most common birth defects of the foot. Out of one thousand new-born babies, one to two have this deformity. This deformity affects a new-born’s muscles, tendons, and blood vessels. It is caused when the tissues that connect the muscles to the bone are not the usual size. In congenital clubfoot, one or both feet are rotated downward and inward. It is also known as congenital talipes equinovarus in medical terms, and the child born with this deformity can’t place their foot flat on the ground for walking. Clubfoot is not painful, but if this congenital disease is not treated on time, the foot will remain deformed forever. Mostly, clubfoot can be treated without surgery, but in severe cases, follow-up surgery is required later on.
Types of Clubfoot
Clubfoot can be divided into two major categories non-isolated clubfoot and Isolated (idiopathic) clubfoot. Isolated clubfoot is a common musculoskeletal birth defect. It generally occurs without any other medical problems. On the other hand, non-isolated clubfoot happens along with other serious medical problems, including arthrogryposis and spina bifida. Arthrogryposis is a joint problem, and spina bifida is a neural tube disorder. If anyone in your family has clubfoot, your baby will be at higher risk of congenital clubfoot. Also, boys are at a greater risk of developing clubfoot than girls. Babies also have a higher chance of developing clubfoot if they have another birth defect known as spina bifida. Women who had oligohydramnios during pregnancy are also at a higher risk of having a clubfoot baby.
Symptoms of Congenital Clubfoot
If your new-born baby has clubfoot, their foot will be twisted inward and downward. The affected foot or leg will also be slightly shorter. In some cases, the foot is so severely turned that it seems as if it is upside down. Clubfoot is a serious health concern that will not improve on its own without any treatment. A baby with untreated clubfoot will use the outer edge of their foot to walk, leading to painful calluses. But with proper treatment, clubfoot can be treated, and your baby can lead a normal life.
How can clubfoot affect your baby
Clubfoot will not affect your baby until your child starts to walk. Untreated club food can limit your baby’s daily activities. They might have difficulty walking, standing, and wearing their shoes. A child with clubfoot may walk on the top and side of their feet. Clubfoot can also lead to calluses which is a thick layer of skin that usually develops on the foot’s sole. It can also lead to arthritis, a disease that causes stiffness and painful inflammation of the joints.
Causes of clubfoot
The definite cause of clubfoot has still not been identified by the researchers. But according to a popular theory, clubfoot is caused due to environmental and genetic factors. Families with a history of clubfeet are at higher risk of this disease. If a pregnant woman has one child with clubfoot, their chance of having a second child with this deformity is 1 in 35. In some cases, clubfoot is also linked to spina bifida, a congenital deformity that mostly occurs when the spinal cord and spine have not formed properly. Sometimes it can be linked to a developmental dysplasia of the hip or a developmental hip condition called hip dysplasia. If one of the parents has clubfoot, there is a 1 in 30 chance that your baby will have it. In 20016, research was conducted in which it was shown for the first time that a gene variation that processes folate in the body might be the cause of clubfoot.
2 notes
·
View notes
Text
Chỉ số nước ối AFI là gì và có ý nghĩa như thế nào?
Chỉ số nước ối AFI là gì và có ý nghĩa như thế nào?
Chỉ số nước ối AFI (Amniotic Fluid Index) là một phần của quá trình đánh giá nước ối trong tử cung của một bà bầu. Nước ối là chất lỏng trong túi nước ối bao bọc thai nhi trong tử cung và có vai trò quan trọng trong việc bảo vệ và cung cấp môi trường cho sự phát triển của thai nhi. Chỉ số AFI được tính dựa trên kết quả siêu âm thai kỳ.
Cụ thể, để tính chỉ số nước ối AFI, bác sĩ sử dụng siêu âm thai để đo chiều sâu của túi nước ối ở nhiều vị trí khác nhau trong tử cung của bà bầu. Sau đó, các giá trị đo được tổng hợp lại để tạo thành chỉ số tổng lượng nước ối. Chỉ số AFI thường được tính bằng cm hoặc được đánh giá dưới dạng số.
