#spinal fusion recommended
Text
Writing Modern Steve Roger's Health Issues: A compendium
AKA How do Steve Rogers' MCU canon illnesses hold up in a modern setting?
I am writing something that is SO NICHE and so NERDY I feel absolutely, positively deviant about it. Who knew you could have this much fun while eating a burrito and sitting in the sun on your back porch?
OKAY! This one goes out to all of you writing modern AU's with a modern Steve Rogers. (There are literally dozens of us!). Let's go.

So, I find it somewhat problematic when people write disabled or otherwise medically complicated characters and are wishy-washy about the diagnosis they have. In real life, everyone I know with ongoing medical issues is a fucking expert on their exact shit. A great tumblr reference for disabled characters is Cripple Characters, but I also use reddit threads to read about people’s day to day experiences with different issues in their own words. If nothing else, just decide what your character has and take ten minutes and read through a basic website article about it.
So let's walk through what modern Steve's medical history and diagnoses might be. If you feel like I missed any details or got things wrong, happy to have comments to that end.
We'll start with the list of “ailments,” going with the MCU canon and combining the images from the museum exhibit and screen shots of Steve’s enlistment forms:
Asthma
Scoliosis
Fallen arches
Partial deafness
Scarlet Fever, Rheumatic Fever
Heart arrhythmia
High blood pressure
Palpitation or pounding in heart
Easy fatigability
Stomach ulcers
Pernicious anemia
Nervous trouble of any sort
Sinusitis
Chronic or frequent colds
Caveat: I am not a doctor, but I am a person who enjoys reading medical journal articles about illnesses I do and don’t have. The human body is a fascinating and terrible place to live. Talk to me about your medical complications - I will always find them interesting. I love small talk about Crohn’s disease and/or extremely graphic details about the time you had surgery because one of your wrist bones was the wrong length.
Sucks To Your Assmar: Asthma! How has asthma changed?
Kids who have their asthma well managed at a young age are going to have less scarring and lung damage (this is called airway remodeling). Thus a modern kid will likely have less severe asthma than a kid born in Steve’s time. Further, allergy medicines got way better from the 1990s, so kids with allergy induced asthma would have had fewer attacks. Fewer attacks as kids = less severe asthma as they age.
I would also note that asthma is highly connected to environmental issues. If Steve grew up in a house with cigarette smoke, cockroaches, rats, or mold present, as is fairly easy to imagine, especially without dehumidifiers in a swampy Brooklyn summer, those are environmental factors that would have made his asthma much worse.
They are also all factors that kids today certainly face, depending on how you write your modern Steve’s childhood. While people today certainly can have very severe asthma, it’s also entirely possible that modern Steve’s relationship to his asthma is pretty chill and easy to manage. (My partner has relatively severe asthma with a lot of environmental triggers; modern allergy medicine was a big game changer.)
Let’s talk about scoliosis ~~
There are a lot of variations to how scoliosis impacts people. I have very minor scoliosis and it's barely a thing in my life. I’m not trying to speak for everyone, but for what it’s worth, there are professional athletes with spinal fusion. I used Kyra Condie as my justification for writing climbing coach post-spinal fusion small Steve Rogers in one fic. My younger brother and best friend in high school both had spinal fusions.
In reality the athletic and physical abilities of people with spinal fusion vary pretty much exactly as much as people without spinal fusion, so you have a lot of leeway for how you decide to write a character with scoliosis. I recommend reddit threads to read about people talking about how their bodies felt before and after spinal fusion, or why they decided not to have the surgery, if you want to get a sense of how it might affect your character’s day to day life.
Wait, so how tall is modern small Steve Rogers?
You can see in this article that gains in height post scoliosis corrective surgery/spinal fusion varies, but the mean was 27 mm (1 inch) and the maximum was 66 mm (2.5 inches).
The more severe the curve in the spine, the more height gained with surgery.
We know Steve had scoliosis, we don’t know how severe it was (do we?). But if he was 5’4” without spinal fusion, and with all of his childhood fevers, and possible poor nutrition due to the Great Depression and untreated stomach ulcers, then it’s very reasonable that a modern Steve raised with proper nutrition and his gastrointestinal issues (see below!) properly treated and a spinal fusion could be easily 1-10 inches taller.
I think it’s great if you want to write modern Small Steve as 5’4” - but I tend to write him as 5’7” or so.
I think it is entirely likely that a modern Steve Rogers could end up being 6 feet tall given modern medical intervention and a healthy digestive system and adequate nutrition. As an example of how people with more or less the same genetics having different heights due to environmental factors, I know of one family of four brothers that immigrated from Italy in the 40s. Their height was 100% correlated to their age when they moved to the US/started having access to food: the oldest brother was around 5’4” and the youngest around 6 feet. The oldest was also a chain smoker and worked full time from around age 8, so you know, he was a fucking badass 5'4" Italian guy, if that's not clear.
What about fallen arches?
Fun story, but I have fallen arches/flat feet and had a lot of foot pain as a kid, but I thought it was normal. I wear custom orthotics and/or birkenstocks and do exercises to strengthen my feet muscles and it's fine now as long as I remember to do the things I just mentioned. My dad had to have multiple surgeries on his feet, so I think it helped that they caught it earlier in me.
Should I write modern non-serum Steve as deaf?
Maybe! I think it’s lovely when people write characters with hearing issues. There are great blogs that cover ways to do that well (a good link, another one, and another one and I think this one on hearing aids is particularly good if you are trying to bring in subtle day to day routine differences a character that wears hearing aids may have. Another great option is, again, reddit, especially for questions around how sexual intimacy might vary in small ways that can be nice to bring in. (I am working on a fic with a seeing character whose ex is blind and also read a lot of couples first hand experience with sexual intimacy around that dynamic on reddit).
But how likely is it that modern Steve would be deaf?
I think that it’s reasonably likely that Steve’s hearing issues were a result of Scarlet Fever, which is a bacterial infection that can result in rheumatic fever, an inflammatory condition that develops in more severe cases of scarlet fever.
Scarlet fever caused deafness - in fact, both Helen Keller and Thomas Edison had hearing loss due to scarlet fever infections. Further, sustained fevers of over 104 degrees can also cause hearing loss, so there is a reasonable chance that some other fever caused Steve’s hearing issues.
Today, the kind of hearing loss caused by fevers and infections can usually be surgically repaired or never occur because we have better antibiotics and better medicines to treat fevers. However, I have a friend who has partial hearing loss and lots of other life long nervous system and fatigue issues due to complications from childhood chicken pox in the 80s (this vaccine came around in 1995).
I don’t know if it’s canon or fanfiction, but I often see Steve as having one bad ear. For what it’s worth, hearing loss in one ear is much less common than hearing loss in both ears.
However, potential causes of hearing loss in one ear are infections that result in a high fever and some kind of head trauma, both of which are easy to imagine would have affected a Steve born in 1918, and while possible in a modern Steve, also easier to avoid.
Heart Stuff: Heart arrhythmia, High blood pressure, Palpitation of pounding in heart, Easy fatigability
The aforementioned fevers that can cause hearing loss can also cause heart issues. I think it’s reasonably likely that Steve’s heart issues were from his fevers as a young kid, but I often write him with a congenital heart defect, because why not?
