#and andrew’s just like. showing symptoms of severe depression and ptsd
Text
nicky and aaron: when andrew’s on his meds he’s unhinged, but you haven’t seen him when he’s sober! he’s so much worse
andrew off his meds: *has clinical depression*
nicky and aaron: he’s craaazy
#I can’t stop thinking about nicky saying andrew is soulless when he’s off his meds#and andrew’s just like. showing symptoms of severe depression and ptsd#like bestie…#when neil said is anyone else calls andrew soulless he’ll have to fight them#I get it neil. I get it#andrew minyard#aaron minyard#nicky hemmick#aftg#andreil#tfc#all for the game#the foxhole court
3K notes
·
View notes
Text
Why PTSD May Plague Many Hospitalized Covid-19 Survivors
https://sciencespies.com/nature/why-ptsd-may-plague-many-hospitalized-covid-19-survivors/
Why PTSD May Plague Many Hospitalized Covid-19 Survivors

While neuropsychologists Erin Kaseda and Andrew Levine were researching the possibility of hospitalized Covid-19 patients developing post-traumatic stress disorder (PTSD), they heard reports of patients experiencing vivid hallucinations. Restrained by ventilators and catheters, delirious from medication and sedatives and confused by the changing cast of medical professionals cycling through the ward, intensive care unit (ICU) patients are especially prone to trauma. For Covid-19 ICU patients, a combination of factors, including side effects of medication, oxygenation issues and possibly the virus itself, can cause delirium and semi-consciousness during their hospital stay. Kaseda says as these patients slip in and out of consciousness, they may visualize doctors wheeling their bodies to a morgue or see violent imagery of their families dying. Such instances, though imagined, can cause trauma that may lead to PTSD in patients long after they have physically recovered from Covid-19.
In addition to hallucinations during hospitalization, some Covid-19 survivors describe a persistent feeling of “brain fog” for weeks or months after recovery. “Brain fog” is an imprecise term for memory loss, confusion or mental fuzziness commonly associated with anxiety, depression or significant stress. As scientists grappled with whether such brain damage could be permanent, Kaseda and Levine warn that cognitive issues often attributed to “brain fog” may, in fact, be signs of PTSD. Kaseda, a graduate student at Rosalind Franklin University of Medicine and Science in Chicago, and Levine, a professor of neurology at the University of California Los Angeles, co-authored a study published in Clinical Neuropsychologists in October intended to alert neuropsychologists to the possibility of PTSD as a treatable diagnosis for those who survived severe illness from Covid-19.
“You have this unknown illness: there’s no cure for it, there’s high mortality, you’re separated from your family, you’re alone,” Kaseda says. “If you’re hospitalized that means the illness is pretty severe, so there’s this absolute fear of death that even if you aren’t having the delirium or the other kind of atypical experiences, just the fear of death could absolutely constitute a trauma.”
How Post-Traumatic Stress Develops in Covid-19 Patients
PTSD arises from experiencing or witnessing a traumatic event, specifically exposure to actual or threatened death and serious injury, according to the American Psychiatric Association.
Historically associated with combat veterans, PTSD was called “shell shock” or “combat fatigue” before it became a named disorder in 1980. But in 2013, the definition of PTSD broadened to include more common place traumatic experiences.
Psychiatrists are now increasingly seeing PTSD develop after traumatic stays in the ICU for any health problem, but researchers are still unsure of the scope of this issue. A paper published in 2019 in the Lancet reports that roughly a quarter of people admitted to the ICU for any health issue will develop PTSD. Another study found that between 10 and 50 percent of people develop PTSD after ICU discharge, and, in a 2016 study of 255 ICU survivors, one in ten reported PTSD within one year after discharge.
Before hospitalized patients are diagnosed with PTSD, their symptoms may be described as post intensive care syndrome (PICS). PICS can manifest as a number of physical, cognitive and mental health problems that a patient may experience in the weeks, months or years after being discharged from the ICU.
