#procalcitonin
Text
Procalcitonin Market Trends, Size to 2026
The global procalcitonin market size was valued at USD 118.7 million in 2018, growing at a CAGR of 14.9% during the forecast period of 2019–2026.
0 notes
Text
Analyzing the Procalcitonin Tests Market by Test Type, End User, and Region
Analyzing the procalcitonin tests market by test type, end user, and region provides valuable insights into the factors driving demand and the dynamics of this market.

Buy the Full Report for More Insights on the Procalcitonin Tests Market Forecast,
Download a Free Sample Report
Here's an analysis of each category:
Test Type:a. Procalcitonin Assay Kits: Procalcitonin assay kits are used in clinical laboratories and healthcare facilities to measure procalcitonin levels in patient blood samples. These kits typically utilize immunoassay techniques such as enzyme-linked immunosorbent assay (ELISA) or chemiluminescent immunoassay (CLIA) to quantitatively detect procalcitonin levels. Assay kits may be available in various formats, including manual assays and automated assay systems.b. Point-of-Care (POC) Tests: Point-of-care procalcitonin tests are rapid diagnostic tests designed for use at the bedside or in outpatient settings. POC tests offer the advantages of fast turnaround times, enabling timely decision-making regarding antibiotic therapy in patients with suspected sepsis or bacterial infections. These tests are typically based on lateral flow immunoassay or other rapid immunoassay technologies.
End User:a. Hospitals and Clinics: Hospitals and clinics represent the largest end-user segment for procalcitonin tests, accounting for a significant portion of test volumes. Procalcitonin testing is commonly performed in hospital laboratories and clinical settings to aid in the diagnosis and management of sepsis, bacterial infections, and other inflammatory conditions. Hospitals may utilize both laboratory-based assays and point-of-care tests depending on their testing requirements and infrastructure.b. Diagnostic Laboratories: Independent diagnostic laboratories and reference laboratories also play a key role in the procalcitonin tests market. These laboratories offer testing services to healthcare providers, including hospitals, clinics, and physician offices, and may perform procalcitonin testing as part of routine clinical laboratory services or specialized infectious disease testing panels.c. Ambulatory Care Centers: Ambulatory care centers, including urgent care centers and outpatient clinics, may perform procalcitonin testing to aid in the diagnosis and management of infectious diseases in ambulatory patients. Point-of-care procalcitonin tests are particularly well-suited for use in ambulatory care settings due to their rapid turnaround times and ease of use.
Region:a. North America: North America is a significant market for procalcitonin tests, driven by factors such as the high prevalence of sepsis and bacterial infections, well-established healthcare infrastructure, and increasing adoption of advanced diagnostic technologies. The region is characterized by a strong presence of key market players, extensive research and development activities, and stringent regulatory standards governing diagnostic testing.b. Europe: Europe is another major market for procalcitonin tests, with countries such as Germany, France, and the United Kingdom leading in terms of market share. The region benefits from a robust healthcare system, growing awareness of sepsis management protocols, and favorable reimbursement policies for diagnostic testing. Increasing efforts to combat antimicrobial resistance also drive demand for procalcitonin testing in Europe.c. Asia-Pacific: The Asia-Pacific region represents a rapidly growing market for procalcitonin tests, fueled by factors such as the rising incidence of infectious diseases, expanding healthcare infrastructure, and increasing healthcare expenditure. Countries such as China, India, and Japan are witnessing significant market growth, driven by investments in healthcare modernization, improving access to diagnostic services, and growing awareness of sepsis management strategies.d. Latin America, Middle East, and Africa: These regions also contribute to the global procalcitonin tests market, albeit to a lesser extent compared to North America, Europe, and Asia-Pacific. Market growth in these regions is influenced by factors such as the burden of infectious diseases, healthcare infrastructure development, and efforts to enhance diagnostic capabilities in underserved areas.
Analyzing the procalcitonin tests market by test type, end user, and region enables stakeholders to identify key market segments, understand regional variations in demand, and formulate targeted strategies to address the needs of different market segments. Factors such as healthcare infrastructure, regulatory landscape, reimbursement policies, and disease epidemiology play a crucial role in shaping market dynamics and market growth opportunities across different regions.