These days, most of the time, such issues are detected at or before birth and fixed when the person is a baby, but there are plenty of heart issues that can require multiple heart surgeries at various points. Regardless, a modern Steve would most likely either have had access to corrective surgery or medication to manage these heart conditions. Which is not to say that he wouldn’t suffer mental and physical trauma from this medical complication.
There are plenty of professional athletes you can find who have all of the above heart issues. And plenty of people with heart issues who have no interest in being professional athletes, so like, follow your bliss.
Digestive System Stuff: Easy fatigability, Stomach ulcers, Pernicious anemia
I have easy fatigability under heart stuff too, because lots of shit can make you tired.
My personal head canon is that Steve Rogers has celiac disease and/or lactose intolerance, it would cause all of the above. Both can also lead to poor growth - in fact falling off growth charts is one of the most common symptoms of celiac disease in children.
While people have been aware of celiac disease since there were people, gluten wasn’t identified as the clear cause till the 50s.
I typically write modern Steve with some kind of food allergy, and I think that addresses quite a few of his canon medical complications.
Because so many causes of this category of symptoms are relatively easily solved with modern medical intervention/avoiding the problem, I would point folks towards Crohn’s disease if you are looking to write a modern character with medical issue that is more likely to be an ongoing source of similar medical complications today.
(Also, kids with Crohn’s are likely to have reduced height. I have a friend who has Crohn's whose 3 siblings are well over 6 feet and he is around 5'8" (so 4-6 inches aka 11+ cm shorter due to his severe childhood illness).)
Nervous trouble of any sort
Kids with medical complications and food allergies are much more likely to have anxiety. I’m so proud of all the kids making it through the day with anxiety. Luff you anxiety kids, I see you working twice as hard to be present as the non-anxious kids. Tough as hell. Give yourself a high five. I’m so damn proud of you.
Sinusitis and Frequent colds
I mean, god bless modern decongestants and allergy meds. Celiac disease and lactose intolerance can both cause sinus issues, so here is another one of Steve's ailments that can be "cured" through that diagnosis.
Other stuff
When you look at the above, you can see a lot of scenarios where modern era Steve, like many children/adults today, had multiple surgeries and serious and scary health complications as a child, but as an adult would appear as a relatively healthy able bodied person, with the possibility of even becoming a top athlete if he was so inclined. It’s also likely that some issues like chronic fatigue etc, might linger into adulthood as relatively invisible illnesses that nonetheless affect his everyday.
In some ways his character arc given the advances of modern medicine could mimic his arc due to the serum.
Being medically complicated as a kid sucks. Even if you have surgeries to treat and/or learn how to live with things like Crohn’s and celiac and reduce flare ups, lingering mental health trauma can have an impact.
Lastly and most importantly, I have a personal headcanon that young Steve Rogers of any era spent a lot of time sick in bed and staring into a mirror learning how to raise one eyebrow and perform other eyebrow gymnastics so he could more effectively sass his nurses.

IN CONCLUSION:
I think it's actually reasonable for an author to say, "My modern Steve never had any fevers, and got his severe lactose intolerance diagnosed as a baby, and had good nutrition, had medications/clean environment that prevented his asthma."
So this Steve is 6 feet tall and healthy as long as he doesn't eat dairy and takes his daily zyrtec (cetirizine - it's an allergy med). The only medical issue he has from canon left is scoliosis, flat feet, and an astigmatism.
You can also choose to write a Steve with more complex medical issues, and there are lots of things that can be good and interesting and value about that. I think the main thing is to pick a diagnosis and write it realistically, hopefully this helps some with that!
#stucky fanfiction#smol steve#writing disability#steve roger#pre serum steve rogers#modern steve rogers#honestly whats wrong with me#I don't even know but I feel like I'm dealing with my mental illnesses well enough and I had fun writing this#meta#headcanon#stony fanfiction
440 notes
·
View notes
Note
hiiiiiii <3 i saw you dont mind talking about your past spinal fusion surgery and i LICHERALLY dont know anyone else to ask about it lol i guess my question is like. do you i guess RECOMMEND it? its something im considering cos im like almost in too much pain to function but im scared of being MORE fucked up afterwards :( any insight would be immensely appreciated tysm <3
it’s been about 10 years since my fusion with Harrington rods, I had mine done at 10 levels (from T2-T12 I think) when I was 14 at the University of New Mexico children’s hospital (I’m fine sharing this because I live across the country now)


the first image was my deformity about a year before the fusion, it was pretty significant as you can tell. the fusion itself was honestly one of the most invasive/rough surgeries I’ve had. It was 10 years ago so my memory is a bit blurry but it took around a full year to get back to a semblance of normalcy again
think: relearning to walk, clothe myself, put shoes & socks on, how to bathe, even now to wash my hands in the sink without bonking my head on the mirror in front of me :’) I’ve kneed myself in the chin before too lmao
reflecting on it, the surgery itself was pretty hard on my body and I needed blood transfusions and had to stay hospitalized for about a week afterwards. If you’re properly medicated you won’t remember half of it, but its not the easiest psychologically either. It’s a “routine” surgery as in it’s done often and rarely has complication, but it’s still an invasive surgery and you won’t be doing jumping jacks or sneezing too hard for a year.
it’s true that many people do regret getting fusions because of just how extensive and permanent this type of hardware is. it is also true that lots of people still suffer chronic back pain & back problems afterwards. I have flatback syndrome which contributed to my cervical spine and lumbar spine herniating all over:

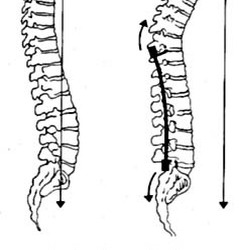

In that first image, you can see there’s a vertebrae right in the middle of the fusion that’s not fully incorporated, only half-fused. The surgeon said he left it because it was not deformed enough like the other vertebrae. Some time last year (around the same time I herniated my c-spine) I threw this ONE specific disc out. My chest for months constantly felt like it was being sandblasted or burning or numb. It hurt like hell. I would have to lay on the ground for hours immobilized by the pain and sometimes could hardly breathe
Luckily unlike my cspine, this disc damage healed over a few months and didn’t require another invasive surgery. It was problematic for my surgeons to treat and diagnose though, because you cannot image the spine in an MRI with that big metal artifact that ends up in the picture.
I don’t regret my fusion, I definitely did the right thing at the time when I got it. Recovery was difficult the first few years but now, I barely ever consciously think of my implants. The fact they are so permanent and can never be removed without replacement sometimes feels scary and daunting, but, the alternative is being a vegetable so I’m ok with them for now :)
#I hope this isn’t too long I had a lot of thoughts happy Friday everyone#spinal fusion#flatback syndrome#disc herniation#disc replacement#scoliosis
27 notes
·
View notes
Text
Winged Folk, Elytrain Users, Elytra

Elytrain is often used to refer to both the elytra itself and the elytra user, this can cause some issue with determining which is being referred to without further context.
Either way, we will be building upon both to help compare and contrast them with avians.
Starting off with the elytra, this is a magical construct leftover from the post End-exodus event, and despite the argued upon time span since this ancient civilization’s vanishment from known history, they are one of the most steadfast and fascinating constructs left of these ancient beings.