Kristina Pecora, a clinical psychologist at NVisionYou in Chicago, sees a variety of patients, including frontline medical professionals and Covid-19 survivors. Pecora was a contributing author of a brief submitted to the American Psychological Association in May describing the signs of PICS and urging psychologists to prioritize screening and referral for behavioral health problems related to hospitalization for Covid-19. At that time, some of Pecora’s patients showed signs of the lingering trauma typical of PICS within six months of their ICU discharge. Because a PTSD diagnosis can often only be made after this period, it was too early to tell then whether her patients’ PICS symptoms could be classified as PTSD. But the impact of the virus on their psychiatric health was clearly substantial.
“It becomes this gradual realization that what they’re experiencing is persisting week after week and ‘oh my goodness, this is a longer-term experience than what we thought it would be,’” Pecora says.




Restrained by ventilators and catheters, delirious from medication and sedatives and confused by the changing cast of medical professionals cycling through the ward, ICU patients are especially prone to trauma.
(Photo by Sebastian Gollnow/picture alliance via Getty Images)
A “Delirium Factory”
One major factor in whether patients develop long-term psychological effects after ICU discharge is whether or not they experience delirium during their stay. Delirium is a state of severe confusion and disorientation, often characterized by poor memory, nonsensical speech, hallucinations and paranoia. Patients who experience delirium may not be able to differentiate between real and imagined humans or events.
Side effects of sedatives, prolonged ventilation and immobilization are common factors that put many ICU patients at-risk for delirium. A study from 2017 found that up to 80 percent of mechanically ventilated people enter a hallucinogenic state known as ICU delirium.
Add isolation and the unknown cognitive effects of the virus to the mix and an ICU becomes a “delirium factory” for Covid-19 patients, as authors of a study published in BMC Critical Care in April wrote. In a different study from June, which has not yet undergone peer review, 74 percent of Covid-19 patients admitted to the ICU reported experiencing delirium that lasted for a week.
“Any time anyone is in a fearful experience and they’re isolated—they can’t have anybody in their rooms—they wake up in a strange experience or a strange place, or they know already while they’re in there that they can’t have anyone hold them or be with them. All of that is going to attribute to the emotional impact,” Pecora says.
Such intense visions and confusion about the reality of hospitalization can be especially scarring, leaving patients with intrusive thoughts, flashbacks and vivid nightmares. If such responses persist for more than one month and cause functional impairment or distress, it may be diagnosed as PTSD.
To help reduce ICU-related trauma, doctors may keep a log of the patient’s treatment to help jog their memory once they have been discharged. Having a record of the real sequence of events can help a patient feel grounded if they have hallucinations and flashbacks to their hospitalization experience.
But even for patients experiencing Covid-19 symptoms that aren’t severe enough to warrant a hospital visit, the fear of death and isolation from loved ones can be sufficiently distressing to cause lasting trauma. They may experience shortness of breath and worsening symptoms, fueling a fear that their condition will quickly deteriorate. For several days, they may avoid sleeping for fear of dying.
“Some people are more resilient in the face of that sort of trauma and I would not expect them to develop lasting psychological symptoms associated with PTSD,” says Levine. “But other people are less resilient and more vulnerable to that.”
Learning from SARS and MERS
Covid-19 isn’t the first epidemic to cause a domino effect of persisting psychiatric health problems across a population. The current pandemic has been compared to the severe adult respiratory syndrome (SARS) outbreak in 2003 and the Middle East respiratory syndrome (MERS) outbreak in 2014 in Saudi Arabia—both diseases caused by coronaviruses. In an analysis of international studies from the SARS and MERS outbreaks, researchers found that among recovered patients, the prevalence of PTSD was 32.2 percent, depression was 14.9 percent and anxiety disorders was 14.8 percent.
Much like those who fall ill with Covid-19, some patients sick with SARS and MERS developed acute respiratory distress syndrome (ARDS), which causes patients to experience similar feelings of suffocation and delirium during treatment in the ICU. Levine says that many of the people who developed PTSD during the SARS and MERS epidemics were hospitalized.
By contrast, Levine anticipates Covid-19 survivors with relatively mild symptoms may experience traumatic stress too, due to an inundation of distressing images, frightening media reports and a higher expectation of death.