0 notes
Text
Drive high CAGR by Global Procalcitonin (CAS 56645-65-9) Market

Procalcitonin (PCT) is a peptide hormone that is used as a biomarker for the diagnosis and management of bacterial infections. The procalcitonin (CAS 56645-65-9) market refers to the market for the synthetic form of procalcitonin used in diagnostic tests and therapies.
For Sample Report Click Here:-https://www.globmarketreports.com/request-sample/215251
The market for procalcitonin is primarily driven by the increasing prevalence of bacterial infections, the growing demand for rapid and accurate diagnostic tests, and the need for effective antibiotic stewardship programs. Procalcitonin is used in a variety of clinical settings, including hospitals, clinics, and laboratories.
The global procalcitonin market is expected to grow at a significant rate in the coming years, driven by factors such as increasing awareness among healthcare professionals and patients about the benefits of procalcitonin testing, the rise in the number of patients with sepsis and other bacterial infections, and the availability of advanced diagnostic technologies.
North America and Europe are the largest markets for procalcitonin, owing to the high prevalence of bacterial infections, well-established healthcare infrastructure, and the presence of major market players. Asia-Pacific is expected to grow at the highest rate, due to the rising incidence of infectious diseases, improving healthcare infrastructure, and increasing healthcare expenditure.
Some of the key players operating in the global procalcitonin market include Thermo Fisher Scientific, Roche Diagnostics, bioMérieux SA, Merck KGaA, and HyTest Ltd. These companies are focusing on product development, strategic collaborations, and mergers and acquisitions to strengthen their market position and expand their product portfolio.
0 notes
Text
Procalcitonin Antibody Market Size, Share & Trends, Product, Region & Forecasts 2030
Procalcitonin Antibody Market Size, Share & Trends, Product, Region & Forecasts 2030
Description
The impact of a number of factors such as economic, legal, social, political, technological, and modern business developments on market dynamics is briefly examined in the Procalcitonin Antibody market analysis. The global Procalcitonin Antibody market analysis focuses on market share and competitiveness index, which helps evaluate the top player’s contributions to the industry.…
View On WordPress
0 notes
Text
Global Procalcitonin Antibody Market regional Outlook
The Procalcitonin Antibody market is divided into North America, Europe, Asia Pacific, Latin America, and the Middle East and Africa based on region (MEA). The North American continent is further divided into nations like the United States and Canada. Europe is further divided into the United Kingdom, France, Germany, Italy, Spain, Russia, and the Rest of Europe. China, Japan, South Korea, India, Australia, South East Asia, and the rest of Asia Pacific make up the subregion of Asia Pacific. The MEA region is further separated into GCC, Turkey, South Africa, and Rest of MEA. The Latin America region is further divided into Brazil, Mexico, and Rest of Latin America.

Read More:
https://www.coherentmarketinsights.com/market-insight/procalcitonin-antibody-market-1907
0 notes
Text
Procalcitonin Tests Market
Market report scope
Market size (year – 2021)>$850 millionGrowth (CAGR)>10%Base year2021Forecast period2022-2030Key categoriesProcalcitonin enzyme immunoassay tests and procalcitonin other tests.Regional coverageNorth America, Europe, Asia-Pacific, South & Central America, and the Middle East & Africa.Key companiesbioMerieux SA, F. Hoffmann-La Roche Ltd, Abbott Laboratories, Siemens AG, Beckman Coulter Inc, Radiometer Medical ApS, Thermo Fisher Scientific Inc, Bio-Rad Laboratories Inc, DiaSorin SpA, Ortho Clinical Diagnostics Holdings Plc, and Diazyme Laboratories Inc.
This report provides a comprehensive overview of the procalcitonin tests (in vitro diagnostics) market. It also includes:
Currently marketed Procalcitonin Test and evolving competitive landscape:
Insightful review of the key industry trends.
Annualized total Procalcitonin tests (in vitro diagnostics) market revenue by segment and market outlooks from 2015- 2030.
Market level data on units, average selling prices, and market values.
Global, Regional, and Country level market specific insights:
Qualitative market-specific information is available with global trends further broken down into regional trends. In addition, GlobalData analysts provide unique country-specific insights on the market.
SWOT analysis for Procalcitonin tests (in vitro diagnostics) market.
Competitive dynamics insights and trends provided for Procalcitonin tests (in vitro diagnostics) market.
