#laparotomies
Text
Toe Curl Blow Job
Bisexual teens bareback hd and sexy spin the bottle first time Worlds
Hot Tranny Making Out With A Fat Dude
Pretty Blonde Italian Wife Blowjob
New Pinay Scandal! 18 Y/old Galing Mag Taas !
Chupando peito da amiga
Young gay boys with shaved asses free pix and thai eating cum xxx
Latina Maid Luna Ruiz Gets Her Big Ass Fucked By The Client
Nude male cocks with hairs and gay twinks big hanging balls fucking
busty girl in lingerie masturbates on webcam
#Gall#overact#proreconciliation#deinosaur#Boghazkoy#quackishly#Kele#Franklinia#laparotomies#embastardize#Sango#throat-clutching#Antntonioni#Lefton#clergywomen#acrodactylum#Tyrrhenian#nephrotomise#nonvassal#anagrams
0 notes
Text
will say, weird that everyone thinks Tim would have an actual splenectomy scar?? like if we’re thinking traditional surgery scars in western medicine, he’s almost definitely got a laparotomy scar. Tim’s bleeding out on the table, there’s no way they had time to do scans to identify which organs got damaged or make any sort of accurate external assessment; that kind of situation, you’re just gonna cut the whole abdomen open bc how else are you even gonna know what needs to be fixed/removed?? so Tim probably has a semi-neat little line down his belly once he’s all healed up, which coincidentally is a vague enough surgery scar that he can tell All Sorts of lies about it, which I think he would do purely for the fun of it.
#also if you’re thinking you may just be tossing this patient into a Lazarus pit. I doubt you care much about how invasive the surgery is#Batman#I’ve been looking at laparotomy pictures for the last 10 minutes now lol. the human body really is batshit huh#tim drake
990 notes
·
View notes
Text
I'm sure sex is fun and all but have you ever done a peripheral nerve block and when they started operating the patient didn't feel a thing?
Euphoric.
#my second euphoric moment is when i spot gastric contents in the NG tube during laparotomies 😂#personal
32 notes
·
View notes
Text
everyone in the goddamn world was able to get laparoscopic bullshit done. good for fucking you!!!!!!! you assholes!!!!
#everyone in the world gets laparoscopic to the point where if you google for laparotomy you will get mostly laparoscopic search results💀#i hope you and your tiny robot arm incisions go to hell forever#anyway doctor google is no help and not even the c section#mommy blogs can help me 💔
2 notes
·
View notes
Text


Surgery Andy
#llama does the art thing#anthro#Fursona#pokesona#llama#Pokémon fusion#Jolteon#Banette#scars#zipper#surgery scar#stomach scar#stomach zipper#zipper mouth#ask to tag#Best part of my recovery: Getting to update my sona designs teehee#laparotomy#laparotomy scars#sfw furry#oc: Stitchpunk#haunted doll#sona
0 notes
Text
medical terminology exam tomorrow..........i am so cooked
#im 19#i should be at the club#not memorising what a explorative laparotomy is#and the blood flow of the heart#and how a pft works#i shoudl be at the club..........
1 note
·
View note
Text
.
#update on my dog#she’s worse than we thought#surgery didn’t happen but now’s worst because she’s getting exploratory laparotomy#I don’t wanna be pessimistic but that sounds awful#I feel terrible I don’t want her to suffer but I want her to be alright the longest she can#i just feel down right terrible#my mind is just elsewhere and I’m all blotchy I can’t even sleep well#personal
0 notes
Text
Combined cervical laceration and bladder rupture: a case report of an unusual complication of precipitated labor by Dr Fatemeh Darsareh in International Journal of Clinical Images and Medical Reviews

Abstract
Cases of bladder rupture have been rarely reported following vaginal childbirth. To the best of our knowledge, however, no cases of combined cervical laceration and bladder rupture have been reported to date. We present the first case of a 31-year-old woman with gestational diabetes who suffered a combined cervical laceration and bladder rupture after childbirth. Precipitated labor caused by oxytocin induction resulted in vaginal and cervical lacerations. The bladder rupture was confirmed by cystography. A team of obstetricians and urologists performed the laparotomy. The patient was kept under observation for two weeks before being discharged with no serious complications.
Keywords: Bladder rupture; Cervical lacerations; Precipitated labor; Childbirth trauma; Case report.
Introduction
Spontaneous bladder rupture following normal vaginal delivery is a surgical postpartum emergency. Previous cesarean section, vacuum/forceps-assisted vaginal deliveries, and distended bladder compressed by engaged head in birth canal are all risk factors for bladder injuries in healthy parturient women 1. Cases of bladder rupture, accompanied by uterine rupture, have been rarely reported following vaginal birth after cesarean section 2. To the best of our knowledge, however, no cases of combined cervical laceration and bladder rupture have been reported to date. We present the first case of spontaneous bladder rupture with cervical laceration after a precipitated vaginal delivery.
Case Presentation
A 31-year-old, G2P1L0D1, woman with gestational diabetes, was admitted to our maternity ward at 38 weeks of pregnancy for elective induction of labor to terminate her pregnancy. She had a history of preterm birth and was a known case of minor thalassemia. The induction of labor began at 5:00 a.m. with oxytocin, and contractions began approximately two hours later. Table 1 depicts the progress of labor. During her labor, the patient urinated once. Finally, at 10:40 a.m., she gave birth to a baby boy weighing 3700 grams with an Apgar score of 7/9. Excessive vaginal bleeding was observed following placental expulsion. The examination revealed an extensive laceration in the vagina and cervix that was repaired by the obstetrician and midwife. The patient was catheterized and was being closely monitored. A urologist was consulted due to the oliguria and hematuria (100 cc output with gross hematuria within 5 hours of childbirth). Cystography, as recommended by the urologist, revealed the bladder rupture. The patient was prepared for a laparotomy immediately. The laparotomy was performed by a team of obstetricians and urologists. Several hematomas were discovered in the uterine body and the broad ligament that the team decided not to manipulate because it did not grow during the surgery. A bladder rupture was found at the dome of bladder that was repaired in two layers. One pack cell unit and two FFP units were transfused. A peritoneal drain was placed posterior to the bladder and the skin incision was closed in layers. The patient was observed for two weeks. The result of the ultrasound revealed the shrinking of the hematoma. The blood and renal tests were normal. The catheter was removed after 2 weeks and the patient was discharged.
Table 1: The progress of labor
Discussion
Precipitate labor is defined as the expulsion of the fetus within three hours of the start of contractions. Few studies have found that precipitated labor is harmful to both the mother and the newborn. Precipitated labor, which is most commonly associated with placental abruption and induction of labor, is a significant risk factor for maternal complications 3. Maternal morbidities reported included extensive birth canal lacerations, uterine rupture, placenta retention, the need for revision of uterine cavity, post-partum hemorrhage, and blood transfusions 3,4. The lower urinary tract's anatomic proximity to the reproductive tract predisposes it to iatrogenic injury during obstetric procedures. The bladder and lower ureter are two of the most commonly involved organs. Because the dome of the bladder is the weakest area, most bladder ruptures occur through the peritoneal cavity 5. In our case, in addition to deep vaginal tears and extensive cervical laceration, bladder rupture occurred, but the diagnosis was delayed by a few hours. Given the nonspecific clinical features of bladder rupture, the diagnosis should be approached with caution. Oliguria and gross hematuria after a traumatic childbirth increase the likelihood of bladder rupture. In such cases, a cystogram is thought to be the best method for early detection.
In our case the patient had induced labour with oxytocin. The use of oxytocin to induce labour can result in tachy-systole and thus shorter deliveries. So in our case we believe that the power of uterine contractions and quick descent of passenger (3700 grams fetus) were the main risk factors of precipitated labour and the complications accompanied with it. A distended bladder during labor, particularly in our case, where the fetus descended quickly, could also be a factor in bladder rupture. Although the patient urinated normally during labor, it was critical to ensure that the bladder was empty, especially during the active phase of labor, to avoid bladder damage.
