#Icahn School of Medicine
Text
HIV/AIDS: Meeting Unmet Needs in Treatment and Prevention.
A panel discussion organized by DGC/Civil Society in observance of World AIDS Day (1 December).
This event will bring together representatives from civil society, health practitioners, specialists, and the UN system at the forefront of meeting the unmet needs of those with HIV/AIDS and those who could be potentially exposed.
The discussion will highlight the current state of HIV/AIDS globally, key obstacles that have been preventing those who need care from getting it, and how to overcome those obstacles and meet the treatment and prevention needs of those living with or potentially exposed to HIV on an individual, community, state, and global level. Featured speakers will share their experiences and give insight into the session theme.
Speakers:
Raymond Ayala, Medical Case Manager, Path, The Brooklyn Hospital Center.
Nkwenti Guedem Edwige, Nurse Practitioner and HIV Specialist.
Emma Kaplan-Lewis, Clinical Quality Director HIV Services at NYC Health and Hospitals.
Toyin Falusi Nwafor, MD, Senior Medical Director, HIV Prevention at ViiV Healthcare.
Antonio Urbina, MD, Mount Sinai; Associate Professor of Medicine, Icahn School of Medicine.

#HIV/AIDS#state of HIV/AIDS#Brooklyn Hospital Center#NYC Health and Hospitals.#ViiV Healthcare#Icahn School of Medicine#hiv prevention#panel discussion#world aids day#medical treatment#civil society organizations
0 notes
Text
Long Covid blood test shows differences in the immune system, research finds
The research is among the first to prove that "long Covid is, in fact, a biological illness," said David Putrino, principal investigator of the new study and a professor of rehabilitation and human performance at the Icahn School of Medicine at Mount Sinai in New York.
This will need to be investigated with more research, but at least it's something because, quite frankly, right now we don't have any blood tests" either to diagnose long Covid or help doctors understand why it's occurring, he said.
163 notes
·
View notes
Text

Illustration by Monica Garwood
* * * *
From The New York Times Well newsletter
By Carolyn Todd
Feb. 9, 2024
Of the thousands of self-help books on the market, which ones are truly helpful? “It’s uncommon to find a self-help book that feels different,” said Vienna Pharaon, a marriage and family therapist in New York City.
But genuinely useful titles abound. The best of the genre invite reflection or offer practical tools to promote emotional, psychological or spiritual well-being. And there are some that therapists personally turn to or suggest to their patients.
“Almost every therapist I know has a whole list of self-help books to recommend,” said Daniel Tomasulo, a counseling psychologist and the academic director of the Spirituality Mind Body Institute at Teachers College, Columbia University.
When sorting through the self-help stacks, who better to help than mental health professionals? We asked seven to share their picks.
1. "The Book of Joy: Lasting Happiness in a Changing World," by the Dalai Lama, Desmond Tutu with Douglas Abrams
How do we experience joy in the face of personal and collective suffering? The Dalai Lama and Desmond Tutu spent five days reflecting on their own lives to answer that question, and they compiled their stories and guidance in this 2016 book.
“The Book of Joy” is an opportunity to learn from two spiritual leaders in an intimate, accessible way, said Sona Dimidjian, director of the Renée Crown Wellness Institute at the University of Colorado Boulder.
Through their dialogue, which is punctuated with laughter and tears, the Dalai Lama and Archbishop Tutu teach readers how to cultivate joy and work through difficulties like illness and despair. Dr. Dimidjian recommends the book to “anyone who is feeling overwhelmed by the realities of our world and daily life today,” she said.
2. "The Happiness Trap: How to Stop Struggling and Start Living," by Russ Harris
This book, first published in 2007, teaches you to accept your negative thoughts and feelings as they arise, instead of resisting or being consumed by them — a refreshing approach known as acceptance and commitment therapy.
Diana Garcia, a South Florida-based therapist, says this easy-to-read primer made her “first fall in love” with ACT. She has clients use the book as a supplement to their sessions and recommends it to friends who are feeling stuck. It teaches you how to keep taking actions that move you in a positive direction regardless of how you’re feeling, she explained.
