Text
Unraveling the Surge: Syphilis Epidemics in Canada
Syphilis, a sexually transmitted infection once believed to be under control, is making a concerning resurgence across Canada. We'll attempt to examine the recent uptick in syphilis rates, the factors contributing to this increase, and the strategies being explored to curb the epidemic. We'll draw insights from several key research articles that shed light on the situation.
The Resurgence of Syphilis in Canada
Aho et al. (2022) provide a comprehensive overview of the rising syphilis rates in Canada from 2011 to 2020. Their research explores the epidemiology of the disease, highlighting the troubling trend of increasing syphilis cases. The highest increases are seen in the Prairie provinces, and rates among females, particularly among females aged 15-39, have been increasing at a much higher rate than among males. In addition, there has been an increase in early congenital syphilis cases. Syphilis can have serious health consequences and can be transmitted to the fetus during pregnancy. While the proportion of cases among gay, bisexual, and other men who have sex with men has decreased, they still represent a significant portion of cases. Social and structural determinants of health contribute to the inequitable occurrence of syphilis. More research is needed to understand the reasons behind these changes. The article serves as a critical starting point for understanding the scale of the issue in the country.
Spatial Epidemiology of the Syphilis Epidemic in Toronto
The study by Gesink et al. (2014) hones in on Toronto, Canada's largest city, to explore the spatial epidemiology of the syphilis epidemic. The research delves into the geographic distribution of syphilis cases, shedding light on localized hotspots of infection. The study suggests that peripheral sexual networks may be influencing the high syphilis infection rates. This geographical perspective is vital for tailoring targeted interventions.
The Impact of Screening Coverage on Syphilis Infection Dynamics
Tuite and Fisman (2016) investigate the role of screening coverage in shaping the dynamics of syphilis infections. Their research emphasizes the importance of screening as a key component of control strategies. The research found that screening for syphilis in urban men who have sex with men is crucial for controlling transmission, with an annual screening coverage of 20-30% resulting in the highest equilibrium incidence of syphilis. For local elimination, an optimal annual population-wide screening coverage of 62% would be needed, with 6-monthly or 3-monthly screening reducing the required coverage. The article highlights that achieving higher screening coverage can lead to a significant reduction in infection rates.
Using Mathematical Models to Inform Syphilis Control Strategies
Mathematical modeling is a valuable tool in shaping control strategies. Tuite, Fisman, and Mishra (2013) employ mathematical models to inform syphilis control strategies. Their work delves into the balance between the frequency of screening and the population covered, providing insights into the most effective screening strategies to mitigate the epidemic. The research found that increasing the frequency of syphilis screening to every three months was found to be the most effective strategy in reducing reported and incident syphilis infections among men who have sex with men (MSM).
--
The resurgence of syphilis in Canada is a complex issue that demands a multifaceted response. The research articles highlighted in this blog post underscore the need for comprehensive strategies that encompass surveillance, screening, geographic targeting, and mathematical modelling to control the epidemic effectively.
To combat the rising syphilis rates in Canada, it is imperative to consider a holistic approach. This approach includes not only increasing screening coverage but also engaging in education, community outreach, and comprehensive public health campaigns. The collaboration of healthcare providers, policymakers, and the affected communities is essential in the battle against syphilis.
While the resurgence of syphilis is a concerning trend, the insights and research provided in these articles offer hope and guidance for a more effective response. By employing these strategies and continuously monitoring the situation, Canada can work towards halting the spread of syphilis and protecting the sexual health of its citizens.
References!
Aho, J., Lybeck, C., Tetteh, A., Issa, C., Kouyoumdjian, F., Wong, J., Anderson, A., & Popovic, N. (2022). Rising syphilis rates in Canada, 2011–2020. Canada Communicable Disease Report, 48(23), 52–60. https://doi.org/10.14745/ccdr.v48i23a01
Gesink, D., Wang, S., Norwood, T., Sullivan, A., Al-Bargash, D., & Shahin, R. (2014). Spatial Epidemiology of the Syphilis Epidemic in Toronto, Canada. Sexually Transmitted Diseases, 41(11), 637–648.
Tuite, A., & Fisman, D. (2016). Go big or go home: Impact of screening coverage on syphilis infection dynamics. Sexually Transmitted Infections, 92(1), 49–54. https://doi.org/10.1136/sextrans-2014-052001
Tuite, A. R., Fisman, D. N., & Mishra, S. (2013). Screen more or screen more often? Using mathematical models to inform syphilis control strategies. BMC Public Health, 13(1), 606. https://doi.org/10.1186/1471-2458-13-606
#medical anthropology#anthropology#global health#medicine#scientific literacy#syphilis#syphilis in canada#canadian health#canadian healthcare#public health#STD#STDs in Canada#STD awareness
0 notes
Text
The Complex Web of HIV/AIDS in Sub-Saharan Africa: A Multidimensional Perspective
Sub-Saharan Africa has long been at the forefront of the global battle against HIV/AIDS. The region carries a significant burden of the virus, with a complex web of social, cultural, and geographical factors impacting the epidemic. The multifaceted nature of HIV/AIDS in Sub-Saharan Africa will be explored in this blog post, drawing insights from recent research articles that provide valuable perspectives on various aspects of the issue.
Tackling AIDS-Related Stigma: The Role of Church Groups
In the quest to address HIV/AIDS in Sub-Saharan Africa, a critical aspect is the reduction of AIDS-related stigma. Campbell, Skovdal, and Gibbs (2011) examine the role of church groups in creating social spaces to combat stigma. These groups play an essential role in providing support, raising awareness, and fostering acceptance, illustrating the power of community-driven efforts in the fight against HIV/AIDS. Nonetheless, more research is needed to understand why some churches are more effective than others in responding to HIV/AIDS.
The Geographical Understanding of HIV/AIDS
Mayer (2005) delves into the geographical aspect of HIV/AIDS in Sub-Saharan Africa. Understanding the spatial distribution of the virus is crucial for effective resource allocation, intervention planning, and targeted healthcare delivery. Research has shown that migrant labourers, truckers, and the Ugandan military have played a role in spreading the disease. Gender inequalities and the epidemic's impact on orphans are also significant issues. This research emphasizes the importance of a location-specific approach to combat the epidemic.
Stigma of People with HIV/AIDS: A Literature Review
Stigmatization of individuals with HIV/AIDS is a persistent issue in Sub-Saharan Africa. Mbonu, van den Borne, and De Vries (2009) conducted a comprehensive literature review to shed light on the stigma faced by those affected by the virus and the current research on the topic of stigma related to HIV/AIDS in Sub-Saharan Africa. This research highlights the urgency of reducing stigma to enhance care and support for individuals living with HIV/AIDS.
Gender and HIV/AIDS Impact Mitigation
Seeley, Grellier, and Barnett (2004) explore the gender dimension of HIV/AIDS in Sub-Saharan Africa. The research recognizes the unique challenges faced by women in the context of the epidemic and emphasizes the need for gender-sensitive interventions. It highlights gender-specific constraints such as access to resources, services, markets, and the incidence of gendered violence. The differential involvement of men and women in development programs also affects access to resources. Addressing these constraints is vital for reducing the impact of HIV/AIDS on women in the region.
HIV/AIDS and the Construction of Sub-Saharan Africa
Yeboah (2007) offers heuristic lessons from the social sciences for policy formulation in Sub-Saharan Africa. The article emphasizes the importance of multidisciplinary approaches in understanding the complex dynamics of the epidemic and in developing effective policies to combat HIV/AIDS. The article presents an argument that the Eurocentric construction of the region has hindered a comprehensive understanding of the virus and its impact.
--
HIV/AIDS in Sub-Saharan Africa is a complex issue with multiple dimensions. To combat the epidemic effectively, a multidisciplinary approach is essential, drawing upon research in social sciences, geography, and public health. Addressing AIDS-related stigma, understanding the geographical distribution of the virus, recognizing gender-specific constraints, and involving local communities and religious groups are all critical aspects of the battle against HIV/AIDS.
While progress has been made, much work remains to be done in the region. The fight against HIV/AIDS in Sub-Saharan Africa requires a multifaceted strategy, collaboration, and an unwavering commitment to reducing the impact of the virus on individuals and communities. By taking a holistic approach, we can work towards a future where HIV/AIDS is no longer a devastating burden in Sub-Saharan Africa.
References!
Campbell, C., Skovdal, M., & Gibbs, A. (2011). Creating Social Spaces to Tackle AIDS-Related Stigma: Reviewing the Role of Church Groups in Sub-Saharan Africa. AIDS and Behavior, 15(6), 1204–1219. https://doi.org/10.1007/s10461-010-9766-0
Mayer, J. D. (2005). The geographical understanding of HIV/AIDS in sub-Saharan Africa. Norsk Geografisk Tidsskrift - Norwegian Journal of Geography, 59(1), 6–13. https://doi.org/10.1080/00291950510020493
Mbonu, N. C., van den Borne, B., & De Vries, N. K. (2009). Stigma of People with HIV/AIDS in Sub-Saharan Africa: A Literature Review. Journal of Tropical Medicine, 2009, e145891. https://doi.org/10.1155/2009/145891
Seeley, J., Grellier, R., & Barnett, T. (2004). Gender and HIV/AIDS impact mitigation in sub-Saharan Africa—Recognising the constraints. SAHARA-J: Journal of Social Aspects of HIV/AIDS, 1(2), 87–98. https://doi.org/10.1080/17290376.2004.9724831
Yeboah, I. E. A. (2007). HIV/AIDS and the construction of Sub-Saharan Africa: Heuristic lessons from the social sciences for policy. Social Science & Medicine, 64(5), 1128–1150. https://doi.org/10.1016/j.socscimed.2006.10.003
#medical anthropology#anthropology#global health#medicine#scientific literacy#HIV#AIDS#HIV/AIDS#sub saharan africa#healthcare#culturally sensitive
0 notes
Text
Fostering Indigenous Health: A Journey Towards Culturally Safe Care in Canada
The health and well-being of Indigenous communities in Canada have been a longstanding concern. These communities face unique challenges related to healthcare access, cultural safety, and the interplay of social determinants of health. In this blog post, the state of Indigenous health in Canada will be explored, drawing insights from recent research studies that shed light on the importance of culturally safe care and community-driven interventions
Culturally Safe Health Initiatives for Indigenous Peoples
A scoping review conducted by Brooks-Cleator, Phillipps, and Giles in 2018 delves into the concept of culturally safe health initiatives for Indigenous peoples in Canada. The study underscores the significance of culturally tailored healthcare, respecting and honoring the unique cultural and historical aspects of Indigenous communities. This approach acknowledges the importance of addressing healthcare disparities while fostering trust and collaboration.
Enhancing Health through Indigenous Culturally-Based Interventions
The research by Murdoch-Flowers, Tremblay, and colleagues in 2019 explores the positive impact of Indigenous culturally-based interventions on participants' health in Canada (through various interventions focused on traditional cooking, physical activity, mind-focusing techniques, cultural traditions, and social interaction). By integrating cultural traditions and practices into healthcare, these interventions provide a holistic approach to health improvement. Culturally-based interventions, including the involvement of lay health workers and the promotion of cultural identity, have been found to improve participants' social dimension of health. The study emphasizes that interventions rooted in Indigenous culture have the potential to make a meaningful difference in health outcomes.
FORGE AHEAD Program: Community-Driven Quality Improvement
The FORGE AHEAD program, as described by Naqshbandi Hayward and colleagues in 2016, highlights the importance of community-driven quality improvement initiatives. This program empowers Indigenous communities to take charge of their healthcare and implement culturally sensitive strategies to enhance chronic disease care. It represents a promising shift towards self-determination and control over healthcare delivery and outcomes.
Indigenous Populations Health Protection: A Canadian Perspective
Richardson, Driedger, Pizzi, Wu, and Moghadas (2012) revealed that in the 2009 H1N1 pandemic, there was a disproportionate impact on Canadian Aboriginal communities, highlighting their vulnerability to infectious diseases, and a workshop was held to address the challenges and improve public health planning for these communities. The workshop emphasized the importance of involving Aboriginal stakeholders in policy-making and program delivery. The concept of "two-eyed seeing" was introduced, which combines indigenous and Western perspectives for the benefit of all. The research acknowledges that health disparities are deeply rooted in historical injustices, and addressing these disparities requires not only healthcare but also broader societal and policy changes. Indigenous health must be protected, supported, and elevated at all levels of Canadian society.