CONCLUSIONS
Bladder and cervical rupture should be considered, after precipitated vaginal delivery. When there is gross hematuria, a urinary catheter should be inserted to monitor the hematuria and urine output. If the hematuria persists and other associated symptoms appear, cystography is a useful tool for determining the severity of the bladder injury and determining the cause.
Funding
This study received no specific funding from public, commercial, or not-for-profit funding agencies.
Conflict of Interest
Authors had no conflicts of interest to declare.
Patient consent
Obtained.
For more details: https://ijcimr.org/editorial-board/
#Bladder rupture#Cervical lacerations#Precipitated labor#Childbirth trauma#Case report#postpartum#oxytocin#vacuum#laparotomy#Cystography#hemorrhage#Dr Fatemeh Darsareh#ijcimr
0 notes
Text
Spontaneous Rupture of Wandering Spleen: Case Report by Mina Alvandipour in Journal of Clinical and Medical Images, Case Reports

Abstract
Keywords: Spleen; wandering spleen; ectopic spleen; splenic rupture.
Introduction
A wandering spleen is a rare clinical occurrence with fewer than 500 cases reported and an incidence of less than 0.2% [1]. wandering spleen is caused by either extreme laxity or absence of the normal ligaments that anchor the spleen to the left upper quadrant. Gravity also plays a role by allowing the spleen to descend into the lower abdomen attached by its vascular pedicle [2]. Symptoms depend on the degree of torsion and range from chronic abdominal pain in mild torsion to acute pain in severe torsion and infarction. Accurate clinical diagnosis is difficult because of the rarity of the condition and non-specific symptoms. Radiological evaluation includes usage of ultrasound, Doppler, abdominal CT or MRI depending upon availability or preference [3]. A wandering spleen can be either congenital or acquired. In the congenital condition the ligaments fail to develop properly, whereas in the acquired form the hormonal effects of pregnancy and abdominal wall laxity are proposed as determining factors .However, the precise etiology of the wandering spleen is not known [1]. We present a spontaneous rupture of a wandering spleen with severe torsion and infarction and abdominal pain without any history of trauma.
Case Report
A 25 years old female present to emergency unit with 2 week history of progressive abdominal pain, recurrent constipation ,vomiting and loss of appetite. There was no history of melena, fever, and hematochezia and weight loss. On examination there was periumbilical and epigastria tenderness and a firm and tender mass in the right side of the abdomen without muscle guarding and rebound tenderness. The vital sign and laboratory results were all within the normal ranges, except decreased hematocrit (hemoglobin-8.4). The plain abdominal radiograph was un-remarkable while abdominal ultrasonography with color Doppler showed absence of spleen in its normal location in the left upper abdomen. Also it detects a heterogeneous hypoechoic capsulated mass with diameter of 175mm in right lower abdomen. Other organs of the abdomen were normal. Abdominal pelvic CT scan with and without contrast was recommended and findings was Absence of the spleen in its normal position in the left hypochondrium, and presence of large diameter mass (splenomegaly)in the right sub hepatic area(Wandering spleen) . Other organs of the abdomen were normal. Contrast-enhanced computed tomography (CECT) of the abdomen revealed whirlpool sign near the umbilicus. The splenic parenchyma showed abnormal enhanced areas, suggestive of splenic torsion and infarction.
A final diagnosis was wandering spleen with torsion of the vascular pedicle and infarction. The patient underwent a total splenectomy. During the laparotomy, an enlarged and infarcted mass was seen in right side of abdomen. The characteristic “whirlsign” can be seen in the area of the splenic vascular pedicle, indicative of torsion. Histological examination confirmed total infraction of the wandering spleen. The postoperative course was uneventful, and the patient was discharged on the 4th day after the operation.
Discussion
A wandering spleen is a rare but well-known entity. The incidence is < 0.2%. It is more common in females than males between the second to fourth decade of life and children [4]. Splenic weight >500 g in more than 8 out of 10 cases [5]. Interestingly, it has been reported that one out of three cases of wandering spleen appears in children bellow the age of 10 years old [7].
Wandering is characterized by splenic hyper mobility that results from elongation or mal-development of its suspensory ligaments. It is also known as aberrant, floating, displaced, prolapsed, ptotic, dislocated or dystopic spleen. Ectopic spleen, splenosis and accessory spleens are separate clinical entities and must be distinguished from it [5]. If the pedicle is twisted in the course of movement of the spleen, blood supply may be interrupted or blocked, resulting in severe damage to the blood vessels .Acute splenic torsion compromises venous outflow, which causes congestion and impairment of arterial inflow. Pain is originated from the splenic capsular stretching with rapid splenic enlargement and localized peritonitis [6]. Etiology is congenital or acquired. In case of congenital anomaly, a failure occur in fusion of the dorsal mesogastrium with the posterior abdominal wall during the second month of embryogenesis. Acquired risk factors that predispose to wandering spleen include pregnancy, trauma and splenomegaly [7]. Splenic torsion is usually clockwise. Complications of splenic torsion include: gangrene, abscess formation, local peritonitis, intestinal obstruction and necrosis of the pancreatic tail, which can lead to recurrent acute pancreatitis [8].
Wondering spleen had nonspecific symptoms such as abdominal pain that make diagnosis extremely challenging. As a result, radiologists play a major role in the diagnosis of this condition and its complications. Torsion may occur acutely and present with infarction or peritonitis. Chronic intermittent torsion can lead to pain, splenomegaly, and functional splenectomy. Contrast-enhanced computed tomography (CT) is the best imaging tool to make this diagnosis, although ultrasound may be used as well. Imaging findings on CT include identification of a spleen in an abnormal location, or with an abnormal orientation in the left upper quadrant. Often the wandering spleen is identified as a “comma” shaped mass in abdomen, with no normal left upper quadrant spleen [9].
Laboratory investigations are non-specific. Thrombocytopenia, through a mechanism of spleen enlargement secondary to compression of the splenic pedicle is rarely found [7]. The clinical presentation of wandering spleen is variable; it is either asymptomatic or noted incidentally during physical and radiographic examination or presents as acute abdomen due to torsion with subsequent infarction. The most common presentation is a mass with non-specific abdominal symptoms or intermittent abdominal discomfort due to congestion resulting from torsion and spontaneous detorsion [10]. Today, the only recommended treatment for wandering spleen is operation [7]. Splenectomy is indicated for infracted spleen and sometimes for huge splenomegaly precluding splenopexy. Splenopexy is the choice of treatment if the spleen is not infarcted [6]. Splenic preservation is highly recommended for young patients—those under one year of age up to those in their thirties—who are at particular risk for overwhelming post-splenectomy sepsis [10]. This should be appropriately followed up by the prophylactic vaccines against post-splenectomy sepsis syndrome. Ideally they should be administered before surgery; however, in emergencies this is not always possible [1].
Conclusion
In this case, splenectomy was done due to spleen infarction. Laparotomy was done in this case because of low experience at laparoscopy splenectomy. This report highlights the investigations and management necessary for a patient who presents with an ischaemic torted wandering spleen.
Acknowledgement: None.
Conflict of Interest: None.
Funds: None.