For those who recover from Covid-19, their trauma may be compounded by social isolation and physical distancing practices after they are discharged from the hospital. “If you did experience a trauma, it can make it so much harder to naturally recover from that when you lack the social support from family and friends that maybe would be possible to receive in different circumstances,” Kaseda says.
Screening for PTSD in Covid-19 survivors soon after recuperation is important, Kaseda says, so that patients can receive the right treatment for their cognitive difficulties. If PTSD is treated early on, it can speed a person’s entire Covid-19 recovery.
“If we can treat the PTSD, we can see what parts of the cognition get better,” Kaseda says. “And that will give us more confidence that if problems persist even after the PTSD is alleviated, that there is something more organic going on in the brain.”
A Constantly Shifting Landscape
As more information about the traumatic effects of Covid-19 treatments become clear, neuropsychiatrists and psychologists can shift their approach to dealing with the cognitive effects of Covid-19. Scientists don’t yet have a full grasp on how Covid-19 directly affects the brain. But by maintaining an awareness of and treating PTSD in Covid-19 patients, psychiatrists and clinicians may be able to minimize some cognitive problems and focus on the unknowns.
“Part of the problem is that all of this is so new,” Pecora says. “We’ve only really been seeing this for six or seven months now and the amount of information we have gleaned, both in the medical and the psychological worlds has increased so exponentially that we have a hard time keeping up with what were supposed to be looking out for.”
Deeper understanding of which symptoms arise from brain damage and which are more psychological will help both clinicians and psychologists address patients’ needs in their practice.
“The social and emotional impact of Covid-19 hasn’t even dawned on us yet. We clinicians and doctors are certainly trying to prepare for it.,” Pecora says. “But the way this has impacted society and mental health is going to be so vast.”
#Nature
0 notes
Photo

The Suicidal Elephant in the Parlour
or Anne of Green Gables and Depression, Loss, & Suicide
by Adrianna Prosser
It’s no secret I’m a redhead, and it’s likely no surprise that when I was young I pretended I was Anne of Green Gables. In fact, my first best friend from junior kindergarten was a raven haired girl that I nicknamed Diana (hi Erin!) and she in turn called me Anne. When I was 14 I played Anne in my regional community theatre show in the musical (see community newspaper photo below) and it caused quite a stir: the theatre sweetheart who was supposed to play Anne with her beau as Gilbert was thwarted by me, an awkward untrained teenager who already knew the libretto by heart and I owned a straw hat. That show defined my love for theatre and my love of Anne transformed into a love of performing and storytelling. Anne was my life. Anne was me. From her temper to her bombastic nature, her hyperbolic narratives and of course her wild imagination, and let us not forget her competitive nature at school was all playing out pretty much the exact same way only in 1980s Canada in Barrie, instead of PEI in the 1880s.

^1998 newspaper article photo with me and my “schoolmates” in Avonlea school for South Simcoe’s Anne of Green Gables musical production in Cookstown, Ontario.
Naturally I watched the Megan Follows series of Anne until the VHS tapes wilted and wouldn’t play in my VCR. I used the musical version as my audition songs to get into theatre school and plays. I even grew up to be a schoolhouse teacher in a 1910 museum where I involuntarily (ok ok I did it on purpose) looked like Anne in Anne of Avonlea when she gives up her scholarship to stay with Marilla and teaches at the nearby school. I made time in my curriculum to read aloud from Anne of Green Gables the infamous chapter “Tempest in the School Teapot” to my grade 3’s and did voices for Diana, Anne, Gilbert and Mr Andrews; the crack on the head was always the best part played by the schoolhouse strap and a quick thwack to an antique desk. The kids would jump and laugh and want me to read more - what happened to Anne with an e?
Anne has been a big part of my life since I was 5 years old.
Then the CBC casts RH Thompson as Matthew and all of a sudden I’m back in Avonlea with earnest dread: what are they doing to Anne? I hear mixed reviews, I can’t seem to make myself watch it. It has been years since I have shed tears for the reveal of LM Montgomery’s secret: her granddaughter went public to say that Lucy had died by suicide. There was a note in her journal that seemed to indicate as much. I haven’t grieve the author of my youth, but now with this new rendition coming to TV I was going to have to face much more than childhood memories.