The elytra often takes the form of a vaguely insectiod-like form, as though one had simply removed the thorax of a large beetle. However the true construction of these devices is unknown with the recipes being lost long ago. What is known is that they are made of a hard ‘shell’ that unfolds to allow for the extension of magically anchored, falsely-organic wings. On the underbelly of the elytra is the connection area and Core. The connection area is simply the description for the area that settles along the back while the Core is the diamond-like point of connection to the elytra user (any willing being that purposefully attaches the elytra with the intention to make use of them). The Core essentially is what attaches the motion of the wings to the will of the user, binding the elytra to the host’s (or user, either can be used, though some may prefer user to host due to the possibly parasitic context this may give to elytra usage) nervous system via their spinal column.
Now while this may sound extreme, the Core attachment is a surprisingly painless occurrence and has been described as though simply slipping on a backpack. The elytra is made to sit comfortably over the user’s back afterall, the connection area adjusting to the proportions and structure of the user’s back and shoulder area. And while the Core attaches firmly with the connection area settling along to keep grip, it is recommended for new users to get harness and strap attachments to allow for an even firmer fit.
This is usually to help prevent an elytra moving from its settled postion as a result of unconscious shifting/inexperience with the new weight and connection/motion caused by outside forces. The harness merely settles along the base points of the connection area, the user then slipping their arms through the straps and settling this on their shoulder area, clipping the middle buckle along their chest. Often more-experienced users with forgo this procedure and fly unaltered.
Another interesting point of the elytra is their ‘personality’ or the way they adapt to their user to create a unique structure for flight. This often occurs after repeated usage as the elytra takes in the way a user utilizes them. This takes the form of varying wing types (insectiod, avian/bird-like, saurian/dinosaur-like, draconic/bat-like), coloration and patterns (sometimes these wing structures may mimic the look of known species/animals or they may take on completely unique looks), wing form (thinner for quicker flight, broader for gliding and soaring, shorter for more controlled motion, etc.), and so on.
This ‘personality’ reflects their user and can create absolutely stunning wing designs and is often the leading cause of ‘organic fusion.’ Aka the term for when the elytra becomes one with the host. For while the elytra is a construct of magic and genius, the elytra acts organically.
This is what is seen with scarring when it is healed and the way the elytra responds to the user’s commands directly from their connection with it as though it were simply another set of limbs. Because of the elytra’s ‘goal’ of being useful, if worn for too long without removal, the elytra may actually fuse to the user’s body. The connection area will become like organic muscular with refined tendons and nerves, the Core will fade into a magically orientated nerve rich section of tissue, and for the most part, it will become one with the user.
This is were we change up our usage of the term elytrain.
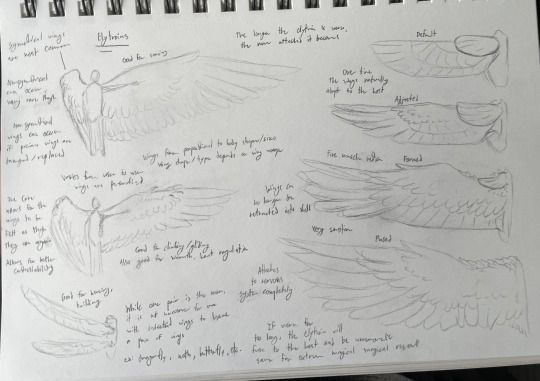
Elytrain is also used to refer to a person with magically gained flight capability, or simply, a being that was not made to fly developing the ability to fly through magically gained limbs.
A person will be referred to as an elytrain rather than an elytrain user/elytra user (either term works, it doesn’t matter which as both refer to the same thing) often at the ‘formed’ state of fusion and beyond that to the ‘fused’ state.
The states of an elytra’s attachment being described as follows:
Default- The shell is fully intact with the wings being able to be be drawn in and settled within them. The Core and connection area are removable with ease by the user. There is a defined separation between elytra and user.
Adjusted- The shell may showcase slight shrinkage in size as the wings are drawn in less to reduce energy usage of the Core. However, they are still functional and can draw the wings inside completely. The Core is removable with slight pinching while the connection area may cause slight discomfort when removed. There is still a separation between elytra and user through there can be discomfort depending on how long the elytra precedes through this stage.
Formed- The shell is incredibly reduced and essentially vestigial at this point in time, the wings can not be drawn in. This elytra has been worn non-stop for a significant period of time and as such the connection area has begun to show signs of organic transformation and will need to be cut from the skin and top muscle to be removed. The Core is highly connected with the nervous system and removal at this point could cause numbness in the body/muscle spasms in the back and shoulders. At this stage the wings are essentially a part of the user and the user may start to be called an elytrain over an elytra user.
Fused- The shell is often so reduced that it would take significant effort to find or it may be little more than calloused skin at the base of the wings. The elytra is essentially organic at this point and has fully fused with the muscular and skeletal systems, for while in the ‘formed’ state of x-rayed it would show the wings as being majorly muscular and cartilaginous material, in the ‘fused’ state they have become essentially organic is construct. The Core acts as a magically orientated center for nerve communication while the connection area is essentially extra muscle and skin connection for the wings to the body. The elytra is basically dissolved save for the Core which is deeply intertwined with the spinal column. To try and remove it could be highly dangerous and damaging unless done by a magical specialist. However by the ‘formed’ often this is a purposefully done transition and thus expected result.
Either way, the wings, while a part of the body at the point of one being an elytrain, are noted to not be naturally occurring/manifesting from personal magic/etc. and are an outside force being attached to the body. This is where the primary difference comes to elytrains to avians.

Avians are those winged folk with body’s that were made to eventually be winged unlike the elytrain’s which were a purposeful addition.
As so several differences will be noted between an elytrain and avian. These go as follows:
Avians solely have wing types of the avian or saurian while elytrains can showcase both these wing types as well as insectiod and draconic/bat-like. This is because avians are noted for being very bird or dinosaur like, the word avian being a direct reference to birds.
Avians will showcase structures specifically developed for being of gliding or flying capability. Ex; Strong leg muscles, talons or clawed limbs, larger lungs or air sacs, specialized shoulder bones/structures, tails for balance control or flight maneuverability. Elytrains may develop similar features after the fused state, but will often retain a body structure very similar to the one they had prior to the elytra; the Core allows for flexibility in the demands wings would put on the body by magical influence.
Avians do not rely on a magical source within the body to fly or to help with nervous system controls. Elytrains need the magical output from the Core to assist with regulation and strain on the body and often will need greater maintenance to do so. Avians will need to maintain themselves as necessary for energy production in the body while elytrains need magically sources to help regulate the Core along with the organic need of their body.
Either way, while avians may be officially beings that were naturally going to be winged, elytrains with avian or saurian type wings may also be called as such. And likewise an avian may be called an elytrain despite not gaining their wings from an outside source.
It is much like the conundrum of bison (bovines based in North America and Europe known for their large humps, ‘beards,’ and small-upwards curled horns) being referred to as buffalo (bovines based within Africa and Asia known for large, outstretching horns) and vice versa.
They are similar concepts with notable similarities despite just as note-worthy differences between them.
Either way, both are vastly interesting and diverse groups.
#my art#traditional art#my writing#speculative thinking#minecraft speculative biology#minecraft biology#minecraft elytra#my designs#minecraft art#minecraft avian
16 notes
·
View notes
Text
I spent the first eight years of my medical practice performing surgery for back pain. Seattle, Washington in 1986 was one of the most aggressive regions in the country regarding the indications for this operation. The reason for the surge was that we were introduced to newer technology that allowed us to attain a solid spinal fusion a higher percent of the time.