Challenges and the Path Forward
Indigenous health in Canada has long been characterized by challenges, including limited access to healthcare, disparities in health outcomes, and cultural insensitivity. However, the research presented in these studies paints a promising picture of positive change. The emphasis on culturally safe healthcare, community-driven initiatives, and the protection of Indigenous health demonstrates a growing commitment to rectify the historical injustices faced by Indigenous communities.
--
The journey towards improving Indigenous health in Canada involves a commitment to culturally safe care and community-driven solutions. It recognizes that health disparities in Indigenous communities are not solely a medical issue but are deeply intertwined with historical, cultural, and socio-economic factors. By acknowledging the importance of culture and community engagement, and by empowering Indigenous communities to take control of their healthcare, there is hope for a brighter, healthier future for Canada's Indigenous peoples. It is a path that requires collaboration, respect, and a deep commitment to reconciliation and equity.
References!
Brooks-Cleator, L., Phillipps, B., & Giles, A. (2018). Culturally Safe Health Initiatives for Indigenous Peoples in Canada: A Scoping Review. Canadian Journal of Nursing Research, 50(4), 202–213. https://doi.org/10.1177/0844562118770334
Murdoch-Flowers, J., Tremblay, M.-C., Hovey, R., Delormier, T., Gray-Donald, K., Delaronde, E., & Macaulay, A. C. (2019). Understanding how Indigenous culturally-based interventions can improve participants’ health in Canada. Health Promotion International, 34(1), 154–165. https://doi.org/10.1093/heapro/dax059
Naqshbandi Hayward, M., Paquette-Warren, J., Harris, S. B., & On behalf of the FORGE AHEAD Program Team. (2016). Developing community-driven quality improvement initiatives to enhance chronic disease care in Indigenous communities in Canada: The FORGE AHEAD program protocol. Health Research Policy and Systems, 14(1), 55. https://doi.org/10.1186/s12961-016-0127-y
Richardson, K. L., Driedger, M. S., Pizzi, N. J., Wu, J., & Moghadas, S. M. (2012). Indigenous populations health protection: A Canadian perspective. BMC Public Health, 12(1), 1098. https://doi.org/10.1186/1471-2458-12-1098
#medical anthropology#anthropology#global health#medicine#scientific literacy#indigenous health#indigenous health canada#public health#healthcare disparities#canadian healthcare#healthcare#inclusivity#culturally sensitive
1 note
·
View note
Text
Understanding the Unique Challenge of Type 2 Diabetes in South Asians!
Diabetes is a recognized global health concern, affecting millions of people around the world. However, certain populations are at a higher risk, and among them, South Asians stand out. Type 2 diabetes is a significant health issue for this group, with a higher prevalence and unique genetic and environmental factors contributing to their susceptibility. In this blog post, we will explore the complex relationship between South Asians and type 2 diabetes, drawing insights from recent research studies.
The Genetic Link: Insights from KCNQ1 Variants
One of the key factors contributing to the high prevalence of type 2 diabetes in South Asians is their genetic makeup. A study by Been et al. (2011) found that specific variants in the KCNQ1 gene increase susceptibility to type 2 diabetes in South Asians. The research, which involved 3,310 subjects from India and the US, highlighted the importance of genetics in understanding the risk factors for this group.
A Systematic Overview of Genetic Studies
Chowdhury et al. (2014) conducted a systematic overview of genetic studies related to type 2 diabetes in South Asians. Their research consolidated findings from various studies, shedding light on the complex genetic factors that contribute to diabetes susceptibility in this population. The study provides a comprehensive understanding of the genetic landscape of type 2 diabetes in South Asians.
South Asian Diabetes in a Global Context
Gujral et al. (2013) examined the similarities and differences between type 2 diabetes in South Asians and other populations, including white Caucasians. The research revealed the unique challenges faced by South Asians and how their genetic and environmental contexts influence the disease. Understanding these distinctions is essential for tailoring effective diabetes prevention and management strategies. The impact of past famines in a condensed period of time (specifically induced by colonialism during the 19th and 20th centuries) can also be argued to have shaped the South Asian epigenetic framework to hold onto fat in a comparatively different manner than white Caucasian counterparts.
Exploring Underexplored Pathways
Narayan and Kanaya (2020) proposed a hypothesis to answer the critical question: "Why are South Asians prone to type 2 diabetes?" They explored underexplored pathways that might contribute to the increased risk in this population. Their hypothesis opens new avenues for research and the development of targeted interventions.
The Role of Lifestyle and Socioeconomic Factors
Type 2 diabetes is not solely a genetic issue. Unnikrishnan, Gupta, and Mohan (2018) emphasized the significance of lifestyle and socioeconomic factors in understanding the phenotype, clinical presentation, and natural history of diabetes in South Asians. This comprehensive approach takes into account the broader context in which diabetes develops in this population.
The Urgency of Action
In their 2007 article, Patel and Bhopal highlighted the diabetes epidemic in the South Asian diaspora. The piece underscores the importance of taking action to address this growing health crisis. Early interventions and awareness are crucial to preventing further escalation of diabetes in the South Asian community.
--
The high prevalence of type 2 diabetes among South Asians is a multifaceted issue influenced by genetics, lifestyle, and socioeconomic factors. Research, such as the studies mentioned in this blog post, helps shed light on the complexities of this disease in this population. By understanding the unique context of South Asians, we can develop more effective strategies for prevention and management, ultimately reducing the burden of type 2 diabetes in this at-risk group. This is a topic I'm incredibly interested in researching and will probably write more about in future posts!
References!
Been, L. F., Ralhan, S., Wander, G. S., Mehra, N. K., Singh, J., Mulvihill, J. J., Aston, C. E., & Sanghera, D. K. (2011). Variants in KCNQ1 increase type II diabetes susceptibility in South Asians: A study of 3,310 subjects from India and the US. BMC Medical Genetics, 12(1), 18. https://doi.org/10.1186/1471-2350-12-18
Chowdhury, R., M. Venkat Narayan, K., Zabetian, A., Raj, S., & Tabassum, R. (2014). Genetic Studies of Type 2 Diabetes in South Asians: A Systematic Overview. Current Diabetes Reviews, 10(4), 258–274.
Gujral, U. P., Pradeepa, R., Weber, M. B., Narayan, K. M. V., & Mohan, V. (2013). Type 2 diabetes in South Asians: Similarities and differences with white Caucasian and other populations. Annals of the New York Academy of Sciences, 1281(1), 51–63. https://doi.org/10.1111/j.1749-6632.2012.06838.x
Narayan, K. M. V., & Kanaya, A. M. (2020). Why are South Asians prone to type 2 diabetes? A hypothesis based on underexplored pathways. Diabetologia, 63(6), 1103–1109. https://doi.org/10.1007/s00125-020-05132-5
Patel, K. C. R., & Bhopal, R. (2007). Diabetes epidemic in the South Asian Diaspora: Action before desperation. Journal of the Royal Society of Medicine, 100(3), 115–116. https://doi.org/10.1177/014107680710000303
Unnikrishnan, R., Gupta, P. K., & Mohan, V. (2018). Diabetes in South Asians: Phenotype, Clinical Presentation, and Natural History. Current Diabetes Reports, 18(6), 30. https://doi.org/10.1007/s11892-018-1002-8
#medical anthropology#anthropology#global health#medicine#scientific literacy#diabetes#diabetes type 2#diabetes type II#south asians#epigenetics#medicine and history#diabetes mellitus
0 notes
Text
Debunking the Romanticization of the Medical Field: Unveiling the Reality of a Doctor's Career
The medical field has long been a subject of romanticization in popular culture, often depicted as an extraordinary and noble profession. From iconic television shows like "Grey's Anatomy" to heartwarming movies that highlight doctors as heroes, society has become accustomed to an idealized image of the medical profession. However, it is crucial to recognize that this portrayal often misrepresents the realities of being a doctor and overlooks the challenges, sacrifices, and complexities that come with the profession.
One of the primary misconceptions perpetuated by the romanticization of the medical field is the notion of glamour. The media tends to focus on the adrenaline rush of emergency rooms, the portrayal of doctors as constantly saving lives, and the extravagant lifestyles they supposedly lead. While it is true that medical professionals experience moments of triumph, these moments are often overshadowed by the countless hours of hard work, dedication, and immense pressure that comes with the job.
Another aspect that is often ignored in the romanticized portrayal is the toll that a medical career can take on an individual's mental and physical well-being. Doctors face long and grueling work hours, often stretching far beyond the standard 40-hour workweek. The constant exposure to human suffering, traumatic events, and the responsibility of making life-or-death decisions can lead to high levels of stress, anxiety, and even burnout. The pressure to maintain a perfect work-life balance can be overwhelming, with many doctors sacrificing personal relationships and time for self-care.
Contrary to the glorified depiction of doctors as infallible and all-knowing, the reality is that they are humans who face limitations and challenges. While medical professionals strive to provide the best care possible, they are not immune to mistakes or the limitations of medical science. Coping with patient loss, dealing with the emotional weight of delivering difficult news, and making tough ethical decisions are all part of a doctor's reality that is often overlooked in the romanticized portrayal.
The depiction of doctors enjoying lavish lifestyles and exorbitant incomes is another misleading aspect perpetuated by the romanticization of the medical field. While doctors can earn comfortable salaries, the years of extensive education, student loan debt, and the costs associated with running a medical practice often eat into those earnings. Moreover, the increasing complexity of the healthcare system and the administrative burdens can detract from the core practice of medicine, leading to frustration and financial strain.
It is essential to move beyond the romanticized portrayal of the medical field and acknowledge the reality faced by doctors. While the profession can be immensely rewarding, it is not without its challenges, sacrifices, and limitations. By shedding light on the true complexities of a doctor's career, we can encourage a more realistic understanding and appreciation for the incredible work done by medical professionals. It is crucial that aspiring doctors, as well as the general public, understand the realities of the medical field to make informed decisions and support those who dedicate their lives to healing and saving others.
#medical anthropology#anthropology#global health#medicine#scientific literacy#medical career#heatlhcare#doctor#physician#surgeon#medical drama
0 notes
Text
Unveiling the Health Impacts of Climate Change: Insights from Medical Anthropology
Climate change poses significant challenges to human health, affecting communities worldwide. In this blog post, we explore the impact of climate change on health through the lens of medical anthropology, drawing insights from the book "Understanding and Applying Medical Anthropology" edited by Brown and Closser (2016). This interdisciplinary field provides valuable perspectives on the complex interactions between climate change, culture, and health. Let's delve into some key points from the book, showcasing the interplay of climate change and health outcomes:
1. Climate Change and Environmental Vulnerabilities:
Medical anthropology highlights how climate change exacerbates existing environmental vulnerabilities, disproportionately affecting marginalized communities. The book emphasizes that vulnerable populations, such as indigenous peoples and those living in poverty, often face heightened health risks due to environmental degradation and climate-related disasters. For example, rising temperatures and extreme weather events can disrupt access to clean water, leading to waterborne diseases and malnutrition, particularly in impoverished regions.
2. Cultural Perceptions and Adaptation:
Understanding cultural perceptions and beliefs is crucial in addressing the health impacts of climate change. Medical anthropology emphasizes the importance of recognizing diverse cultural perspectives and knowledge systems when designing interventions and policies. For instance, indigenous communities possess valuable traditional ecological knowledge that can inform climate change adaptation strategies. By incorporating indigenous wisdom into decision-making processes, it becomes possible to foster resilient and culturally appropriate responses to climate-related health challenges.
3. Mental Health and Climate-Induced Displacement:
Climate change-induced displacement and migration have profound effects on mental health and well-being. The book highlights how environmental disruptions, such as loss of livelihoods or forced relocation, contribute to psychological distress and trauma. Displaced populations may experience anxiety, depression, and post-traumatic stress disorder as they grapple with the loss of familiar environments, social support networks, and cultural identity. Examining these mental health impacts helps guide interventions that support psychological resilience and community healing.
4. Infectious Diseases and Ecological Transformations:
Climate change influences the distribution and transmission of infectious diseases, presenting complex challenges for public health. Medical anthropology recognizes the interconnections between ecological transformations and disease dynamics. For example, changing temperatures and precipitation patterns can alter vector habitats and increase the spread of vector-borne diseases such as malaria and dengue fever. Understanding these ecological complexities is vital for developing effective prevention and control strategies.