The CBC version called Anne The Series is wonderful: the vistas, the costumes, the character work… but there is something hard and dark around the edges. Gone are the warm hues, the bright scenery, the soft focus - this version has the contrast up, the grit and clarity filter showing weathering and wrinkles, and blues and greys highlight most every scene. I am intrigued to see some scenes play out exactly as I remember, and then others make me weep.
I enjoy adaptations, I am an actor and playwright and have read and performed several Shakespearean renditions of the same title over and over again in different ways throughout my career. I get it. Why do the exact same thing when it’s been done before? My thoughts and feelings are that of someone who GETS IT. I liked that in 2017 when this version premiered, we have such days celebrating mental health and focusing on mental illness like #MentalHealthWeek or #BellLetsTalk or suicide prevention day is September 10th and we as a collective here in Canada are getting better at being mental health advocates and de-stigmatizing depression, therapy, suicide and mental illnesses to the point that we are able to talk about it in pop culture (ie. 13 Reasons Why, The Virgin Suicides, The Perks of Being a Wallflower, etc…) and we are left to unpack it at our own pace and level of understanding as an audience member. So when this Anne adaptation starts to inject Lucy Maud Montgomery’s narrative into Anne’s I feel two things:
OF COURSE now we can talk about this! Now we can interpret the reasons why Anne was talking to her reflection in a glass window and named her mirrored self Katie and talked to herself like as if she was two people - THAT isn’t normal. They could be dissociative disorder and throughout the show we see ways in which Anne has dealt with trauma, loss, and the loss of her innocence (though I don’t think rape was implied she has heard and or seen sex and possibly witnessed rape in this adaptation,) at such a young age that of course she needs imaginary friends to help her deal with her situation, or even just the profound loneliness she lives. OF COURSE there would be residual PTSD moments that leave Anne riddled with inaction and mental scarring hearing from every person that she is not a person but a tool to keep the household running and forced to care for three sets of triplets; being told all the while that she is not a family member and reminded of it constantly. OF COURSE we should raise awareness of the things that were happening in Canada around this time like the beginnings of the Suffragettes and women’s rights activism, and of course we should inject that history into a retelling where we as a viewing audience can accept that lens showing us a bit beyond the warm fuzzy historical narrative we are used to.
BUT. And it’s a but I am still struggling with… When the show paints a portrait outside of what’s in the book and rewrites the scope of its characters ambitions and actions - I get mad. And I don’t know why. The specific scene I’m talking about is when Matthew, brilliantly portrayed by RH Thompson (of Road to Avonlea fame,) Here is the show and the book version:
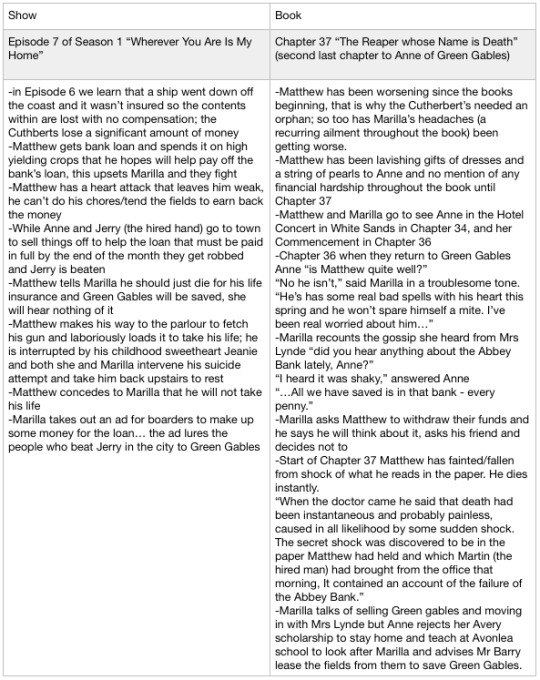
Having re-read all of Anne of Green Gables to see where the artistic liberties by Walley-Beckett for the CBC version (she wrote on Breaking Bad and I joke that this is Breaking Anne,) are and where the book informs the adaptation. (I wanted to know if Marilla and Matthew had been given made-up backstories or if they were indeed in book *fun fact Marilla WAS courted by John Blythe, but the Jeanie button story, though adorable, never happens for Matthew as we are constantly reminded in the book of how shy he is to women, Anne being the only exception.) And of course the suicide scene was never in my recollection but I had to be sure that as a child I wasn’t just misunderstanding LM Montgomery’s intentions.