Reasons to Buy
Understand the impact of COVID-19 on procalcitonin tests (in vitro diagnostics) market.
Develop and design your in-licensing and out-licensing strategies through a review of pipeline products and technologies, and by identifying the companies with the most robust pipeline.
Develop business strategies by understanding the trends shaping and driving the Procalcitonin tests (in vitro diagnostics) market.
Drive revenues by understanding the key trends, innovative products and technologies, market segments, and companies likely to impact the procalcitonin tests (in vitro diagnostics) market in the future.
Formulate effective sales and marketing strategies by understanding the competitive landscape and by analyzing the company share of market leaders.
Identify emerging players with potentially strong product portfolios and create effective counterstrategies to gain a competitive advantage.
Track device sales in the global and country-specific procalcitonin tests (in vitro diagnostics) market from 2015-2030.
Organize your sales and marketing efforts by identifying the market categories and segments that present maximum opportunities for consolidations, investments, and strategic partnerships.
To view the complete report, click here.
0 notes
Text
HYPER, a case report
20 something years old man of Asian descent presented with a history of 1 week of temperatures, retrosternal chest pains and just not doing that hot. COVID test was negative.
During his physical, I could tell he was sick, pale, sweaty, tachypneic and tachycardic. His pressure was normal. Meningeal signs are negative. Neuro negative. Abdomen negative. No peripheral signs of emboli or rashes. There was a bit of a weird chest sound (listed I have been doing ID for some years but for the life of me sometimes I can't tell which one it is...I just know it's not supposed to be there)) and I think I heard a heart mummer.
His labs: high white cell count, elevated CRP and procalcitonin. In the differential, neutrophils took the prize. Lactate thru the roof. Liver enzymes were elevated (transaminases).
He got a chest x-ray which was clear. Ultrasonography of the abdomen was negative.
His history was insignificant, he doesn't have any preexisting medical conditions, and he is updated on all his vaccinations. He is straight, married for a few years. He likes to play football with his friends who are all of Asian descent. They don't have kids but they have a dog. He is a teacher, he teaches English. He hasn't been to his country of origin since he was a child and nobody around him has travelled anywhere lately. He doesn't travel, he hates flying.
I admitted him and started him on co-amoxicillin with metronidazole bc all I had was tachypnoea and fevers. Tho his chest x-ray was negative, we decided to order a chest and abdomen CT scan, his ddimeres were elevated so I wanted to make sure he doesn't have a PE, which he did not. However, what the CT scan described - was 2 small abscesses peripherally liver approximately 3cm each.
Meanwhile, his blood cultures came back positive for...
GIF by thegalaxyrailways
Klebsiella pneumoniae, the hypervirulent kind
lol
ok. I wanted to prescribe cefta+avibactam. My boss laughed and laughed and laughed and asked from which pocket that will go so...
In the end, we did a CT navigated drainage and gave him colistin.
He did well.
But I think it's something he got from the community. At least it's what the lit says.
Do u have any experience with hypervirulent Klebsiella pneumonia infection? Drop a msg in my inbox I wanna hear all your tips and tricks!
Also, I hope all my ID folks are having the best time at ID week. I hope I will be able to go one day!
#Suzy´s adventures in ID#another case#this time I tell u the answer immediately bc I can go away for a few months again lol#medblr#ID stuff#infectious diseases#klebsiella pneumoniae
11 notes
·
View notes
Text
In any patient presenting with acute pancreatitis, the greatest laboratory predictor of mortality is change in BUN over the first 48 hours with adequate fluid resuscitation. Studies have shown that for every 5-mg/dL increase in BUN during the first 24 hours, the age and gender-adjusted odds ratio for mortality increased by 2.2 (95% confidence limits, 1.8, 2.7). This is why current guidelines on the management of pancreatitis have begun to focus more on goal-directed fluid administration to lower the BUN (and hematocrit, though this does not predict mortality) if these are significantly elevated at admission with a target of normal values by 48 hours. It is felt that both of these numbers probably represent an overall hypovolemia and lack of adequate perfusion and that aggressive fluid administration is probably most necessary when these values are elevated at admission or continue to rise after admission. Guidelines recommend fluid administration at a rate of 5-10 mL/kg/hr of isotonic crystalloid. Increased fluid administration should be considered if BUN/hematocrit continue to rise after admission.