3. "Tattoos on the Heart: The Power of Boundless Compassion," by Gregory Boyle
Gregory Boyle is a Jesuit priest who founded Homeboy Industries, a rehabilitation and re-entry program for former gang members. His 2011 book is a collection of real, raw stories about people he worked with and the lessons we can all draw from their experiences.
“Each chapter reads like a Sunday sermon to be savored and meditated upon,” said Jacob Ham, director of the Center for Child Trauma and Resilience at the Icahn School of Medicine at Mount Sinai. While faith is woven throughout the book, Dr. Ham recommends the title to anyone who feels “that their traumas and all the ways they’ve coped with them have left them broken and unredeemable.”
4. "The Artist’s Way: A Spiritual Path to Higher Creativity," by Julia Cameron
This 1992 workbook from Julia Cameron, a teacher and author, is a 12-week guide to recovering your sense of childlike creativity. And it’s not just for artists and writers, said Britt Frank, a trauma specialist in Kansas.
“Of all of the books I have ever used with clients, this one has the most staying power,” she said. “Because everyone is creative, and creativity is medicine.”
For years, Ms. Frank has returned to the book’s tools — like the “morning pages,” a stream-of-consciousness journaling practice. And she uses “The Artist’s Way” when treating clients with issues like depression and addiction. But skimmers beware, Ms. Frank cautioned: “It’s not a book you read. It’s a book you work.”
5. "Homecoming: Healing Trauma to Reclaim Your Authentic Self, by Thema Bryant
Thema Bryant is a trauma therapist, ordained minister and professor who offers a “distinctive lens on health, hope and healing trauma,” said Ayanna Abrams, a psychologist in Atlanta.
Drawing on her clinical work, spirituality and personal recovery from trauma, Dr. Bryant shares stories, reflections and exercises in this 2022 title. She helps people believe in their capacity to heal, Dr. Abrams explained. Dr. Bryant also avoids the “gimmicky, bypassing or vague” language that so many self-help books lean on, she added.
6. "The Power of Character Strengths: Appreciate and Ignite Your Positive Personality," by Ryan M. Niemiec and Robert E. McGrath
This 2019 guide helps people recognize, honor and nurture their brightest qualities, Dr. Tomasulo said. The idea of cultivating your “character strengths” comes from positive psychology, which centers on promoting well-being, he explained. “It’s about moving from focusing on ‘what’s wrong’ to ‘what’s strong.’”
People who lean into their character strengths tend to be happier, Dr. Tomasulo said. This book, he explained, is a good pick for “people who are doing OK, but want to have more joy and well-being in their life.”
[Follies of God]
8 notes
·
View notes
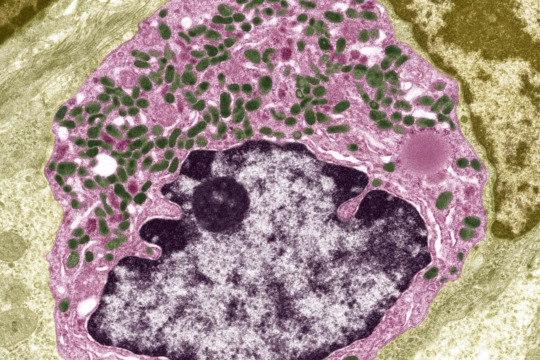
Photo

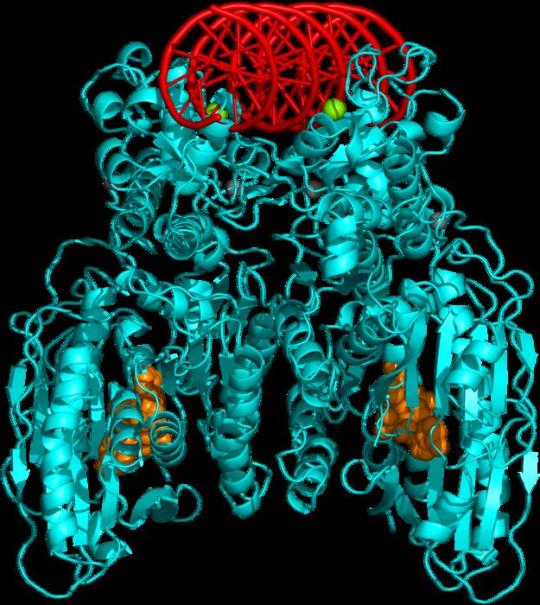
Macrophage Defector
Natural killer cells are a type of immune cell that protects the body against not only invading pathogens but also cancer, providing an innate defence against these rogue cells. Some tumours, however, keep natural kill cells at bay and thereby avoid destruction. And recent research in lung tumours reveals this natural killer cell exclusion is achieved with the help of another immune cell – the macrophage. The particular culprit is a type of macrophage covered in a protein called TREM2 – an anti-inflammatory factor. Shown above is a lung tumour (green) packed with TREM2-expressing macrophages (red) that are protecting the cancer from attack. Why these macrophages switch allegiance and side with enemy is unclear, but blocking TREM2 while boosting natural killer cell activity was shown to reduce lung tumour growth in mice suggesting a similar approach might be effective in promoting tumour regression in humans too.
