#gabaergic dysfunction
Text
Thanks to my recent Plans TM and shit + good conversations with @indigochromatic @whybrainhere and @reimeichan (shouting out cause they're awesome people / blogs and great individuals to chat about experiences with; ily guys) about ADHD and neurotransmitters I've started getting a bit really into reading about neurochemistry / neurobiology as well as the similarities and differences with Autism and I have to do something else so I havent finished reading this but for those that are interestsed
I found a really good article that is open access to read about the GABAergic function in autism across a large number of different studies and methods of exploring the relationship between GABA and autism.
It's a relatively "hard" read I think (especially in some parts if you aren't familiar with transgenic rodent models and genetics / neurobiology) but its really informative so far
For those up for it and with the time, I do recommend. It cites some interesting studies that have made my reading time on this stupid longer cause I keep falling down rabbit holes of the cited studies help
3 notes
·
View notes
Text
Best Natural Choice Of Remedy For Women's Sexual Dysfunction

Normal Female Sexual Function
Female sexual health is influenced by many physical and emotional factors. It is important for women to have a healthy sex life, which can improve their overall well-being.
The female sexual response involves the genitals, brain, and spinal cord. The brain releases chemicals called neurotransmitters that control sexual function. Hormones also play a role in sexual health.
A healthy sex life is important for women of all ages.
Different factors that contribute to female sexual health:
- Physical factors: These include the health of the genitals, the brain, and the spinal cord. Any condition that affects these organs can impact sexual health. For example, diabetes can damage nerves and blood vessels, which can lead to sexual dysfunction.
- Emotional factors: These include stress, anxiety, and depression. These can all affect sexual desire and performance.
- Hormonal factors: Sex hormones, such as estrogen and testosterone, play a role in sexual desire and function. Changes in hormone levels can affect sexual health. For example, menopause can cause a decrease in estrogen levels, which can lead to vaginal dryness and other problems.
FemVigor
FemVigor has helped millions of women around the world overcome their female sexual dysfunction, including low libido, vaginal dryness, and difficulty reaching orgasm. It has helped them to enjoy a healthy and fulfilling sex life, and has improved their relationships and overall well-being.
FemVigor is a unique herbal capsule that is specifically designed to help women with female sexual dysfunction. It is made from a blend of natural herbs that have been clinically proven to be effective in increasing blood flow to the vaginal area, improving sexual desire and satisfaction, and reducing the symptoms of female sexual dysfunction.
FemVigor is also free from any side effects, making it a safe and effective option for women of all ages. It is also doctor-endorsed, which means that it is a safe and effective product.
Why is FemVigor the preferred choice?
FemVigor is a popular choice for women because it is a safe and effective way to improve sexual health. It is made from natural herbs, so it does not have any harmful side effects. FemVigor can help to boost libido, prevent vaginal dryness, and increase energy levels. It is also doctor-endorsed, which means that it is a safe and effective product.
Ingredients:
Indian Kudzu (Pueraria tuberosa):
Indian kudzu is a plant that has been used for centuries in traditional medicine. It is known for its aphrodisiac, rejuvenating, and vitalizing properties. Indian kudzu also increases breast milk production in nursing mothers.
Due to its estrogenic activity, Indian kudzu can increase vaginal lubrication, clitoral sensitivity, and overall sexual response in females. It also acts on the cholinergic, GABAergic, adrenergic, and serotonergic systems, which can help to relieve anxiety and depression and improve sexual function in both males and females.
Here are some of the potential benefits of Indian kudzu:
- Increased libido
- Improved sexual function
- Reduced anxiety and depression
- Increased breast milk production
- Anti-inflammatory properties
- Antioxidant properties
- Cancer-fighting properties
Indian Spider Plant (Chlorophytum arundinaceum):
Chlorophytum arundinaceum, also known as the African spider plant, is a plant that has been used in traditional medicine for centuries. It is said to have aphrodisiac and libido-enhancing properties, and is also used as a tonic to strengthen the body.
Chlorophytum arundinaceum contains compounds that may help to reduce stress and improve sexual performance.
These compounds include:
- Flavonoids: These compounds have antioxidant and anti-inflammatory properties, which may help to improve blood flow and reduce stress.
- Saponins: These compounds have been shown to increase testosterone levels in men, which can boost libido.
- Amino acids: These compounds are essential for the production of hormones, including testosterone and estrogen, which can also affect libido.
Musk Mallow (Hibiscus abelmoschus:
Hibiscus abelmoschus, also known as Abelmoschus moschatus, is a plant that has been used in traditional medicine for centuries. It is said to have aphrodisiac and anti-infertility properties. Hibiscus abelmoschus contains a compound called myricetin, which has antioxidant and cytoprotective properties. Myricetin may help to reduce depression and anxiety, and improve sexual performance and libido in females.
Licorice (Glycyrrhiza glabra):
Licorice has been used traditionally as an aphrodisiac and tonic for memory, voice, and eyes. It contains compounds that act like estrogen and can increase vaginal lubrication, clitoral sensitivity, and overall sexual response in females. Licorice also has mood-boosting and antioxidant effects, which can improve self-esteem and sexual drive.
Spanish Pellitory (Anacyclus pyrethrum):
Anacyclus pyrethrum is a plant that has been used traditionally as a rejuvenator and tonic. It has been shown to improve sexual function in females, and may also help to deal with female gynacological disorders. Anacyclus pyrethrum also has anti-stress, adaptogenic, and immunomodulatory effects.

Read the full article
#boostyourconfidence#enjoyyoursexlifeagain#femalearousalpills#FemVigor#getyourmojoback#liveafulfillinglife#naturallibidoenhancer#overcomesexualdysfunction#reclaimyoursexuality#sexualenhancementforwomen
0 notes
Text
Dr. O’Dowd lecture 8-22-23
Neuroleptic Malignant Syndrome and Serotonin Syndrome
NMS – rapidly progressive neurovegetative state first seen in early clinical trials of haloperidol in 1960
Typical antipsychotics – NMS occurs 0.01-.0%
Atypical antipsychotics – unclear whether atypicals are less likely to cause NMS. Atypical relieve psychotic symptoms with fewer adverse effects compared to typical antipsychotics.
Pathophysiology: Central dopamine hypoactivity. All antipsychotics implicated share DA receptor antagonism. Withdrawal of DA agonists or “freezing” episodes in Parkinson’s disease have induced NMS-like state. DA agonists appear beneficial in treatment.
Pts susceptible to NMS may have a baseline central hypodopaminergia. Pts with basal ganglia disorders are at greater risk for NMS, which supports this theory. So already having low DA levels makes you more susceptible to NMS.
NMS develops over hours to days; change in mental status, catatonia, EPS unresponsive to Parkinson’s tx. Hyperthermia, lead pipe muscle rigidity; delirium and/or catatonia. Pts tachycardia, diaphoretic, labile BP. Labs show high CPK (rhabdomyolysis), leukocytosis, metabolic acidosis. EEG is consistent with delirium and neuroimaging is usually normal. Clozapine has lower incidence of rigidity when it does cause NMS. Aripiprazole-induced NMS may be less likely to cause delirium or hyperthermia. “Atypical NMS” = non-malignant catatonia induced by antipsychotics. Mortality of atypical NMS is 5.5%. Is there really “typical” or “atypical” NMS? It’s not clear, as NMS pts don’t always all present the same.
Treatment: fluids, electrolyte management
Caroff’s criteria:
Treatment with neuroleptics
Hyperthermia
Muscle rigidity
Five of the following: change in mental status, tachycardia, labile BP, diaphoresis, tremor, incontinence, CK elevation, leukocytosis, metabolic acidosis
Exclusion of other causes
Levinson’s criteria is another set of criteria someone made to try to help diagnose NMS; includes major and minor criteria, which help indicate probability of NMS.
Adityanjee’s research criteria are another set of past diagnostic criteria
There used to be a hotline you call to speak to an expert, but most of the time, they would just say it’s probably NMS. The hotline doesn’t exist anymore.
DSM V doesn’t list diagnostic criteria for NMS. Previous criteria had overlap with other syndromes or were too specific. Debate whether autonomic dysfunction are the core criteria.
International consensus study if your score is 74 or greater, it’s considered NMS.
Risk factors: heredity, organic brain disease (especially basal ganglia disorders), low iron levels, substance use (especially GABAergic drug withdrawal), dehydration, agitation, prior history of NMS, history or current episode of catatonia.
Pharmacologic variables: exposure to drugs that block D2 receptors; high potency drugs; high dosage; rapid dose escalation. Unclear whether the risk for NMS is increased with IM drugs.