--
Medical anthropology offers valuable insights into the health impacts of climate change by examining the interplay between culture, environment, and health outcomes. From recognizing environmental vulnerabilities to understanding cultural perceptions and adapting interventions, this interdisciplinary field sheds light on the complexities of climate change and its implications for human well-being. By integrating diverse perspectives, including those of marginalized communities and indigenous knowledge systems, it becomes possible to design contextually relevant strategies for climate change adaptation and mitigation. Moreover, addressing the mental health consequences of climate-induced displacement and considering the ecological transformations that shape disease dynamics are crucial for comprehensive public health responses. Ultimately, by drawing on the principles and knowledge offered by medical anthropology, we can forge a path toward climate-resilient health systems, equitable interventions, and sustainable solutions that prioritize both human well-being and the health of our planet.
References!
Brown, P.J., & Closser, S. (Eds.). (2016). Understanding and Applying Medical Anthropology (3rd ed.). Routledge. https://doi.org/10.4324/9781315416175. -> (Highly recommend this read, even if its just a few chapters!)
#medical anthropology#anthropology#global health#medicine#climate change#global warming#healthcare#health#health outcomes#environmental impact#environment#future health
2 notes
·
View notes
Text
Fundal Pressure in Labor: Balancing Practice and Potential Risks
During labor, healthcare providers may employ various techniques to assist with the delivery process. One such technique is fundal pressure, which involves applying pressure on the upper abdomen to aid in the descent and expulsion of the baby. While fundal pressure has been used for decades, its effectiveness and potential risks have been the subject of debate. In this blog post, we will explore the main points from several studies and shed light on the practice of fundal pressure, its purpose, and the associated consequences.
Understanding the Practice and Prevalence:
A systematic review and meta-analysis conducted by Farrington et al. (2021) examined the prevalence of uterine fundal pressure during the second stage of labor. The study revealed that fundal pressure was utilized in a considerable number of cases, with variations observed across different regions and healthcare facilities. For instance, in some low- and middle-income countries, the use of fundal pressure was more prevalent compared to high-income countries, highlighting the influence of local protocols and traditions.
The Potential Effects and Consequences:
To assess the impact of fundal pressure, Buhimschi et al. (2002) conducted a study on intrauterine pressure during the second stage of labor. The research demonstrated that fundal pressure increased the intrauterine pressure significantly. While this might aid in fetal descent, it also raises concerns about potential adverse effects on maternal and fetal well-being. Excessive uterine pressure can lead to potential complications, including maternal perineal trauma, prolonged second stage of labor, and fetal distress, as highlighted by Pinar and Karaçam (2018).
The Call for Caution and Critical Appraisal:
Papadakis (2019) critically appraised the role of fundal pressure in labor, emphasizing the principle of "First, do no harm." The study highlighted the lack of scientific evidence supporting the routine use of fundal pressure, especially in cases where it is not medically indicated. Papadakis cautioned against the potential risks associated with fundal pressure and stressed the importance of individualized care and shared decision-making between healthcare providers and birthing individuals.
The Importance of Informed Decision-Making:
Fundal pressure should be employed cautiously and with a thorough understanding of the potential risks and benefits. Healthcare providers must engage in shared decision-making with birthing individuals, considering their unique circumstances and preferences. Informed consent and adherence to evidence-based practices are crucial in ensuring the well-being of both mother and baby during childbirth.
--
The practice of fundal pressure during labor continues to be a subject of debate in the medical community. While it is employed in certain circumstances to aid in the delivery process, there are potential risks and adverse consequences associated with its use. Healthcare providers must carefully consider the benefits and harms, taking into account the specific context of each laboring individual.
For example, in low-resource settings where alternative interventions may be limited, fundal pressure could be utilized judiciously to assist with delivery. However, in other cases, the routine use of fundal pressure without medical indication may pose unnecessary risks. Individualized care, shared decision-making, and critical appraisal of the available evidence are essential in ensuring the safety and well-being of birthing individuals and their infants.
As research continues to advance, it is crucial to critically evaluate the practice of fundal pressure and prioritize the principles of beneficence and non-maleficence in childbirth. By promoting informed decision-making and evidence-based practices, healthcare providers can navigate the complexities of fundal pressure and strive to optimize outcomes for both mothers and babies.
References!
Buhimschi, Catalin S., et al. "The effect of fundal pressure manoeuvre on intrauterine pressure in the second stage of labour." BJOG: an international journal of obstetrics and gynaecology 109.5 (2002): 520-526.
Farrington, Elise, et al. "The prevalence of uterine fundal pressure during the second stage of labour for women giving birth in health facilities: a systematic review and meta-analysis." Reproductive Health 18.1 (2021): 1-17.
Mahendru, Rajiv, Savita Malik, and Tina Anand. "Age old practice of Uterine Fundal Pressure in Labor-more risky than beneficial." Biomedical Research 21.3 (2010): 295-296.
Papadakis, Konstantinos. "Critical appraisal of the role of applying uterine fundal pressure in labour: First, do no harm." Hypertension Research in Pregnancy 7.1 (2019): 22-26.
Pinar, Semra, and Zekiye Karaçam. "Applying fundal pressure in the second stage of labour and its impact on mother and infant health." Health care for women international 39.1 (2018): 110-125.
#medical anthropology#anthropology#global health#medicine#fundal pressure#maternal health#neonatal health#obgyn#cultural practices#traditional practices#do no harm#pregnancy#childbirth#birth
0 notes
Text
The Crucial Role of Hygienic Practices in Medicine: Exploring Attitudes and Practices Worldwide
Hygienic practices, particularly hand hygiene, play a vital role in preventing the spread of infections in healthcare settings. However, the knowledge, attitudes, and practices surrounding hygiene can vary across different regions and educational institutions. In this blog post, we will examine the importance of hygienic practices in medicine and explore the similarities and differences in attitudes towards it, drawing insights from various studies conducted in India, Ghana, the USA and across South Asia.
In a study conducted by Nair et al. (2014) in India, medical and nursing students demonstrated a significant gap between their knowledge and practice of hand hygiene. While they acknowledged the importance of hand hygiene, barriers such as lack of time, inadequate facilities, and a perception of low infection risk hindered their optimal adherence to recommended hygiene practices. For example, despite being aware of hand hygiene protocols, the students often struggled to put them into practice due to time constraints and limited access to handwashing facilities.
Similarly, Odonkor et al. (2019) conducted a study among university students in Ghana to assess their hygiene practices. While the students showcased a positive attitude towards hygiene, there were gaps between their knowledge and actual practices, particularly regarding hand hygiene techniques and the use of personal protective equipment (PPE). For instance, despite recognizing the importance of hand hygiene, some students exhibited inconsistent adherence to proper handwashing techniques, potentially increasing the risk of infection transmission.
The influence of mentors on students' hygiene practices was explored in a study by Snow et al. (2006) in the USA. The research revealed that mentors who consistently practiced good hand hygiene positively influenced their students' adherence to hygiene protocols. By serving as role models, these mentors created a culture of hygiene, emphasizing its importance to their students. For example, when mentors consistently demonstrated proper hand hygiene techniques, their students were more likely to follow suit, leading to improved overall hygiene practices within the healthcare setting.
Examining hygiene practices during clinical training, Jayarajah et al. (2019) found variations among South Asian medical students. While the majority recognized the importance of hygiene, discrepancies in knowledge and adherence to recommended protocols were evident. This highlighted the need for standardized hygiene training programs and continuous reinforcement of best practices during clinical training. For instance, some students exhibited better hygiene practices when they received consistent training and reminders about the importance of hand hygiene and infection control measures.
Hygienic practices, especially hand hygiene, are vital in healthcare settings to prevent infections. The studies reviewed in this blog post emphasize the importance of addressing knowledge-practice gaps and fostering a culture of hygiene among healthcare students. By providing adequate resources, implementing standardized training programs, and promoting consistent role modeling, healthcare institutions can nurture positive attitudes and behaviors towards hygienic practices. For instance, in India, the barriers to hand hygiene faced by medical and nursing students can be addressed by improving facilities and incorporating time-efficient strategies for handwashing. In Ghana, bridging the gap between knowledge and practice can be achieved through targeted interventions that focus on practical skills training and raising awareness of proper hand hygiene techniques. In all settings, the influence of mentors in shaping students' attitudes and practices highlights the significance of strong leadership and role modelling. Ultimately, a collective commitment to hygiene is essential for safeguarding patient safety and improving healthcare outcomes worldwide. By fostering a culture of hygiene through education, mentorship, and adequate resources, we can promote effective hygienic practices in medicine and enhance the overall quality of healthcare delivery.
References!
Jayarajah, U., et al. "Hygiene practices during clinical training: knowledge, attitudes and practice among a cohort of South Asian Medical students." BMC medical education 19.1 (2019): 1-8.
Nair, Sreejith Sasidharan, et al. "Knowledge, attitude, and practice of hand hygiene among medical and nursing students at a tertiary health care centre in Raichur, India." International Scholarly Research Notices 2014 (2014).
Odonkor, Stephen T., et al. "Self-assessment of hygiene practices towards predictive and preventive medicine intervention: a case study of university students in Ghana." BioMed research international 2019 (2019).
Snow, Michelle, et al. "Mentor's hand hygiene practices influence student's hand hygiene rates." American journal of infection control 34.1 (2006): 18-24.
#medical anthropology#anthropology#global health#medicine#hygiene in medicine#hygiene practices#scientific literacy#standard practices
0 notes
Text
Looking at a Systematic Review of Environmental Risk Factors for Child Stunting
Child stunting, characterized by impaired growth and development, is a significant public health concern globally. While nutrition plays a crucial role, there are other environmental factors that contribute to this condition. In this blog post, we will delve into the findings of a systematic review conducted by Vilcins et al. (2018) to highlight the key environmental risk factors associated with child stunting. This research sheds light on the multifaceted nature of stunting, beyond nutritional aspects, and provides valuable insights for effective interventions.
Household Air Pollution:
The systematic review by Vilcins et al. emphasizes the impact of household air pollution on child stunting. Exposure to indoor air pollution from sources like solid fuel for cooking and heating, such as biomass or coal, can lead to respiratory infections and chronic inflammation. These conditions can impair a child's growth and development. For instance, in regions where solid fuel is commonly used, such as parts of Africa and Asia, children exposed to high levels of indoor air pollution have an increased risk of stunting.
2. Water, Sanitation, and Hygiene (WASH) Practices:
Inadequate access to clean water and sanitation facilities significantly contribute to child stunting. Vilcins et al. highlight how poor WASH practices, including limited access to clean water for drinking and hygiene, and inadequate sanitation facilities, increase the risk of infectious diseases and nutrient deficiencies. For example, in areas where open defecation is practiced, the risk of stunting is higher due to the increased likelihood of fecal-oral transmission of diseases like diarrhea and intestinal parasites.
3. Environmental Contaminants:
The presence of environmental contaminants, such as heavy metals and pesticides, is associated with child stunting. Exposure to these pollutants, either through contaminated soil, water, or food, can interfere with a child's growth and development. For instance, in agricultural communities where pesticides are extensively used, children may be exposed to these harmful substances, which can impair their cognitive development and contribute to stunting.
4. Poor Housing Conditions:
Inadequate housing conditions, including overcrowding, lack of ventilation, and dampness, are identified as risk factors for child stunting. These conditions increase the likelihood of respiratory infections, which can impact a child's nutritional status and growth. For example, in slum areas with crowded living spaces and insufficient ventilation, children are more susceptible to respiratory illnesses, leading to stunting.
Vilcins et al.'s systematic review highlights the environmental risk factors associated with child stunting beyond nutritional aspects. Household air pollution, poor WASH practices, exposure to environmental contaminants, and inadequate housing conditions all contribute to stunting. Addressing these factors requires comprehensive interventions that improve access to clean energy, promote proper WASH practices, reduce environmental pollution, and enhance housing conditions. By understanding and addressing the environmental risk factors associated with child stunting, policymakers, health professionals, and communities can work together to develop effective strategies for prevention and intervention. It is through targeted actions and investments in improving environmental conditions that we can reduce child stunting rates and ensure healthier futures for children worldwide.
References!
Vilcins, Dwan, Peter D. Sly, and Paul Jagals. "Environmental risk factors associated with child stunting: a systematic review of the literature." Annals of global health 84.4 (2018): 551.