Numerous scoring systems have been created to help predict severity of illness in pancreatitis. Some which have been tested in the past include the Ranson score, BISAP Score, modified Glasgow score, and APACHE II. None of these scoring systems have good diagnostic accuracy with many studies showing somewhere between 40-60% accuracy at determining severity. Ranson scoring is probably the best after 48 hours, but is poor at admission. Therefore, while being familiar with these scoring systems may help you get a question correct, memorizing the components and cut offs is likely low yield. It is more important to realize that in the current literature a rising BUN and hematocrit over the first 48 hours of treatment are associated with increased mortality and increased risk of pancreatic necrosis respectively. Not surprisingly, many of these scoring systems incorporate changes in BUN and hematocrit as part of their scores. Of note, procalcitonin is currently being evaluated as a marker of severity and has shown some promise in predicting severity of disease.
In any patient presenting with acute pancreatitis, the greatest laboratory predictor of mortality is change in BUN over the first 48 hours with adequate fluid resuscitation. Studies have shown that for every 5-mg/dL increase in BUN during the first 24 hours, the age and gender-adjusted odds ratio for mortality increased by 2.2 (95% confidence limits, 1.8, 2.7). This is why current guidelines on the management of pancreatitis have begun to focus more on goal-directed fluid administration to lower the BUN (and hematocrit, though this does not predict mortality) if these are significantly elevated at admission with a target of normal values by 48 hours. It is felt that both of these numbers probably represent an overall hypovolemia and lack of adequate perfusion and that aggressive fluid administration is probably most necessary when these values are elevated at admission or continue to rise after admission. Guidelines recommend fluid administration at a rate of 5-10 mL/kg/hr of isotonic crystalloid. Increased fluid administration should be considered if BUN/hematocrit continue to rise after admission.
Peritoneal signs, such as rebound tenderness and guarding, are strong indications for surgical evaluation in patients with a small-bowel obstruction.
A CT of the abdomen and pelvis gives good information about all of the anatomical structures within the abdomen and pelvis, including the appendix, liver, pancreas, kidneys, biliary system, ovaries, and uterus, and the use of IV contrast will allow the detection of even small amounts of inflammation or abscesses.
Morphine is generally a good first-line pain medication in a patient with severe pain. Morphine is dosed by body weight in the acute setting and can be safely administered at a dose of 0.1 mg/kg body weight with redosing of 0.025 to 0.05 mg/kg every 5 minutes until adequate analgesia is achieved.
Antibiotics should be given for acute appendicitis, even in the absence of perforation. Studies have shown improved outcomes with 24 hours of antibiotics especially administered before a trip to the operating room. If there are signs of perforation, up to 5 days of therapy are continued postoperatively. Antibiotics that cover intestinal flora are generally acceptable, such as penicillins/cephalosporins. If the beta-lactam antibiotic chosen does not have good anaerobic coverage, then metronidazole should be added. Cefoxitin is a second-generation cephalosporin and has sufficient coverage to be used as monotherapy.
Antibiotic Options For Non-perforated Appendicitis: Cefoxitin
Cefotetan
Cefazolin + Metronidazole
Penicillin Allergic Options:
Clindamycin + (any of the following)
Ciprofloxacin
Levofloxacin
Gentamicin
Aztreonam
Perforated Appendicitis (Or Delayed Surgery)
Ertapenem
Piperacillin/tazobactam
2nd or 3rd Generation Cephalosporin or Fluoroquinolone + Metronidazole
I had a pt with diverticulitis in the ED the other day who was treated previously with cirpofloxacin and metronidazole. His PCP gave him moxifloxacin and my attending discharged him on cipro and metronidazole again. After reading the answer to this question, I think he should have been discharged on cefdinir (the oral version of ceftriaxone) and metronidazole instead. Maybe his was resistant to the fluoroquinolones and he should've been on a cephalosporin instead.