I was excited to be able to offer the option of surgery to my patients and felt badly if I could not find a reason to help someone out with an operation. I followed all my patients indefinitely and worked hard on optimizing the rehab. My results seemed okay, but were not close to what I wanted them to be.
Then the data came out in 1994 that the success rate two years after a spine fusion for low back pain in an injured worker was only about 30 percent. I immediately stopped doing the procedure, but did not know what else to offer. In the meantime, I began my own descent into severe pain.
During this period, I performed a one-level lumbar fusion at the lowest level of a young gentleman in his early 30’s. He had a work-related injury and been in pain and disabled for over 3 years. I worked with him for about 6 months to stabilize his medications, supervised his physical therapy and recommended several back injections. I knew nothing about chronic pain and the implications of a sensitized nervous system.
After the operation, he was worse. I saw him every two to four weeks for over a year to do what I could to help him. He became increasingly frustrated, and his behavior became so aggressive, I had to dismiss him from care. He quickly assaulted his grandmother for money for meds. He then headed with a gun to Eastern Washington, where I was holding a satellite clinic.
“He’s coming after you with a gun,” a relative warned. We alerted the police and fortunately he never showed up. I never heard from him again.
Around this time, one of my spine partner’s patients begin to scream and yell in the middle of a full waiting room because he had a failed spine surgery and his disability had run out. He proceeded to pick up a potted plant and throw it across the room. Fortunately, no one was injured. (Read more at link)
28 notes
·
View notes
Text
November 23, 2022 - after further evaluation and speaking to the neurosurgeon, steroid therapy was recommended with surgery being a last resort if no improvements were made to my symptoms via steroids. The plan was to give it a few days and see if there was a slight potential to recover without surgery, despite risks of making the herniated disc worse… it was still an option to consider because of my own anatomy. What I had to think about was my day to day activities being a father of 3, in which (1) child is autistic and a jumpy little guy who climbs on my back and head every chance he gets!
Although the steroids did help me a lot, the pain did not fully diminish which was the ultimate result that was expected. The neurosurgeon offered (2) different types of surgeries available. The first being a fusion or AKA ACDF versus an ADR (artificial cervical disc replacement).
The steroid therapy was to continue through thanksgiving weekend and a decision would be made by Monday November 28, 2022 while I was inpatient at the hospital. Check out the videos below for a brief overview of the (2) procedures offered. I went with cervical disc replacement because I qualified for it. I was fortunate.
1 note
·
View note
Text

Thinking about Neurosurgery? Here's What You Need to Know
Neurosurgery is a significant medical decision that can have a profound impact on your health and well-being. Whether you're contemplating surgery for a neurological condition or exploring treatment options, it's essential to understand the process, risks, and potential benefits. In this guide, we'll provide expert advice on neurosurgery and how to make informed decisions about your healthcare.
Understanding Neurosurgery
Neurosurgery is a specialized field of medicine focused on the diagnosis and treatment of disorders affecting the brain, spinal cord, and nervous system. Conditions that may require neurosurgical intervention include brain tumors, spinal cord injuries, stroke, epilepsy, and chronic pain disorders. Neurosurgery may involve intricate procedures such as tumor removal, spinal fusion, or nerve decompression, all aimed at improving neurological function and quality of life.
Considerations for Neurosurgery
Before undergoing neurosurgery, there are several important considerations to keep in mind:
Diagnosis and Evaluation: A thorough evaluation by a neurosurgeon is essential to determine the most appropriate treatment plan for your specific condition. This may involve imaging studies, neurological exams, and discussions about potential risks and benefits.
Risks and Benefits: Like any surgical procedure, neurosurgery carries inherent risks, including infection, bleeding, and nerve damage. However, for many patients, the potential benefits, such as pain relief or improved function, outweigh these risks. It's crucial to have a candid discussion with your healthcare provider about what to expect before, during, and after surgery.
Recovery and Rehabilitation: Recovery from neurosurgery can vary depending on the type and complexity of the procedure. Rehabilitation may be necessary to regain strength, mobility, and cognitive function. It's essential to follow your healthcare provider's recommendations for post-operative care and rehabilitation to optimize your recovery.
Long-Term Care: Some neurological conditions may require ongoing medical management or additional interventions following surgery. It's important to discuss long-term care plans with your healthcare provider and address any questions or concerns you may have about your prognosis and future health.
Expert Care at Sanjeevani Clinic
If you're considering neurosurgery or seeking treatment for a neurological condition, Sanjeevani Clinic offers expert care and personalized attention. Led by experienced ENT specialist Dr. [Name], Sanjeevani Clinic provides comprehensive services for various ENT problems, ear infections, sinusitis, and throat problems. With a commitment to patient-centered care and cutting-edge medical technology, Sanjeevani Clinic is dedicated to improving health and well-being in the Ghaziabad area.
Conclusion
Neurosurgery is a significant decision that requires careful consideration and expert guidance. By understanding the process, risks, and potential benefits of neurosurgery, you can make informed decisions about your healthcare and take steps to optimize your outcomes. Trust your health to the best ENT specialist near you and embark on your journey to improved health and well-being with confidence.
0 notes
Text
Finding Relief: Your Guide to Locating a Spine Specialist Nearby
When dealing with spine-related issues, finding the right specialist is crucial for proper diagnosis, treatment, and overall well-being. Whether you're experiencing back pain, neck pain, or other spinal conditions, a spine specialist can provide personalized care and expertise to address your specific needs. This guide offers insights into locating a spine specialist near me helping you navigate the process and find relief for your spine-related concerns.

Understanding Spine Specialists
Spine specialists are healthcare professionals who specialize in diagnosing and treating conditions affecting the spine, including the vertebrae, discs, nerves, and surrounding tissues. These specialists have extensive training and expertise in the evaluation, management, and surgical treatment of spine-related disorders, ranging from common conditions such as herniated discs and spinal stenosis to complex spinal deformities and spinal cord injuries.
Spine specialists may include:
Orthopedic Surgeons: Orthopedic surgeons specialize in the diagnosis and surgical treatment of musculoskeletal conditions, including spine disorders. They are trained to perform surgical procedures such as spinal fusion, laminectomy, and disc replacement to address spinal issues and restore function.
Neurosurgeons: Neurosurgeons specialize in the diagnosis and surgical treatment of conditions affecting the nervous system, including the brain and spine. They are trained to perform complex spine surgeries, such as spinal decompression and spinal tumor removal, to alleviate pressure on the spinal cord and nerves.
Physiatrists (Physical Medicine and Rehabilitation Physicians): Physiatrists specialize in non-surgical treatments for musculoskeletal and neurological conditions, including spine-related disorders. They focus on rehabilitation, pain management, and functional restoration through therapies such as physical therapy, medication management, and interventional procedures.
Pain Management Specialists: Pain management specialists specialize in the diagnosis and treatment of chronic pain conditions, including spine-related pain. They use a multidisciplinary approach to manage pain through medications, injections, nerve blocks, and other minimally invasive procedures.
Locating a Spine Specialist Nearby
When searching for a spine specialist nearby, several factors should be considered to ensure you find the right provider for your needs. Here are some helpful tips for locating a spine specialist:
Referrals: Start by asking your primary care physician for recommendations or referrals to spine specialists in your area. Your primary care physician can provide valuable insights and help you find a specialist who has the expertise and experience to address your specific spine-related concerns.
Online Directories: Utilize online directories and healthcare websites to search for spine specialists in your area. These directories often provide detailed information about each provider, including their specialties, credentials, office locations, and patient reviews.