#medical anthropology#medicine#global health#global medicine#child stunting#paediatrics#social determinants#systemic review#anthropology#scientific literacy#environmental factors
2 notes
·
View notes
Text
Looking Critically at the Impact of Social Determinants on Indigenous Health
Indigenous communities worldwide face alarming health disparities compared to non-Indigenous populations. These disparities are not coincidental; they are intricately tied to a complex web of social determinants of health. In this blog post, we will explore the significant influence of social determinants on the health outcomes of Indigenous peoples, as highlighted by insightful studies conducted by Reading and Wien (2009), George et al. (2019), and Greenwood and de Leeuw (2012).
Reading and Wien's (2009) study sheds light on the health inequalities experienced by Aboriginal peoples. For example, they highlight the impact of colonization on cultural continuity, which affects the mental and emotional well-being of Indigenous communities. The study also emphasizes the influence of socioeconomic factors, such as poverty and limited access to healthcare, in perpetuating health disparities among Indigenous populations. George et al. (2019) conducted a scoping review analyzing problem representation regarding Indigenous health and Indigenous rights in policy. They found that social determinants, such as education and employment, play a crucial role in shaping the health outcomes of Indigenous peoples. For instance, limited educational opportunities can contribute to a higher prevalence of chronic diseases and lower overall health status within Indigenous communities. Inadequate access to employment opportunities further exacerbates these disparities. Greenwood and de Leeuw's (2012) study focuses on the social determinants impacting the well-being of Aboriginal children in Canada. The authors highlight the importance of income and education in shaping health outcomes. For instance, lower household income often limits access to nutritious food and safe housing, leading to increased rates of malnutrition and respiratory illnesses among Indigenous children. Additionally, limited educational resources can hinder academic achievement and future employment prospects, further impacting health and well-being.
The studies reviewed in this blog post provide valuable examples of how social determinants significantly influence Indigenous health. From the impact of colonization on cultural continuity to the role of education and employment opportunities, these determinants shape health outcomes within Indigenous communities. Recognizing and addressing these factors is crucial for reducing health disparities and promoting the well-being of Indigenous populations. Achieving health equity for all requires a comprehensive approach that considers the social determinants of health. By implementing policies and interventions that address issues such as poverty, access to education, employment opportunities, and cultural preservation, we can make meaningful strides in improving the health outcomes of Indigenous peoples. It is through collective efforts, informed by research and guided by social justice, that we can work towards a healthier future for Indigenous communities worldwide.
References!
George, Emma, et al. "Social determinants of Indigenous health and Indigenous rights in policy: A scoping review and analysis of problem representation." International Indigenous Policy Journal 10.2 (2019): 4.
Greenwood, Margo Lianne, and Sarah Naomi de Leeuw. "Social determinants of health and the future well-being of Aboriginal children in Canada." Paediatrics & child health 17.7 (2012): 381-384.
Reading, Charlotte Loppie, and Fred Wien. "Health inequalities and the social determinants of Aboriginal peoples' health." (2009).
#medical anthropology#anthropology#indigenous health#indigenous health canada#intersectionality#healthcare#healthcare disparities#global health#scientific literacy#social determinants
1 note
·
View note
Text
This article is super interesting in better understanding determinants of health in a Canadian-specific context (or in a broader application to a developed region). The article investigates intersectionality to better understand and respond to the ‘foundational’ causes of illness and disease. The analysis highlights the current limitations on the methods of acknowledging health determinants (such as gender, social, political and economic conditions). The intersectional paradigm offers an approach to better understand social determinants of health and embrace the complexities that are crucial in recognizing inequalities.
#medical anthropology#medicine#public health#canadian healthcare#sociology#anthropology#health#global health#health inequalities
0 notes
Link
A team of Florida International University (FIU) drug development scientists has found a possible new way to counteract the effects of the disease that turns bones into honeycomb-like structures—so fragile even a cough can cause a fracture or break. The discovery, recently published in Communications Biology, is the first step toward cheaper, effective, easy-to-take treatments for osteoporosis and other diseases associated with bone loss.
Currently available drugs only stop bone loss and require expensive daily injections. Researchers from FIU’s Herbert Wertheim College of Medicine—along with a collaborative team from the National Center for Advancing Translational Sciences (NCATS), part of the National Institutes of Health (NIH), and University of Arkansas for Medical Sciences—identified a method that can be taken orally and helps bone-producing cells make more bone.
Continue Reading
135 notes
·
View notes
Text
Super cool article linked with a brief summary listed above!!
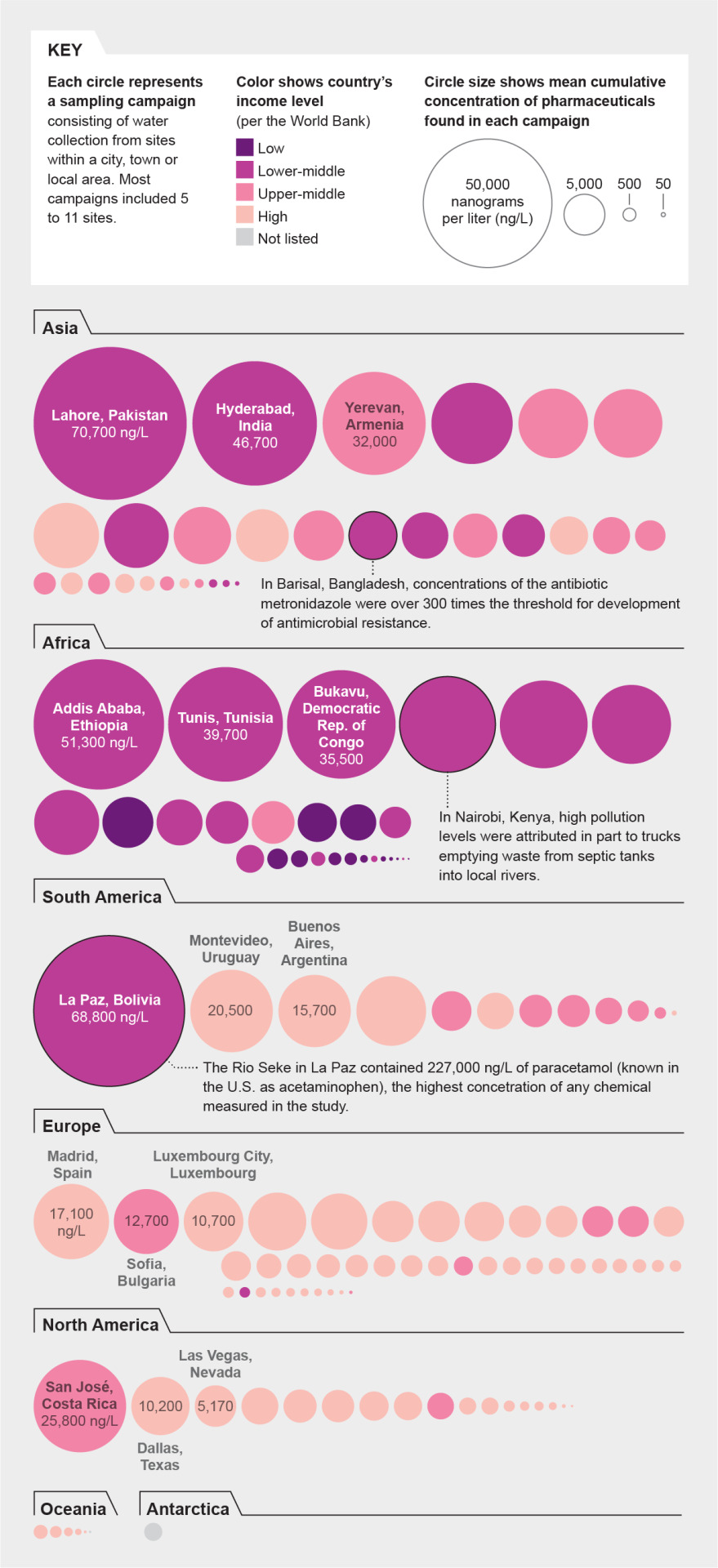
Summary
Four compounds—caffeine, nicotine, acetaminophen and cotinine (a chemical produced by the body after exposure to nicotine)—showed up on every continent, including Antarctica
Another 14, including antihistamines, antidepressants and an antibiotic, were traced on all continents except Antarctica.
Many of the most heavily-polluted rivers are in Asia and Africa, possibly because access to medicines have improved, but water treatment infrastructure are still developing
11 notes
·
View notes
Text
The link leads to an interesting article about the dismissal of pain in relation to biological sex in healthcare settings. The book Invisible Women: Data Bias in a World Designed for Men also provides valuable insight on the matter and how for a long time the anatomical male was considered the standard and the anatomical female was considered a variation.
From heart disease to IUDs: How doctors dismiss women’s pain
Several studies support the claim that gender bias in medicine routinely leads to a denial of pain relief for female patients for a range of health conditions
“One woman was told she was being “dramatic” when she pleaded for a brain scan after suffering months of headaches and pounding in her ears. It turned out she had a brain tumor.
Another was ignored as she cried out in pain during a 33-hour labor. She was supposed to be getting pain medication through her epidural, but it had fallen out.
Dozens of women complained of torturous pain as their vaginal walls were punctured during an egg retrieval process. They were told their pain was normal, but, in actuality, they were getting saline instead of anesthesia.
These are just some of the stories of women who say their pain and suffering has been dismissed or misdiagnosed by doctors. Although these are anecdotal reports, a number of studies support the claim that women in pain often are not taken as seriously as men.”
13 notes
·
View notes
Text
Super cool read about the potential influence of the development of impact bonds on the future of global health and humanitarian aid. Insightful, considering pandemic responses, including references to the Ebola and various other outbreaks, and how finances may affect the global community in regards to recovering from pandemics if investors and governments can’t/won’t pay.
Global Health Futures?
—
Abstract
Since 2010, there has been a discernable expansion of global health financing forms using private equity, bonds, and ‘facilities’ to finance international development and humanitarian endeavors. I present the logics of the Pandemic Emergency Facility (PEF), a World Bank device that lashes together a bond, cash, and swaps to lie in reserve for an infectious disease outbreak. I explain how the PEF is emblematic of financial devices that have the potential to fund global health aid while offering investors a chance to make money. Reckoning with the pandemic bond means that we take account not only of the PEF (what does it organize and by what logics?) but also of the relationships it cultivates (what does it bind together?) and reproduces (what does it aim to multiply and what does it forsake?). I use ‘reckoning with’ as an analytic concept to help us think about measures and futures of global health in both economic and ethical registers, as well as to take account of how death data is used. Reckoning with something lets us pause to take account of where we are and where we are going, and helps us think about what we want. Is it necessary to translate the ethical obligation to help those who are suffering into financial devices that make people money, a trend we are clearly in the initial stages of? Are there conditions when the suffering of others as the source of financial speculation becomes desirable?
As government funding for public health care becomes increasingly forsaken, and as global investors elect to pick up where nation states have left off, practical and ethical questions emerge about the mechanisms through which collective health futures will be financed. Reckoning with these questions is urgent because new financial mechanisms to fund health are being established now, mostly outside of public view. The devices are complex and born of multiple and competing interests and perspectives. They force a reckoning: If money for pandemic emergency response is not otherwise available, should investors be able to make money speculating on pandemics? What does pandemic investability mean for our collective health futures?
As part of my research on the financialization of global health, I reckon with these questions through the emergence of the ‘pandemic bond’, which is the money-making part of the World Bank’s Pandemic Emergency Facility (PEF), a financial device designed to provide money for pandemics. My ethnographic entry point into this bond is the 2014–2016 Ebola outbreak in Sierra Leone, where I have worked for decades.[note 1] My interest in the bond emerged from a first research project, conducted coincidentally at the same time as the Ebola outbreak, in which I was ‘following’ health data, which led me to a second project in 2016 to ‘follow the money’.
The PEF appeared on the global health financial scene in 2017, decades after governments around the world chose austerity-driven cutbacks in health care or had them imposed upon them, weakening or underbuilding health care infrastructures. The governments of Sierra Leone, Liberia, and Guinea, and their respective health care systems, were severely challenged when the Ebola virus killed thousands of their citizens from 2013 through 2016. But health care response-ability (Haraway 2016) had been circumscribed in those West African nation states for decades. Domestic political strife and war had depleted treasuries, making monies far less available for health, education, and welfare. The World Trade Organization and international financial institutions such as the World Bank and the International Monetary Fund also hobbled the implementation of a Sierra Leonean health system and curtailed its capacity to respond (Kentikelenis et al. 2015; Zack-Williams 2012; see also Pfeiffer and Chapman [2010] for health impacts from structural adjustment and Basu, Carney, and Kenworthy [2017] for post-2008 impacts resulting from austerity policies).