This patient should be treated with antibiotics for acute diverticulitis. Additionally, there is evidence of sepsis with fever, tachycardia, and an elevated WBC count. Ciprofloxacin and metronidazole are appropriate choices for outpatient management. Given worsening resistance to fluoroquinolones, many hospitals now request the use of alternate antibiotics while inpatient. Ceftriaxone is a third-generation cephalosporin and is appropriate in this case as it covers all standard gut microbiota that could be contributing to infection, except for anaerobes, which are covered by metronidazole. Given continued signs of infection, pain, and tachycardia, the patient should be admitted to the hospital and made nil per os until their pain is improving and they are ready to be started on a trial of diet. He should be admitted to a medical ward where he can receive IV antibiotics and fluids until he can tolerate oral intake. This can take 1-2 days in severe disease. Diverticulitis should be treated with broad-spectrum antibiotics in most cases (though there are reports of treatment of very mild, uncomplicated diverticulitis without antibiotic therapy by using bowel rest alone.) The antibiotics should cover gut microorganisms and are generally continued for 7-10 days depending on severity and clinician preference. Patients who cannot tolerate oral intake, have signs of sepsis, are elderly or fail outpatient treatment may require hospital admission. Antibiotic choices are listed if you click here. Note that medications that can be used as single agents have innate anaerobic coverage.
The most likely diagnosis is Burkitt lymphoma. Burkitt lymphoma is a type of non-Hodgkin lymphoma, which usually occurs in adolescents or young adults. It may have an association with Epstein-Barr virus (EBV), and is common in AIDS patients. It presents as a jaw lesion in the endemic form, which is common in Africa. The sporadic form is more common in the United States, and usually presents as an abdominal or pelvic mass. Biopsy of the mass often reveals sheets of lymphocytes with interspersed macrophages, also described as a starry sky appearance. The translation in Burkitt lymphoma is t(8;14) c-myc. The c-myc oncogene on chromosome 8 is translated next to the heavy chain Ig gene on chromosome 14. Treatment for Burkitt lymphoma is rituximab.
Flushing, diarrhea, and bronchospasm are the classic signs of carcinoid syndrome, caused by metastasis of a carcinoid tumor. Carcinoid tumors usually occur in the appendix or small bowel. Malignancies typically are related to the appendix, though the most common site of carcinoid tumors is the terminal ileum. Elevated 5-HIAA is diagnostic, and elevated chromogranin A will also be seen. After spreading to the liver, carcinoids can metastasize to the lung, bone, skin, and other areas. Associated symptoms occur after carcinoid tumors metastasize. Management of carcinoid tumor is surgical resection in localized disease. Octreotide can be used for symptomatic control.
3 notes
·
View notes
Text
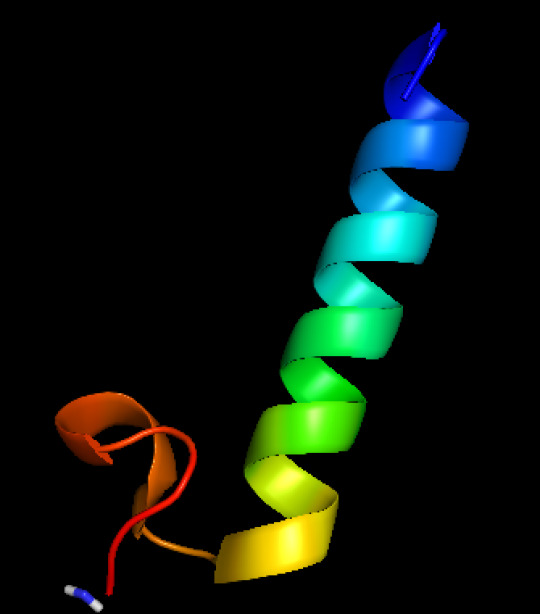
Polyclonal Antibody anti-procalcitonin (PCT)
Polyclonal Antibody anti-procalcitonin (PCT)
Catalog number: B2016325
Lot number: Batch Dependent
Expiration Date: Batch dependent
Amount: 500 ug
Molecular Weight or Concentration: N/A
Supplied as: Solution
Applications: a molecular tool for various biochemical applications
Storage: 2-8°C
Keywords: Polyclonal anti-procalcitonin (PCT)
Grade: Biotechnology grade. All products are highly pure. All…

View On WordPress
0 notes
Text
Pneumonia In Children And Adults

Introduction
Pneumonia stands as a prevalent respiratory infection, exerting a significant burden on global public health. Its impact extends beyond mere morbidity, contributing to substantial healthcare costs and socioeconomic consequences. This discussion aims to elucidate the general nature of pneumonia, encompassing its pathophysiology, clinical presentation, diagnostic modalities, treatment strategies, complications, and preventive measures. By indulging into these factors, we aim to provide a better understanding of pneumonia’s complexity and underscore the importance of timely recognition and management.