Ý nghĩa của chỉ số nước ối AFI là đánh giá mức lượng nước ối có sẵn trong tử cung của một bà bầu. Mức nước ối có thể thay đổi theo thời gian trong suốt thai kỳ. Mức nước ối thấp (oligohydramnios) hoặc mức nước ối cao (polyhydramnios) có thể gây ra các vấn đề sức khỏe cho thai nhi và mẹ.
Oligohydramnios (nước ối thiếu): Có thể gây ra vấn đề về phát triển của thai nhi, vấn đề về hệ tiết niệu của thai nhi, hoặc nguy cơ sinh non tăng lên.
Polyhydramnios (nước ối quá nhiều): Có thể gây ra vấn đề về tiền sản giật, khó đặt thai, hoặc vấn đề về dây rốn.
Chỉ số nước ối AFI giúp bác sĩ theo dõi và đánh giá mức nước ối trong tử cung của bà bầu và có thể giúp trong việc xác định xem cần thực hiện các xét nghiệm hay can thiệp y tế nào để bảo vệ sức khỏe của thai nhi và mẹ.
1 note
·
View note
Text
2023 Icd-10-cm Prognosis Code O41 8x90: Different Specified Issues Of Amniotic Fluid And Membranes, Unspecified Trimester, Not Relevant Or Unspecified
If you might be involved about your pregnancy, you must converse along with your healthcare provider. The reverse of oligohydramnios is polyhydramnios, an excess quantity of amniotic fluid in the amniotic sac. Interestingly, these 24-hr BMP therapy samples present totally squamous amnion cysts which might be morphologically and molecularly much like these handled over 48-hr. That is, they show uniformly squamous cyst morphogenesis and outstanding expression of GATA3, TFAP2A and ISL1, (Fig. 1I,J, quantitation for fluorescent intensity and nuclear side ratios in Fig. 1K,L), as well as relatively similar nuclear pSMAD1/5 alerts (Fig. 1M).
AmnioBand SL is a minimally processed human allograft which retains the structural properties of the amnion extracellular matrix. AmnioBand SL incorporates progress factors and cytokines that assist the membrane’s native function to advertise cell proliferation and tissue reworking during the wound therapeutic section. AmnioBand SL is out there in rectangular and circular shapes starting from 0.79 square centimeter to forty nine square centimeters. The Provant Wound Closure System (Regenesis was cleared by the FDA as a wound therapeutic device primarily based on a 510(k) premarket notification. Treatment with the Provant System is normally administered for 30 minutes right through dressing twice-daily.
Dermis on Demand (DOD) allograft is a human cell-, tissues or mobile, or tissue-based product (HCT/P). It is an allogeneic, processed acellular dermis supposed for homologous use solely, including the supplemental support, safety, reinforcement or covering of soft tissue. This allograft is a 5-year shelf stable human dermis product that can be utilized to augment current delicate tissue directly in line with existing surgical procedures.
types of placenta
There is a lack of proof within the peer-reviewed published medical literature to support the effectiveness of Supra SDRM. There is an absence of proof within the peer-reviewed published medical literature to support the effectiveness of Relese. There is a lack of evidence within the peer-reviewed published medical literature to assist the effectiveness of MLG Complete. The skin regeneration system requires a blood provide for the development of a neo-dermis from both bone or neighboring mucosa in the defect.
Even after profitable surgery, these procedures usually result in lowered joint mobility and tendon or ligament strength. A novel flowable tissue matrix allograft, derived from human placental connective tissue, has recently been made obtainable for minimally invasive remedy of damaged or insufficient tissue (PX50®, Human Regenerative Technologies LLC, Redondo Beach, CA). Based on the common role of connective tissue in the physique, and its reported anti-microbial, anti-adhesive, and anti inflammatory properties, these researchers assessed the effects of using this placental tissue matrix in the treatment of a series of decrease extremity accidents. In this pilot examine, 9 of 10 sufferers reported ache levels of 2 or less by week 4 utilizing the visible analog scale (VAS) ache scale.