For more details : https://jcmimagescasereports.org/author-guidelines/
#Spleen#wandering spleen#ectopic spleen#splenic rupture#Radiological#ultrasonography#Contrast-enhanced computed tomography#laparotomy#laparoscopy#Mina Alvandipour#JCMICR
0 notes
Text
I think my career as an RN in the middle of the worst of C19 on a med/surg unit plus now working a vascular/thoracic PCU/ICU has desensitized me to so much weird and traumatizing shit
#honestly i thought my m/s C19 unit was wild#but the shit ive seen on VPCU and VTICU?#fucking wild#have yall ever seen a bedside exploratory laparotomy?#cause i have#we put a fucking Foley cath in this ladys abdomen#to drain fuckin feces#ive kept corpses breathing for no reason than the family says so#ive bleached pt blood off my shoes then went to dinner with my fam immediately after#ICU is a wild experience#personal#work shit#if someone needs me to tag this stuff specifically please let me know#im used to it#but if yall arent#let me know
0 notes
Photo
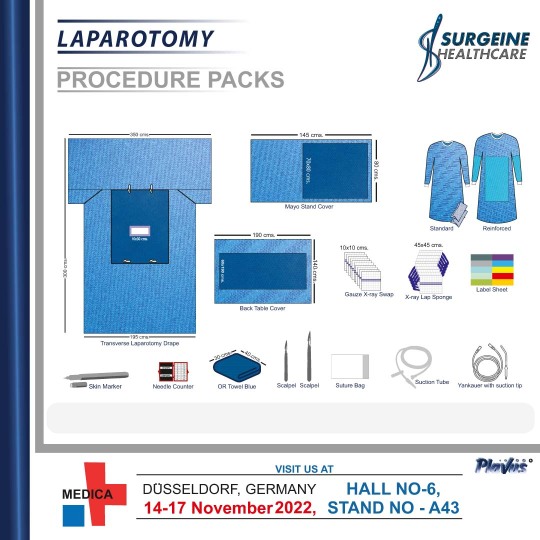
The Laparotomy Procedure Packs are specially designed for various general types of surgical procedures in the operating room. These products offered by us are developed using superior quality raw material in accordance with #international medical standards. Our products are hygienic and are well appreciated in the market for their durability.
0 notes
Text
https://joyrulez.com/blogs/199905/Global-Laparotomy-Sponges-Market-Size-Overview-Key-Players-and-Forecast
0 notes
Text
Evaluating the Utility of Fast in Acute Blunt Abdominal Trauma in the Emergency Department: 20 Years On by Lateef F*

Abstract
Introduction: Blunt abdominal trauma (BAT) is a common presentation in the Emergency Department (ED) and associated with high mortality and morbidity. Given the time-sensitive nature, it is necessary to evaluate if FAST possesses adequate sensitivity and specificity to confidently rule out life-threatening injuries and guide the course of management. A positive FAST result would indicate intra-abdominal injury and prompt urgent surgical intervention, particularly in hypotensive patients. This review aims to examine relevant literature to evaluate the diagnostic utility and outcomes of FAST, and important external factors to be considered.
Methodology: Keyword search of PubMed and the Cochrane Library yielded 514 articles, from which 61 studies were chosen based on the inclusion and exclusion criteria.
Results: FAST demonstrates low to moderate sensitivity and Negative Predictive Value (NPV) and high specificity and Positive Predictive Value (PPV) in detection of hemoperitoneum and associated intra-abdominal injuries. Sensitivity for detecting peritoneal fluid is the highest. While superior to DPL, it has yet to surpass the diagnostic utility and accuracy of CT.
Conclusion: FAST is essential and should remain the primary preliminary radiological assessment of acute BAT. A positive FAST is highly predictive of intra-abdominal injury but a negative FAST cannot accurately rule out intra-abdominal injury. Negative FAST results should be succeeded by continued clinical observation, and serial FAST examinations or CT-scan should clinical signs not correlate. Current literature offers no evidence that FAST should replace CT as the diagnostic standard for BAT or a definitive ability to determine the necessity of immediate surgical management.
Keywords: Focused Assessment for Sonography; FAST; E-FAST; Ultrasonography; Point Of Care Ultrasound; Pocus; Blunt Abdominal Trauma; Laparotomy and CT
Introduction
Abdominal trauma is a common presentation in the ED and also one of the leading causes of death in young adults, under 45 years. It can be broadly classified into high or low energy injuries, and blunt or penetrating abdominal trauma. Blunt abdominal trauma (BAT), may be the result of road traffic accidents, physical assault or falls from height. Penetrating injuries are generally caused by firearms and stabbings. The focus of this review will be blunt abdominal trauma, as it is by far the more common presentation. A study was conducted by The Western Trauma Association Multi-Centre Trials of 392,315 blunt trauma patients at 12 major trauma centres. Majority of the injuries were caused by motor vehicle collisions (60%). 47% of the patients had documented hypotension and solid organ, small bowel, and large bowel injuries occurred in 38%, 35%, and 28% respectively. The most commonly associated injuries were spine fractures (44%) and pneumothorax/haemothorax (42%) [1].
Up to 50% of patients with severe abdominal trauma and/or multiple distracting injuries are reported to either have a normal initial abdominal exam, or are obtund and unable to provide a reliable index of suspicion. This affects both the physical and imaging examinations [2]. Diagnostic errors are responsible for approximately 10%–15% of preventable deaths in trauma centre audits. The sole reliance on clinical assessment as the main indication for surgery has led to negative laparotomy rates of as high as 40% [3]. A retrospective analysis found the incidence of short‐term complications caused by negative laparotomy to be 43% [4].
A quick, effective and efficient imaging approach is necessary to exclude life-threatening injuries. This modality would preferably need to have high sensitivity and specificity [5]. Prior to FAST, Diagnostic Peritoneal Lavage (DPL) was the standard initial diagnostic investigation. Although an invasive test, it could be done rapidly and was relatively safe with high sensitivity but had a significant false‐positive rate, which potentially exposed patients to the risks of an unnecessary laparotomy [6]. All patients who sustain blunt trauma to below the nipple line, are assumed to have intra-abdominal injuries until proven otherwise. Prompt reliable diagnosis and characterization of the abdominal injuries is essential to reduce risk of mortality and morbidity. Hemodynamic instability is a high-risk clinical sign and as such, both the diagnostic and interventional thresholds for these patients should be lowered. The three main types of blunt abdominal trauma injuries are solid organ injury, hollow viscos/mesenteric injury and vascular injury. The most commonly injured intra-abdominal organ is the spleen, followed by the liver and the genitourinary tract [7].
Immediate laparotomy should be done for patients with signs of peritoneal irritation, fresh blood on rectal exam, fresh blood aspirated from nasogastric tube, stab wounds with implement in-situ, gunshot wounds traversing the abdominal cavity, suspected intra-abdominal injury with hemodynamic instability, ultrasound evidence of active haemorrhage, and X-ray evidence of pneumoperitoneum or diaphragmatic rupture. In a retrospective cohort study of consecutive normotensive blunt trauma patients at 2 trauma centres, there was a strong association between a positive FAST and the need for therapeutic laparotomy. (Adjusted OR 44.6, 95% CI 1.77–1124). Thirty-seven percent of patients with a positive FAST required therapeutic laparotomy vs. 0.5% with a negative FAST [8]. Another study quoted lower figures, where only 25% of patients with intra-abdominal fluid required laparotomy [9].
Imaging modalities most often used to evaluate abdominal trauma in the ED are the Focused Assessment for Sonography for Trauma (FAST) and the Computed Tomography scan (CT-scan) which is the current reference diagnostic gold standard. The purpose of this study is to present a systematic review on the utility of the primary first line imaging modality FAST, in the acute assessment of blunt abdominal trauma.
Methodology
A systematic review of the literature was achieved using the electronic database PubMed and the Cochrane Library. Various query terms were tested to obtain enough data and to avoid unspecific information. Duration of search was from 1stMarch 2020 to 1stApril 2020. There was no limit on geography, age, type of study or date of article. Only original studies published in English were considered for this review. Keyword search yielded 514 articles, from which 61 studies were chosen based on the inclusion and exclusion criteria.
The keywords used in the search include: Focused Assessment for Sonography, FAST, E-FAST, Ultrasonography, Point of Care Ultrasound, PoCUS, Blunt abdominal trauma, Laparotomy and Computed tomography, CT
For studies to be included in this study, the inclusion criteria are as follows:
Acute presentation of blunt abdominal trauma at the ED
PoCUS/FAST or E-FAST examination done performed by radiologists, non‐radiologist clinicians, or ultrasound technicians
Definitive diagnosis verified by CT-scan or operative diagnosis.