In this context, Jim Yong Kim, a physician, anthropologist, and the then World Bank president, promoted the PEF as a response to those failures. In October 2014, Kim began publicly advocating for ‘a new pandemic emergency facility’ that would deliver ‘money to countries in crisis’ during future disease outbreaks (World Bank 2014a). It was a message he repeated three months later at the World Economic Forum in Davos, Switzerland, where he won over global financial thought leaders, many of whom had complained for years about the aid industry’s inefficiencies. Typically, after a disastrous event, donors pledge funds, but fewer than half fulfill their commitments (Grépin 2015). Shifting pandemic emergency response from bilateral and donor funding to Wall Street financing is meant to fix a central problem of crisis financing: money is unavailable at the optimal time to stop or contain a threat. (‘Wall Street’ is meant here in the metonymical sense, inclusive of global-capital market sites where people, institutions, and corporations can buy and sell financial instruments to make money.)
Kim backed the PEF, saying that if it had existed: ‘in 2014 during the Ebola outbreak in West Africa, we could have mobilized 100 million dollars months before money actually flowed at a time when the epidemic was only one-tenth as severe. Instead, it cost 10 billion dollars for emergency response, recovery efforts and in economic losses to the affected countries’ (World Bank 2016b). The next year, in his 2017 American Anthropology Association keynote address, Kim (AAA 2017) championed the PEF as a way to ‘insure the poor against pandemics’: ‘We went to the capital markets and we actually raised $450 million, now it exists! We have pandemic insurance! So the 74 poorest countries in the world, including Liberia, Sierra Leone and Guinea. … Now when Ebola happens, with the first case, we have a bunch of cash that will go right out to try and stop it. [Audience spontaneously applauds.] Thank you’ (emphasis added).
To be clear, the PEF does not insure poor people per se: it is not health insurance in the conventional sense. And despite what Kim said, the PEF money raised in the capital markets is not available at the first case of Ebola, or even the 249th. Until the official death count reaches 250, no money is released. And even then, there are other criteria to meet.
In what follows, I explore the pandemic bond portion of the PEF in more detail, but first offer some thoughts on the work that ‘reckoning with’ can do when a device like the PEF augurs new ethical economies of global health aid. Influenced by Nelson (2009), I use ‘reckoning with’ as an analytic concept to help think about measures and futures of global health in both economic and ethical registers. Reckoning with is a process, a way of taking account of where we are and where we are going. It is a pause that gives a chance for the unnoticed to be noticed. Reckoning with is not an undoing but rather a reflection in the moment. It makes space for some contemplation and understanding before condoning or condemning. We can consider: Does this financial device shape a world we want? In this case, reckoning with the PEF means considering not only the financial device (what does it organize and by what logics?) but also the relationships it cultivates (what does it bind together?) and reproduces (what kinds of relationships are strengthened and which are forsaken?). Reckoning with the PEF raises Simmelesque questions about the obligations and exchanges between people who have much and people who have too little. Reckoning with the means of financial and health inequities is important, which brings up a second way I reckon with: I take account of the counting, of the global health data that triggers the pandemic bond. Should a poor country’s health care failures become sites of wealth speculation and accumulation, which would be one way to merge poor people’s right to health with the obligation of wealthy people and countries to alleviate suffering? In embracing this new financing, what do societies give up? An Economist editorial suggests that the bond ‘means becoming less queasy about putting the words “profit” and “human suffering” in the same sentence’ (2017, 68). But the ethical heft of what the pandemic bond sets in motion is graver than overcoming an upset stomach. The PEF is a harbinger of future global health finance. What do we want to do about that? Maybe nothing, maybe something. That’s what ‘reckoning with’ means.
Governments shaped the public health successes of the last 150 years, but this is changing as they draw back under austerity dictates. Before deciding to endorse or denounce the fact of the pandemic bond, let’s stay with the trouble (Haraway 2016) long enough to see the world in which the privatized securitization of and for healthy futures is used to justify financial accounting mechanisms that create interest-bearing bodies (see Baucom 2005). Let’s reckon with living in worlds where it may be necessary to translate the ethical obligation to help those who are suffering into financial devices that make people money, a trend we are clearly in the initial stages of. One important data point to reckon with: everyone I interviewed who had worked to create the PEF – to the person – believed it was a moral good of a high order. So let’s consider whether in our current and future worlds investors deserve the ‘right’, as PEF advocates phrase it, to potentially make money off other people’s suffering because other remedies will not be paid for by governments, by ideological design. Are there conditions in which making money from the suffering of others is desirable and should be scaled up?
What is the PEF?
With the PEF, the World Bank brings together more than sixty diverse groups to frontload money for quick future disbursement if a qualifying pandemic occurs in any of the seventy-seven International Development Association (IDA) countries, deemed the world’s poorest by the World Bank. According to the World Bank (2016a), the PEF will deliver timely, faster, and more cost-effective pandemic response; more private-sector money involvement; improved transparency and accountability; a strengthening of health systems; and a new market. The PEF covers several diseases, including the Lassa and Rift Valley fevers, coronaviruses like SARS and MERs, and influenza. Because the pandemic bond covers Ebola, a disease that devastated a country whose economy I know well, Ebola is the disease I use as a touchstone reference throughout this article.
To clarify, the Pandemic Emergency Facility is not a facility in any kind of bricks-and-mortar sense. And although it is sometimes described as insurance, it’s not insurance in the classic sense that a person pays a premium and then receives money to cover losses from an event. And despite the fact that most of its money-raising capacity was offered to investors by the World Bank as a bond, it is not a conventional or ‘vanilla’ bond. With vanilla bonds, people or countries buy in, that is, loan their money for a predetermined duration of the bond, while something gets built or funded;. at maturation, a guaranteed principal and interest is paid out. Instead, the PEF is a multiaspected, largely speculative financial device – part insurance, part bond, part swaps, part cash grant – that is structured by contractual arrangements, many of which are legally binding, among the groups involved. These arrangements are detailed in a 386-page prospectus (World Bank 2017c).
The PEF works as a container (see figure 1). The World Bank PEF account ‘holds’ donor contributions, the pandemic bond, and swaps (an exchange derivative) that total US$450 million. It also hosts a ‘cash window’ bestowed with a 50-million-euro donation from Germany (to which Australia added US$7 million in 2018) and augmented by other World Bank money pots on an as-needed basis. Cash-window money can be disbursed on request and operates like old-style bilateral aid but with all decisions on payments from the cash window made by a PEF Steering Body (World Bank 2019, 3) rather than a country’s department of state or ministry of foreign affairs. In this article, I focus on the pandemic bond, not the cash pot, because the pandemic bond is a sign and symbol of the big change in humanitarian finance, as governments draw down and capital markets rise up to take over obligations for human health. Of course, these governments and capital markets are peopled, and the social life of the bond is the story I tell here as well.
For the insurance part of the PEF, the World Bank pays insurance premiums with donated money from Germany and Japan to reinsurance companies on behalf of the seventy-seven IDA countries covered by the PEF. The reinsurance companies, SwissRe and MunichRe, pocket those premiums paid by the donors. (In the future, the World Bank expects that countries facing pandemic threats will find a way to pay their own premiums.) That’s the insurance part. The bond part of the PEF launched in July 2017 when twenty-six investors bought into a three-year bond designed to raise US$320 million for pandemic response. Investors give their money to the World Bank to hold for three years. Some investors paid US$250,000, the minimum qualifying amount; some invested US$50 million.
If there is a pandemic during those three years, the World Bank (2019, 3) gives some of the investors’ money to ‘responding agencies’ to administer emergency care:
PEF funds can be used to finance the cost of response efforts during an outbreak, in line with what is described in the country response plan. This includes, but is not limited to, deployment of human resources, drugs and medicines, essential and critical lifesaving medical equipment (including personal protective equipment), logistics and supply chain, non-medical equipment, essential life-saving goods, minor civil works (such as setting up temporary care centers), services, transportation, hazard payments, communication and coordination, etc.
There are restrictions: The maximum payout, for example, for filoviruses, of which Ebola is one, is capped at US$150 million. Also, PEF funds cannot be used for preparedness: ‘Funds will only be made available in times of crises, when countries have been affected by an outbreak’ (World Bank 2019, 4). And the standing pre-vetted ‘PEF-accredited responding agencies’ have been limited to four: World Health Organization (WHO), United Nations Children’s Fund (UNICEF), United Nations Population Fund (UNFPA), and Food and Agriculture Organization (FAO). IDA countries and aid organizations can apply to become a PEF responding agency by submitting an application. A World Bank–chaired steering committee of no more than seven voting and five nonvoting members decide which organizations qualify as responding agencies and get PEF funds (World Bank 2017a, 9).
If there is no pandemic during the three years, the investors get back their money, plus interest. If they invested in the higher-risk portion of the bond, they will get back the money they put into the bond plus annual interest of about 14 percent.[note 2] If a PEF bond investor invested US$50 million (there were reportedly such investors), they would receive annual interest of about US$6.81 million. Over the three-year life of the bond, they would earn about US$20.43 million in addition to getting their US$50 million back. An investment of US$50 million becomes approximately US$70.5 million in three years if there is no pandemic event.
Semiannual interest payments are paid to the investors with the money donated by the German and Japanese governments, an aspect of the bond’s design that Stein and Sridhar (2017) suggest is unsustainable. That donor money, which is earmarked as humanitarian aid, could otherwise go directly to pandemic relief. This has prompted criticism about whether the money should be given directly as aid, an opinion that has gained some traction in European and North American aid circles.
If you find the PEF’s operational mechanisms confusing so far, it’s not you. The PEF is confusing, I found, even to people working in the finance industry. At the World Bank, I met people who understood singular ‘silo-ed’ elements of the PEF very well but were not able to answer questions about other parts. Part of the problem is that the PEF combines aspects of many different financial products, so that a public health expert may not fully understand the insurance elements and vice versa. As a financial device, it is clever but also confusing, and I was not surprised to learn it took more than two and a half years to design. It had to be made up laboriously, combining features of the finance industry with pandemic public health measures.
The design element that took the longest time to create was the payout triggers. Money is released (or not) for emergency care depending on the number of confirmed deaths. In the event of a future Ebola outbreak in Sierra Leone, for example, no money from the pandemic bond is released for a single case or for any cases up to the 249th. When the 250th death is officially counted and other criteria are met, US$45 million becomes available, which is 30 percent of the money designated for filoviruses, of which Ebola is one. Sixty percent is available when 750 deaths are documented. One hundred percent, US$150 million, of the bond money designated for filoviruses becomes available when the official count reaches 2,500 deaths. Other qualifying criteria are written into the bond contract too: no matter how many deaths occur within a country, payout is only permitted when cases occur in two bordering countries or in a total of eight noncontiguous countries (see table 1).
Note: 100 percent payouts do not equal the total US$320 million paid in because no single qualifying epidemic event (such as Filoviridae viruses like Ebola) can claim all the bond money raised.
Further, as in the recent Ebola outbreak in the Democratic Republic of Congo (DRC) (which began 1 August 2018), there is also a ‘growth rate’ threshold, that is, a number and case growth calculation, that must be met for the investors’ money to be released (World Bank 2017c, PT-32). As of this writing, there are more than two thousand confirmed deaths, with a few additional deaths over the border in Uganda, but the growth-rate threshold is still being analyzed. In later sections, I take up the practices and politics of the death counts, but first I provide a genealogy to explain the pandemic bond as a logical outcome of changing humanitarian-aid practices.
The pandemic bond is born: A genealogy
The World Bank expanded its bond ‘family’ when it issued its pandemic bond in 2017. With its first green bond issuance in 2008 and its first catastrophe bond issuance in 2014, World Bank–backed bonds have become more complex with each generation. Green bonds work in the conventional way of raising money: A bank issues a bond on behalf of, for example, a government goal. Investors buy in, and if the goal is met by a certain deadline (the life of the bond, usually three to twenty years), the bank, for a fee, pays investors back the money they put in and the government pays them interest. During interviews, World Bank economists referred to green bonds – designed to build environmentally sound (‘green’) facilities and programs – as ‘vanilla bonds’ for their lack of complexity. World Bank officials consider green bonds a precursor to the more complex World Bank–issued catastrophe bonds, which in turn inspired pandemic bonds. With the issue of the pandemic bond, the World Bank hopes to catalyze a pandemic bond market in the way that the World Bank fostered the development of the green and catastrophe bond markets.