Depot formulations – longer duration, may last longer, little evidence of increased mortality. Concomitant meds increase risk. Anticholinergics impair temperature regulation. Abrupt cessation of DA agonists (Anti-Parkinson’s meds, buproprion) increases risk of NMS. Abruptly stopping antipsychotics could cause NMS.
Ddx for NMS includes catatonia, delirious mania, agitated delirium, serotonin syndrome, malignant hyperthermia, “benign” EPS, infections, seizures, thyrotoxicosis, fever, heat stroke, pheochromocytoma
NMS vs catatonia: stupor, rigor, autonomic dysfunction occur in both. Not all catatonia from antipsychotics is NMS.
NMS is self-limited once neuroleptics are stopped.
NMS outcomes: 16-25% have renal insufficiency; respiratory failure; cardiac
Tx: stop the neuroleptics; reintroduce DA agonists if they were stopped, hydration, fever control, monitoring, supportive cause
NMS – iatrogenic malignant catatonia. Benzos (IV lorazepam preferred) reduce rigidity and catatonia; high dose (18-24 mg qd often required). Literature suggests dantrolene 1-10 mg/kg/day in divided days may help.
Amantadine, bromocriptine may help as they are dopaminergic. Levodopa can be given.
Definitive treatment for NMS: ECT
But pts usually get better with just supportive care.
Tx guidelines: mild or early NMS = supportive care and benzos; moderate NMS (rigidity and temp 38-40) - high dose benzos, DA agonists; severe NMS – all of the aforementioned and ECT.
Two weeks from recovery, you can do antipsychotic re-challenge. Gradually titrate with los starting dose. Make sure pt is hydrated and has good iron stores.
Serotonin syndrome (SS) – serious complication of tx with SSRIs, TCAs, MAOIs, and other serotonergic meds; usually occurs with 2+ serotonergic meds. Increased central serotonergic activity, hyperstimulation of 5HT1A receptors. Presents as delirium, catatonia, agitated or hypoagitated catatonia, lethargyà coma, tachycardia, diaphoresis, myoclonus, hyperreflexia, rigidity. Hyperreflexia/clonus is unique to SS. Labs in pts with SS: elevated WBC, rhabdo, DIC, metabolic acidosis, renal failure, ARDS
Sternbach’s criteria include agitation, AMS, myoclonus, hyperreflexia, r/o other causes
Revised criteria – major and minor criteria.
Risk factors: 2+ serotonergic drugs; OD on serotonergic drugs; lithium use may be a risk factor
Mechanisms that lead to overstimulation of serotonin: precursors (buspirone, L-dopa, lithium, LSD, L-tryptophan, trazodone); MAOI (decrease SE metabolism like linezolid, phenelzine, tranylcypromine, slegiline); increased SE release (amphetamines, cocaine, MDMA, fenfluramine, reserpine).
Washout period needed for MAOI and SSRI use.
SE syndrome mimics: discontinuation of SE meds, catecholamine excess, anticholinergic toxidrome, infections, EtOH and substance withdrawal, toxic metabolic delirium
SS – rapid onset with self-limited resolution once offending med is stopped. Look for it on any pt on more than 4 psych meds, twitchy pts. Tx: cool the pt, cyproheptadine, benzos may blunt hyperadrenergic component
Cyproheptadine – 1st gen antihistamine with SE antagonist properties; usually not necessary; antagonized 5HT receptors. Chlorpromazine may also be used to tx SS. Dr. O’Dowd favors conservative management.
NMS vs SS:
SS may have quicker onset, SE agents, HTN, tachycardic, hyperthermia, clonus/hyperreflexia
NMS – DA antagonists use, HTN, tachycardia, lead pipe rigidity
1 note
·
View note
Video
youtube
Liked on YouTube: Which Neurotransmitter is the Most Stimulating? (Neurotransmitter Lore) || https://www.youtube.com/watch?v=vMEBliw9lmA || Grab Atlas VPN for just $1.83/mo + 3 months extra before the SUMMER DEAL expires: https://ift.tt/K8hugTX 👈 #ad #atlasvpn This is the neurotransmitter tier list – I hope you find this video to be very stimulating! I guess this is neurotransmitter lore ;) Support the Channel on Patreon - https://ift.tt/RxBCSHL Join the Community Discord! - https://ift.tt/wTYe86A 0:00 Intro 4:53 Ad 6:15 Dopamine 9:30 GPCRs 14:39 Noradrenaline 17:42 Serotonin 21:25 Glutamate 24:55 GABA 27:00 Acetylcholine 29:35 Banana Outro 30:21 Dopamine (again?) *Team* Writer/Producer/Thumbnail Artist - That Chemist (Joey) Lead Animator/Graphic Designer/Editor – David Vesicle Animator - Chogi Lead Writer/Biochem Research - Exergonick (Nicholas) Writer/Biochem Research – Trev Chemistry Assistant - Maurice Technical Lead - Polygorg (Georg) Rigging/3D Systems Engineer - Robot Chicken *Acknowledgements* Ballerene for his ballin' biochem help *Music* - A huge thanks to @S3RL for letting us use his music in the video! "Dopamine - S3RL feat Sara" Contact S3RL - https://ift.tt/9ugsXJU *References* Dopamine: https://ift.tt/8Sxptec, https://ift.tt/Um9vzFN, https://ift.tt/2oSxqdQ, https://ift.tt/iMJUfms Noradrenaline: https://ift.tt/4kSc8Rs Serotonin: https://ift.tt/MGimTvY, https://ift.tt/uIGimMr Tryptophan: https://ift.tt/xqsZ810 Glutamate: https://ift.tt/Tnlavgj Gaba: https://ift.tt/kcgYdVW ACH: https://ift.tt/6y9psI7 Dopamine:Function & Symptoms: https://ift.tt/7hXCwZN Acetylcholine in Learning and Memory: https://ift.tt/OUaMi3S Cholinergic Crisis: https://ift.tt/ojw8mJc Cholinesterase Inhibitors for Alzheimer’s: https://ift.tt/LUqlBD7 Myasthenia Gravis: https://ift.tt/1pdieBb Cholinergic Receptors: https://ift.tt/4BSoIgE Otto Loewi: https://ift.tt/Onedr2f Acetylcholine (ACh: https://ift.tt/iUIqADB GABAergic Dysfunction: https://ift.tt/sKePxbT GABA Receptors: https://ift.tt/9WHziZq The Neurobiology of Addiction: https://ift.tt/whktJdy Mechanism of Action - Benzodiazepine: https://ift.tt/ICy6DbN Anxiety Disorders and GABA Neurotransmission: https://ift.tt/FuE9NJS Gamma-Aminobutyric Acid (GABA): https://ift.tt/nA3tHhr Molecular Mechanisms GABAB: https://ift.tt/uPjTsBb GABA and Glycine Receptors: https://ift.tt/t0EAjZ4 GABA Receptor: https://ift.tt/PNbeou1 NMDA Receptor-Dependent LTP/LTD: https://ift.tt/K1L0paq Glutamate and Depression: https://ift.tt/8J7Kmct Glutamate Transporter 1: Target for the Treatment of Alcohol Dependence: https://ift.tt/ZkbPKI1 Glutamate: What It Is & Function: https://ift.tt/9Ycbt5m Glutamate Receptors: https://ift.tt/OsKJN9R The History of (MSG): https://ift.tt/vJCFVYK Serotonin Syndrome Case Report: https://ift.tt/9tRjkOK Brain Serotonergic Circuitries: https://ift.tt/WR1jmVU Abnormal Cells Constipation: https://ift.tt/K62Wpxo Serotonin: https://ift.tt/iUIqADB Dopamine D1 Receptor: https://ift.tt/1RgANx8 Dopamine in Motivational Control: https://ift.tt/W1Ehted Norepinephrine: https://ift.tt/SkpJREf Adrenergic Neurons and Receptors: https://ift.tt/jzZ7LCx Noradrenergic Synapse: https://ift.tt/4BSoIgE Adrenal Stress Hormones and Enhanced Memory for Emotionally Arousing Experiences: https://ift.tt/ECvPrM2 Dopamine and Noradrenaline in the Brain https://ift.tt/onUx0jJ Noradrenergic Synapse: https://ift.tt/4BSoIgE Dr Julius Axelrod: https://ift.tt/Xfln2rF Adrenal Gland: https://ift.tt/Wgv1YwH Locus Coeruleus-Norepinephrine: https://ift.tt/zpaLqoP Food-Related Reward Signals: https://ift.tt/EUpXG5O Drugs Disrupt Presynaptic Dopamine Neurotransmission: https://ift.tt/t3LHEYC Biochemistry, Dopamine Receptors: https://ift.tt/PZ035Qf Parkinson’s Disease: https://ift.tt/K9ujlFi Signaling Dopamine D1-like Receptor Activation: https://ift.tt/Vyma8Tz Ventral Tegmental Area, in Rat: https://ift.tt/skSUTcN Arvid Carlsson: https://ift.tt/KzLE6p3 Anatomy and Function of VTA : https://ift.tt/B7Fjom3 Dopamine in Motivational Control: https://ift.tt/W1Ehted Relevant human Proteins found in RCSB PDB RCSB.org 10.1093/nar/28.1.235 And predicted proteins found at https://ift.tt/G0JzLMk
0 notes
Text
El yate fajardo