Pathophysiology

Pneumonia ensues from the infiltration of infectious agents, including bacteria, viruses, fungi, and less commonly, parasites, into the lower respiratory tract. Upon inhalation or aspiration of these pathogens, they gain access to the alveoli, where they incite an inflammatory response. This inflammatory cascade triggers the release of pro-inflammatory cytokines and chemokines, recruiting immune cells to the site of infection. Neutrophils, macrophages, and lymphocytes converge to eradicate the invading pathogens, leading to the characteristic consolidation and exudate formation within the affected lung tissue. As the infection progresses, alveolar edema, impaired gas exchange, and parenchymal damage ensue, culminating in the clinical manifestations of pneumonia.
Clinical Presentation

The clinical presentation of pneumonia encompasses a spectrum of symptoms, ranging from mild respiratory complaints to life-threatening respiratory failure. Common symptoms include cough, productive sputum production, fever, chills, pleuritic chest pain, dyspnea, tachypnea, and systemic manifestations such as malaise and fatigue. The severity of symptoms varies depending on factors such as the underlying pathogen, the extent of lung involvement, the host’s immune status, and comorbidities. In pediatric populations, pneumonia may present with nonspecific symptoms such as feeding difficulties, lethargy, and irritability, posing diagnostic challenges. Conversely, elderly individuals may exhibit atypical presentations characterized by confusion, hypothermia, and exacerbations of underlying chronic conditions.
Diagnostic Modalities

The diagnosis of pneumonia hinges on a comprehensive clinical assessment, augmented by various diagnostic modalities to confirm the presence of pulmonary infection and reveal its etiology. A thorough history and physical examination provide invaluable insights into the patient’s symptomatology, risk factors, and clinical trajectory. Symptomatic findings such as crackles, wheezes, and diminished breath sounds may aid in localizing the site of infection and assessing disease severity. Radiographic imaging, notably chest X-rays and computed tomography (CT) scans, serves as the cornerstone of pneumonia diagnosis, revealing characteristic radiographic findings such as airspace opacities, lobar consolidation, and interstitial infiltrates. Laboratory investigations, including complete blood count (CBC), C-reactive protein (CRP), and procalcitonin levels, may corroborate the clinical suspicion of pneumonia and guide therapeutic decisions. Additionally, microbiological testing of respiratory specimens through techniques such as sputum culture, blood cultures, and polymerase chain reaction (PCR) assays facilitates pathogen identification and antimicrobial susceptibility testing, thereby informing targeted therapy.
Treatment Strategies

The management of pneumonia hinges on prompt initiation of empiric antimicrobial therapy tailored to the likely causative pathogen(s) and disease severity. Antibiotics represent the mainstay of treatment for bacterial pneumonia, with the choice of agent dictated by factors such as local antimicrobial resistance patterns, patient age, comorbidities, and recent antibiotic exposure. Commonly prescribed antibiotics include beta-lactam agents (e.g., penicillins, cephalosporins), macrolides, fluoroquinolones, and combination regimens for severe or healthcare-associated infections. Conversely, viral pneumonia necessitates supportive care measures, given the limited efficacy of antiviral agents in most cases. Influenza-associated pneumonia may benefit from neuraminidase inhibitors such as oseltamivir, while respiratory syncytial virus (RSV) pneumonia may warrant ribavirin therapy in select cases. Adjunctive therapies such as oxygen supplementation, bronchodilators, and corticosteroids may mitigate respiratory distress and improve clinical outcomes, particularly in severe or hypoxemic patients. The duration of antimicrobial therapy varies depending on factors such as the causative pathogen, clinical response, radiographic resolution, and the presence of complications. Close monitoring of clinical parameters and serial imaging studies guide the decision-making process, enabling clinicians to tailor therapy to individual patient needs.