The World Bank is considered at the forefront of ‘innovative financing for development’. But it is not alone: the United Nations (2009) has been promoting financial innovation for almost a decade, and the Rockefeller Foundation has made a hard push for an ‘innovative finance revolution’ (Madsbjerg and Keohane 2016). ‘Advancing universal development goals through the breathtaking power of [financial] innovation’ (Nabarro and Schroeder 2016, 100) is a concept already well embedded in some international-development and humanitarian-aid circles. The Gates and Clinton foundations have advocated financial innovation since about 2010. In rich and poor countries alike, something was needed to make up for the tax-revenue shortfalls in health, education, and social-welfare provisions resulting from the neoliberal austerity schematics introduced in the 1980s.
Market remedies have become the prescriptive fix, ushering in the current era of what is called ‘impact investing’.[note 3] If investors are willing to risk their money on the chance that their money may be lost, the logic goes, then they deserve to make money. Taking on financial risk for the public good should be rewarded, according to this view. ‘Paying for success’ has become the mantra of impact investing and financial devices known as social impact bonds (SIBs) and development impact bonds (DIBs) have proliferated in earnest.
SIBs got off to a precarious start, beginning with the first one issued in England in 2010. The Peterborough Prison SIB did not meet its goal of reducing recidivism, but it set a financial precedent nevertheless because the bond device was considered a success. This raises a key critique of impact-bond logic: the social goal need not be fully met if the bond device works to deliver financial returns to investors.
The first SIB issued in the United States was launched in 2012 to reduce the number of sixteen-to-eighteen-year-olds returning to New York City jails within twelve months of their release. The goal was to cut recidivism rates through a brief cognitive behavioral therapy intervention. Goldman Sachs, who operated as both the bank and the investor, put up US$7.2 million and stood to make between US$500,000 and US$2 million if predetermined benchmarks were met (City of New York 2012). The therapy program failed, and Goldman Sachs lost some of its money (the US$7.2 million loss was reduced to a US$1.2 million loss by a US$6 million backup guarantee paid by Bloomberg Philanthropies). The failure of the bond to meet its goals is well known among SIB advocates, critics, and fence-straddlers alike (see, for example, Rudd et al. 2013; Cohen and Zelnick 2015; Dodge 2015, respectively). But the bond device worked as designed, and a model was born. Since then, the number of SIBs has grown: as of 2018, there were 108 SIBs in twenty-four countries (Rosenberg 2018). Most have not yet come to maturity.
Development impact bonds (DIBs) followed, applying SIB tenets to international development. The first, the Educate Girls Development Impact Bond – a three-year bond that raised US$270,000 to improve educational outcomes for girls in Rajasthan, India – was launched in 2015 and matured in June 2018. The investor, UBS Optimus Foundation, stood to make money even if results fell short (Instiglio[note 4] 2015, 15).Projections were that if education targets were fully met, the investor would get back its principal investment of US$270,000 plus US$89,085. Even if the outcomes met only 86 percent of the projected performance, the investor would get an additional US$36,657, a 13 percent return on investment (Instiglio 2015, 5). The interest payment was paid by the Children’s Investment Fund Foundation, a charity created by a former hedge fund manager, who would be able to write off the paid interest as a tax deduction.
When the bond was initiated, the investor was speculating on trial outcomes three years in the future. Their payout was determined by calculating student-learning outcomes using standardized tests in clustered randomized control trials (see table 2). Outcomes would eventually trigger the amount of investor return. Putting the debates about standardized testing and randomized control trials in education aside, this SIB example highlights how outcome data was used to make the investor money, an issue that affects the pandemic bond as well.
Results from its first two years suggested that the DIB was unlikely to meet its education and inclusion goals fully (IDinsight 2018, 8). But by year three, the Educate Girls Development Impact Bond had officially exceeded its enrollment and learning targets. The investor got their principal back plus 52 percent interest (US$270,000 + US$144,085 = US$414,085), as was directed by the bond contract. But measurement challenges troubled this bond, which comes to light in the eleven pages of footnotes and appendixes to the final evaluation report, half of the twenty-two-page report (IDinsight 2018). Numerous dubious and debatable decisions made by the Working Group[note 5] highlight just how central data is to bond investing. Working Group members needed the bond to work as an investment; that is, they needed it to succeed in paying out to investors. Decisions about the data reflect this; the data machinations were extensive. Questions about what to do with age-grade dissonance, for example, prompted footnotes like this: ‘An 8-year-old child in grade 3 during Year 3 Endline is shown as a 6-year-old child in grade 1 in this table’ (IDinsight 2018, 16). Debates within the Working Group about how to count learning gains inspired this decision: ‘The Working Group agreed to err on the side of overestimating learning gains for this group by assuming that the effect of the Educate Girls program on students not assessed at Baseline in grade 5 were the same as the effect on students assessed at Baseline’ (IDinsight 2018, 19). Some of the descriptions of what counts were simply nonsensical.
Measurement qualifiers, especially in the third year, were copious: ‘Newly-enrolled girls were omitted from all analyses’ (IDinsight 2018, 20). Students dropped out. A few schools closed. Some schools were dropped by the Working Group. In year 3, after years 1 and 2 were less than promising, the service provider increased remedial tutoring sessions for some students to twice a day, along with home visits. The service provider reported spending US$12 per student per year, when less than US$5 per student was usually spent on students in that region (Brookings 2018, 16). The point is not to belittle the measurements but to point out that behind the conclusion that ‘DIBs are successful!’ lies sometimes dubious and often debatable data-analysis decision making. Serious questions of long-term, population-wide applicability and sustainability abound and are cause for concern. For example, who will educate students who do not measure up in any given year when investors only pay for success?
There is one more essential precursor in the pandemic bond’s genealogy: the rise of catastrophe bonds (called ‘cat bonds’). Introduced in the mid-1990s, cat bonds are bonds of one to three years, sold by banks and purchased by private investors willing to ‘hold’ the chance that an insurance company will have to pay out claims if a catastrophe happens. Investors make money when they hold the bond for an event that does not happen (and that insurance companies do not pay out for). Natural disasters like hurricanes, earthquakes, wildfires, meteorite impacts, and volcanic eruptions fall into this category of investment device. Extreme mortality bonds were introduced in the mid-2000s to protect insurance companies against ‘losing too much money’ to life insurance claims in the event of a catastrophe. Investors bet on bonds speculating on the where, the magnitude, and the timing of the catastrophe.
In June 2014, as the Ebola pandemic raged, the World Bank had just issued its first cat bond, raising US$30 million, covering earthquakes and cyclones in sixteen Caribbean countries. Although the bank was about twenty years late to the party, its new cat bond was hailed as ‘innovative’ and a ‘milestone’ (World Bank 2014b). The then president of the World Bank Jim Kim took credit for putting the two – the Ebola pandemic and the cat bond model – together (AAA 2017). The PEF, with its catastrophe bond–like device and a 50-million-euro cash pot, became a signature contribution of Kim’s tenure.
It is important to reckon with this part of the genealogy: the pandemic bond grew out of a neoliberal milieu in which earlier precursors – SIBs, DIBs, catastrophe, and extreme mortality bonds – were hailed as the remedy to ‘bad, slow government’. The pandemic bond is a manifestation of larger trends away from direct investment in health care systems–infrastructure and toward pay-for-performance financing (Soucat et al. 2017) and accountable-care systems (McClellan et al. 2014). Never mind that governments have orchestrated astonishing public health improvements over the last 150 years (Rosling 2010): innovative global health financing eschews governments, and making money on disease is considered a problem-solving ‘win-win’ by many of the people I interviewed.
At the World Bank, I encountered a widespread embrace of development projects and products that provide ‘return’. When I asked my interlocutors there about future developments and whether to expect a pandemic bond 2.0, one of them said that the pandemic bond 1.0 issuance was a test to see if it functioned as imagined: ‘It’s proof of concept. … It’s a pilot and we’ll see how it goes. … [A 2.0] to a large extent, depends on whether the 1.0 triggers or not. Part of me is like, “I hope there isn’t another public health outbreak with pandemic potential”. But another part of me says, “Well, until that happens, we can’t really test it”’. In the summer of 2019, the World Bank announced it is working on a PEF 2.0.
Finance sociality: Relationships strengthened, relationships forsaken
The development of the bond portion of the PEF was, by many reports, a creative, iterative, and exciting process. For some, it was completely nerve-racking. ‘It was my life for two years’, a financial analyst said, sounding both proud and exhausted. A core group of officers from World Bank departments – Treasury, Health, and Development Finance – developed the bond using various exemplars from successful green and catastrophe bond issuances. As the PEF developed, the World Bank brought in reinsurance companies, a bond-brokerage company, and a data-modeling company to structure the bond.
When it came time to solicit investors, the World Bank turned to a familiar bond broker, the Guy Carpenter company.[note 6] A cat bond investor told me: ‘[The relationship between the World Bank and Guy Carpenter] is a typical kind of investment banking relationship. … [The World Bank] needs to turn to some expert who deals with us as investors every day. [Guy Carpenter] knows the whole universe of investors who have bought bonds before, what they’re thinking, who would care or not care. That’s their value to the World Bank’.
‘The whole universe of investors’, as it turns out, is a rather stable group of people. No mom-and-pop investors are allowed. Only institutional investors approved by the US Security and Exchange Commission (SEC) will do. (An SEC-accredited investor has to have earned at least US$200,000 in each of the prior two years and have a net worth over US$1 million. Banks, partnerships, corporations, nonprofits, and trusts may be accredited investors if their total assets exceed US$5 million or if all of the equity owners are SEC-accredited investors [SEC 2013].) SEC rules specify that an investor must be ‘sophisticated’, meaning that ‘the [investor] must have … sufficient knowledge and experience in financial and business matters’ (SEC 2013, ‘Who Is an Accredited Investor’). During an interview, a World Bank officer mentioned ‘going on a roadshow’ to look for investors:
SLE: The roadshow? I’m sorry, but I don’t know what that would mean for the World Bank to – ?
WB: Oh, so that would just mean we went to some cities, you know, to London, Zurich, Tokyo, New York, where we spoke with the bond investors and explained to people who were potentially interested in investing in this pandemic bond. We explained it to them.
SLE: And at any point did you seek investors or share the model in Sierra Leone, Liberia, or Guinea?
WB: No, we have a Steering Committee[note 7] for that.
From the World Bank’s perspective, the pandemic bond needs to work, and to work it needs to draw the ‘right’ kind of attention from the ‘right’ people. This meant getting investor buy-in from wealthy established capital networks. More than 80 percent of the investors covering the Ebola portion of the PEF are in Europe, with dedicated cat bond investors (35 percent) and pension funds (42 percent) making up the investor type (Artemis 2018b). Sierra Leoneans, Liberians, and Guineans (and people from other qualifying recipient countries) are imagined only as the intended recipients of a pandemic payout. They were not consulted in the making of the bond.
In 2016, about fifty senior health and national-security officers from Africa, North America, and Europe met near London. Three G7 governments hosted the meeting to share lessons learned from the Ebola outbreak. I was invited to explain the financialization of Ebola. After I finished explaining how the PEF works as a new form of pandemic financing, a high-ranking African officer immediately commented: ‘We’re not in this. I have never heard of this’. That officer and others around the room were visibly upset. At issue was the lack of consultation with African leaders in the making of the bond. Later, when I joined a lunch table where several country officers were eating and discussing the pandemic bond, the general tone had shifted to one of resignation. By the end of lunch, I left the table with the impression that during a national emergency like the one posed by the West African Ebola outbreak, it did not matter much where the money came from. Just that some came.
But, in a pandemic, is it always the money that matters most? This presumption begs reckoning with. Yes, of course, money is absolutely necessary to respond to pandemics. But during the Ebola outbreak, nonfinancial factors also severely affected disease containment (see Wilkinson and Leach 2014; Shepler 2017), most of which were minimized, in my findings, when compared with the World Bank’s aggrandizement of the PEF. And what of the big development banks’ responsibilities for economic structuring failures in Sierra Leone, those that stunted the growth of a health care system capable of thwarting early cases of Ebola (Kentikelenis et al. 2015)? Might the pandemic bond be part of a contemporary impact-bond juggernaut that is ‘a dramatic expansion of economic rationality and its penetration into new areas of human life’, when best practices like local consultation fall away in pursuit of capital (Cooper and Konings 2015, 2)?