Glyceraldehyde phosphate dehydrogenase (GAPDH) was used as endogenous control and the primer sequences had been proven in Table 1. The cells migrate both towards the amniotic cavity and yolk sac side or towards the cytotrophoblast aspect, abandoning an area in the center. By day 10, some epiblast cells differentiate into extraembryonic mesoderm, they usually settle between the amniotic cavity and the cytotrophoblast, ultimately creating a thick layer of extraembryonic mesoderm tissue between the 2. So mainly, by the middle of the second week, the two-layered embryonic disc is sandwiched between the amniotic cavity and the yolk sac. During day 9, hypoblast cells start emigrate to type a skinny membrane lining the rest of the blastocoel, forming the walls of the yolk sac. Medtronic Allograft Tissue covers surgical procedures in spinal, orthopedic, sports activities drugs, and dental functions — literally from head to toe.
Cytokines and development elements, epidermal development factor and transforming progress factor-beta3 in Grafix CORE mediate integral occasions corresponding to angiogenesis, cell recruitment and proliferation. Once thawed and rinsed, Grafix CORE is utilized to the wound and lined with a normal, non-adherent dressing. Additional applications are used as needed with frequency starting from each 7-14 days until the wound is closed. Grafix CORE is equipped as a cryopreserved membrane mounted on nitrocellulose paper and is on the market in 2 sizes; 2cm x 2cm and 5cm x 5cm. According to the producer, the presence of MSCs in Grafix distinguishes it from all other pores and skin substitutes. AmnioAMP-MP (Stratus BioSystems), a decellularized dehydrated human amniotic membrane (DDHAM) which is derived from the placental amnion and includes epithelial and stromal components that provide a collagen-rich extracellular matrix, cytokines, and progress components.
Biobrane does provide the pediatric affected person with burns immediate comfort and protection, and enhances patient compliance and parental satisfaction. These researchers in contrast the effectiveness of Biobrane and Duoderm for the therapy of small intermediate thickness burns in kids in a potential, randomized fashion to determine their relative impact on wound therapeutic, ache scores, and value. Patients under 18 years of age with intermediate thickness burns on a surface area lower than 10 % were enrolled and handled with one of many two dressing techniques. Data collected included mechanism of injury, time to finish therapeutic, ache scores, and institutional cost of materials till healing was complete. No vital distinction in time to healing or pain scores was detected between the 2 teams.
Similarly, AM decreased severity of peritendonous adhesion formation macroscopically and histologically and resulted in greater active and passive vary of movement in an identical chicken mannequin [32]. These variations were more pronounced when augmented with hyaluronic acid to protect towards AM breakdown. Willett and colleagues investigated the use of an injectable formulation of dehydrated human amniotic/chorionic membrane (dHACM) for the treatment of OA in rats [25].
In breast reconstruction, it closes the house between the pectoralis muscle and the chest wall. Often a number of items of AlloMax are sutured collectively to repair an abdominal wall wound or defect. According to the producer, there are significant differences in product attributes even among comparable products. The strategy of peripheral nerve restore and regeneration is affected by a number of elements, such as the encircling microenvironment, in which native scar adhesion is especially important [36].
#placenta banking#placenta position#amnion#types of placenta#placenta tissue banking#placenta banking benefits#placenta cord blood banking#placenta stem cell banking#cord blood and placenta banking#placental cells#what are placental cells#amnion and placenta#amnion stem cells#placenta amnion#placenta and amnion
1 note
·
View note
Video
youtube
Oligohydramnios #whylowamnioticfluidinthirdtrimester,#lowamnioticfluid,#whatslowamnioticfluid,#canlowamnioticfluidcausecramping,#Islowamnioticfluidisdangerous,#dr.j,#ayurvedaoverwesternmedicine,#ayurvedaanccare,#garbhasanskara,#ayurvediyagarbhasanskara,#1sttrimesterofpregnancy,#2ndtrimesterofpregnancy,#3rdtrimesterofpregnancy,#pune,#india,#amnioticfluid amniotic fluid [ 7.9cms to 12.74cms in 1 month]@d...