Sufficient information on diagnostic test accuracy (i.e. sensitivity, specificity)
The studies were excluded if:
Insufficient information on diagnostic test accuracy
Case reports, case series
Unclear index or reference tests
Diagnostic case-control studies that compared patients with known case status to healthy controls. (This creates artificial populations and tends to overestimate sensitivity of the index test)
Patients with penetrating abdominal injuries
Results
Focused Assessment for Sonography for Trauma (FAST)
Ultrasound based trauma algorithms were only introduced formally into trauma literature in 1996.FAST is a limited abdominal ultrasound modality used in acute trauma as part of Advanced Trauma Life Support (ATLS)protocol to identify intra-abdominal fluid collections using a 3.5Hz sector transducer. FAST was established in 1999 after the FAST consensus conference and a subsequent study done at Massachusetts General Hospital in Boston, USA, showed the number of FAST scans increased from 15 % to approximately 34 % in the period 2002–2011, while the number of abdominal CT scans decreased from 35 % to 14 % in the same period [10]. In a prospective study on influence of FAST on trauma management, 194 patients underwent FAST. It was shown that FAST prevented an unnecessary laparotomy in 1 patient, CT in 23 patients, and DPL in 15 patients. There was an overall reduction in CT requests (from 47% to 34%) and DPL requests (from 9% to 1%) (p < 0.0001) [11].The goal of FAST is to detect hemoperitoneum in the right and left sub phrenic space, peri-splenic fossa, hepatorenal recess, suprapubic window (Pouch of Douglas or rectovesical pouch) and hemopericardium in the subxiphoid space. A positive FAST result would mean that there is free fluid in either of these abdominal compartments, which is a surrogate for active haemorrhage and in one study, has demonstrated a 65% sensitivity in detection of abdominal injuries requiring surgery [12].
E-FAST and Ex-FAST
E-FAST was established in 2004 and is now the diagnostic standard of ATLS, virtually replacing DPL. The E component refers to bilateral anterior thoracic sonography which searches for free air in the pleural cavity as evidence of an acute traumatic pneumothorax. It has been shown to have greater sensitivity and specificity than traditional chest radiography [13]. There is also some reference to Extended FAST or Ex-FAST. It is a combination of both physical examination and FAST. An abnormal examination constitutes signs of hemodynamic instability, abdominal bruising, tenderness, absence of bowl sounds, peritonism, seatbelt sign, lacerations etc. [14]. In a retrospective study of 354 children in the ED of which 14% (n=50) had intrabdominal injury (IAI), the use of Ex-FAST showed greater sensitivity (sensitivity of 88% (95% CI: 76‐96%) and Negative Predictive Value (NPV) 97.3% (95% CI: 94.5‐98.7%)) over either physical examination [OR, 15.2; 95% CI: 7.7 ‐ 31.7] or FAST [OR, 14.8; 95% CI: 7.5 ‐ 30.8] alone [15].
The execution time of E-FAST examination averaged 2.3 ± 2.9 min for chest US and ≤5 min for standard FAST [16]. FAST has been reported to be able to detect as little as 200ml of fluid in Morrison’s pouch and can completed in less than a minute in the hands of an experienced operator. This is many times faster than a CT-scan which on average takes approximately 30minutes and hence unsuitable for an unstable patient in an emergent setting. Moreover, it is easily repeatable, physicians can be easily trained, inexpensive, non-invasive and does not require contrast nor exposes the patient to ionizing radiation. Although these are insufficiently substantiated by sufficient evidence, other possible beneficial outcomes include shortening of the primary trauma assessment, more precise triaging, avoidance of unnecessary interventional procedures, and associated costs
The reliability and quality of images obtained from FAST is also greatly dependent on the training and experience of its operator. A comparison of the reproducibility of FAST results between Emergency Medicine Residents (EMRs) and Radiology Residents (RRs) showed sensitivities, specificities, PPV, NPV and accuracy of evaluating intra-peritoneal fluid to be very similar at 80%, 95%, 57%, 98% and 94% and 86%, 95%, 59%, 98% and 94%. This shows that EMRs are well-trained to use FAST and their results would be similar if not identical to an RR [17]. However, a comparism done in another study amongst US operators with low, moderate and extensive experience reported sensitivities of 45%, 87%, and 100% respectively in detecting <1L of peritoneal fluid [18].
A recent review article has quoted FAST sensitivities that range between 63 % and 99 % and specificities range from 90% to 100%. These results are similar for the detection of free intraperitoneal fluid, with sensitivities ranging from 69 % to 98 % and specificities of 94% to 100% [19]. Another study reviewing literature from various institutions around the world has reported lower thresholds of sensitivities ranging from 42.0%–91.7%, specificities 83%–100% and accuracies 9%–96% for the utility of E-FAST examinations. Its own prospective observational study examining the diagnostic accuracy of E-FAST done by emergency physicians compared to CT at the ED of a level 1 trauma centre found that out of 132 patients with blunt abdominal trauma, FAST sensitivities (only abdomen) was 42.9% (95% CI: 9.9%, 81.6%) and specificity was 98.4% (95% CI: 94.3%, 99.8%). The + LR of the FAST exam for abdominal free fluid as 26.8 (95% CI: 5.3, 135.2) and − LR was 0.58 (95% CI: 0.31, 1.1) [20]. This consistently high reported specificity of FAST was highlighted in a systemic review of 11 articles containing prospectively derived data with FAST results, patient disposition and final diagnoses. It showed that out of the 2,755 patients, 448 (16%) went to the OR. In total, there were 5 false-negatives derived from FAST; 3 involving inadequate scans and 2 of blunt trauma-induced small bowel perforations without hemoperitoneum [21]. The sensitivity of an examination is the “correct positive test rate” and measures the proportion of patients with an intraabdominal injury who have a positive test result. A high degree of sensitivity is not useful to rule in a diagnosis, but rather to rule out a particular condition. Similarly, high levels of specificity indicate that positive findings will detect the presence of a pathology. This suggests that when FAST is positive, there is high certainty of injury but when it is negative there’s a higher chance the injury was undetected. Hence, there is still large uncertainty in diagnostic confidence, with its wide sensitivity range and cannot confidently or safely exclude the presence of intra-abdominal injury.
FAST in Abdominal Trauma
In a meta-analysis [22] of emergency ultrasonography for BAT, a sensitivity range was observed as low as 28% and as high as 97%, specificities were close to 100%. A summary measure of 0.90 was calculated for the sensitivity-specificity pair closest to the desirable upper left corner of the ROC curve, which could be interpreted as 10% of abdominal injuries will be missed by FAST. Low sensitivities, coupled with low NPV, negative LRs and associated post-test probability, diminishes confidence in negative FAST findings. However, high specificities and LRs>10 would almost confirm intra-abdominal injury if positive and hence the need for surgical management.
In a retrospective study, 3181 blunt normotensive trauma patients presenting at a single level 1 trauma centre were evaluated with FAST and stratified into various groups of Injury Severity Scores (ISS). A one-time, four-view FAST examination in patients with ISS ≥ 25 had a lower sensitivity of 65 % than those with an ISS < 25 (80–86 %). More than 82 % of the FAST-missed injuries in patients with ≥ 25 ISS were solid organ injuries of the liver, spleen and kidneys [23]. An observational study of the diagnostic accuracy of FAST in 105 patients from King Fahad Military Medical Complex Dhahran, Saudi Arabia with blunt abdominal trauma demonstrated sensitivities of 76.1% (95% CI, 64.14- 85.69%), specificity 84.2% (95% CI, 68.75- 93.98%) and accuracy 79% (95% CI, 70.01- 86.38%. FAST could detect free fluid in 37 out of 39 patients with high grade sold intra-abdominal injuries. However, it could not detect small amount of fluid and nearly half of the negatives had low grade visceral injuries [24]. These studies highlight potential factors that may affect the results of the FAST examination, such as the presence of multiple other distracting injuries, higher likelihood for missed solid organ injuries and reduced sensitivity for fluid in patients with only low-grade injuries.The reason for this could be that hemoperitoneum is not always seen in liver or splenic injuries and hence it doesn’t matter if FAST has a high sensitivity for peritoneal fluid [12].