Findings that increased cerebrospinal fluid levels of proNGF mark the onset of MCI and the transition to AD suggests that this proneurotrophin is a potential disease biomarker. In addition to neurotrophin dysfunction, studies indicate alterations in epigenetically regulated proteins occur within cholinotrophic nbM neurons during the progression of AD, suggesting a mechanism that may underlie changes in transcript expression. Despite these degenerative events the cholinotrophic system is capable of cellular resilience and/or plasticity during the prodromal and later stages of the disease. Data indicate a spatiotemporal pattern of degeneration related to the evolution of tau pathology within cholinotrophic neuronal subgroups located within the nucleus basalis of Meynert (nbM). Both transcript and protein data indicate that cholinotrophic neuronal dysfunction is related to an imbalance between TrkA-mediated survival signaling and the NGF precursor (proNGF)/p75NTR-mediated pro-apoptotic signaling, which may be related to alteration in the metabolism of NGF. The current review summarizes the pathobiology of nerve growth factor (NGF) and its cognate receptors during the progression of Alzheimer’s disease (AD). We demonstrate and validate an interrogative quantitative bioinformatic analysis of a key dysregulated neuronal population linking single population transcript changes to an established pathological hallmark associated with cognitive decline for therapeutic development in human DS and AD. The dysregulated transcriptomic profile of trisomic BFCNs provides key information underscoring selective vulnerability within the septohippocampal circuit.Ĭonclusions: We propose both expected and novel therapeutic targets for DS and AD, including specific DEGs within cholinergic, glutamate, GABAergic, and neurotrophin pathways, as well as select targets for repairing oxidative phosphorylation status in neurons. Leveraging Ingenuity Pathway Analysis and KEGG analysis, we linked differentially expressed gene (DEG) changes within MSN BFCNs to several canonical pathways and aberrant physiological functions. Results: Ts65Dn mice had unique MSN BFCNs transcriptomic profiles at ~6 MO clearly differentiating them from 2N mice. We performed high-throughput, single population RNA sequencing (RNA-seq) to interrogate transcriptomic changes within medial septal nucleus (MSN) BFCNs, using laser capture microdissection to individually isolate ~500 choline acetyltransferase-immunopositive neurons in Ts65Dn and normal disomic (2N) mice at 6 months of age (MO). Methods: We utilized Ts65Dn mice to understand mechanisms underlying BFCN degeneration to identify novel targets for therapeutic intervention. The Ts65Dn trisomic mouse model recapitulates both cognitive and morphological deficits of DS and AD, including BFCN degeneration. Current therapeutics have been unsuccessful in slowing disease progression, likely due to complex pathological interactions and dysregulated pathways that are poorly understood. Background: Basal forebrain cholinergic neuron (BFCN) degeneration is a hallmark of Down syndrome (DS) and Alzheimer’s disease (AD).

0 notes
Text
GABA, Schizophrenia, and Iomazenil: A Digestible Overview of a Complicated Study
Schizophrenia is a complex mental health disorder which has been of interest to study for quite some time. The degree of understanding of this disorder has widely increased as more and more research is conducted about its genetic and environmental risk factors for psychiatric development, in addition to how it is expressed both genetically and behaviorally. Within the last two decades, evidence gathered from post-mortem, genetic, and brain-imaging studies has suggested that dysfunction of the GABA (gamma-amino butyric acid) system is involved in the pathophysiology of schizophrenia. This involvement can take form in several mechanistic ways, one in which involves GABA interneurons playing a critical role in synchronizing neural activity and participating in information processing. Sensory perception, as well as several cognitive functions such as memory and emotion, tend to be disrupted in schizophrenia.

GABA’s role in this disruption is that GABAergic interneurons are typically inhibitory, but when this inhibition is disrupted, psychotic symptoms can develop due to a disruption of synchrony of pyramidal cell functions, a loss of associative functions, and eventually a disruption of important gating mechanisms. Another mechanistic way in which GABA is involved in the pathophysiology of schizophrenia is its interaction with the dopamine (DA) system. GABA-A receptors have been found to control the activity of DA neurons in the ventral tegmental area (VTA), in an inhibitory way. Research has also found that inverse GABA-A agonists can activate VTA neurons. Iomazenil is a drug which behaves as an inverse GABA-A agonist–it decreases GABA function. Researchers Kyungheup Ahn, Roberto Gil, John Seibyl, Richard Andrew Sewell, and Deepak Cyril D’Souza were interested in examining how iomazenil may induce psychosis by inducing GABAergic deficits and worsening DA dysregulation. The hypothesis of their study was that if GABA deficits contribute to an increased propensity toward psychosis in schizophrenia, then enhancement of these deficits should exacerbate psychotic symptoms in some schizophrenia patients, but not in healthy normal controls.
The study of Ahn et al. included recruiting both schizophrenia patients and healthy controls (both groups were composed only of males). The subjects underwent testing for a total of two days and were randomly assigned to receive either a placebo or active iomazenil over a 10 minute period, during such testing days. After some baseline assessments were made, behavioral ratings were collected from patients who received iomazenil, both before and after its administration.
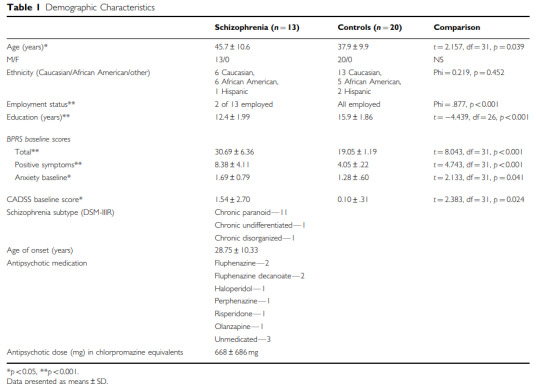
Positive symptoms of schizophrenia were measured using the BPRS (Brief Psychiatric Rating Scale), the CADSS (Clinician Administered Dissociative Symptoms Scale) was used to measure any experienced perceptual alterations, and anxiety of the patients was measured using the BPRS as well. Results of this study found that iomazenil increased positive symptoms of schizophrenia and perceptual alterations in about half of the schizophrenia patients, but not in controls, which is consistent with the GABA-deficit hypothesis of schizophrenia and with the researchers' hypothesis.

While this study has strengths of being a double-blind study, having a placebo-controlled design, and having measures which are well-validated, it also has the following limitations: small sample size, groups not matched for treatment with antipsychotic drugs or for age, and this study did not include women. Additionally, this study presumes that any differential responses to iomazenil reflect a trait rather than a state, but this presumption can only be confirmed with future studying of the effects of iomazenil in various stages of schizophrenia.
So what's the key takeaway in this study? Iomazenil exacerbated psychosis in some schizophrenia patients. This study has relevance in that identifying patients with GABA deficits can be helpful for ensuring proper treatment of these patients with drugs that can enhance GABA function. The findings of this study also open the door for future studies to investigate iomazenil in a larger sample with more proximal measures of GABA function that might be more sensitive in assessing GABA deficits in schizophrenia. All-in-all, this research is very helpful for advancing the neurobiological understanding of schizophrenia and advancing the development of treatment for the disorder as well.
Link to the original paper from which this post was created: https://www.nature.com/articles/npp2010198
All information presented is accredited to the following researchers:
Kyungheup Ahn, Roberto Gil, John Seibyl, Richard Andrew Sewell, and Deepak Cyril D’Souza
0 notes
Text
Interesting Papers for Week 25, 2021
Confidence can be automatically integrated across two visual decisions. Aguilar-Lleyda, D., Konishi, M., Sackur, J., & de Gardelle, V. (2021). Journal of Experimental Psychology. Human Perception and Performance, 47(2), 161–171.
From statistical regularities in multisensory inputs to peripersonal space representation and body ownership: Insights from a neural network model. Bertoni, T., Magosso, E., & Serino, A. (2021). European Journal of Neuroscience, 53(2), 611–636.