This is where my very biased opinion takes the milk crate:
Matthew Cuthbert from the novel never exhibited depression, suicidal attempts, nor “invitations”. When I say invitations I mean the signs that one may perceive as invitations to recognize inner thoughts and feelings to be that of a suicidal nature. And the show version of Matthew also does not exhibit these invitations. But that is not to say that impulsive suicides don’t exist, just that they are very very rare. Also, in Christian Victorian society they are DOUBLY rare. So to, speaking to his character (in both book and show version) do I question Walley-Beckett and her exploitative use of suicide in this narrative - it seems wildly out of character and ridiculous.

It seemed the choice was made for ratings and getting fangirls like me bawk at this rendition and give buzz to the show rather than playing into the original story’s nuance - like how I applaud her use of mental illness in Anne and that is why she is the “gypsy witch” that everyone calls her in the book: it is why she isn’t like everyone else on the island because everyone else on the island hasn’t been abused like Anne has. The stigma of being an orphan is explored and highlighted with the picnic scene in the show that doesn’t happen in the book. Anne has to triumph over her snobby neighbours not once like in the book (she saves Diana’s sister from croup) but defies a RAGING HOUSE FIRE in the show at the Gillis homestead to save a child and help put out the fire (a nod to her reading everything under the sun even a fire fighting manual at the train station, a call back to the first episode).

Sure. I like the in-between the lines bits like that. In fact upon re-reading it a lot of the action doesn’t take place on the page, it is usually recounted to us by our grand storyteller Anne herself, so the events are wide open to interpretation because often LM Montgomery says ‘and the concert happened’ or ‘and the school year passed’ and that’s it. My friend JM Frey writes how "Anne is an unreliable narrator.” and I agree.
But, what I can’t handle is imposing trendy topics into a show that is near and dear to many a Canadian heart for the sake of ratings. I thought it a bit odd how blunt the feminist sewing circle was. Not in the book by the way but huzzah for modern narratives and exploring what that gossip and chit-chat would be at Mrs. Lynde’s sewing bees (in the book it’s her gatherings). And clearly what spurned this whole blog-novel is the suicidal elephant in the parlour...

Then the other side of my heart believes this is a good thing, this new Matthew who is depressed because he is getting older and can’t “spare himself a mite” and then his reluctance to listen to his sister leads to them losing all their money. He has the same symptoms of the men who jumped from the ledge of their workplace in the Great Depression. Guilt. Blame. Loss of hope. Burden. And being the sole provider, or being told that one is by culture and society, he is overwhelmed and not only that he is weak in body so he can’t fight as hard as he used to… is suicide so unheard of for our dear Matthew? Many a Christian soul has taken their own lives. Many a Victorian had too, so too our dear writer LM Montgomery is believed to have taken her own life just outside of Toronto proper at the house she nicknamed “Journey’s End.”
While I cannot deny my anger and resentment and frustration with this new rendition of Anne of Green Gables I am reminded that the original still lays intact on my bookshelf and I can re-read it anytime. That maybe this new Anne is taking characters we have invested our love and time with for over a century and that perhaps this unsettling feeling that Matthew would try to take his life is the exact hurt we need to feel to address the suicidal elephant in our own lives.
When my brother died by suicide I was, am, beside myself with questions, guilt, blame, and looking for reasons. This scene made me react in a similar visceral way, to be sure because I am suicide bereaved, but also I had a pre-existing connection with Matthew since I was 5 years old! Matthew is a fictional character and I am not equating him with my real life brother, but I can’t deny that the way this rendition of the story being told rattled me to the core, and I don’t think it would have elicited the same response with a new tv show about a teenage girl with a distraught father figure who attempts suicide after a huge money loss. My love and time wouldn’t be as invested, and so using a beloved cultural phenomenon like Anne to share these themes, and with a main character no less, seems…. bold. And perfectly infuriating for the right reasons.