Making what global health becomes
Among the people I interviewed, there was a widespread belief that the PEF was a moral good and that the financial performance of the pandemic bond would set in motion the future conditions of global health. In making the pandemic bond, development banks, reinsurance companies, data analysis firms, and investors aim to design anew what the field of global health becomes. For centuries, governments unceremoniously – and often unprofitably – held our collective disease-security risks, but now we are in an era of private takeover of and profit from that obligation. The global financial powerhouses who made the PEF believe the private sector should take over government tasks. By their logic, investors who ‘buy’ the risk of a pandemic deserve to make money; and they aim to cultivate a pandemic bond market that will establish and provide pandemic-response financing in perpetuity. They may be wrong, but increasingly they hold the power to shape global health futures to their liking and advantage. They design humanitarian devices, structure processes, and determine triggers. They do this outside the realms of democratic processes, without constituents constitutionally empowered to complain, critique, or improve.
Reckoning with their imagined global health futures means reckoning with the neoliberal logics and metrics that are taking us there. Making the pandemic bond is not only about constructing a vehicle in which both investors and pandemic responders share the chance to make money. It’s also about constructing another capital market for investors, including the reinsurance companies and development banks themselves, to diversify their portfolios. Diversifying investment portfolios is a common investment strategy, as different kinds of investments are not likely to lose money all at the same time.
An investor summed up for me the World Bank’s leadership role in the promotion of the pandemic bond market: ‘The bond relies heavily on the World Bank. Without their credibility and stamp of approval on this, it wouldn’t have been issued. … So it’s very important that everyone agree to what the deal is that they’re entering because, god forbid something happens, everybody’s got to be on the same page because otherwise the market doesn’t grow’. The World Bank understands that the market they are trying to cultivate with the pandemic bond is not something found ‘out there’ but rather something that must be painstakingly constructed. The bond’s designers aim to catalyze the future conditions of a global health field that will be able to rely on capital markets for funding.
It took two years to develop the PEF bond, and it was created with the hope that it would create a new market, a market for transferring the risks of outbreaks and pandemics from governments to private investors. Officially, according to the World Bank, ‘the PEF is expected to play a key market development role by helping create a new market for pandemic risk insurance. The private sector may take this forward on its own in a few years. … It is likely that over time, as the market matures, the PEF will scale up and pricing will become more competitive – as has been seen with catastrophe risk insurance facilities’ (World Bank 2016a, iii). The World Bank is counting on the pandemic bond to perform well enough to establish a pandemic bond market, much as the green and cat bond markets have over the last ten to twenty years. The growth of the green bond market established a solid faith in development bonds, but it was the catastrophe bond market – that mechanism for investing in natural and climate disasters – that set the sights and expectations for the pandemic bond market. The cat bond market took about fifteen years to mature and stabilize. Now it is thriving, valued at US$40 billion (Artemis 2019, as of 2 September 2019). Pensions are invested in the cat bond market with regularity. An investor pointed out, ‘From the investor perspective, many years went by where there wasn’t a loss in the cat bond market, so that helped a lot’.
If investors regularly lose the money they put into the pandemic bond, the market will cease to exist, and the pandemic bond will be considered a market failure. But it is completely possible that pandemic bond devices may successfully yield profits that will build a market but not correlate to disease containment and improved health outcomes. This is because only the data has to meet the contracted measures to profit. Much like Dumit (2012) and Sunder Rajan (2012) found with pharmaceutical profiting, well bodies and populations can become secondary. In essence, investors do not need to care about disease containment, only about the data representing disease containment. And if the pandemic bond performs and makes money for investors, that success will spawn other instruments like it and a new market will be born.
Speculative finance is now poised to catalyze what global health becomes. Caring about data that supports investor return may not necessarily correlate with well-body outcomes. We need to reckon with health data and health care systems that may soon need to be even more investor friendly. Many people say we can do both, but let’s interrogate that declaration, starting with an examination of how the data that determines returns on the bond actually works.
Reckoning the dead (I of II): Modelling Ebola risk
If there is a single element that could shake investors’ faith in the pandemic bond and undermine a future pandemic bond market, it’s the triggers. The numbers. The assignation of financial risk. The counting of the dead. It made sense when a World Bank officer told me: ‘The investors asked a lot of questions about the data and the veracity of the data and the trigger, because for them, that’s what matters the most. … The triggers took the most time to set up’.
In conversations about the pandemic bond and Ebola, there was a lot of slippage between the 250, 750, and 2,500 death triggers and the counting of the dead. But they are not the same. The triggers work on two registers. This section takes up how risk is defined and assessed by modelers and how investors assess their financial risk via the triggers; the next section takes account of how the dead are counted (and not counted) relative to the trigger thresholds.
The pandemic bond’s parametric triggers were assessed relative to the risk of a pandemic for investors, that is, the risk that they would lose their money, rather than the risk of pandemic for the people who would experience it. Data modelers hired by the World Bank assess this risk statistically. They start with retrospective WHO population health data and add data from other sources.[note 8] Parametric measures are data points projected for a given population using historical inputs and conditions chosen by the data modelers. It is a biostatistical exercise employing biostatistical conventions that include sampling and projection.
What data modelers bring to the project are models that help investors determine how risky the bond is, that is, the chance that they will lose their money. This is central to the bond as a speculative enterprise. One data modeler explained probabilistic modeling to me this way:
Data modeler (DM): No one claims that whatever’s presented is 100 percent representative of what’s going to happen. That’s why we do five hundred thousand years [of probabilistic modeling] because we want to consider all the feasibilities. Some things we can’t see, some things that are very severe, some things that are less severe, and that’s why we do probabilistic modeling.
SLE: Five hundred thousand years of modeling?
DM: Pick January 1 as your start date to December 31. [We model] what could happen from a pandemic or a large-scale epidemic or something like that if you resimulate [all the variables for a] whole calendar year five hundred thousand times. It’s the same thing as if I roll the die five hundred thousand times. You’d have lots of outcomes of that. You can run the probabilities many, many, many times until you see convergence [patterns in the results]. That’s why we selected five hundred thousand times to be able to figure out what might happen, based on the historical data and possibilities that we have.
Using the triggers as a guide, investors figured out the chance that they would lose their money or make a profit. The risk of death, and therefore of financial loss, is translated into financial risk for the investors. Details on this are deep in the fine print of the Prospectus Supplement (also called the ‘Term Sheet’) (World Bank 2017c, appendix II).
Thinking about the triggers as absolute thresholds is misleading, I was told, because they are meant more as intermediaries, as modes of thinking about risk. A modeler explained:
With the outbreak bond, you have the person selling the risk [the World Bank] and the person buying the risk [investors]. When we were on the investor roadshow, we were not necessarily trying to sell them that the 250 [death trigger] is right or the 750 [death trigger] is right. Our objective is to say our model can estimate these various numbers with reasonable accuracy. … We operate as this third-party thing, trying to not be biased in one’s favor or another. We’re trying to create what we believe is a reasonable estimate of the risks. We have to just go with best available data to get there [to set the trigger].
Like the making of a market, establishing a parametric trigger takes serious effort. The modeler continued:
The parametric model is kind of a weird structure. You could do a myriad of different ways that the structuring can get made, and our objective is to give [the World Bank] quantifiable risk against a lot of different assessments. When they ask a question, we might provide just that one: ‘Oh, you asked about A, here’s the risk’. Or we might do a few different things and say, ‘Here’s a few options based on what you said’. Or they might sometimes just say, ‘Before we do A and B, have at it and figure something out for us’, and then we’ll come up with an option, and then they’ll look at it and then be like, ‘We wanted to do some more stuff around it’, then you do that kind of stuff. So it’s this back-and-forth process.
Another modeler joked, ‘All the models are wrong, but some of them are useful’.
In the end, data modelers used their pandemic-risk model to help write conditions that were not likely to result in too much investor loss. The World Bank’s (2017a, 6) Operations Manual lists these conditions, which need to be met before investors lose their money in an Ebola outbreak event.
At least 12 weeks have passed from the start date of the event.
The outbreak is in more than one country, with each country having greater than or equal to 20 Confirmed Deaths.
The Growth Rate of disease needs to be greater than zero to ensure that the outbreak is growing at a specific statistical confidence level.
The Total Confirmed Death Amount needs to be greater than or equal to 250.
The Rolling Total Case Amount needs to be greater than or equal to 250.
The Rolling Confirmed Case Amount needs to comprise a minimum percentage of the Rolling Total Case Amount.
Regional outbreaks affecting two to seven countries would activate payments at three stages as the number of total confirmed deaths increases. Global outbreaks affecting eight or more countries also activate payments at three stages, but at higher funding levels at the first two triggers.
In talk about the pandemic bond as a financial device, there is regular and unself-conscious slippage between risk to investors and risk to people who are likely to experience the disease. Many people I interviewed talked about the two kinds of risk as if they were one and the same, when of course they are not. A deep reckoning with the pandemic bond forces an essential confrontation: for some people, the stakes are about losing or gaining money; for others, the risks are death or long-term disability. The numeric triggers obscure that difference, thereby creating another risk: losing sight of which risks to prioritize.
Reckoning the dead (II of II): Taking account of the counts
In World Bank documents, investor synopses, and bond blogs, the numeric triggers of the pandemic bond (table 1) are characterized as clear-cut and uninfluenced: ‘Parametric [health] triggers use publicly available and observable data to determine the payment amounts. As these triggers are based on observable data, they provide more transparency, increase the speed of payment and allow for an objective benchmarking of risk. … Bonds would be constructed around the same transparent and indisputable activation criteria’ (World Bank 2016a, 13–14).
What is striking in conversations about the pandemic bond with reinsurance, data-modeling, and finance personnel is the enduring faith they place in the triggers. Even when data limits are acknowledged, the prevailing sentiment was: ‘they’re the best we’ve got, and we’ve got to use something’. Counting the dead is beset by a similar sensibility. The pandemic bond uses counts published in WHO Disease Outbreak News or Situation Report, and there is faith in that data. When I interviewed one World Bank manager of the bond, I found that my knowledge of data collection in Sierra Leone was more granular than theirs:
WB: It’s data that WHO puts out. … WHO puts out those numbers in the moment.
SLE: By the month, or –
WB: No, they take it in real-time. You should talk with the health team because they’re the ones who gave us the assurance that WHO is doing this really in real-time.
SLE: Thank you, yes, I’ll follow up. In my research, though, I travel around with the people who collect the numbers for WHO. … I mean, I know the guys who collect the numbers in Sierra Leone.
WB: Okay. Alright. Well. … I’m a third-party receiver of the numbers. I don’t know whether it is a suspected case or a probable case or a confirmed case. I don’t track that. That’s not my job. It is WHO’s job, so we entrusted them with that responsibility. That is the data that we go on. … There was sufficient comfort, you know, in the data the WHO provides.
During research in Sierra Leone in 2014, our team collected ethnographic data on how health data is generated. In Freetown, the capital city of Sierra Leone, and in small cities in the eastern and northern provinces, we met with, interviewed, and observed the work of people involved with health-data generation. In the process, we learned that Sierra Leonean freelance enumerators are the most significant group of data collectors in the country. A cohort of mostly men and a few women in their twenties and thirties, these enumerators work on short-term contractual bases for any organization that ‘needs numbers’. For example, an enumerator is hired to collect data in twenty villages from people who suffer from a disease. Their job is to travel to these villages in, for example, two weeks’ time, collect disease data, and usually fill in a survey on a smart phone or tablet. That may sound straightforward, but in actual practice it is not. It’s precarious wage labor, complicated by language – in Sierra Leone there are about twenty different languages spoken in an area the size of Scotland – and further by work schedules often put together by people who have never been to Sierra Leone or driven on its roads (see images in figure 2). Nor do they understand the precarious rhythms of labor and labor mobility during the dry and rainy seasons. Collecting health data in Sierra Leone is physically and socially demanding work, and during an epidemic, be it cholera, measles, or, Ebola, even more so. One enumerator described the challenge: ‘The last time I went to Kailahun district [a region where the early Ebola outbreak occurred] I walked twenty-one miles to go to a village and twenty-one miles to come back. When you go to the field, your very first problem is how far it is. … Just imagine walking twenty-one miles to go and twenty-one to come back, and you have four villages to cover!’ Another Sierra Leonean enumerator mentioned similarly, ‘Enumerators have to go through frightful and dangerous roads. There is water, bridges, and bush paths in forests. Dangerous!’