0 notes
Photo

#volume 1 #volume 2 #CPT #hcpcs #alphabeticalindex #ICD #ICD 10CM #medicalbilling #medicalcoding #insurance #medicalcodingtraining #healthcareindustry #rcmbusiness #coding #drram #drramasubbu This video discusses human placenta and its layers – decidua, chorion, amnion and the fluid which is amniotic fluid. Conditions like polyhydramnios and oligohydramnios are gone over together with the goal treatment which is amniocentesis done…
0 notes
Link
In this article, you will get to know about oligohydramnios, including their symptoms, causes, prevention, and much more. Read this article by the Fetal Well Being Scan Clinic ofAylesbury in detail to know all about it.
#Fetal Health Scan Aylesbury#baby scan clinic aylesbury#gender scan clinic aylesbury#4d baby scan clinic aylesbury
0 notes
Text
قلة السائل السلوي – Oligohydramnios لماذا يحدث وكيف يمكن علاجه
قلة السائل السلوي هي حالة تحدث أثناء الحمل حيث يكون السائل الأمنيوسي المحيط بالجنين أقل من المعتاد. تعرف على أشهر أسبابها، وطرق تشخيص قلة السائل الأمينوسي.
0 notes
Text
Introduction to High-Risk Pregnancy- What Does It Mean

Pregnancy can indeed be a joyous time, but it can also be overwhelming and stressful. Expectant mothers need to take care of themselves and their unborn babies. However, for some women, their pregnancy is considered high-risk.What is a high-risk pregnancy? It means the mother has an increased chance of experiencing complications during pregnancy, labor, delivery, and even after birth. Understanding this can help expectant mothers plan accordingly.Factors that contribute to high-risk pregnancy can vary from woman to woman. Some common factors include age, weight, medical history, and lifestyle choices. Awareness of these factors can help women make informed choices during this crucial time.So, let's dive deeper and understand what medical conditions can cause high-risk pregnancies and how to reduce the risks.So, let's get started!High Risk Pregnancy: Quick Overview!Pregnancy is a unique and beautiful journey, but it has challenges. As the name suggests, a high-risk pregnancy involves a higher likelihood of complications than a typical pregnancy. These complications can arise due to various factors, such as pre-existing medical conditions, age, or a history of pregnancy-related issues. Let's explore some common aspects that can categorize a pregnancy as high-risk.Factors that Contribute to High-Risk Pregnancy!Age is one of the factors that contribute to high-risk pregnancy. Women older than 35 are at increased risk. Other factors include Pre-existing medical conditions, Multiple pregnancies, substance abuse, and more.According to the insights, high-risk pregnancies accounted for 11.5% of all pregnancies, whereas moderate pregnancies accounted for 21.6%. 33.1% of pregnancies overall had high or medium risk.Pregnancy brings a lot of physical changes in a woman's body, making it more vulnerable to certain medical conditions. Some medical conditions that can cause high-risk pregnancy include hypertension, gestational diabetes, and preeclampsia.1. HypertensionHypertension or high blood pressure is a condition in which the mother's blood pressure is higher than the ideal range. Hypertension can lead to complications such as preterm labor, low birth weight...2. Gestational DiabetesGestational diabetes is a condition that can really affects pregnant women who didn't have diabetes before pregnancy. It indeed leads to high blood sugar levels, which can indeed cause complications such as preterm labor, macrosomia or a giant baby, and respiratory distress syndrome.3. PreeclampsiaPreeclampsia is a condition that affects pregnant women after 20 weeks of gestation. It leads to high blood pressure and damage to organs like the kidneys and liver. Preeclampsia can cause complications such as preterm delivery, low birth weight, and long-term health problems for both the mother and the baby.