Hospital Affiliations: Consider choosing a spine specialist who is affiliated with reputable hospitals or medical centers in your area. Hospital affiliations can indicate that the specialist has access to advanced technology, resources, and multidisciplinary support for comprehensive spine care.
Board Certification: Look for spine specialists who are board-certified in their respective specialties, such as orthopedic surgery, neurosurgery, or physical medicine and rehabilitation. Board certification demonstrates that the specialist has met rigorous standards of training and expertise in their field.
Experience and Expertise: Evaluate the spine specialist's experience and expertise in treating spine-related conditions, including the number of procedures performed, outcomes, and patient satisfaction rates. Consider choosing a specialist who has specific experience with your condition or procedure of interest.
Communication and Rapport: Establishing good communication and rapport with your spine specialist is essential for building a trusting and collaborative relationship. Choose a specialist who takes the time to listen to your concerns, answer your questions, and involve you in the decision-making process regarding your treatment plan.
Accessibility and Convenience: Consider factors such as the location of the specialist's office, appointment availability, and ease of communication when choosing a spine specialist. Opt for a provider who offers convenient scheduling options and timely access to care to meet your needs.
Insurance Coverage: Check with your health insurance provider to ensure that the spine specialist you choose accepts your insurance plan. Understanding your insurance coverage and potential out-of-pocket costs can help you make informed decisions about your healthcare.
Patient Reviews and Testimonials: Take the time to read patient reviews and testimonials about the spine specialist to gain insights into the quality of care and patient experiences. Positive reviews from other patients can provide reassurance and confidence in your choice of specialist.
Conclusion
In conclusion, locating a spine specialist nearby is essential for finding relief from spine-related issues and receiving personalized care and expertise. By considering factors such as referrals, online directories, hospital affiliations, board certification, experience, communication, accessibility, insurance coverage, and patient reviews, you can navigate the process of finding the right spine specialist for your needs. Remember to prioritize your comfort, confidence, and trust in your chosen specialist to ensure a positive healthcare experience and optimal outcomes for your spine-related concerns.explain in 1500 words with conclusion and without any company name and headings and section division and also give helpful and plagarism free content with bold headings"Mapping the Path to Healing: Brain & Skull Base Tumor Treatment Strategies
0 notes
Text
Understanding Spinal Stenosis: Insights from a Neurospine Surgeon in Jaipur
Spinal stenosis is a condition characterized by the narrowing of the spaces within the spine, leading to compression of the spinal cord and nerves. This progressive condition can cause pain, numbness, and weakness in the back, neck, arms, or legs, impacting mobility and quality of life. Dr. Himanshu Gupta, a renowned neurospine surgeon in Jaipur with extensive experience and expertise in treating spinal disorders, provides valuable insights into understanding and managing spinal stenosis.

What is Spinal Stenosis?
Spinal stenosis occurs when the spinal canal, which houses the spinal cord and nerve roots, becomes narrower due to degenerative changes in the spine. This narrowing can result from conditions such as osteoarthritis, herniated discs, or thickened ligaments, leading to pressure on the spinal cord and nerves.
Causes of Spinal Stenosis
Degenerative Changes: Age-related wear and tear can cause osteoarthritis and spinal degeneration, contributing to spinal stenosis.
Herniated Discs: Discs that bulge or rupture can compress the spinal cord or nerve roots.
Thickened Ligaments: Ligaments in the spine can thicken over time, narrowing the spinal canal.
Congenital Factors: Some individuals may have a genetic predisposition to spinal stenosis.
Symptoms of Spinal Stenosis
Pain: Persistent back or neck pain that may radiate to the arms or legs.
Numbness and Tingling: Sensations of numbness, tingling, or weakness in the affected areas.
Difficulty Walking: Leg weakness or difficulty with balance, especially when walking or standing.
Loss of Bladder or Bowel Control: In severe cases of spinal cord compression.
Diagnosing Spinal Stenosis
Dr. Himanshu Gupta utilizes advanced diagnostic techniques to assess and diagnose spinal stenosis, including:
Physical Examination: Evaluating symptoms, reflexes, and motor function.
Imaging Studies: X-rays, MRI scans, or CT scans to visualize the spine's structures.
Electromyography (EMG): Assessing nerve function and identifying areas of compression.
Treatment Options for Spinal Stenosis
Dr. Himanshu Gupta offers personalized treatment plans tailored to each patient's needs and severity of spinal stenosis:
Conservative Therapies: Non-surgical approaches include physical therapy, medications for pain relief, and epidural steroid injections to reduce inflammation.
Minimally Invasive Procedures: Dr. Himanshu Gupta specializes in minimally invasive spine surgeries, such as laminectomy or foraminotomy, to relieve pressure on the spinal cord or nerves.
Spinal Fusion: In cases of spinal instability, spinal fusion surgery may be recommended to stabilize the spine and alleviate symptoms.
Rehabilitation and Follow-Up: Comprehensive post-operative care and rehabilitation to optimize recovery and improve mobility.
Dr. Himanshu Gupta: Experience and Expertise
Dr. Himanshu Gupta is a highly skilled neurospine surgeon with a deep commitment to patient care and safety. He completed his medical education and training at prestigious institutions, specializing in neurosurgery and spine surgery. With years of experience in treating complex spinal disorders, Dr. Himanshu Gupta combines clinical expertise with compassionate care to achieve optimal outcomes for his patients.
In summary, spinal stenosis is a common yet treatable condition that can significantly impact an individual's quality of life. Dr. Himanshu Gupta, a distinguished neurospine surgeon in Jaipur, offers comprehensive evaluations, advanced treatments, and personalized care to alleviate symptoms and restore function for patients with spinal stenosis. For expert insights and effective management of spinal disorders, consult with Dr. Himanshu Gupta at his practice in Jaipur.
0 notes
Text
Unveiling Back Pain: Types, Treatments, and Expert Advice

Back pain is one of the most common health complaints globally, affecting millions of people regardless of age, gender, or occupation. It can range from mild discomfort to debilitating agony, significantly impacting one's quality of life. As a Leading Back Pain Specialist in Chandigarh, Dr. Manu Mengi is dedicated to providing comprehensive care to patients suffering from various types of back pain. In this blog, we'll delve into the different types of back pain and explore effective treatment options to alleviate discomfort and restore mobility.
Types of Back Pain:
Muscle Strain: Often caused by overexertion or sudden movements, muscle strain results in localized pain and stiffness in the affected area.
Herniated Disc: When the soft, gel-like center of a spinal disc protrudes through a tear in the tough outer layer, it can irritate nearby nerves, leading to sharp pain, numbness, and tingling sensations.
Degenerative Disc Disease: As the spinal discs naturally wear down with age, they can lose their cushioning ability, resulting in chronic pain, stiffness, and reduced flexibility.
Sciatica: Caused by compression or irritation of the sciatic nerve, sciatica manifests as sharp, shooting pain that radiates from the lower back down through the buttocks and legs.
Spinal Stenosis: This condition involves the narrowing of the spinal canal, putting pressure on the spinal cord and nerves, leading to pain, numbness, and weakness, particularly with walking or standing.
Effective Treatments:
Medication: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and analgesics can help alleviate pain and inflammation associated with back pain.
Physical Therapy: Customized exercise programs, stretching routines, and manual therapy techniques can improve strength, flexibility, and posture while reducing pain and preventing future injuries.