A systemic review evaluating the diagnostic accuracy of point‐of‐care sonography (POCS) for diagnosing thoracoabdominal injuries in patients with blunt trauma included 34 studies with a cumulative cohort of 8635 participants. For abdominal trauma, POCS had a sensitivity of 0.68 (95% CI 0.59 to 0.75) and a specificity of 0.95 (95% CI 0.92 to 0.97), with statistically significant lower values in children. To put this in perspective, it meant 73 false negatives and 29 false positives for every 1000 adult patients, assuming the observed median prevalence of thoracoabdominal trauma of 28% [25].
In paediatric BAT patients, the diagnostic accuracy of FAST has been reported to be lower compared to adults. A multi-institutional (n=14) analysis of level1 paediatric trauma centres yielded low sensitivities (28%) and high specificities (91%) for IAI consistent with paediatric literature but improved sensitivities (44%) and similar specificities (89%) for IAI requiring acute intervention. However, FAST missed 75% of liver injuries and 57% of spleen injuries and 56% of 27 patients whom required acute intervention for IAI had negative FAST. All the patients were normotensive and had abnormal abdominal examination [26]. However, in a separate observational prospective study comparing FAST evaluation of hypotensive and normotensive children with BAT, FAST showed a 100% sensitivity in detecting peritoneal fluid in hypotensive patients [27]. A prospective study was done on 160 hemodynamically stable paediatric trauma patients who had undergone both FAST and CT. Forty-four of the 160 patients had an intraabdominal injury on CT, 24 (55%) of which had normal screening sonography. Accuracy of sonography compared with CT was 76% with a negative predictive value 81% [28]. While the statistics of these three studies on the use of FAST in paediatric BAT patients do vary, sensitivities and specificities are both generally on the lower threshold of the adult range. They also show consistency of hypotension as a strong predictor of IAI and the poor ability of FAST to detect solid organ injuries.
FAST and Other Modalities
A prospective study [16] was done of 601 adult trauma patients at the ED who underwent a Chest Abdominal-Focused Assessment Sonography for Trauma (CA-FAST) exam prior to a thoracoabdominal CECT. Free fluid was detected in 116 patients with an overall accuracy of 91 % (95 % CI 85–93%). The following table illustrates the results of 4-view FAST and its individual views
FAST has different sensitivities for each abdominal cavity view, which translates to different diagnostic accuracies for the various types injuries previously mentioned in the methodology has well. In this study, FAST exhibits moderate to good sensitivity than previously quoted and with similar sensitive for the upper abdominal regions, followed by the pelvis and least able to detect fluid in the subxiphoid, pericardial space. It also shows good PPV, high specificity and NPV, consistent with previous studies [16].
This is supported by a 2-year review at a level1 trauma centre of 1027 patients who underwent FAST were stratified by operator skill level. It was shown that compared to patients with concordant FAST results, those with equivocal results had higher mortality (9.8 vs 3.7%, P = 0.02), decreased positive predictive value in the right upper quadrant (RUQ) (55 vs 79%, P = 0.02) and left upper quadrant (LUQ) (50 vs 83%, P < 0.01). However, unlike the previous study, this study observed worse outcomes has a result of the high rate of false negatives in the FAST examination.
However, some of these findings were obtained from only a single FAST scan (i.e. [23]), with the underlying assumption that fluid accumulates in the deepest parts of the abdomen. This can be influenced by anatomy, location of bleed, respiratory physiology, intra-abdominal adhesions etc. Thus, it would be prudent to consider the value of serial FAST scans, Contrast Enhanced Ultrasonography (CEUS), additional abdominal views and other imaging modalities such as CT with or without contrast media. A retrospective analysis [29] comparing the use of CTAP and Complete Ultrasonography of Trauma (CUST) in 19128 patients to screen for blunt abdominal trauma (BAT) from 2000 to 2011 in a Level 1 trauma centre was performed. It found that outcomes in CUST is equivalent to routine CTAP for BAT and leads to an average of 42% less radiation exposure and more than $591,000 savings per year.
The shortcomings of FAST can be bolstered by the application of CEUS. A recent meta-analysis [30] of 9 studies investigating the diagnostic accuracy of CEUS of abdominal trauma patients at the ED demonstrated that the CEUS had a sensitivity of 0.981 (95% CI: 0.868-0.950) and a false positive rate of 0.018 (95% CI: 0.010-0.032) for identifying parenchymal injuries, with an AUC of 0.984. These accuracies are similar to that of contrast-enhanced CT. Another study done on the application of CEUS in paediatric patients concluded CEUS proved to be an effective investigation in the hemodynamically stable child for identifying parenchymal injuries and for the characterization of focal liver lesions. It also showed comparable performance to CT and MRI with a specificity of 98% for identifying benign lesions and a negative predictive value of 100% [31]. However, the need for contrast in identifying intra-abdominal injury may not always be relevant in contributing diagnostic value. It can add confidence in cases of interpretation doubts or diagnostic difficulties, but some studies have shown CEUS to have similar sensitivities to baseline US [32].
Splenic injuries are the most common intra-abdominal injury followed the liver in the setting of acute blunt abdominal trauma. CEUS has been shown to be able to overcome the lower sensitive of FAST in detection of traumatic injuries with the reference standard as CT, to reach almost similar levels of accuracies. Evaluation of severity of splenic injuries is particularly important in the decision for surgical management as the spleen should be preserved if possible, due to the dual immunological and haematological functions [33]. However, a retrospective cohort study [34] at a level 1 trauma centre of 332 patients found that patients with spleen, liver, or abdominal vascular injuries were less likely to have false-negative FAST examination results (OR 0.3; 95% CI 0.1 to 0.5). Surprisingly, false-negative FAST results were not associated with increased mortality (OR 0.89; 95% CI 0.42 to 1.9) and these patients were fortunately also less likely to require therapeutic laparotomy. (OR 0.31; 95% CI 0.19 to 0.52).This at first glance may seem puzzling compared to previous studies; however, this is consistent with the generally high specificities of FAST and its lower sensitivities for solid organ injury and lower grade injuries which naturally may be less likely to require surgical intervention or carry a high mortality rate.
Computed Tomography and Abdominal Injuries
Computed Tomography is superior to FAST in evaluating solid organ, hollow vicus, mesenteric injuries and active haemorrhage. However, it has disadvantages such as radiation exposure, risk of contrast nephropathy or allergy, high cost, limited availability, requires more time and the potential need for sedation in paediatric patients. A level 1 trauma canter in the USA reported the radiation exposure of patients with a median ISS of 14 within the first 24 hours at a median of about 40 mSv. The lifelong risk of dying from a carcinoma is assumed to increase by about 0.1 % per 10 mSV. This risk also depends on gender, age and radiation location [19]. Although this is a minute amount, we can conclude that CT scans should be avoided when possible as it does expose the patient to a significant amount of radiation, enough cause a measurable increase in cancer risk.
A recent retrospective analysis evaluated the diagnostic performance of CT for detection of hollow vicus injury (HVI) in patients presenting with penetrating abdominal trauma at a level 1 Nordic trauma centre. Out of the 636 patients with penetrating abdominal trauma, 155 (85%) had a CT-scan on arrival, of which 41 (30%) subsequently underwent emergent surgery. Surgery revealed only 26 (63%) has HVI, showing that CT had 69.2% sensitivity and 90.5% specificity in detecting HVI [35].