On the effect of neuronal spatial subsampling in small‐world networks. Bonzanni, M., Bockley, K. M., & Kaplan, D. L. (2021). European Journal of Neuroscience, 53(2), 485–498.
Multiple cannabinoid signaling cascades powerfully suppress recurrent excitation in the hippocampus. Jensen, K. R., Berthoux, C., Nasrallah, K., & Castillo, P. E. (2021). Proceedings of the National Academy of Sciences of the United States of America, 118(4).
Release probability increases towards distal dendrites boosting high-frequency signal transfer in the rodent hippocampus. Jensen, T. P., Kopach, O., Reynolds, J. P., Savtchenko, L. P., & Rusakov, D. A. (2021). eLife, 10, e62588.
Environment-based object values learned by local network in the striatum tail. Kunimatsu, J., Yamamoto, S., Maeda, K., & Hikosaka, O. (2021). Proceedings of the National Academy of Sciences of the United States of America, 118(4).
Dissecting the Roles of Supervised and Unsupervised Learning in Perceptual Discrimination Judgments. Loewenstein, Y., Raviv, O., & Ahissar, M. (2021). Journal of Neuroscience, 41(4), 757–765.
Molecular mechanisms within the dentate gyrus and the perirhinal cortex interact during discrimination of similar nonspatial memories. Miranda, M., Morici, J. F., Gallo, F., Piromalli Girado, D., Weisstaub, N. V., & Bekinschtein, P. (2021). Hippocampus, 31(2), 140–155.
Human subjects exploit a cognitive map for credit assignment. Moran, R., Dayan, P., & Dolan, R. J. (2021). Proceedings of the National Academy of Sciences of the United States of America, 118(4).
Prioritization in visual attention does not work the way you think it does. Ng, G. J. P., Buetti, S., Patel, T. N., & Lleras, A. (2021). Journal of Experimental Psychology. Human Perception and Performance, 47(2), 252–268.
Linking metacognition and mindreading: Evidence from autism and dual-task investigations. Nicholson, T., Williams, D. M., Lind, S. E., Grainger, C., & Carruthers, P. (2021). Journal of Experimental Psychology. General, 150(2), 206–220.
Neural mechanisms of visual sensitive periods in humans. Röder, B., Kekunnaya, R., & Guerreiro, M. J. S. (2021). Neuroscience & Biobehavioral Reviews, 120, 86–99.
Orientation Effects in the Development of Linear Object Tracking in Early Infancy. Tham, D. S. Y., Rees, A., Bremner, J. G., Slater, A., & Johnson, S. P. (2021). Child Development, 92(1), 324–334.
How do stupendous cannabinoids modulate memory processing via affecting neurotransmitter systems? Vaseghi, S., Nasehi, M., & Zarrindast, M.-R. (2021). Neuroscience & Biobehavioral Reviews, 120, 173–221.
Theta power and theta‐gamma coupling support long‐term spatial memory retrieval. Vivekananda, U., Bush, D., Bisby, J. A., Baxendale, S., Rodionov, R., Diehl, B., … Burgess, N. (2021). Hippocampus, 31(2), 213–220.
Layer 6 ensembles can selectively regulate the behavioral impact and layer-specific representation of sensory deviants. Voigts, J., Deister, C. A., & Moore, C. I. (2020). eLife, 9, e48957.
Using pharmacological manipulations to study the role of dopamine in human reward functioning: A review of studies in healthy adults. Webber, H. E., Lopez-Gamundi, P., Stamatovich, S. N., de Wit, H., & Wardle, M. C. (2021). Neuroscience & Biobehavioral Reviews, 120, 123–158.
Data-driven reduction of dendritic morphologies with preserved dendro-somatic responses. Wybo, W. A., Jordan, J., Ellenberger, B., Marti Mengual, U., Nevian, T., & Senn, W. (2021). eLife, 10, e60936.
Dysfunction of Orbitofrontal GABAergic Interneurons Leads to Impaired Reversal Learning in a Mouse Model of Obsessive-Compulsive Disorder. Yang, Z., Wu, G., Liu, M., Sun, X., Xu, Q., Zhang, C., & Lei, H. (2021). Current Biology, 31(2), 381-393.e4.
Speed modulation of hippocampal theta frequency and amplitude predicts water maze learning. Young, C. K., Ruan, M., & McNaughton, N. (2021). Hippocampus, 31(2), 201–212.
#science#Neuroscience#computational neuroscience#Brain science#research#cognition#cognitive science#neurons#neurobiology#neural networks#psychophysics#neural computation#scientific publications
14 notes
·
View notes
Text
Diversity of the Body’s Neurobiological Stress Response: Racial/Ethnic and Sex Differences
There is an extensive body of literature in the field of neuroscience surrounding the stress response and its connections to poor psychological and physiological health outcomes. It is known that the Hypothalamic-Pituitary-Adrenal (HPA) axis, which is the central stress response, can lead to mood disorders or other possible diseases when it is chronically over-activated due to long term stress. Certain demographics of people, such as racial/ethnic minorities and females, are more susceptible to the negative physiological effects of stress and are disproportionately affected by these disorders. To explain this disparity, recent literature has elucidated the presence of racial/ethnic and sex differences in the neurobiology behind the stress response.
Racial/Ethnic Differences
In a recent review article, existing literature was summarized to show the changes in neurobiology caused by racial discrimination experienced by racial/ethnic minority groups. Racial discrimination has been found to increase allostatic load, which is the body’s to constantly adapt to changes in demands over time, contributing to wear and tear, and leading to higher risk of diseases. This relationship is mediated by chronically elevated levels of the stress hormone cortisol and dysregulated HPA axis in the stress response.
*Please click keep reading to continue*
When an individual perceives acts of racial discrimination, this social stress leads to activation of the HPA axis, the autonomic nervous system and other neurotransmitter pathways, such as dopamine, noradrenaline, and serotonin. As a result, allosteric overload of the body can occur from the over activation of the HPA axis producing excess cortisol and over activation of the autonomic nervous system causing heart rate variability. In addition to causing poor physical health outcomes through the allosteric overload, those three types of neural pathways activated by social stress can also affect functional brain networks. Brain regions such as the prefrontal cortex, anterior cingulate cortex, and salience networks receive the hormonal and neurotransmitter inputs causing hypervigilance and salience network dysfunction that is associated with poor mental health outcomes.
Diving deeper into the functional brain networks affected, neuroimaging has also shown effects of racial discrimination on the anterior cingulate cortex (ACC). The ACC is responsible for integrating social cues and experiences. It is closely involved with emotional reactivity and connected the limbic system. fMRI brain scans have shown that this region is activated by experiences of social exclusion and altered by perceived social stress. These are characteristic of the experiences of racial discrimination. Altered activity of this region as a result of racial discrimination is relevant because a region of the ACC has a high density of glucocorticoid receptors, meaning that increased activation and structural changes of this region during perceived discrimination is indicative of an altered stress pathway.
In these ways, racial discrimination can have neurobiological effects on the stress pathway of the brain. Racial/ethnic minority groups who are more likely to experience situations of discrimination throughout their lives are more susceptible to these chronic stress effects and are more at risk of developing psychiatric mood disorders, as a result.
Sex Differences
There are disparities of biological sex in the prevalence of various psychiatric disorders, which can be explained by the role of stress in the onset and severity of these disorders. For instance, post-traumatic stress disorder and depression occur more frequently in women than men. A recent study revealed underlying sex differences in the neurological response to stress, causing these disparities.
A comparison of stress response by the HPA axis showed that female rats have a greater release of corticotropin releasing factor (CRF) from the hypothalamus, adrenocorticotropic hormone (ACTH) from the pituitary gland and glucocorticoids from the adrenal gland cortex. This can be explained by sex differences in these regions of the brain due to the ovarian hormones of females. For instance, in the adrenals, the female hormone estrogen can enhance ACTH sensitivity and increase glucocorticoid release for this sex. Estrogen can directly regulate vasopressin and CRF gene expression using the promoter region of these genes. The overall implication of this neuroendocrine difference in sexes is that females tend to release more glucocorticoids in response to stress compared to males, which can be more harmful for their health.
Female rats were also found to have reduced negative feedback effect of glucocorticoids due to sex differences in the GABAergic inhibition and glucocorticoid receptor (GR) expression and translocation. In a normal stress response, glucocorticoids provide feedback to limit the activation of the HPA axis by inhibiting hypothalamic release of CRF and pituitary release of ACTH. In this case, the decreased feedback effect is indicated by the fact that it takes longer for glucocorticoid levels to return to baseline for female rats since the hormones in the HPA axis are still being released. One explanation for this sex difference is that estrogen in females reduces GABAergic inhibition in the hypothalamus, thus impairing the feedback. Additionally, estrogen can also downregulate the expression of GR. The normal process of negative feedback requires GRs to be translocated, or moved from the cytosol to the nucleus, in order to repress gene transcription of CRF, CRF receptors, and ACTH precursors. However, this translocation is reduced in female rats as chronic stress exposure upregulates co-chaperone proteins that inhibit the movement of GRs into the nucleus, thus reducing the glucocorticoid negative feedback. As a result, females are more likely to have a dysregulated HPA-axis stress response, making them more susceptible to damaging psychiatric disorders.