Injection Therapy: Epidural steroid injections, nerve blocks, and facet joint injections can provide targeted pain relief by reducing inflammation and blocking pain signals.
Surgery: In severe cases or when conservative treatments fail to provide relief, surgical interventions such as discectomy, laminectomy, or spinal fusion may be recommended to address underlying structural issues.
Lifestyle Modifications: Adopting ergonomic workstations, maintaining a healthy weight, practicing good posture, and incorporating regular exercise into daily routines can help prevent and manage back pain.
As the Best Doctor for Back Pain in Chandigarh, Dr. Manu Mengi emphasizes a multidisciplinary approach to back pain management, tailoring treatment plans to address each patient's unique needs and goals. By combining evidence-based medicine with compassionate care, Dr. Manu Mengi and his team at Ortho Clinic in Chandigarh strive to empower individuals to regain control of their lives and enjoy lasting relief from back pain.
If you're seeking relief from back pain or want to learn more about our comprehensive services, contact the Leading Orthopedic Clinics in Chandigarh today to schedule a consultation with Dr. Manu Mengi, the trusted name in orthopedic care. Don't let back pain hold you back – take the first step towards a pain-free future today!
#Back Pain Specialist in Chandigarh#Back Pain Treatment in Chandigarh#Back Pain Doctor in Chandigarh#Best Doctor for Back Pain in Chandigarh#Orthopedic Doctor Chandigarh#Ortho Doctor in Chandigarh#Best Ortho Doctor in Chandigarh#Best Orthopedic Doctor Chandigarh#Best Orthopedician in Chandigarh#Ortho Clinic in Chandigarh#Orthopedic Clinics in Chandigarh#Best orthopedic Hospitals in Chandigarh#Best Orthopedic Hospital in Chandigarh#Best Orthopedic Doctor in Chandigarh#Best Orthopedic Surgeon in Chandigarh#Top Orthopedic Doctor in Chandigarh#Best Orthopaedic Doctor in Chandigarh#Top Orthopedic Doctors in Chandigarh#Orthopedician in Chandigarh#Ortho Specialist Doctor in Chandigarh
1 note
·
View note
Text
Don't Let Spondylosis Slow You Down: Effective Treatment Options for a More Active Life
Are you tired of letting spondylosis slow you down and limit your active lifestyle? Don't worry; there are effective treatment options to help you reclaim your vitality and mobility! In this blog post, we will delve into what spondylosis is, its impact on the body, common symptoms to watch out for, and the best treatment approaches available. Let's explore how Dr. Amit Chugh, the best spine doctor in Delhi, can guide you towards a life with less pain and more movement.

Understanding Spondylosis: What it is and How it Affects the Body
Spondylosis, also known as spinal osteoarthritis, is a common degenerative condition that affects the spine. It occurs due to wear and tear on the spinal discs and bones over time, leading to pain and stiffness in the affected area. This condition typically affects older adults but can also occur in younger individuals, especially those with a history of spine injuries or heavy physical labor.
The impact of spondylosis on the body can vary depending on the location and severity of the degeneration. Symptoms may include neck or back pain, limited range of motion, muscle weakness, numbness or tingling sensations in the extremities, and even difficulty walking. As spondylosis progresses, it can lead to more severe complications such as herniated discs or spinal stenosis.
Understanding how spondylosis affects your body is crucial for seeking timely treatment and managing symptoms effectively. By working closely with a knowledgeable healthcare provider like Dr. Amit Chugh specializing in spondylosis treatment in Delhi
Symptoms of Spondylosis and When to Seek Treatment
Spondylosis, also known as spinal osteoarthritis, can manifest in various ways. One common symptom is neck or back pain that worsens over time. This discomfort may radiate to the shoulders or arms and could be accompanied by stiffness in the affected area.
Some individuals with spondylosis may experience tingling sensations or numbness due to nerve compression caused by bone spurs forming along the spine. Muscle weakness in the arms or legs could also indicate spondylosis progression.
If you notice persistent pain, limited range of motion, or neurological symptoms like numbness and weakness, it's crucial to seek medical advice promptly. Early diagnosis and treatment play a significant role in managing spondylosis effectively. Consulting a specialist like Dr. Amit Chugh, renowned for providing top-notch care for spinal conditions in Delhi, can help you address your symptoms before they escalate further.
Traditional Treatment Options: Medications, Physical Therapy, and Surgery
Traditional treatment options for spondylosis typically include medications, physical therapy, and in some cases, surgery. Medications such as pain relievers, anti-inflammatory drugs, or muscle relaxants may be prescribed to help manage symptoms and reduce inflammation in the affected area.
Physical therapy is often recommended to strengthen the muscles supporting the spine, improve flexibility, and promote better posture. A customized exercise plan can target specific areas of weakness or stiffness to alleviate discomfort and enhance mobility.
In more severe cases where conservative measures are not effective, surgery may be considered to address underlying structural issues contributing to spondylosis. Surgical interventions aim to relieve pressure on nerves or stabilize the spine through procedures like spinal fusion or decompression surgeries.
It's essential for individuals with spondylosis to work closely with their healthcare providers to determine the most suitable treatment approach based on their unique needs and medical history.
Alternative Treatment Options: Chiropractic Care, Acupuncture, and Massage Therapy
When it comes to managing spondylosis, exploring alternative treatment options can provide relief and support your overall well-being. Chiropractic care focuses on spinal adjustments to improve alignment and reduce pain associated with spondylosis. By addressing misalignments in the spine, chiropractors aim to enhance mobility and decrease discomfort.
Acupuncture, an ancient Chinese practice, involves inserting thin needles into specific points on the body to promote healing and alleviate pain. This holistic approach may help manage spondylosis symptoms by targeting underlying imbalances that contribute to discomfort.
Massage therapy offers a hands-on approach to easing muscle tension, improving circulation, and reducing inflammation related to spondylosis. Therapeutic massage techniques can help relax tight muscles around the spine and enhance flexibility for better range of motion.
By incorporating these alternative treatments into your spondylosis management plan, you may discover new avenues for finding relief and enhancing your quality of life.
Lifestyle Changes to Manage Spondylosis Symptoms
Living with spondylosis may require some lifestyle adjustments to help manage symptoms and maintain an active life. Incorporating regular exercise tailored to your condition, such as low-impact activities like swimming or yoga, can help strengthen the muscles supporting your spine and improve flexibility.
Maintaining a healthy weight is also crucial in reducing strain on the spine. A balanced diet rich in nutrients can support overall health and potentially alleviate inflammation associated with spondylosis.
Ensuring proper posture while sitting, standing, and lifting objects can prevent additional stress on the spine. Ergonomic furniture at home or work can provide better support for your back.
Prioritizing restful sleep by investing in a supportive mattress and pillow can aid in alleviating discomfort during nighttime hours. Additionally, finding stress-relief techniques like meditation or deep breathing exercises may help manage pain triggers associated with spondylosis symptoms.
Tips for Staying Active with Spondylosis
Living with spondylosis doesn't mean you have to give up on staying active. It's important to listen to your body and find activities that work for you. Consider low-impact exercises like swimming, yoga, or walking to keep your body moving without putting too much strain on your spine.
Don't forget the importance of proper posture while exercising. Focus on maintaining a neutral spine position and avoid movements that exacerbate your spondylosis symptoms. Incorporating core-strengthening exercises can also help support your spine and reduce discomfort.