Continue Reading: https://www.drshubhragoyal.com/welcome/blogs/introduction-to-high-risk-pregnancy--what-does-it-mean
#High Risk Pregnancy#Pregnancy with heart disease#Rh incompatibility#Oligohydramnios#Uterine fibroids pregnancy#Pregestational diabetes#Cervical insufficiency#Pregnancy after 35#Recurrent miscarriages#Intrauterine growth retardation#Placental abruption#VBAC risks (Vaginal Birth After Cesarean)#Perinatal infections#Pregnancy-induced hypertension#Chronic kidney disease pregnancy#Antiphospholipid syndrome pregnancy#Congenital anomalies risk
1 note
·
View note
Text
UpToDate Article on Term PROM
Prelabor rupture of membranes refers to rupture of the fetal membranes prior to the onset of regular uterine contractions. Over 50% of expectantly managed patients will be in active labor within 1 day and 95% will be in active labor within 3 days.
The most prudent approach is prompt assessment to confirm membrane rupture, determine fetal position, evaluate maternal and fetal status, and discussed options for further management.
You diagnose prelabor rupture of membranes based on the history and physical exam showing fluid flowing from the cervical os or a diagnostic test on the fluid that is in the posterior fornix.
Fetal well-being is evaluated with a nonstress test (NST). You can do a transabdominal ultrasound or use Leopold's maneuvers to determine fetal position. Evaluate the mother by assessing for contractions, signs of infection, and oligohydramnios (single deepest pocket less than 2 cm or amniotic fluid index less than or equal to 5 cm). Get baseline labs such as CBC (WBC greater than 20,000 could indicate chorioamnionitis).
For term patients with PROM, you can either induce labor with oxytocin or manage expectantly. Prompt intervention reduces the risk of cord prolapse or abruption. Labor tends to be longer with induction rather than letting it begin spontaneously.
Obviously signs of infection would be an indication to stop expectant management and just induce labor. Inducing labor reduces the risk of chorioamnionitis, endometritis, and neonatal sepsis.
ACOG recommends delivery for patients with PROM at greater than or equal to 37 weeks but also states that a short period of expectant management may be offered.
As long as there are no contraindications to labor and vaginal delivery, you can induce with oxytocin without preinduction cervical ripening. You can also use prostaglandins, but there is no evidence that they work better than oxytocin.
The UpToDate article says that they suggest not using a balloon catheter for cervical ripening in the setting of PROM because of the increased risk of chorioamnionitis. A balloon catheter (Cook catheter) dilates the cervix mechanically. [Last week, one of the attendings did use a Cook catheter as well as oxytocin for induction of one of her patients. But she hadn't ruptured yet.
For patients who do not want to be induced, you can manage expectantly as long as they have reassuring fetal testing, no contraindications to labor and vaginal delivery, and no sign of clinical chorioamnionitis or other medical or obstetric complications that increased maternal/fetal risk if delivery is delayed.

ROM plus is a test to help you determine whether the membranes have ruptured. The ROM Plus® Rupture of Membranes Tests are unique in that they detect both Alpha-fetoprotein (AFP) and Insulin-like growth factor-binding protein 1 (IGFBP-1) using a monoclonal/polyclonal antibody approach–improving its sensitivity.