Complications

Pneumonia harbors the potential for various complications, ranging from mild to life-threatening sequelae, necessitating vigilant monitoring and timely intervention. Common complications include pleural effusion, empyema, lung abscess, respiratory failure, septic shock, and acute respiratory distress syndrome (ARDS). Pleural effusion denotes the accumulation of fluid within the pleural space, secondary to inflammation or impaired lymphatic drainage, manifesting as dyspnea, pleuritic chest pain, and dullness to percussion on physical examination. Empyema represents a purulent collection within the pleural cavity, often complicating bacterial pneumonia and necessitating drainage via thoracentesis or chest tube placement. Lung abscesses manifest as circumscribed cavities containing necrotic debris and pus within the lung parenchyma, triggered by persistent fever, productive cough, and hemoptysis. Respiratory failure ensues from impaired gas exchange and alveolar hypoventilation, caused by worsening hypoxemia, hypercapnia, and respiratory acidosis, necessitating mechanical ventilation and intensive care support. Septic shock represents a life-threatening complication of severe pneumonia, characterized by systemic inflammatory response syndrome (SIRS) and end-organ dysfunction, requiring aggressive fluid resuscitation, vasopressor therapy, and broad-spectrum antibiotics. ARDS denotes a severe form of acute lung injury, characterized by diffuse alveolar damage, refractory hypoxemia, and bilateral infiltrates on chest imaging, necessitating lung-protective ventilation and supportive care in the intensive care unit (ICU). The occurrence of complications portends a poor prognosis and underscores the need for early recognition and intervention to mitigate adverse outcomes.
Preventive Measures

Preventing pneumonia entails a broad approach encompassing vaccination, infection control measures, and health promotion strategies aimed at reducing the risk of respiratory infections and their sequelae. Vaccination stands as a cornerstone of pneumonia prevention, targeting common bacterial and viral pathogens implicated in pneumonia pathogenesis. Vaccines such as the pneumococcal conjugate vaccine (PCV13) and pneumococcal polysaccharide vaccine (PPSV23) confer protection against Streptococcus pneumoniae, the leading bacterial cause of pneumonia, particularly in high-risk populations such as young children, older adults, and immunocompromised individuals. Influenza vaccination remains paramount in mitigating influenza-associated pneumonia and reducing disease transmission, underscoring the importance of annual vaccination campaigns targeting vulnerable populations. Additionally, adherence to infection control measures, including hand hygiene, respiratory etiquette, and environmental sanitation, plays a pivotal role in reducing the spread of respiratory pathogens in healthcare settings and the community at large. Health promotion efforts aimed at smoking cessation, optimizing nutrition, and addressing underlying comorbidities such as chronic obstructive pulmonary disease (COPD), asthma, and immunodeficiency bolster immune resilience and mitigate pneumonia risk. Furthermore, early identification and management of predisposing factors such as malnutrition, homelessness, and overcrowded living conditions attenuate pneumonia susceptibility and enhance overall health outcomes.
Conclusion
In conclusion, pneumonia emerges as a formidable respiratory infection, posing significant challenges to global public health. Its diverse etiology, clinical manifestations, diagnostic modalities, treatment modalities, complications, and preventive measures underscore the nature of pneumonia management. Timely recognition and intervention are imperative in mitigating the morbidity and mortality associated with pneumonia, necessitating a collaborative approach among healthcare providers, public health authorities, and policymakers. By fostering a comprehensive understanding of pneumonia’s manifest and implementing evidence-based strategies, we can strive towards reducing its burden and improving patient outcomes. Through ongoing research, education, and advocacy efforts, we can envision a future where pneumonia-related morbidity and mortality are substantially diminished, paving the way for enhanced respiratory health and well-being worldwide.
In managing pneumonia, compassion, empathy, and a holistic approach are essential alongside clinical expertise. Striving for excellence in knowledge and practice allows us to enhance respiratory medicine and patient outcomes.
As we address pneumonia and broader cardiovascular health complexities, let’s remain committed to optimal patient care. Together, we can impact lives positively and foster a healthier future.
Email [email protected] to discover how we can support your academic and professional goals. Wishing you ongoing success in your medical journey.