Although this study was conducted on rats, its findings can still help draw conclusion about human neuroscience as well. For instance, the resulting increased glucocorticoid levels in female rats can explain the hormonal differences in women with depressions compared to men with depression. It also can help to explain previous literature on why women with psychiatric disorders tend to have greater HPA axis dysregulation than men. In general, these findings provide insights into the neurobiological mechanisms behind the sex disparities of stress-related psychiatric disorders.
References:
Bangasser, D. A. & Valentino, R. J. (2014). Sex differences in stress-related psychiatric disorders: Neurobiological perspectives. Frontiers in Neuroendocrinology, 35, 303-319.
Berger, M. & Sarnyai, Z. (2015). “More than skin deep:” Stress neurobiology and mental health consequences of racial discrimination. Stress, 18(1), 1-10.
2 notes
·
View notes
Photo

Genetics
Secondary to a mutation on the short arm of chromosome 4, in the HTT (aka IT15) gene: a CAG trinucleotide repeat, which encodes for the huntingtin protein.
HD is an autosomal dominant disorder with significant genetic anticipation: the sequence length is unstable and can expand during meiosis, especially down paternal inheritance lines.
It encodes a polyglutamine ('polyQ') stretch at the N-terminus of the huntingtin protein.
The anticipation helps us remember that this is a trinucleotide repeat disorder, specifically a CAG repeat disorder:
Classic trinucleotide repeat expansion disorders
Huntington's disease (CAG), myotonic dystrophy (CTG), and fragile X syndrome CGG) are the three classic trinucleotide repeat expansion disorders: the trinucleotide sequence is repeated many times in a row.
Additional CAG repeat disorders include: Kennedy's disease (aka X-linked spinal and bulbar muscular atrophy), spinocerebellar ataxia type 1 (SCA 1) and type 3 (SCA3, aka Machado-Joseph disease).
Pathology ("CAG" mneomnic)
We use the acronym CAG to highlight some key aspects of HD neuropathology:
On gross examination, there is caudate (C) and putamen (aka striatum) atrophy (A) with resultant anterior horn dilatation.
Accordingly, there is a loss of striatal GABAergic (G) medium spiny neurons, which is what primarily constitutes the striatum.
Mneomnic via Number 4
The HD gene is on chromosome 4
Greater than 40 CAG repeats is abnormal (but, truly, anything more than 36 can be symptomatic)
The average age of onset is 40 years-old but the longer the repeat length, the earlier the age of onset.
Onset younger than 20 years old, is referred to as Juvenile HD; it manifests with an akinetic-rigid syndrome, rather than chorea, referred to as the Westphal variant, which is typically the end-stage of HD in adults.
Clinical
HD is predominantly a neuropsychiatric and movement disorder.
It's often mistaken as alcoholism early on but ultimately becomes parkinsonian, later.
Typical survival from onset is 15 years, much like the timeline of degeneration in Parkinson's disease.
Key domains:
Psychiatric. Depression and anxiety, early, and obsessive/compulsive thoughts, profound apathy, and physical aggression, later. Note that suicide is the 2nd most common cause of death in HD.
Cognitive. Executive dysfunction, early, such as trouble with organizational tasks, planning, and task sequencing.
Simple abnormal involuntary movements: tics, dystonia, myoclonus.
Complex abnormal involuntary movements: Chorea (excessive movements that flow from body part to body part).
Failure of voluntary movements: Akinetic, rigid syndrome (parkinsonism).
#ditki#pathology#chorea#huntington's disease#huntingtondisease#medstudyblr#medstudy#medicalstudent#medicalschool
12 notes
·
View notes
Text
Anticonvulsants for Neuropathic Pain Market Product Type, Applications/end user, Key Players and Geographical Regions 2025
Global Anticonvulsants for Neuropathic Pain Market: Snapshot
Neuropathic pain, which refers to kind of chronic pain resulting from an injury to or disease of the central or peripheral nervous system, remains a therapeutic challenge to clinicians as it does not respond well to conventional pain therapies. Although the clinical knowledge regarding the pathogenesis of the condition has significantly increased over the past few decades, the actual mode of action of most popular treatment mechanisms and the pathogenesis of neuropathic pain remain somewhat unclear.
Owing to the several similarities between the pathophysiological symptoms observed in neuropathic pain models and in some epilepsy models, anticonvulsants are finding increased usage in the symptomatic management of neuropathic pain conditions. Carbamazepine, the world’s first anticonvulsant examined in clinical trials, continues to remain one of the key choices of healthcare practitioners for neuropathic pain conditions. Apart from carbamazepine, a number of new anticonvulsants in the anticonvulsants for neuropathic pain market or in high quality clinical trial represent a new era in the treatment of neuropathic pain.
Get Brochure of the Report @ https://www.tmrresearch.com/sample/sample?flag=B&rep_id=32
The overall role of anticonvulsants in the treatment of neuropathic pain continues to evolve. Further advances in the overall understanding of the mechanisms of neuropathic pain conditions and well-designed clinical trials are expected to further improve the opportunities to make anticonvulsants an established course of action in the treatment of neuropathic pain. This report examines the current state of development of the global anticonvulsants for neuropathic pain market, with applications in the treatment of neuropathic pain at the center of focus. Recent developments and future scope of development of the anticonvulsants for neuropathic pain market are also analyzed.
Global Anticonvulsants for Neuropathic Pain Market: Overview
Neurapthic pain (NP) is a severe pain associated with a number of diseases such as cancer, diabetes, and herpes zoster. This pain affects almost 1% of the world’s total population and is aggravated as a result of dysfunction, lesion, or transitory perturbation in the peripheral and central nervous system. Some other causes of neuropathic pain include trigeminal neuralgia, peripheral and entrapment neuropathy, brachial plexus avulsion pain, spinal cord injury pain, post-herpetic neuralgia, arachnoiditis, phantom limb pain, and post-stroke pain.
The report presents a definitive analysis of market drivers, market restraints, and trends that will impact progression of the global anticonvulsants for neuropathic pain market until the end of 2025. The report charts the developmental growth map in the future by analyzing the past performance of the market.
Buy this Report @ https://www.tmrresearch.com/checkout?rep_id=32<ype=S
The research report analyzes the global anticonvulsants for neuropathic pain market from a competitive viewpoint as well. The report finds out how innovations and product development will present growth opportunities to market players to serve niche patient areas. The analysis of changing competitive hierarchy is presented through graphs and pictorial representations. The report is compiled after collecting data from industry-centric databases and scrutinized using validated analytical tools.
Global Anticonvulsants for Neuropathic Pain Market: Drivers and Restraints
The increasing incidence of people with neuropathic pain is one of the major factors driving the anticonvulsants for neuropathic pain market. In addition, a high number of patients refractory to alternate treatment methods, increasing use of generic drugs compared to branded drugs, and a high rate of polypharmacy are some other factors driving the growth of this market.
The development of novel drug molecules for neuropathic drug indications is also propelling the growth of this market. This is because less than 50% of the patients respond to existing drugs that are available for neuropathic drug indications. Moreover, these drugs are associated with a number of side effects, particularly when administered systemically. Hence, new drug variants that can provide convincing action mechanism will be a game changer in the global anticonvulsants for neuropathic pain market.
Some of the newer anticonvulsant drugs for neuropathic pain include Depomed’s Gralise (gabapentin gastric-retention), which is available since 2011 and is a ‘once –daily’ formulation. XenoPort’s Horizant (gabapentin encarbil) was introduced in 2012 and is a “twice-daily’ formulation.
Global Anticonvulsants for Neuropathic Pain Market: Advantages of Anticonvulsants
Neuropathic pain can be managed by opioids such as morphine, non-steroidal anti-inflammatory drugs, and anticonvulsant drugs. Anticonvulsants are normally used to control epileptic seizures but may also be used for treating neuropathic pain conditions such as fibromyalgia and postherpetic neuralgia. Anticonvulsants impede seizures through multiple mechanisms such as:
Functional obstruction of voltage-gated-calcium channels
Impediment of glutamergic neurotransmission
Functional obstruction of voltage-sodium channels
Direct or indirect enhancement of hindering GABAergic neurotransmission
Companies Mentioned in report
The report provides a detailed vendor landscape of the global anticonvulsants for neuropathic pain market with a business profile of major companies that operate in this market. These are Teva Pharmaceuticals, Depomed Inc., Janssen Pharmaceutical Inc., Cephalon Inc., GlaxoSmithKline plc, Novartis AG, Pfizer Inc., AbbVie Inc., and XenoPort Inc.