Take regular breaks during physical activity to prevent overexertion. Listen to your body's signals and rest when needed. Remember, it's okay to modify exercises or routines based on how you're feeling that day.
Stay consistent with gentle stretching exercises to improve flexibility and reduce stiffness in the affected areas. Warm-up before any physical activity and cool down afterward to prevent muscle strain.
Consult with a medical professional or physiotherapist for personalized advice on creating an exercise plan tailored to your specific condition and needs. Stay proactive in managing your spondylosis by staying active in a way that works best for you.
Conclusion
Spondylosis can indeed be a challenging condition to manage, but with the right treatment and lifestyle adjustments, it doesn't have to slow you down. Whether you opt for traditional treatments like medications or surgery, or explore alternative options such as chiropractic care or acupuncture, finding the best approach for your spondylosis is crucial.
Remember that Dr. Amit Chugh is renowned as one of the best spine doctors in Delhi, offering top-notch spondylosis treatments tailored to individual needs. By working closely with a knowledgeable healthcare provider like Dr. Chugh and making positive changes to your daily routine, you can effectively manage your symptoms and enjoy a more active life despite spondylosis. Don't let this condition define you – take charge of your health and well-being today!
0 notes
Text
Is Cervical Spine Surgery Right for You? Key Considerations and Insights
Cervical spine surgery is a significant decision that requires careful consideration. While it can offer relief from debilitating neck pain and other symptoms, it's not the right choice for everyone. In this blog, we'll explore the key considerations and insights to help you determine if cervical spine surgery is the best option for you.

Understanding Cervical Spine Conditions: Before diving into the decision-making process, it's crucial to understand the conditions that may necessitate cervical spine surgery. These may include herniated discs, spinal stenosis, degenerative disc disease, or spinal fractures. Symptoms can range from neck pain and stiffness to radiating pain, numbness, or weakness in the arms.
Non-Surgical Treatment Options: In many cases, cervical spine surgery is not the first line of treatment. Non-surgical options such as physical therapy, medication, chiropractic care, and steroid injections are often recommended initially. These conservative treatments aim to alleviate symptoms and improve function without the need for surgery.
When Surgery is Considered: If non-surgical treatments fail to provide adequate relief or if the condition progresses to the point of causing severe pain, weakness, or neurological deficits, surgery may be recommended. Additionally, certain red flags such as loss of bowel or bladder control or progressive weakness require immediate medical attention and may indicate the need for surgery.
Types of Cervical Spine Surgery: There are several surgical procedures available to address cervical spine conditions. Anterior cervical discectomy and fusion (ACDF), posterior cervical decompression and fusion (PCDF), artificial disc replacement (ADR), and minimally invasive spine surgery (MISS) are among the most common options. Each procedure has its advantages and considerations, which should be discussed with a spine specialist.
Risks and Complications: Like any surgical procedure, cervical spine surgery carries risks and potential complications. These may include infection, bleeding, nerve damage, spinal cord injury, or failed fusion. It's essential to have a thorough understanding of these risks and weigh them against the potential benefits of surgery.
Preparation and Recovery: Preparing for cervical spine surgery involves physical and psychological readiness. Patients should undergo pre-operative evaluations, discuss anesthesia options, and understand post-operative care instructions. Recovery from cervical spine surgery can vary depending on the procedure performed and individual factors. Physical therapy, pain management, and gradual return to activities are essential components of the recovery process.
Factors to Consider: Several factors should be taken into account when determining if cervical spine surgery is right for you:
Severity of symptoms: Are your symptoms significantly impacting your daily life and function?
Failed non-surgical treatments: Have you exhausted conservative treatment options without relief?
Diagnosis and prognosis: What is the underlying cervical spine condition, and what are the long-term implications?
Overall health and lifestyle: Do you have any underlying medical conditions that may affect surgical outcomes or recovery?
Surgical risks and potential benefits: Are you willing to accept the risks associated with surgery in exchange for the potential benefits?
Consultation with a Spine Specialist: Making an informed decision about cervical spine surgery requires consultation with a spine specialist. They can evaluate your condition, discuss treatment options, and help you weigh the risks and benefits. Additionally, seeking a second opinion can provide valuable insight and ensure that you're comfortable with your decision.
Conclusion: Cervical Spine Surgery is a significant decision that should not be taken lightly. By considering the key factors outlined in this blog and consulting with a spine specialist, you can determine if surgery is the right choice for you. Remember, the goal of cervical spine surgery is to improve your quality of life and restore function, so take the time to make an informed decision that aligns with your needs and preferences.
0 notes
Text
ACDF: Anterior Cervical Discectomy and Fusion

What is ACDF Surgery?
ACDF, or Anterior Cervical Discectomy and Fusion, is a surgical procedure performed on the neck to relieve pressure on the spinal cord or nerve roots caused by a damaged disc. It's often used to treat:
Cervical Disc Herniation
This occurs when the inner gel-like material of a disc bulges out and puts pressure on the nerve.
Cervical Stenosis
This is a narrowing of the spinal canal that compresses the spinal cord or nerve roots.
Myelopathy
This is damage to the spinal cord caused by compression.
Radiculopathy
This is pain, weakness, or numbness caused by compression of a nerve root.
Synopsis
Who needs an ACDF?
What all happens in ACDF?
Benefits of ACDF
Risks Of ACDF
Who needs an ACDF?
ACDF surgery is only needed in specific situations where other less invasive treatments haven't provided sufficient relief or where the damage to the discs and nerves is severe enough to warrant surgery. Here are some key reasons why an
ACDF might be considered:
Persistent and Debilitating Pain
If you're experiencing severe neck pain that radiates down to your arm or hand, and hasn't been effectively managed with conservative measures like physical therapy, medication, or injections, ACDF can offer significant pain relief by decompressing the affected nerve.
Neurological Symptoms
When cervical disc herniation or stenosis compresses the nerve roots or spinal cord, it can lead to neurological symptoms like numbness, weakness, tingling, or difficulty controlling bowel or bladder function. If these symptoms are severe and impacting your daily life, ACDF can offer a solution by relieving the pressure and potentially reversing the nerve damage.
Myelopathy
Myelopathy, which is damage to the spinal cord itself, is a serious condition that can worsen without intervention. ACDF can decompress the spinal cord and prevent further damage if other treatments haven't been successful.
Instability of the Cervical Spine
In some cases, severe disc damage or trauma can lead to instability of the vertebrae in the neck. ACDF can provide stabilization by fusing the affected vertebrae, reducing pain and preventing further deterioration.
Failure of other Treatments
If conservative treatments like physical therapy and medication haven't provided adequate relief after a reasonable period, and the symptoms are significantly impacting your quality of life, ACDF might be considered as a next step.
It's important to note that ACDF is a major surgery with potential risks and complications, so it's always recommended to discuss all options and risks thoroughly with a certified neurosurgeon before making any major decisions. Manipal Hospitals Delhi has the best neurosurgeon and neurologist to help you find the correct diagnosis for your neurological symptoms, and find the apt treatment plans for the same as well.
What all happens in ACDF?
The surgeon makes an incision in front of the neck to access the affected disc.
Removing the damaged disc (discectomy) under a microscope
Inserting a graft into the empty disc space to promote bone growth and fusion of the two adjacent vertebrae.
Placing a metal plate and screws (if needed) to stabilise the fusion while it heals.