So while I digest all these feelings I am resolved to let them stay in this area of grey. The show isn’t wrong and the book isn’t right, or vice versa. What I can take away with certainty that I am glad LM Montgomery’s work is being appreciated all over again, along with her new Heritage Minute
youtube
^which not only focuses on her talented writing, but that she wrote such an epic while struggling with depression. That message that you can still create and create great things while depressed is a message we need to hear and celebrate. We also need to own that some people are suicidal and we all need to step up our efforts to help our loved ones around us know that they can talk about it, seek help without judgement, and lean on us. There is no need to read between the lines like we are here with Anne, and we can ask our friends and family directly for help when we too have thoughts and feelings that make us want to end our lives.
“It was the last night before sorrow touched her life, and no life is ever quite the same again once that cold, sanctifying touch has been laid upon it.”
-LM Montgomery, Anne of Green Gables, Chapter 36 “The Glory and the Dream”
Thank you Anne for once again growing up with me and helping me understand my thoughts and feelings a bit better.

#anne of green gables#anne shirley#am reading#am watching#Anne the series#cbc#opinion#rant#depression#mental illness#lucy maud montgomery#lm montgomery#suicide#loss#grief#books#novels#tv show#adaptations#red head
2 notes
·
View notes
Text
mental heath disorders
Mental heath disorders
Before I move on with looking at my final piece Ideas, I wanted to reach mental heath disorders. Because it gives me more knowledge on the people that I’m trying to reach out to and better understanding of mental heath disorders.
Mental heath is a cognitive, behaviour and emotional well-being. It is all about how we think, feel and behave. This affects daily life, relationships and physical heath. This is why it is important to have a good mental heath so it has a positive effects on your life.
The term mental heath is sometimes used to mean an absences of a mental disorder (Timothy j legg.2020). There is more then 200 mental heath disorders. (Andy 2020) The most common are, Anxiety disorder, mood disorder[1],schizophrenia and psychotic disorder. (Dr Glen Xiong 2018).
Lots of people suffer with mental heath issues, in 2017 approximately 1 in 4 people in the UK alone had experienced mental heath problems. In England, 1 in 6 report experiencing a common mental heath problem (such as anxiety and depression) in any given week (anonymous 2017) , this roughly calculated up to 16 million people (MCManus,S 2017).
Bad Environments can effect your mental heath and lead into mental heath disorders. Certain genes may increased the risk of developing a mental illness and your life situation may trigger it. Environmental exposure before birth e.g. inflammatory conditions, toxins, alcohol or drugs while in the womb can sometimes be linked to mental heath. (Anonymous 2019)
Depression
Depression in psychology is defined as mood or emotional state that is marked by feelings of low self – worth or guilt and a reduced ability to enjoy life. This is a very common mental heath disorder.
When experiencing depression it feels like your thought are a heavy beg pulling of which you try and get off. You do this to try and feel slightly happy again but its stuck, it’s like your trapped in your own bad thoughts that screams at you. this is a 24/7 occurrence that is inescapable.
If you are suffering with depression, the best thing to do go to your GP and they will refer you onto the right support for you. Sometimes they send you to ether therapy or counselling as well as the option of medication. In the instance that your GP dose prescribe medication the best thing is to carry on taking it for the time they have set. although it maybe tempting to stop medication as your mood lifts, continue taking it for as long as the doctor recommends. Most doctor’s advise to taking antidepressants for six months to a year after they no longer feel depressed. (Brenda Conaway 2010)
In 2014, 19.7% of people in the UK aged 16 and over showed symptom of anxiety or depression – an 1.5% increase from 2013. (headscape2020)
Anxiety
Symptoms of Anxiety disorder is persistent and excessive anxiousness and worry about activities or events, even ordinary things such as going out the house (mayo cinic staff 2018) . Other symptoms can be nightmares, obsessive thoughts, even physical such as pain and headache (timothy j legg.2020). This is most likely to form into a panic attack when there overwhelmed. A panic attack is every common when you have anxiety disorder, for most people feeling like they can’t breath. When having this the best thing to do Is try the grounding or safe place skills.