Although FAST showed high accuracy for peritoneal fluid, it’s non-specific for solid organ injuries and prevalence of organ injury without accompanying free fluid can range from 5% to 37% [36]. It also lacks sensitivity for hollow viscos and mesenteric injuries, which not are only the most commonly missed but also associated with high morbidity and mortality and has a higher likelihood for requirement of surgical intervention than solid organ injuries. A retrospective study done on 32 patients showed that MDCT could diagnose bowel injury in all of the patients except one. The minor signs showed a higher sensitivity than the major signs [3]. This suggests a sensitivity for bowel injury much greater than FAST which was 12.5% amongst 4 patients and 37.4% in another study [36]. Other studies have also quoted high sensitivities (94%) and PPV (92%) for CT in detecting bowel injury [37]. A meta-analysis [38] of articles concerning the incidence and significance of free intra-abdominal fluid on CT scan of blunt trauma patients without solid organ injury concluded that isolated finding of free intra-abdominal fluid on CT scan in patients with blunt trauma and no solid organ injury does not warrant laparotomy. Instead, its aetiology should be evaluated and other CT signs of GI perforation should be searched for. Small bowel injury had the highest incidence of positive free fluid without evidence of solid injury, but the combination of both pneumoperitoneum and free fluid increased the sensitivity of detection of small bowel injury [3].
When compared with its predecessor DPL, it showed significant advantage in its pre-test probabilities with a positive LR of 10.83 (95% CI 6.45 ± 18.17) and a negative LR of 0.11 (95% C.I. 0.06 ± 0.21). When compared to CT, FAST still had a positive LR 11´42 (95% C.I. 8.01 ± 16.29)) in confirming presence of intra-abdominal injuries, but it was still below acceptable thresholds in safely excluding abdominal injuries (negative LR 0.21 (95% C.I. 0.16 ± 0.29)), which is essentially the gold for immediate trauma management. Hence FAST is unable to be the diagnostic standard for obtaining a definite diagnosis [22].
Whole body CT (WBCT) is the gold standard for trauma imaging, however it is usually only supported by highly specialised trauma centres with the appropriate infrastructure. A clinical review highlighted observational data that suggested WBCT was associated with decreased mortality and time required for trauma evaluation [39]. On the other hand, randomized controlled data from the REACT-2 trial [40] suggests no mortality benefit to this diagnostic tool. There is no clear evidence or sufficient data to prove that CT should be the first line imaging modality in acute blunt abdominal trauma. As we simply lack the resources and time to conduct CT for every patient, not to mention the higher costs and having to subject every patient to ionizing radiation, the decision for CT should remain on a case to case basis. Decision making should be based on a combination of history, physical examination, clinical signs and other imaging modalities i.e. FAST/X-ray. More studies (i.e. RCTs) will have to be done to assess its outcomes over FAST in the emergency setting of BAT and its utility in assessing need for surgical intervention.
A study [41] assessed CT scans of paediatric patients with abdominal trauma for presence, location, and severity of intraabdominal injury, and amount of peritoneal fluid. It was found that only 17% of the 1,486 children had peritoneal fluid demonstrated by CT but 80% had concomitant intraabdominal injury. This suggests that although presence of peritoneal fluid is a strong indicator of intra-abdominal injury, it can be present without, with solid organ injury being the most frequent (68%). Furthermore, it may also indicate that like FAST, CT may have reduced sensitivity in picking up intra-abdominal injuries without peritoneal fluid. CEUS may be applicable for the 37% of patients with intra-abdominal injuries picked up by CT but no peritoneal fluid was detected.
Discussion
In the emergency department today, E-FAST is still the diagnostic standard for ATLS in the event acute abdominal trauma. Its findings, combined with history taking, physical examination and other imaging modalities (i.e. chest/abdominal radiography) would then determine the need for a CT-scan or emergent surgical intervention (i.e. laparotomy). Training with learning objectives and the duration as well as supervision should be standardized with the help of existing scientific principles. FAST demonstrates low to moderate sensitivity and high specificity as a single examination. There have been no studies that examined the utility of serial FAST examination. This is dependent on several factors such as, the time elapsed since trauma, type and extent of injury, patient group (i.e. age, BMI), quality of ultrasound machine, and skills of the FAST examiner. It was also mentioned previously that FAST results are also made on the assumption that fluid tracks to the most gravity dependant parts of the abdomen, and can be influenced by anatomy, location of bleed, respiratory physiology, intra-abdominal adhesions etc. However, it was seen in many studies that many patients who tested negative on FAST did have intra-abdominal injuries subsequently detected on CT or intra-operatively.
To improve sensitivity, the three standard abdominal FAST views should be supplemented by six further sections: sub diaphragmatic, caudal liver margin, parabolic groove, between intestinal loops, retroperitoneal and right upper abdomen view for the detection of free air. The examination should also include visualisation of solid organs such as spleen, liver, and kidneys to assess for injury. Serial exams can also be done at 12hourly intervals to reduce the likelihood of false negatives and reconfirm earlier findings. The effectiveness of serial FAST examinations in patients of deteriorating clinical status was demonstrated in a study that showed a 50% decrease in false-negative rates by 50% and an 85% increase in sensitivity for free fluid detection. The sensitivity and NPV for injury detection increased to 71% and 97%, respectively [42]. These aforementioned strategies can be investigated further through the conducting of randomized controlled trials. Diagnostic errors owing to human error can also be reduced through a more systematic approach such a diagnostic checklist, or management of physician fatigue. Albanese et al. also believed that serial physical examinations are the gold standard for diagnosing GI perforation from blunt abdominal trauma [43].
FAST does offer greater insight than solely relying on clinical signs but it is unsuitable to obtain a diagnosis with sufficient certainty nor can a negative result safely exclude intra-abdominal injury? Possible reasons for poorer accuracy could be that it was in the early post-injury phase, where sufficient hemoperitoneum had not yet accumulated thus leading to false-negative results. FAST has also shown poor sensitivity to identify hollow viscos or solid organ injuries not associated with hemoperitoneum such as early bowel injury or pancreatic injury and limited utility in detecting retroperitoneal haemorrhage. Other potential sources of error include obesity and subcutaneous fat, body habitus and positioning, ascites due to pre-existing medical condition, pre-existing pericardial effusion, and the presence of intra-abdominal cysts or masses [44]. Patients with these characteristics should be evaluated with a subsequent CT-scan if hemodynamically stable.
A comparative study [45] evaluating the use of FAST was done on 706 patients with blunt abdominal trauma. 460 patients were managed with FAST and 246 without FAST. Respectively, both groups showed similar accuracies at 99.1% and 98.0% respectively, and frequency of laparotomies at 13.5% and 14.2%. FAST patients also had a lower mean diagnostic cost and lower mean time required for diagnostic work up. In the FAST group, the computed tomographic rate was 24%, whereas it was 91% in the no-FAST group. As previously established, it’s been shown in many studies that FAST greatly reduced the need for CT-scans, a recent review quoting rates as high as 50%. Although there are surprisingly no significant differences in mortality or laparotomy rates. These two studies show that FAST is cheaper, fast, decreases the length of hospital stay, duration to definitive treatment, and use of healthcare resources [6]. However, it does not actually improve accuracies nor change the management or treatment outcomes of BAT.
Nevertheless, it is shown that peritoneal fluid if present, is highly sensitive to intra-abdominal injury, specifically active haemorrhage which is an indication for emergent laparotomy. This can not only save crucial time in achieving haemostasis instead of waiting for the results of the CT-scan, but is more accurate than DPL which is invasive, or simply clinical signs alone. Moreover, E-FAST is far superior to chest X-ray in terms of detecting haemothorax and pneumothorax and is the only simple bedside method for detecting hemopericardium. Thus, the purpose of E-FAST is for rapid assessment of intra-abdominal that require immediate surgical intervention, especially if the patient is hypotensive, and/or to evaluate the need for a CT-scan. FAST should not replace the abdominal examination or history taking nor be the sole modality replacing CT, for evaluation of abdominal trauma, particularly in patients with abdominal pain, contusions or altered mental status as it’s been shown to intra-abdominal injury can be present even without peritoneal fluid. While CT should not replace FAST either as the 1st line imaging modalities in BAT, a high index of suspicion and low threshold is required. Also, FAST does reduce the frequency of need for CT-scans in the ED and hence the overall costs and radiation exposure to the patient, along with more efficient use of hospital resources. If a new diagnostic algorithm is faster and less expensive it must also be as safe and accurate as the conventional diagnostic algorithm before it can become the new standard of care. Given the current level of evidence we have today, we can conclude that CT should still remain the gold standard for definitive evaluation of blunt abdominal trauma and guide its subsequent management.