1 note
·
View note
Text
The Effect involving Tranexamic Acidity as well as Tourniquet Experience Tibial Cement Puncture within Major Overall Knee Arthroplasties
Conclusion The particular prognosis of first starting point kidney oligohydramnios can be bad. Predictive factors regarding survival tend to be: GA in diagnosis, character of kidney abnormality (hydronephrosis as opposed to additional), and also presence of connected flaws. Copyright laws. (Chemical) This year David Wiley & Kids, Ltd.Salvia miltiorrhiza (SM), a new commonly common Oriental natural herb, can be produced in numerous regions in The far east. Discovering Text expanded in various regions regarding Cina is tough, and so genotyping these kind of selections will be very useful. Based on the strategies of sequence-related increased polymorphism and target place zoomed polymorphism, a manuscript PCR-based molecular marker approach named protected place sound polymorphism (CoRAP) will be documented within this research to genotype Text messages. The actual CoRAP way is based on the use of a pair of primers: preset along with arbitrary primers. The former is derived from targeted EST series lodged within Genbank; although, the main sequence (CACGC) with the last option is often a conserved region within many introns. In today's examine, we utilized CoRAP in order to genotype Text message from various geographical roots. PCR boosting is carried out regarding Thirty menstrual cycles in an annealing temperatures regarding Fifty-two diplomas H. Every PCR response has generated possibly 30-50 fragmented phrases of fifty to at least one,Thousand blood pressure in dimensions. The successful Genetic genotyping of Text message by simply CoRAP was attained. This specific brand new genotyping method is fast, efficient, as well as reproducible.When frontrunners of the technique choose to go after Magnetic field (R) status, a mandatory high-stake choice is actually to be able to go after this specific designation being a method or even person organizations in the system. To aid market leaders to help make the finest choice, your experts assess the pros and cons regarding program vs . single-entity hunt for Magnet position to help you a method key nursing jobs police officer to ascertain in the event the chance will be worth the acquire.Your impact of an acid comonomer on the architectural Nirmatrelvir cost progression and thermal behaviours of a polyacrylonitrile (PAN) terpolymer that contain about Four.Nineteen wt % methyl methacrylate as well as 2.Ninety-eight wt % itaconic acid (IA) throughout a heating system remedy have been studied simply by Fourier enhance home (FTIR) spectroscopy, differential deciphering calorimetry (DSC), as well as thermogravimetry (TG) and weighed against the Griddle homopolymer. In the outcomes of FTIR spectroscopy as well as DSC, we learned that the presence of the particular IA comonomer advertised cyclization reactions faster as well as widened the actual exothermic optimum; this specific reduced your power heat launch. Simply by evaluating the outcome of the TG files, all of us found out that the existence of the IA comonomer endorsed dehydrogenation tendencies along with the enhancement of a giant quantity of much better step ladder houses. In, the better corporate constructions in which created have been much easier to change from steps buildings straight into graphitelike constructions.
#PI3K Inhibitor Library#JNK inhibitor#PD-1/PD-L1 inhibitor#IU1#Shikonin#Paeoniflorin#Zebularine#Pitavastatin#Caspofungin#Fisogatinib#SANT-1#Piperlongumine#Pioglitazone#Go6976#Asunaprevir#StemRegenin 1#AZD7545#Mifepristone#EED226#Adavivint#NSC-9900#R 41400#ZK-62711#MK-1439#GS 0840#BMS-232632#GS5885#VX-478#ABT-267#ABT-450
1 note
·
View note
Link
0 notes
Text
The Polish state is responsible for the death of a woman in 22 weeks of pregnancy with an oligohydramnios.
Doctors waited for the fetus to die.
In the meantime, the woman died without receiving help.
There are no words.
False defenders of life have the lives of Polish women for nothing.
Really, it is hard to want to live in a country where no one even conceals their hatred of women any more.
#the last few days really made me barely holding up anymore#i have no strength in me no more#poland#abortion#pregnancy#death#pro choice#pro life#feminism#women's rights#women's health
87 notes
·
View notes
Text
Imaging of ARPKD


Autosomal recessive polycystic kidney disease (ARPKD) is often first suspected at prenatal or neonatal ultrasound. Imaging features include enlarged, echogenic kidneys, with poor corticomedullary differentiation, often without discretely discernible cysts. If a linear (high frequency) probe is used, small tubular cysts can be seen, which are the ectatic collecting ducts.
Hepatic fibrosis and biliary abnormalities are associated with ARPKD, and these can also be seen on ultrasound. In patients with severe hepatic fibrosis, splenomegaly and portosystemic varices may also be present.
Case courtesy of Dr Alexandra Stanislavsky, Radiopaedia.org, rID: 14079. Enlarged, echogenic kidneys with poor corticomedullary differentiation in a neonate who had previously had oligohydramnios on prenatal ultrasound. A few discrete cysts are present.
6 notes
·
View notes