#assignment help#medical students#healthcare#nursing student#medicine#medical help#medical school#health and wellness#online writing#nursing school#nurses#nursing#public health#heart disease#pharmacy colleges#pharmacy student#pharmacy technician#pharmacy
0 notes
Text
Procalcitonin Rapid Test Kit Market Size, Share and Forecast 2031
#ProcalcitoninRapidTestKitMarket#ProcalcitoninRapidTestKitMarketReport#ProcalcitoninRapidTestKitMarketGrowth#ProcalcitoninRapidTestKitMarketTrends
0 notes
Link
1 note
·
View note
Text
0 notes
Text
Procalcitonin Antibody Market Growth: Unraveling the Diagnostic Revolution
Procalcitonin Antibody Market: Unveiling the Potential of Diagnostic Advancements
The Procalcitonin Antibody Market, a critical segment of the diagnostic testing landscape, is witnessing a rapid evolution, propelled by advancements in medical science and technology. Procalcitonin, a precursor molecule to the hormone calcitonin, has emerged as a crucial biomarker in the field of infectious disease diagnostics. This protein plays a pivotal role in identifying bacterial infections and differentiating them from viral ones, guiding clinicians in making informed treatment decisions. As the demand for more accurate and efficient diagnostic tools grows, the Procalcitonin Antibody Market is experiencing significant expansion.
Procalcitonin, when released in response to bacterial infections, serves as a reliable indicator of sepsis, a life-threatening condition. With the increasing prevalence of sepsis and other infectious diseases worldwide, the importance of precise and timely diagnostics cannot be overstated. Procalcitonin antibodies, particularly monoclonal antibodies, have gained prominence for their exceptional specificity and sensitivity in detecting elevated levels of this biomarker in patient samples.
Key Market Drivers:
1. Rising Prevalence of Infectious Diseases: The global healthcare landscape is facing an escalating burden of infectious diseases, and the ongoing COVID-19 pandemic has underscored the need for rapid, accurate diagnostics. Procalcitonin antibodies have proven invaluable in identifying bacterial infections and helping physicians make informed decisions regarding the administration of antibiotics.
2. Growing Awareness: As awareness regarding the significance of timely diagnosis and the harmful consequences of antibiotic overuse continues to increase, healthcare providers and institutions are increasingly adopting Procalcitonin testing. This trend contributes to the market's expansion.
3. Advancements in Monoclonal Antibody Technology: Monoclonal antibodies are central to the Procalcitonin Antibody Market. Their exceptional specificity and sensitivity make them ideal for diagnostic purposes. Ongoing research and technological innovations have further improved their performance, bolstering market growth.
4. Integration of Point-of-Care Testing: The demand for point-of-care (POC) testing has surged, particularly in emergency departments and intensive care units. Procalcitonin POC tests offer quick results, enabling immediate treatment decisions, reducing hospital stays, and potentially curbing the misuse of antibiotics.
5. Government Initiatives and Guidelines: Government agencies and healthcare organizations are promoting the responsible use of antibiotics through guidelines and awareness campaigns. This has resulted in increased adoption of Procalcitonin testing as a tool to combat antibiotic resistance.
Challenges and Opportunities:
Despite the promising growth prospects, the Procalcitonin Antibody Market faces challenges. The market is somewhat consolidated, with a few key players dominating, which could lead to limited pricing flexibility. Additionally, the initial cost of implementing Procalcitonin testing in healthcare settings can be a hurdle for resource-constrained institutions.
However, there are also significant opportunities. Research and development efforts are ongoing to improve the affordability and accessibility of Procalcitonin testing. The development of biosensors and portable POC devices can further democratize diagnostic testing, especially in underserved regions.
Moreover, the market's growth is not limited to healthcare institutions. The pharmaceutical industry is exploring the use of Procalcitonin antibodies in clinical trials, particularly for evaluating the efficacy of new antibiotics. This dual application further broadens the market's horizons.
In conclusion, the Procalcitonin Antibody Market is poised for robust growth due to the increasing need for precise diagnostics in infectious diseases, antibiotic stewardship efforts, and technological advancements in antibody-based testing. As the healthcare industry strives for more effective and efficient ways to combat infectious diseases, Procalcitonin antibodies will continue to play a pivotal role in guiding clinical decisions and improving patient outcomes. The ongoing synergy of innovation, awareness, and research makes this market an exciting and critical component of the healthcare diagnostics sector.
Few other promising reports in Biotechnology Industry
Immune Cell Engineering Market
Skin Cancer Drugs Market
Visual Arts Therapy Market
Sildenafil Drug Market
0 notes
Text
0 notes
Link
0 notes