Although CT does have greater diagnostic accuracy compared to FAST and is still the gold standard for definitive abdominal trauma imaging, there are little studies done to evaluate the outcomes of patients who have had a CT-scan done without E-FAST. It is established that CT-scan does carry significantly greater number of risks compared to FAST, including requiring more time which the hypotensive patient may not be able to afford. CEUS FAST has showed higher accuracies than conventional FAST in detecting liver, spleen, or kidney injury and active bleeding, similar to that of CT in children and adults with BAT. However, larger randomized trials to evaluated diagnostic accuracy and outcomes will be required to further validate its clinical use as the standard of care [19]. Assuming that major blunt abdominal or multiple trauma is associated with 15% mortality and a CT‐based diagnostic work‐up is considered the current standard of care, 874, 3495, or 21,838 patients are needed per intervention group to demonstrate non‐inferiority of FAST to CT‐based algorithms with non‐inferiority margins of 5%, 2.5%, and 1%, power of 90%, and a type‐I error alpha of 5% [6].
However, studies have shown that despite steady improvement of sonographic resolution properties over the past 20 years, diagnostic precision has not significantly improved, which may suggest that ultrasonography in the emergent setting and the experienced gain may have already reached its limit [22]. Technological advances have allowed recent development of wireless probes [46] and devices capable of short- and long-distance image transmission to remote displays. As ultrasound technology continues to evolve, we expect to see further miniaturization, better image quality and even holography or wearable technology [47]. The FAST exam is easily learned and educational materials are abundant both online (images and video) and in print. As both FAST and E-FAST increase in popularity, implementation of robust educational programs will become increasingly important so that future generations of practitioners are able to acquire high quality sonographic images, interpret those images, and also make real-time clinical decisions based on that information. Trauma centres can look into optimizing infrastructure and trauma protocols to shorten the time required for CT-scan, which has been reported in some studies to be as quick as only a few minutes. It is also crucial to emphasize integration of various sources of information and not to rely solely on a single modality.
Conclusion
FAST is an essential tool for preliminary assessment of intra-abdominal injury, including BAT. A FAST result if positive, in highly confirmative of intra-abdominal injury, for which emergent surgical management is indicated. However, a negative FAST cannot with sufficient diagnostic confidence, rule out intra-abdominal injury. The results of FAST should be considered in conjunction with clinical signs and relevant patient information. Patients with a negative FAST result should continue to be observed clinically, evaluated with serial FAST examinations or CT-scan should intra-abdominal injury be suspected. Developing technologies in Ultrasonography yield promising improvements to the FAST examination but current literature offers no evidence that FAST should replace CT as the diagnostic standard for BAT or its ability to definitively determine the necessity of immediate surgical management.
For more information about Article : https://ijclinmedcasereports.com/
https://ijclinmedcasereports.com/ijcmcr-ra-id-00152/
https://ijclinmedcasereports.com/pdf/IJCMCR-RA-00152.pdf
#Focused Assessment for Sonography#FAST#E-FAST#Ultrasonography#Point Of Care Ultrasound#Pocus#Blunt Abdominal Trauma#Laparotomy and CT#Lateef F*#IJCMCR#clinical studies
0 notes
Text
Unhinged battlefield surgeon reader and the extended metaphor of surgery as the most intimate form of love (with medical inaccuracies).
ghost/reader
-
Ghost got shot and his shredded kevlar had swallowed most of the shrapnel.
Though one bullet, thankfully, ate a way through and wedged itself in his abdomen.
He’s the only member of the task force you haven’t operated on. Always a little too tactically inclined and apt for your liking. Never with any grave injuries—just a ruddy bullet graze or a broken femur—neither of which you could get your hands on.
Surgery was the only way he would ever notice you. When Soap was in post-op, gauzed and inebriated on painkillers, Ghost reverently nodded at you in thanks. When Gaz got shot and you coordinated a walking blood bank, gingerly asking Ghost if his blood type was a match. It wasn’t, but you already knew that, because his personnel file was a parsed-over sheet branded into your brain—but he leaned down, the fleece of his balaclava grazing the husk of your ear, and asked you to repeat your question.
“Type one SGW,” someone says. A less-experienced medic, your subordinate, his first time downrange. Ashy and blanched in the face as he straps Ghost to a stretcher. “Signs of peritonitis are present.”
You’re already wearing your gloves, splitting a hand on Ghost’s chest. His breaths are irregular and short-winded under your palm, turbulent, like a second heartbeat.
You take a moment to grasp the papery flutter of his eyelashes against his mottled skin. It’s lace-like and scythe-like, disappearing under the crude shell of his macabre mask. And upon your excited fingers catching on the hem of his balaclava, the baby-faced medic stops you with a hand bent around your wrist.
“His face,” he slips an eighteen-gauge needle into Ghost’s bulging forearm. “That's not confidential?”
Irritation threatens to supersede your anticipation. You shrug his hand off of you, snarling, “I need to BVM him. Would you rather he die?”
The medic’s eyes widen. He sputters out apologies, mousy, and shuffles back. Busies himself with something else within the babel of organised chaos and medevac.
The pads of your fingers idle under the lip of Ghost’s balaclava. Slowly, you peel off his mask and feel your soul get eclipsed. He steals your breath, flips your world, and drenches you in ice-cold water. He’s beautiful in a way so specifically masculine. His face striated with lesions and gossamer-like scars, one running through his mouth and hefting up his upper lip, travelling towards his cropped hairline. Disappearing into his awkward cowlick.
Ghost’s hair is trimmed to his skull. There’s slivers of skin peeking through nicks and notches as a result of shaving himself over a ceramic sink. His breath struggles past his thin lips, puckering them. His eyes oscillate under his eyelids, his crows feet leathery and creased.
“Doctor,” another medic says, calling for your attention. “How should we proceed?”
You place an ambu bag on Ghost’s face. Your fingers on his dimpled jawbone, your other hand pumping air into his lungs. It’s electric. You’re giving him life, you’re his God, you’re swelling his lungs like a second-hand kiss too taboo to be direct. “Any exit wounds?”
Ghost gets turned onto his side and has his shirt torn through. You subsist on the heat that pools under your cheeks, sticking your thighs together. His blood congeals into the spindly hairs of his chest, thickening as it disappears below his pants. The other surgeons flit their eyes over the sinews of his back, answering, “No.”
It shouldn’t excite you. Really, it shouldn’t. But the thought of being inside Ghost—of coalescing with him, of being closer to him than anyone ever before—it excites you. For once, you’re not invisible to Ghost. For once, he’s at your mercy. On your table and bleeding out. In need of your deft hands, in need of your attention.
“I’m doing a laparotomy.”
“But–”
“That wasn’t a question.”
A scalpel is quickly dropped in your hand. You use it to dig a divot in Ghost’s skin, slicing a transverse incision that opens him up and spills him onto your hands. You cut through his cutis and off-white subcutis, slicing his abdomen wall, the fibrous sheet of tissue. Blood leaks out of him how rain dribbles down a window. Pearlescent and beady.
“Gimme suction,” you mumble. “And keep it out of my way. I’m removing the bullet.”
Off the fringes of your vision, the other surgeons exchange wary glances. Any protests they have rot on their tongue, stuck under the boot of their chief resident. A tinny, thin sound peals out in the heli, the clang of you throwing your scalpel into the kidney dish.