Get Table of Content of the Report @ https://www.tmrresearch.com/sample/sample?flag=T&rep_id=32
About TMR Research:
TMR Research is a premier provider of customized market research and consulting services to business entities keen on succeeding in today’s supercharged economic climate. Armed with an experienced, dedicated, and dynamic team of analysts, we are redefining the way our clients’ conduct business by providing them with authoritative and trusted research studies in tune with the latest methodologies and market trends.
#Anticonvulsants for Neuropathic Pain Market#Key Players#Neuropathic pain#clinical trial#GlaxoSmithKline plc Novartis AG#healthcare
0 notes
Text
New Treatment Could Address Memory-Related Side Effects Of <b>Neurological</b> Disorders
It is increasingly likely that the cellular receptors that bind to GABA become depleted or dysfunctional in various neurological conditions. As GABAergic ...
from Google Alert - neurological http://bit.ly/2SSE79u
0 notes
Text
Ginsenoside Rb1 may serve as a potential candidate for the treatment of Parkinson's disease.
PMID: Aging (Albany NY). 2019 Jul 17 ;11(14):5008-5034. PMID: 31314744 Abstract Title: Ginsenoside Rb1 regulates prefrontal cortical GABAergic transmission in MPTP-treated mice. Abstract: Parkinson's disease (PD) is a common neurodegenerative disease, featured by motor deficits and non-motor symptoms such as cognitive impairment, and malfunction of gamma-aminobutyric acid (GABA) mediated inhibitory transmission plays an important role in PD pathogenesis. The ginsenoside Rb1 molecule, a major constituent of the extract from the Ginseng root, has been demonstrated to ameliorate motor deficits and prevent dopaminergic neuron death in PD. However, whether Rb1 can regulate GABAergic transmission in PD-associated deficits and its underlying mechanisms are still unclear. In this study, we explored the effects of Rb1 on the GABAergic synaptic transmission in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP) mouse model of PD. We demonstrated that Rb1 can bind with GABARα1 and increase its expression in the SH-SY5Y cells and in the prefrontal cortex (PFC) of MPTP modeland. Furthermore, Rb1 can promote prefrontal cortical GABA level and GABAergic transmission in MPTP-treated mice. We also revealed that Rb1 may suppress presynaptic GABAR1 to enhance GABA release and GABAreceptor-mediated inhibitory transmission. In addition, Rb1 attenuated MPTP-induced dysfunctional gait dynamic and cognitive impairment, and this neuroprotective mechanism possibly involved regulating prefrontal cortical GABAergic transmission. Thus, Rb1 may serve as a potential drug candidate for the treatment of PD.
read more
0 notes
Text
Depression-Let's Talk-Juniper Publishers
Authored by Jyoti Priyadarshini,
Opinion
Mental health is defined as a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community. The positive dimension of mental health is stressed in WHO's definition of health Health is a state of complete physical, mental and social well-being and not merely the absence of disease or infirmity» [1]. The theme for this year's World Health Day campaign is Depression. The slogan is: Depression: Let's talk [2].
Depression is a common mental disorder, characterized by sadness, loss of interest or pleasure, feelings of guilt or low selfworth, disturbed sleep or appetite, feelings of tiredness, and poor concentration for at least two weeks [3,4].
Target Population
Depression can affect anyone whatever your age, sex, or social status. World Health Organization is paying particular attention to three groups that are disproportionally affected: adolescents and young adults, women of childbearing age (particularly following childbirth), and older adults (over 60s)[4].
Depression is a significant contributor to the globalburden of disease and affects people in all communities to affect 350 million people. The World Mental Health Survey conducted in 17 countries found that on average about 1 in 20 people reported having an episode of depression in the previous year. Depressivedisorders often start at a young age; they reducepeople's functioning and often are recurring. Forthese reasons, depression is the leading cause of disabilityworldwide in terms of total years lost due todisability. The demand for curbing depression andother mental health conditions is on the rise globally [5].
Epidemiology
Depression is one of the most common mental health problems. It is estimated that 16 to 20 out of 100 people will have depression or a chronic low mood (dysthymia) at least once in their lives. Women are affected more than men, and it is more common in older people [6]. About a quarter of medical students have depressive symptoms [7,8].
Types of Depression
There are different types of depression, with different levels of severity. Some only arise under certain circumstances, for example after giving birth.Doctors differentiate between the following types of depression based on the symptoms and possible causes:
Unipolar Depression.
Dysthymia.
Seasonal Affective Disorder
Postntal Depression.
Bipolar Depression [9].
Pathophysiology
Depression results from a complex interaction of social, psychological and biological factors. Depression can, in turn, lead to more stress and dysfunction and worsen the affected person's life situation and depression itself [10]. Depression is an interplay of imbalance between various chemicals like Stress hormones, Cytokines, Monoamines, Altered Glutamatergic and Gabaergic Neurotransmission ,Circadian Rhythm etc [11,12]. There is clinical and etiological heterogeneity of major depressive disorder, so it is difficult to elucidate its pathophysiology. Current neurobiological theories with the most valid empirical foundation and the highest clinical relevance are reviewed with respect to their strengths and weaknesses. The selected theories are based on studies investigating psychosocial stress and stress hormones, neurotransmitters such as serotonin, norepinephrine, dopamine, glutamate and gamma-aminobutyric acid (GABA), neurocircuitry, neurotrophic factors, and circadian rhythms. Because all theories of depression apply to only some types of depressed patients but not others, and because depressive pathophysiology may vary considerably across the course of illness, the current extant knowledge argues against a unified hypothesis of depression suggesting that depression is a clinically and etiologically heterogeneous disorder .Multimodality approach with antidepressants, including psychological and biological approaches, should be tailored for individual patients and disease states [13].
Symptoms
Physical symptoms are common in depression, and, in fact, vague aches and pain are often the presenting symptoms of depression. These symptoms include chronic joint pain, limb pain, back pain, gastrointestinal problems, tiredness, sleep disturbances, psychomotor activity changes, and appetite changes. A high percentage of patients with depression who seek treatment in a primary care setting report only physical symptoms, which can make depression very difficult to diagnose. Physical pain and depression have a deeper biological connection than simple cause and effect; the neurotransmitters that influence both pain and mood are serotonin and norepinephrine. Dysregulation of these transmitters is linked to both depression and pain [14].
While depression is the leading cause of disability for both males and females, the burden of depressionis 50% higher for females than males (WHO 2008). In fact, depression is the leading cause of disease burden for women in both high-income andlow- and middle-income countries (WHO, 2008). Research in developing countries suggests thatmaternal depression may be a risk factor for poor growth in young children Rahman [15]. Depression is the leading cause of disease-related disability in women. Epidemiological studies have shown that the lifetime prevalence of a major depressive disorder in women (21.3%) is almost twice that in men (12.7%). This ratio has been documented in different countries and ethnic groups. Sex differences relating to depression vary with age, with male and female children showing similar incidence rates. National comorbidity data reveal that sex differences in prevalence first appear around the age of 10 years and persist until midlife, after which they disappear [16]. Improved methods of assessment and research design have established a robust and causal association between stressful life events and major depressive episodes [17].
WHO Response
Depression is one of the priority conditions covered by WHO's Mental Health Gap Action Programme (mhGAP). The Programme aims to help countries increase services for people with mental, neurological and substance use disorders, through care provided by health workers who are not specialists in mental health. The Programme asserts that with proper care, psychosocial assistance and medication, tens of millions of people with mental disorders, including depression, could begin to lead normal lives - even where resources are scarce [18,19].
Depression is all prevailing, omnipresent associated with social stigma, yet it is treatable. It is an invisible illness with roots in the childhood .On an individual, community, and national level, it is time to educate ourselves and talk about depression and support those whoare suffering from this mental disorder.
For more articles in Journal of Nursing & Health Care please click on https://juniperpublishers.com/jojnhc/index.php
For more Journals in Juniper Publishers please click on https://juniperpublishers.com/journals.php
#Juniper Publishers#Open Access Journlas#journal of nursing#Health Care Journals#journal of public health
0 notes
Text
Anticonvulsants for Neuropathic Pain Market Current Outlook Of Industry & Forecast 2017-2025
Global Anticonvulsants for Neuropathic Pain Market: Snapshot
Neuropathic pain, which refers to kind of chronic pain resulting from an injury to or disease of the central or peripheral nervous system, remains a therapeutic challenge to clinicians as it does not respond well to conventional pain therapies. Although the clinical knowledge regarding the pathogenesis of the condition has significantly increased over the past few decades, the actual mode of action of most popular treatment mechanisms and the pathogenesis of neuropathic pain remain somewhat unclear.