Figure 2. Rural bridges and roads in Sierra Leone and Liberia, 2013. Left-hand photograph by J. B. Dodane, right-hand photograph by Travis Lupik, both used with permission.
Figure 2. Rural bridges and roads in Sierra Leone and Liberia, 2013. Left-hand photograph by J. B. Dodane, right-hand photograph by Travis Lupik, both used with permission.
To enhance data security, employers track enumerators via the Global Positioning System (GPS) in their phones. There is not always enough time to complete all the villages assigned and do all the paperwork. One enumerator’s statement summarizes what several others also said: ‘I have heard that sometimes people will send their smart phones with lorry or motorcycle drivers to a village, while they fill out the questionnaire, because there is just not enough time to do everything they want’. (See also Kingori and Gerrets [2016] and Biruk [2018] on the moralities and realities of data fabrication by fieldworkers.) But there are risks to this strategy, as noted by another enumerator:
The last time I went, [the WHO-contracted NGO] gave us PDAs [later, smart phones] to know if we went to the communities. They knew the GPS [Global Positioning System] coordinates of the village, so now you have the questionnaire and also a GPS. Now they detect you. … If they detect that you have not gone, they will send you back there. And maybe charge you with the full punishment of the law for giving them wrong information. They will retrieve your money they paid you.
Certainty about the health data down to the last digit is not possible. Investors potentially will lose money when the official data show 250 people dead; responding agencies and countries potentially get money for the same. Yet 249 deaths yield dramatically different results. People on both sides of the ledger are hedging their bets. Ministry officials in Sierra Leone have told me that they need ‘bad numbers’ to get foreign assistance. I found in earlier research that one of the ways they accomplish this is by not collecting health data from clinics known for their good outcomes. On the investor side, deflating death-rate data would be as easy as hiring enumerators for more lucrative work, thereby delaying data collection, or hacking into smart phones to alter data. There are many creative ways to play with data triggers, if that’s what stands between money for investors or money for receiving countries.
So much money is riding on the counts that I too must reckon with the potential impacts of my research. An investor told me, ‘If the event happens and investors feel like it wasn’t fairly calculated or there was some monkey business going on, then the market isn’t going to be around for long’. My work pulls back the curtain to show how the data is collected, counted, analyzed, and applied. Will the real-time wobbliness of the data deter potential investors? Will it derail the PEF? Maybe. In the investor worlds I entered, though, I found that investors are mostly agnostic. They go where the money is to be made. If not with pandemic bonds 1.0, then maybe with 2.0 or 3.0. Or they will go elsewhere completely. This is another risk to reckon with: in a possible future where pandemic risk management has been turned over to capital markets after government aid drops to historic lows, how will pandemics be funded if investors flee?
Insuring futures: Whose?
For some time now, the performance and even the viability of the World Bank has been in question. No friend of the Bank, the Financial Times regularly questions its relevance (see, for example, Financial Times 2014), along with other powerful North American and European international-development and finance establishments. The development economist Jeffery Sachs (2012) argues that the World Bank ‘has lacked a clear direction’, ‘solved far too few global problems’, and ‘completely fumbled the exploding pandemics of AIDS, tuberculosis, and malaria during the 1990s’. In a more recent article, in which he took a direct swipe at the World Bank’s Wall Street and Davos leanings, Sachs (2018) pointedly praised funding that used ‘outright grants, not Wall Street loans. Fighting AIDS in poor countries was not viewed as a revenue-generating investment needing fancy financial engineering’. Likewise, an article in the New York Times explored the link between the World Bank’s organizational viability and private-investor profit: ‘In a search for relevance, the bank’s president is altering its approach. … He is pushing private investors – sovereign wealth funds, private equity firms and insurance companies – to pony up trillions of dollars for projects. … They can reap rich returns by putting their money to work alongside the World Bank’ (Thomas 2018).
Reckoning with the pandemic bond means sorting out who has what to gain from its success as a financial device. In early 2015, the World Bank invited ‘some of the largest reinsurance companies in the world’ to help build the pandemic bond, a World Bank interlocutor told me:
Several [reinsurance companies] expressed interest, and we had conversations with them. But then, ultimately, they started dropping out. I mean, at that time, we didn’t know what the PEF would look like. But we said we were interested in partnering with the private sector to put together some sort of mechanism that will help insure countries against the next disease. Ultimately, there were just two that remained interested. They had some comfort in working with the bank because they also worked with the bank on the cat bonds.
I was told that the World Bank paid out about US$1 million to build the pandemic bond, and that the reinsurance companies[note 9] worked pro bono because they were very interested in developing the pandemic bond instrument. Since the 2017 PEF bond initial offering, they have already made US$37 million per year on PEF bond premiums. One economist told me that the reinsurance companies involved in the PEF ‘are expecting to make over $100 million’ on the pandemic bond premiums alone. They have a lot more to gain financially if a pandemic bond market becomes established along the lines of the green and cat bond models. Reinsurers were in it to develop and influence a market that they would be able later to invest in. Their financial security and profit depend on them being able to diversify their own portfolios and spread around their own risk, much as they have done in the cat bond market. A reinsurance executive bluntly explained that just making the pandemic bond alone would not have been worth it: ‘The amount of effort that we [the reinsurance company structuring the pandemic bond] had to invest into it, it was [a] very long and intensive time of work with many, many experts involved, lots of discussions going on. It’s only worth it against the hope that this effort would create a new market. Otherwise the costs involved in developing these types of solutions would be too high’.
But a well-known European economist familiar with the pandemic bond’s mechanics put the reinsurance companies’ interest in a different light: ‘It really doesn’t make much sense when the world’s resources for health care for people in poor countries are very scarce. So, adopting the design where half the money, on average, goes to an insurance company is kind of crazy’.
Dead reckoning
Dead reckoning is a navigational method that uses known plot points to set a direction (Blowditch 2002). It is an apt metaphor for anticipating whether pandemic bonds will establish and continue. What has the pandemic bond launched? Is turning back possible? Given the years in the making, the socialities between the World Bank, the bond brokers, the donor countries, and the reinsurance and data companies, and these parties’ investments of time and money, and all the favors asked, all the chits called in, and all the objections overcome to make the device, to set the stage for a new market, to get the job done, I ask: Is the future of pandemic response aid open? Or do the creation and the processes of the pandemic bond foreclose alternatives? Could pandemic security be returned to governments? Is it stubborn naïveté to continue to imagine worlds where investments in good government produce less financially motivated care? Could the bond as a global health finance device ever fail completely, given that there is so much from the so powerful at stake? Is there an equivalent here to ‘too big to fail’ (too much time spent, too many favors, too many promises, too many concessions, too much exchange)? Can any level of reckoning undo the bond making (double entendre intended) of the pandemic bond?
The ethical stakes of this reckoning ratcheted up a notch when the World Bank invited the reinsurance industry to the pandemic bond design process. The insurance industry’s role in Black Atlantic capitalism in the eighteenth century and its production of ‘interest-bearing bodies’ is instructive. Baucom (2005) tells of a British merchant vessel, the Zong, that sailed the Atlantic Ocean in 1781 en route to Jamaica, with 440 West Africans who would be sold as slaves in Caribbean slave markets. The ship went off course, extending the voyage. Food and water ran low. To compensate – and knowing he could claim insurance for lost ‘cargo’ – the captain directed that 132 men, women, and children from West Africa be thrown overboard, a premeditated mass murder at sea. When the ship arrived in Jamaica, its captain and owners claimed loss of insured property, at £30 per person. The insurers refused to pay; the captain and owner sued. The insurers were ordered to pay. The case was taken for appeal in a higher court, whose chief justice was intent on building England’s economy through his insurance law project (Krikler 2007, 35). The judge had found English commercial law ‘inadequate to the task of improving the efficiency of a burgeoning capitalism and ensuring the security of property and the integrity of business transactions’, including the slave trade (Krikler 2007, 42). Eschewing murder charges, the judge upheld the insurance contract. By the late eighteenth century, British insurance companies were insuring marine contracts, including covering ships carrying enslaved Africans, worth around £100,000,000 a year, which would be billions of pounds today (Krikler 2007, 32). Britain’s shipping industry and navy are widely considered essential to England’s nineteenth- and early-twentieth-century capital accumulation and domination. The association between insurance and profit-for-some – who uses insurance for what, why, and how much – is a historied and racist one.
When I learned of the 2018 Ebola outbreak in the DRC, my involuntary first thought was of the number dead and whether the pandemic bond had been triggered for aid. I checked the numbers; the death data hadn’t triggered the bond. Investors did not lose their money. Two weeks after the first Ebola cases in the DRC were confirmed, the PEF cash-pot mechanism, not the pandemic bond, kicked in. In May 2018, US$12 million from the cash pot was disbursed. The World Bank congratulated itself for moving the dial away from panic and neglect (Evans 2018). It took credit for the money being there, at the ready. Another US$20 million was disbursed in February 2019; US$10 million more was disbursed in May 2019. Deaths mounted, but no matter how many people die in a single country, the pandemic bond money cannot contractually be released as aid until the disease crosses the country’s border. A colleague wrote to me, ‘Saw the PEF numbers are at trigger level but still waiting for the border jump. What a bizarre and twisted situation!’ Then in June 2019, Ebola was confirmed in Uganda. But for the bond to trigger, there are still more conditions: there must be at least twenty deaths and the growth-rate threshold must be met. In August 2019, US$300 million was released for Ebola care from the cash window and other World Bank accounts. Two thousand dead, and still the bond did not trigger.
I continue to track the death data from the DRC outbreak, and reckon with the role of the data just as I continue to reckon with the bond. I am skeptical. I am not there in the Congo. I do not know if more people may have died only to elude count. I am not privy to the conversations in the ministries or to the whisperings of community members. I am not hanging out with the enumerators. Do they have gasoline for their motorcycles? Are they allowed into villages where people are dying from Ebola? What kind of data-collection schedules are they on?And then I catch myself. The death data is both the mainstage and the sideshow in the PEF schematic. Splitting off data from the actual health of populations is normal practice now (Erikson 2012), and care need not even be delivered for a financial device to ‘succeed’. Counting the dead has long been a political act of states, and now it is becoming a special interest of global financiers.
Are pandemic and development impact bonds the future of global health and humanitarian aid? All things considered, maybe they are. And if they are, let’s prepare and reckon with how we as a global community will pay for care during pandemics and other crisis events if investors flee and governments can’t or won’t pay. Is this the future we want? Let’s reckon with this now before the global health bond slot becomes a financial juggernaut, government coffers atrophy further, and pandemic problem solving becomes more circumscribed.
Acknowledgments
Research for this project was supported by the Social Science and Humanities Research Council of Canada; Simon Fraser University; a sabbatical fellowship at the Centre for Global Cooperation Research in Duisburg, Germany; and a 2016 Mercator Fellowship at the University of Halle, Germany. Special thanks to enumerators in Sierra Leone, the article’s anonymous interlocutors, the 2014 SFU-Salone ethnographic research team, the other authors in this special issue, the Stanford Department of Anthropology and Simon Fraser University School for International Studies colloquium groups, Baindu Kosia, Sam Eglin, Musu Abdulai, Puneet Grewal, Iveoma Udevi-Aruevoru, Earum Chaudhary, and Abou Farman. Deep thanks to Richard Rottenburg for lively, long-term encouragement and engagement with this project. Gary Parker was extremely helpful with the interest calculations, though any remaining mistakes are my own.
—
This post was previously published on medanthrotheory.org and is republished here under a Creative Commons license.
◊♦◊
Talk to you soon.
If you believe in the work we are doing here at The Good Men Project and want to join our calls on a regular basis, please join us as a Premium Member, today.
All Premium Members get to view The Good Men Project with NO ADS.
Need more info? A complete list of benefits is here.
—
Photo credit: Istockphoto.com
The post Global Health Futures? appeared first on The Good Men Project.
Global Health Futures? published first on https://manscaped.weebly.com/
2 notes
·
View notes
Text
A Key to Cancer Research: The Origin-of-Life Molecule
Researchers from Spain and Denmark have discovered a technique for attacking cancer cells in the production of one of the origin-of-life molecules.
The molecule that gave rise to life, RNA, has been demonstrated to be important for repairing human genetic material and avoiding mutations that might lead to cancer development. Recent research breakthroughs, such as those reported by Daniel Gómez Cabello’s research team at the University of Seville, propose this compound as a therapeutic target for developing tailored cancer treatment strategies.
8 notes
·
View notes