Gently, as if you’re holding glass, you slip your fingers into Ghost and slowly spread him open. It’s intoxicating. As if you’re splitting a mango open with your thumbs, the blood of it sluicing down your arms. Sweet and sticky. There’s a grotesque sound emanating from it—like when boots press in on a muddy ground. Ghost is all slippery and rubbery as your fingers search for a hot, eroded bullet.
“Any luck, Doctor?”
Your hands catch on gilded metal. You grasp it and pull yourself out, toss it in the kidney dish. You’re handed another instrument and start slice-wise swishes, closing him up. Sewing him back together like your own doll. His chest shudders under your fingers, rattling like wind-chimes. Your sutures are deep-seated and tight, strung out, because you don’t want to stop touching him. Because if you stop, he might unfurl again. Fall all over the place. Over the floor and over your pants and you can’t have that happen—you need Ghost full, thanking you properly for your work when he wakes up.
You’re finished, rubbing your ichor-stained gloves together. You still feel the phantom layer of your hands under Ghost’s skin.
It’s so intimate—holding him and piecing him back together. Carefully, attentively, lovingly.
#simon ghost riley#simon riley x reader#cod mw2#simon riley#simon ghost x reader#cod x reader#ghost x reader#ghost/reader#simon ghost x you#simon riley/reader#simon writing#writing
329 notes
·
View notes
Text
the worst thing about love is… | jason todd (chapter 1)
you’re just trying to get through your surgical residency, but this masked vigilante keeps showing up half-dead on your fire escape and reminding you of your dead best friend. oh well, at least he's cute.
tw: stitches, mentions of blood and injuries, swearing, completely ooc Jason but he’s like my own lil character now and I’m protective, very inaccurate medical terminology and procedure lol
only jerks steal other people's writing (just don't repost, mate)

There’s a dead man on your fire escape.
Well. He’s not actually dead, but his pulse is weak when you drag him into your living room, out of the relentless Gotham rain. Pulling your hand away from under his mask, you crouch down, peeling off the worn leather jacket around his shoulders and unbuckling his pauldrons. You feel around his back, brows furrowed. You can’t feel anything through the padding in his rain soaked shirt.
Hands wandering down to where his front is flat on the floor, you press down on his side, eyes widening when your fingers come back slick with blood. You go into autopilot, flipping him onto his back and yanking up his compression shirt. You might’ve gasped at the knife wound if you weren’t working on instinct. It’s bad.
Shoving away the doubt clawing at the base of your skull, you steady your trembling hands. You’ve been trained for this.
Don’t feel, just do.
The cut is long and serrated, and deep as all hell. It slices through the middle of a jagged, Y-shaped scar that chains over his shoulders like a noose. Jesus.
It’s like he was stabbed and then dragged across the floor, cutting diagonally across his torso. How is he even still alive? Your hands move faster than you can think, completing an internal checklist as you go.
Breathing? Fast and shallow through his modulator, no obstructions. Bleeding? Applied tourniquet to epigastric region - transfusion isn’t even an option… Your brain works overtime, sifting through diagnostics lectures - penetrating abdominal trauma, debrided of devitalised tissue, no visible debris… You trace the edges of the wound looking for inflammation or fluid buildup; signs of peritonitis, but the weapon seems to have missed any internal organs. Lucky. Even luckier that he landed on a surgical resident’s fire escape.
Reaching over to the lamp by your couch, you shift it so that it shines directly over his abdomen. A last check of his wound confirms that there are no external indications that you should conduct a laparotomy. You just have to sew him up and hope to god the knife didn’t puncture anything internal.
You keep a hand planted firmly over his tourniquet, applying constant pressure, reaching for your backpack. Dragging it over, you use your teeth to open your suture kit and your free hand to sterilise his cut with Betadine and alcohol, wiping gentle circles outward from the wound. You dip your needle like Achilles in the Styx, hand and all, into the sterilising liquid, tugging a glove on with your teeth.
You grip the needle driver in your dominant hand, pickups clutched in the other and take a steadying breath. There’s a stillness to the room, quiet save for your heartbeat pounding in your ears. The wound is large - high tension - so… mattress sutures… horizontal so the tension is spread over the edge of the wound.
You take your first bite, adrenaline driving your needle into a clean stitch. You reverse it, passing through his cut again, before tying it off with the practised motions of a thousand surgical knots tied on yarn and thread and fraying jeans. You settle back on your knees after the first suture, readying yourself for the stitching to come, and start the next one.
~
Hours later, you haul him onto your couch, sitting him up on the arm rest to take pressure off of his dressed stitches. Frowning deeply at how uncomfortable he looks - even unconscious, you tuck a throw pillow under his scuffed metal mask.
Leaning close to check his breathing, you hear crackling slow and deep through the helmet’s voice modulator. Bone-deep relief floods your system, a little sigh leaving your mouth involuntarily. Sitting heavily against your coffee table, you press the heels of your hands into your weary eyes.
He’s stable. For now at least.
Head bumping against the edge of your couch, you breathe in deeply, fighting the anxiety twisting in your ribcage. The couch smells like rubbing alcohol, stinging your nose so badly your eyes water. It’s followed by something familiar - underneath the heady scent of petrol and metal - like… if you mixed Gotham up into a single smell; rain and smoke and wet pavement. He… he smells like-
“Jay!”
The faulty fluorescent lights - courtesy of your parent's small family diner - seem to flicker in tandem with your strident yell.
Your best friend looks up at you through a mop of dark hair, collarbones poking out of his thin t-shirt, second-hand leather jacket chucked haphazardly on the other side of the booth. He’s stolen your copy of Jane Eyre, flattened with one hand next to a plate of old fries you’d scrounged for him.
You tug your book from his grasp, tucking your pen into the pocket on your apron. He looks up at you with a mouth full of fries, infuriating confusion written across his face.
“What? You promised I could read it.” You sigh in exasperation.
“When I’m finished! And-” A dramatic gasp rips from your mouth when you examine the book. “Are these- grease stains?” You take the book in both hands, swatting Jason with it.
“What so it’s okay to hit me with a book but not get grease- fuck, jesus, okay, okay!” You raise the book over your shoulder with both hands.
“Do you yield?” His mock-angry expression almost makes you laugh, a hand held up near his face to shield from your attack. There’s a soft twist to his frown, like he’s trying to stop his mouth from pulling into a grin. He raises his hands in surrender, and you relax your hold on the book.
Rookie mistake.
Jason darts forward, faster than you can blink, grasping your waist with both hands and dragging you towards him. He yanks the book from your hands and lets you go, grinning childishly at you with the book in his hands. The cat with the canary.
You throw your hands up in exasperation before planting them on your hips like a disappointed mother. The admonishment on the tip of your tongue turns into a weary sigh when you hear your parents calling for you from the diner kitchen. “Fine. But you actually have to try to not spoil it this time.”
Jason crosses his fingers over his chest, “Scout’s honour, birdie.”
You try not to flush at the nickname, just like you do every time he says it. Still, you fold like a stack of cards.
(He spoils it the next day.)
~
When you wake two hours later for rounds (at the ass-crack of dawn), he’s already gone. You pad quietly around your kitchen making coffee from day-old grounds, cautious not to disturb the sanctity of the early morning (or the ghost of his presence).
The only evidence of him is alight in the dim light that spills over your kitchen counter and into your living room - the deep indents in your couch and the bloodstains on your carpet… The rain on your wood floors, from the fire escape window you’re sure you didn’t leave open.

hi, hello, uhh this is the first fic I've ever posted so bear with me. if anyone actually sees this, i do apologise for the inaccuracies and lengthy prose. also, this will be a series so stick around if you like slow updates, slowburn and second chances. thanks for reading my rambles.
with love, bugsy
#series: the worst thing about love#love-bugsy#jason todd x reader#jason todd fic#jason todd fanfiction#jason todd reader insert#jason todd imagine#x reader
220 notes
·
View notes