Overall It has a massive effect on everyday life because it makes it harder to try new things, to take risks in the work place or personal life. Many people experiencing anxiety feel changed in. they see things they want to do in life but their anxiety keeps them from trying. This can lead into loss of income and unfollowed potential. (Recovery Ways 2018)
To get help with anxiety the best way is to go to the GP, They will try and give you the best help for you. the treatments for it is the same as depression, witch is therapy or counselling as well as the option of medication.
Anxiety and depression are closely linked togethers because it’s hard to differentiate between the two. In most cases one leads to the other; for example if you have bad anxiety you feel very anxious and don’t to go outside due to a fair of interacting. This will then you to stay in and over think witch get you into a bad headspace witch may turn into depression and vice versa. (Karl Nezbit 2020)
In 2013, there wear 8.2 million cases of anxiety in the UK (no panic 20180)
Bipolar
Bipolar disorder is a mood disorder. It’s a condition that causes extreme mood swings. The main symptoms are episodes of extreme highs and lows, which can last for several weeks. (NHS 2020)
Many people with bipolar are still highly functional Individuals and can maintain a healthy professional and personal life when taking treatments. The treatments Persist of medication and talking therapy. (NHS 2020)However, Untreated bipolar is more likely Worsen and interfere with daily life. This can lead into Suicidal thoughts and actions can occur in both manic and depressive episodes. ( timothy J Legg 2018)
In 2013, there wear almost 4 million cases of mood disorders In the UK. In 2014 Experts said younger people was More likely to have bipolar then older people. 3.4% of 16 – 24 year olds was screened positive but only 0.4% of 65-74 year olds screened positive. (Headscape 2020)
Why should we talk?
For people with mental health problems not being able to talk about it can be one of the worst parts of the illness. By getting people to talk about mental heath we brake that barrier down. This improve relationships and gets them on the path of recovery (Andrew Berrie 2019). Without talking, the problems will grow. They may end up using bad coping mechanisms such as self- harm, drug’s and alcohol. Which may lead into Addictions, because these substance effect the way you feel, both physic and mentally. These feelings can be enjoyable for a short Length of time this is called a “hight”, It create a Powerful urge to use the Substance again.
Addiction is when you feel like you need it and can’t life without it. This makes you start depending on it. You can get addicted to anything, not all addictions are bad. The most common addictions are drug, alcohol, gabling and Neurotics (NHS 2020). These all have negative effects on your mental heath, physical health.
Not all people that have addictions start off stuffing with mental heath issues. It may just be in there genetics. Experts have proven that children of addicts are 8 time more likely to become addicted then children of non – addicted family’s. As well, those with certain mental heath illnesses are more likely to develop addiction (Anonymous 2015).
To prevent this from starting or carrying on, the best thing is talking. Talking will help you to find professional help. That can give you heathy copping mechanisms such as safe place and grounding.
My own views
People who are struggling with mental heath issues. Feel alone and are suffering every second of every day and night there is no piece. What can we do to help? Read and learn about the issues, you don’t need to be an expert. You just need to listen and try and spot sights. This will help because then you can advise to them to go to the GP and get the best help they can. Alone side this you can help them with techniques, give the best advice you can to guide them alone the way.
Each mental heath disorder have there own methods to get better. I find with PTSD and anxiety the best thing Is to do grounding techniques this will give you a clear mind so all the bad thoughts will go away. I find for depression the best thing to do is wright about all the thought and feelings so there not stored in your mind pilling up. Then uses grounding techniques when you feel like it’s going to get worst that you can’t control. for each person they will have different techniques that are fit for helping them.
iv learnt a lot about the mental illnesses although when I was going thought this. The reach helped me because now I can been sensitive with how I go about my work and what other ways I should try and add to help people. This has also brought out the importance of having someone there to help so these people are not suffering alone.
0 notes