Get Sample Copy of the Report @ https://www.tmrresearch.com/sample/sample?flag=B&rep_id=32
Owing to the several similarities between the pathophysiological symptoms observed in neuropathic pain models and in some epilepsy models, anticonvulsants are finding increased usage in the symptomatic management of neuropathic pain conditions. Carbamazepine, the world’s first anticonvulsant examined in clinical trials, continues to remain one of the key choices of healthcare practitioners for neuropathic pain conditions. Apart from carbamazepine, a number of new anticonvulsants in the anticonvulsants for neuropathic pain market or in high quality clinical trials represent a new era in the treatment of neuropathic pain.
The overall role of anticonvulsants in the treatment of neuropathic pain continues to evolve. Further advances in the overall understanding of the mechanisms of neuropathic pain conditions and well-designed clinical trials are expected to further improve the opportunities to make anticonvulsants an established course of action in the treatment of neuropathic pain. This report examines the current state of development of the global anticonvulsants for neuropathic pain market, with applications in the treatment of neuropathic pain at the center of focus. Recent developments and future scope of development of the anticonvulsants for neuropathic pain market are also analyzed.
Request TOC of the Report @ https://www.tmrresearch.com/sample/sample?flag=T&rep_id=32
Global Anticonvulsants for Neuropathic Pain Market: Overview
Neurapthic pain (NP) is a severe pain associated with a number of diseases such as cancer, diabetes, and herpes zoster. This pain affects almost 1% of the world’s total population and is aggravated as a result of dysfunction, lesion, or transitory perturbation in the peripheral and central nervous system. Some other causes of neuropathic pain include trigeminal neuralgia, peripheral and entrapment neuropathy, brachial plexus avulsion pain, spinal cord injury pain, post-herpetic neuralgia, arachnoiditis, phantom limb pain, and post-stroke pain.
The report presents a definitive analysis of market drivers, market restraints, and trends that will impact progression of the global anticonvulsants for neuropathic pain market until the end of 2025. The report charts the developmental growth map in the future by analyzing the past performance of the market.
The research report analyzes the global anticonvulsants for neuropathic pain market from a competitive viewpoint as well. The report finds out how innovations and product development will present growth opportunities to market players to serve niche patient areas. The analysis of changing competitive hierarchy is presented through graphs and pictorial representations. The report is compiled after collecting data from industry-centric databases and scrutinized using validated analytical tools.
Global Anticonvulsants for Neuropathic Pain Market: Drivers and Restraints
The increasing incidence of people with neuropathic pain is one of the major factors driving the anticonvulsants for neuropathic pain market. In addition, a high number of patients refractory to alternate treatment methods, increasing use of generic drugs compared to branded drugs, and a high rate of polypharmacy are some other factors driving the growth of this market.
The development of novel drug molecules for neuropathic drug indications is also propelling the growth of this market. This is because less than 50% of the patients respond to existing drugs that are available for neuropathic drug indications. Moreover, these drugs are associated with a number of side effects, particularly when administered systemically. Hence, new drug variants that can provide convincing action mechanism will be a game changer in the global anticonvulsants for neuropathic pain market.
Some of the newer anticonvulsant drugs for neuropathic pain include Depomed’s Gralise (gabapentin gastric-retention), which is available since 2011 and is a ‘once –daily’ formulation. XenoPort’s Horizant (gabapentin encarbil) was introduced in 2012 and is a “twice-daily’ formulation.
Global Anticonvulsants for Neuropathic Pain Market: Advantages of Anticonvulsants
Neuropathic pain can be managed by opioids such as morphine, non-steroidal anti-inflammatory drugs, and anticonvulsant drugs. Anticonvulsants are normally used to control epileptic seizures but may also be used for treating neuropathic pain conditions such as fibromyalgia and postherpetic neuralgia. Anticonvulsants impede seizures through multiple mechanisms such as:
Functional obstruction of voltage-gated-calcium channels
Impediment of glutamergic neurotransmission
Functional obstruction of voltage-sodium channels
Direct or indirect enhancement of hindering GABAergic neurotransmission
Companies Mentioned in report
The report provides a detailed vendor landscape of the global anticonvulsants for neuropathic pain market with a business profile of major companies that operate in this market. These are Teva Pharmaceuticals, Depomed Inc., Janssen Pharmaceutical Inc., Cephalon Inc., GlaxoSmithKline plc, Novartis AG, Pfizer Inc., AbbVie Inc., and XenoPort Inc.
Read Comprehensive Overview of Report @ https://www.tmrresearch.com/anticonvulsants-for-neuropathic-pain-market
About TMR Research
TMR Research is a premier provider of customized market research and consulting services to business entities keen on succeeding in today’s supercharged economic climate. Armed with an experienced, dedicated, and dynamic team of analysts, we are redefining the way our clients’ conduct business by providing them with authoritative and trusted research studies in tune with the latest methodologies and market trends.
Contact:
TMR Research,
3739 Balboa St # 1097,
San Francisco, CA 94121
United States
Tel: +1–415–520–1050
0 notes
Text
Interesting Reviews for Week 26, 2019
Unsupervised excitation: GABAergic dysfunctions in Alzheimer’s disease. Ambrad Giovannetti, E., & Fuhrmann, M. (2019). Brain Research, 1707, 216–226.
Activity-dependent development of GABAergic synapses. Oh, W. C., & Smith, K. R. (2019). Brain Research, 1707, 18–26.
Dopamine and Cognitive Control in Prefrontal Cortex. Ott, T., & Nieder, A. (2019). Trends in Cognitive Sciences, 23(3), 213–234.
Deep learning in spiking neural networks. Tavanaei, A., Ghodrati, M., Kheradpisheh, S. R., Masquelier, T., & Maida, A. (2019). Neural Networks, 111, 47–63.
Theories of Error Back-Propagation in the Brain. Whittington, J. C. R., & Bogacz, R. (2019). Trends in Cognitive Sciences, 23(3), 235–250.
#science#Neuroscience#computational neuroscience#Brain science#research#reviews#scientific publications
4 notes
·
View notes
Text
Baicalin vs Baicalein – What’s the Difference? – LiftMode
Chinese Skullcap is a Traditional Chinese Medicine with a centuries-long history of use. [1] Recently, it has gained interest in the West due to its powerful relaxation and health-promoting properties.
The key active compound in Skullcap is Baicalin, which is metabolized in your stomach into Baicalein.[2] This compound acts as a mild GABA-agonist and reduces signals from the central nervous system to assist with stress and calm.[3] It is also a powerful antioxidant and anti-inflammatory with several secondary health benefits.
Here, we discuss the difference between Baicalin and Baicalein to help you decide which is best!
Baicalin vs Baicalein Benefits
Reduces stress and promotes relaxation
First and foremost, the most important benefit of both Baicalin and Baicalein is their remarkable ability to reduce stress and to promote relaxation.[4]
Both of these compounds bind to GABA receptors in your brain to reduce signals from the central nervous system – in a similar way to many other anti-stress compounds that are available over the counter or by prescription.[5]
Most people who use Baicalin or Baicalein do so because they’re looking for a natural alternative to commercially available stress-relief or sleep aid compounds.
The best thing about Baicalin and Baicalein is that, although they are highly effective in their benefits, their side effects and potential for abuse are way lower than for almost any other stress-reducing compound!
Check Out Our Range of Skullcap Extracts
Health-Promoting Benefits
Apart from their stress-reducing and relaxation-promoting benefits, Baicalin and Baicalein have a number of benefits for health, vitality, and well-being.
When you take a Baicalin or Baicalein supplement, you will definitely notice that they produce the same benefits, overall. These benefits include:
★ Neuroprotection – protects nerve cells from stress and toxins.[6]
★ Learning capacity – may improve the ability to focus and learn.[7]
★ Protects the heart – supports a healthy circulatory system and supports healthy blood sugar levels.[8] [9]
★ Helps to reduce inflammation – both compounds are powerful anti-inflammatories [10]
★ Antioxidant – destroys dangerous ‘free-radical’ chemicals in the body [11]
For a full description of these benefits, check out our Top Baicalin Benefits blog post.
Chemical Differences
Both compounds are flavones – a class of chemicals found in foods, and often with active effects in the human body.[12] Both are extracted from Scutellaria baicalensis plant – a herb with many uses in Traditional Chinese Medicine (TCM).