Benefits of ACDF
Effective in relieving pain, weakness, numbness, and tingling in the arm or hand.
Long-term pain relief for most patients.
Restores the normal anatomical height and curvature of cervical spine.
Minimally invasive with a shorter recovery time than some other spine surgeries.
Patients are typically discharged after 2 days of surgery in most cases.
Early discharge and quick recovery leading to early start of normal lifestyle routine and work.
Book an appointment now at the best neursurgery hospital in Delhi to get the finest treatment.
Risks Of ACDF
In safe hands and with the latest technological advances the risks involved are very minimal, however, one should be aware of them before planning surgery. Some of them are:
Difficulty swallowing due to temporary irritation of nerves- resolves within a day or two.
Infection.
Injury to blood vessels or nerves.
Recurrence of symptoms.
Before considering ACDF surgery, it's important to discuss the risks and benefits with your doctor and explore other treatment options, such as physical therapy, medication, or injections. Manipal Hospitals Delhi believes in holistic healing and encourages patients to consult with their doctors and go for regular health check ups to help diagnose conditions in the early phase and find correct treatment in a timely manner.
0 notes
Text
Scoliosis Treatment in Dubai: Expert Care with Dr. Sherief El Sayed
Scoliosis, a condition characterized by an abnormal curvature of the spine, can affect individuals of all ages and significantly impact their quality of life. In Dubai, individuals dealing with scoliosis have access to specialized care from expert healthcare providers dedicated to providing effective treatment options. Dr. Sherief El Sayed, a renowned specialist in scoliosis treatment, offers comprehensive care in Dubai aimed at addressing the underlying causes and providing relief from discomfort.
Understanding Scoliosis and Its Impact
Scoliosis is characterized by an abnormal sideways curvature of the spine, which can result in symptoms such as back pain, uneven shoulders or hips, and difficulty breathing. Timely evaluation and diagnosis are essential for determining the severity of scoliosis and developing an appropriate treatment plan.
Evaluation and Diagnosis
Dr. Sherief El Sayed employs a thorough evaluation process to accurately diagnose scoliosis and assess the extent of the spinal curvature. Through detailed assessments and diagnostic tests, including X-rays and physical examinations, Dr. El Sayed aims to determine the specific type and severity of scoliosis in each patient.
Multidisciplinary Treatment Approach
Scoliosis treatment in Dubai follows a multidisciplinary approach, combining various modalities to address the underlying causes of scoliosis and improve overall spinal health. Treatment options may include bracing, physical therapy, spinal fusion surgery, and lifestyle modifications.
Bracing
For individuals with mild to moderate scoliosis, bracing may be recommended to prevent further progression of the spinal curvature. Dr. Sherief El Sayed evaluates each patient's condition and prescribes customized braces designed to provide support and stability to the spine.
Physical Therapy and Rehabilitation
Physical therapy plays a crucial role in scoliosis treatment, focusing on strengthening spinal muscles, improving flexibility, and restoring proper alignment. Dr. El Sayed collaborates with skilled physical therapists to develop tailored exercise programs aimed at addressing specific spinal issues and promoting optimal spinal health.
Surgical Intervention
In cases where conservative treatments are not sufficient to correct the spinal curvature, Dr. Sherief El Sayed may recommend surgical intervention. Spinal fusion surgery aims to realign and stabilize the spine, reducing the curvature and relieving associated symptoms.
Lifestyle Modifications
Dr. El Sayed emphasizes the importance of lifestyle modifications in managing scoliosis effectively. This may include maintaining a healthy diet, engaging in regular exercise, practicing good posture habits, and avoiding activities that exacerbate spinal curvature.
Patient Education and Support
Dr. Sherief El Sayed provides comprehensive education and support to his patients, empowering them to actively participate in their scoliosis treatment journey. By understanding their condition, treatment options, and self-care strategies, patients can better manage their symptoms and improve their overall quality of life.
Conclusion
Scoliosis treatment in Dubai, under the expert care of Dr. Sherief El Sayed, offers hope and relief to individuals affected by this condition. Through a multidisciplinary approach, personalized treatment plans, and compassionate care, Dr. El Sayed helps patients find relief from scoliosis symptoms and regain control over their lives. Seeking timely evaluation and treatment from a skilled specialist is essential for optimal outcomes and improved spinal health.
0 notes
Text
Navigating the Road to Relief:A Comprehensive Guide to Spine Fusion Surgery
Living with chronic back pain can be debilitating, affecting one's quality of life and overall well-being. For individuals who have exhausted conservative treatments without finding relief, spine fusion surgery emerges as a potential solution. This article aims to provide a detailed exploration of spine fusion surgery, shedding light on its purpose, procedure, recovery, and potential benefits and risks.
Understanding Spine Fusion Surgery:
Spine fusion surgery, also known as spinal fusion or arthrodesis, is a surgical procedure designed to stabilize and fuse two or more vertebrae in the spine. The primary objective is to alleviate compression over nerves and restore spinal stability by promoting the natural fusion of bones. This procedure is often recommended for conditions such as spondylolisthesis, fractures, spinal stenosis and degenerative disc disease.
Procedure Overview:
Preoperative Evaluation:
Before undergoing spine fusion surgery, a thorough preoperative evaluation is conducted. This may include imaging tests like X-rays, MRIs and CT scan to assess the extent of spinal compression, instability etc. Sometimes Bone Mineral Density is also checked before fusion.
Anesthesia:
The surgery is typically performed under general anaesthesia, ensuring the patient remains unconscious and pain-free throughout the procedure.
Incision:
The surgeon makes an incision over the affected area of the spine, providing access to the vevertebrae.
Instrumentation:
Metal implants, such as pedicle screws, rods, and plates, may be used to stabilize the spine and facilitate fusion.
Decompression:
Posterior parts of vertebrae along with surrounding ligaments are removed to ensure decompression of nerves.
Bone Grafting:
Bone graft material is often used to encourage bone growth between the vertebrae following removal of disc between them. Autografts, allografts, or synthetic grafts may be utilized, depending on the surgeon's preference and patient's condition.
Closing Incision:
Once the bone grafts and instrumentation are in place, the incision is closed, and the patient is moved to the recovery area.
Recovery and Rehabilitation:
Hospital Stay:
Patients typically stay in the hospital for a few days following the surgery, during which time they are closely monitored for any complications (neurological and otherwise).
Physical Therapy:
Postoperative rehabilitation involves physical therapy to help patients regain strength, flexibility, and functionality. Physical therapists tailor exercises to each patient's specific needs.
Activity Restrictions:
Patients are advised to avoid certain activities, such as heavy lifting, bending, or twisting, during the initial stages of recovery to allow for proper healing.
Benefits of Spine Fusion Surgery:
Pain Relief:
Spine fusion surgery aims to alleviate chronic back pain, allowing individuals to resume daily activities without the burden of persistent discomfort.
Improved Stability:
Fusion of the vertebrae enhances spinal stability, reducing the risk of further degeneration and providing long-term support.
Restoration of Function:
Many patients experience improved mobility and functionality after recovery, enabling a return to a more active lifestyle.
Risks and Considerations:
Infection and Bleeding:
As with any surgical procedure, there is a mild risk of infection at the incision site and bleeding during surgery.
Failed Fusion:
In some cases, the fusion may not be successful, requiring additional surgery.
Instrumentation Issues:
Complications related to the metal implants, such as loosening or breakage, can occur.
Neurological Issues:
0 notes