Baicalin and Baicalein are chemically very similar – Baicalin is a flavone glycoside with an added chemical group (the glucuronide version of Baicalein).[13] When taken as a supplement or plant extract, Baicalin is broken down into Baicalein in your stomach.
Many people claim that Baicalein’s effects are stronger and more pronounced than those of Baicalin.
These claims are not without their merit – Baicalein offers a more readily available version of the compound (it doesn’t need to be metabolized in your gut to become active).
The drawback is that the production process to obtain pure Baicalein is more difficult than extracting Baicalin, so the former is a little heavier on the wallet.
Another difference between the two is that Baicalein is soluble in lipids (fats) while Baicalin is mildly soluble in water.[14]
The image below shows the structural differences between these two compounds.
Differences in Effects – Baicalin vs Baicalein
As we mentioned before, both of these compounds create the same effects on the human body. However, Baicalein is said to have better bioavailability than Baicalin, and its effects are often said to be more pronounced (although this hasn’t been proven in clinical studies).
Here’s what people are saying about Baicalin (reviews of LiftMode products):
★ “I take this product 2 times a day on my work days, I feel like it smooths out my coffee jitters and keeps the stress from working in customer service from even manifesting; Highly recommend it and its cheap.” – David.
★ “I find that Baicalin is a very good option for when cycling off of stronger gabaergics. There is research available about its effects as a positive allosteric modulator on Gaba A receptors. I find it to be helpful toward anxiety in a mild kind of way. In my opinion, it is worth having a jar around.”- Dustin.
★ “I purchased this as something to use when I was cycling off of Phenibut FAA and was not disappointed. It’s not the same but it’s very close in its ability to offer a calm relaxed mind set. Also is like half the price of FAA and so far doesn’t seem to have any of the negative side effects.” – Zachary
★ “I discerned a clear perceptibly elevated mood, perhaps owing to the GABA-A action. It was certainly not what I’d call stimulating, but it’s possible that the mild disinhibiting effects lend themselves to greater energy expenditure. Because it is mild in its effect, in my experience, I find it to be a useful adjunct to caffeine as part of a pre-workout supplement regimen.” – Brendon
Check Out Our Range of Skullcap Extracts
Here’s what people are saying about Baicalein (reviews of LiftMode products):
★ “Baicalin was an old favourite of mine, though I haven’t had it in a few years. I saw this, read its description and decided to give it a shot. This stuff is STRONG. Be careful with it. The serving size was 300mg but that resulted in too much difficulty waking up the next morning. A lighter dose, anywhere from 150-225mg, is far more useful to me, especially when taking it during the day. The very first time I took it, I recall thinking as it set in that, wow… “this appears to be nature’s [removed]. Great stuff, will order again without question.” – James.
★ “This product is definitely stronger than baicalin. I’ve used both sublingually and baicalein is stronger mg for mg. I find it gives a relaxing effect as well as some mild pain relief. The only drawback for myself is that it sometimes gives me headaches.” – Djones.
Recommended Usage
The recommended serving sizes for these products differ.
For Baicalein, the serving size is 250 – 300 mg taken up to three times per day.
For Baicalin, the serving size is 200 – 400 mg, taken up to three times per day.
For both products, it is recommended to use a measuring scale with a 10 mg (0.01 gram) accuracy or greater for reliable measurements. Both supplements can be taken in a capsule form by purchasing Pullulan capsules.
Do not exceed the recommended serving size for either of these products! Although side effects are rare and generally mild, larger serving sizes increase your chances of experiencing negative effects. For a list of potential side effects, check out our Baicalin side effects post.
Medical Disclaimer
Not intended to treat, diagnose, or cure any disease or ailment. Please read and fully understand the potential adverse effects before using this product. These statements have not been reviewed by the FDA and are not written by a medical professional. Please consult your doctor before using any supplements, especially if you have any medical conditions.
Tristan
B.Sc. in Molecular Biology and Biochemistry Researched & written by Tristan and verified by the Liftmode.com Research Team
Supporting Citations
[1] Zhao, Q., Chen, X. Y., & Martin, C. (2016). Scutellaria baicalensis, the golden herb from the garden of Chinese medicinal plants. Science bulletin, 61(18), 1391–1398. doi:10.1007/s11434-016-1136-5
[2] Chen, H., Gao, Y., Wu, J., Chen, Y., Chen, B., Hu, J., & Zhou, J. (2014). Exploring therapeutic potentials of baicalin and its aglycone baicalein for hematological malignancies. Cancer letters, 354(1), 5–11. doi:10.1016/j.canlet.2014.08.003
[3] Wang, F., Xu, Z., Ren, L., Tsang, S. Y., & Xue, H. (2008). GABAA receptor subtype selectivity underlying selective anxiolytic effect of baicalin. Neuropharmacology, 55(7), 1231–1237. doi:10.1016/j.neuropharm.2008.07.040
[4] Xu, Z., Wang, F., Tsang, S., Ho, K., Zheng, H., Yuen, C., … Xue, H. (2006). Anxiolytic-Like Effect of Baicalin and its Additivity with other Anxiolytics. Planta Medica, 72(02), 189–192. doi:10.1055/s-2005-873193
[5] Awad, R., Arnason, J. T., Trudeau, V., Bergeron, C., Budzinski, J. W., Foster, B. C., & Merali, Z. (2003). Phytochemical and biological analysis of Skullcap (Scutellaria lateriflora L.): A medicinal plant with anxiolytic properties. Phytomedicine, 10(8), 640–649. doi:10.1078/0944-7113-00374
[6] Sowndhararajan, K., Deepa, P., Kim, M., Park, S. J., & Kim, S. (2018). Neuroprotective and Cognitive Enhancement Potentials of Baicalin: A Review. Brain sciences, 8(6), 104. doi:10.3390/brainsci8060104
[7] Duan, D., Wang, K., Zhou, Y., Qin, X., Gao, L., & Du, G. (2017). Baicalein Exerts Beneficial Effects in d-Galactose-Induced Aging Rats Through Attenuation of Inflammation and Metabolic Dysfunction. Rejuvenation Research, 20(6), 506–516. doi:10.1089/rej.2017.1919
[8] Ku, S. K., & Bae, J. S. (2015). Baicalin, baicalein and wogonin inhibits high glucose-induced vascular inflammation in vitro and in vivo. BMB reports, 48(9), 519–524. doi:10.5483/BMBRep.2015.48.9.017
[9] Fu, Y., Luo, J., Jia, Z., Zhen, W., Zhou, K., Gilbert, E., & Liu, D. (2014). Baicalein Protects against Type 2 Diabetes via Promoting Islet β-Cell Function in Obese Diabetic Mice. International journal of endocrinology, 2014, 846742. doi:10.1155/2014/846742
[10] Hang, Y., Qin, X., Ren, T., & Cao, J. (2018). Baicalin reduces blood lipids and inflammation in patients with coronary artery disease and rheumatoid arthritis: a randomized, double-blind, placebo-controlled trial. Lipids in Health and Disease, 17(1). doi:10.1186/s12944-018-0797-2
[11] Shieh, D. E., Liu, L. T., Lin, C. C. (2000). Antioxidant and free radical scavenging effects of baicalein, baicalin and wogonin. Anticancer Res, 20(5A):2861-5. PubMed PMID: 11062694.
[12] Ming, J., Zhuoneng, L., & Guangxun, Z. (2018). Protective role of flavonoid baicalin from Scutellaria baicalensis in periodontal disease pathogenesis: A literature review. Complementary Therapies in Medicine, 38, 11–18. doi:10.1016/j.ctim.2018.03.010
[13] Akao, T., Kawabata, K., Yanagisawa, E., Ishihara, K., Mizuhara, Y., Wakui, Y., Sakashita, Y., Kobashi, K. (2000). Baicalin, the predominant flavone glucuronide of scutellariae radix, is absorbed from the rat gastrointestinal tract as the aglycone and restored to its original form. J Pharm Pharmacol. 52(12):1563-8. PubMed PMID: 11197087.
[14] Chen, H., Gao, Y., Wu, J., Chen, Y., Chen, B., Hu, J., & Zhou, J. (2014). Exploring therapeutic potentials of baicalin and its aglycone baicalein for hematological malignancies. Cancer letters, 354(1), 5–11. doi:10.1016/j.canlet.2014.08.003
The post Baicalin vs Baicalein – What’s the Difference? – LiftMode appeared first on LiftMode Blog.
Baicalin vs Baicalein – What’s the Difference? – LiftMode published first on https://liftmode.wordpress.com/
0 notes