Written by Ruth Williams
Image from work by Matthew D. Park and Ivan Reyes-Torres, and colleagues
Marc and Jennifer Lipschultz Precision Immunology Institute, Icahn School of Medicine at Mount Sinai, New York, NY, USA
Image copyright held by the original authors
Research published in Nature Immunology, April 2023
You can also follow BPoD on Instagram, Twitter and Facebook
41 notes
·
View notes
Text
Scientists Offer a New Explanation for Long Covid (NYT)
"A team of scientists is proposing a new explanation for some cases of long Covid, based on their findings that serotonin levels were lower in people with the complex condition."
By Pam Belluck
Oct. 16, 2023
The News
A team of scientists is proposing a new explanation for some cases of long Covid, based on their findings that serotonin levels were lower in people with the complex condition.
In their study, published on Monday in the journal Cell, researchers at the University of Pennsylvania suggest that serotonin reduction is triggered by remnants of the virus lingering in the gut. Depleted serotonin could especially explain memory problems and some neurological and cognitive symptoms of long Covid, they say.
Why It Matters: New ways to diagnose and treat long Covid.
This is one of several new studies documenting distinct biological changes in the bodies of people with long Covid — offering important discoveries for a condition that takes many forms and often does not register on standard diagnostic tools like X-rays.
The research could point the way toward possible treatments, including medications that boost serotonin. And the authors said the biological pathway that their research outlines could unite many of the major theories of what causes long Covid: lingering remnants of the virus, inflammation, increased blood clotting and dysfunction of the autonomic nervous system.
“All these different hypotheses might be connected through the serotonin pathway,” said Christoph Thaiss, a lead author of the study and an assistant professor of microbiology at the Perelman School of Medicine at the University of Pennsylvania.
“Second of all, even if not everybody experiences difficulties in the serotonin pathway, at least a subset might respond to therapies that activate this pathway,” he said.
“This is an excellent study that identifies lower levels of circulating serotonin as a mechanism for long Covid,” said Akiko Iwasaki, an immunologist at Yale University. Her team and colleagues at the Icahn School of Medicine at Mount Sinai recently published a study that identified other biological changes linked to some cases of long Covid, including levels of the hormone cortisol. These studies could point to specific subtypes of long Covid or different biological indicators at different points in the condition.
The Back Story: A series of disruptions set off by bits of virus in the gut.
Researchers analyzed the blood of 58 patients who had been experiencing long Covid for between three months and 22 months since their infection. Those results were compared to blood analysis of 30 people with no post-Covid symptoms and 60 patients who were in the early, acute stage of coronavirus infection.
Maayan Levy, a lead author and assistant professor of microbiology at the Perelman School of Medicine, said levels of serotonin and other metabolites were altered right after a coronavirus infection, something that also happens immediately after other viral infections.
But in people with long Covid, serotonin was the only significant molecule that did not recover to pre-infection levels, she said.
The team analyzed stool samples from some of the long Covid patients and found that they contained remaining viral particles. Putting the findings in patients together with research on mice and miniature models of the human gut, where most serotonin is produced, the team identified a pathway that could underlie some cases of long Covid.
Here’s the idea: Viral remnants prompt the immune system to produce infection-fighting proteins called interferons. Interferons cause inflammation that reduces the body’s ability to absorb tryptophan, an amino acid that helps produce serotonin in the gut. Blood clots that can form after a coronavirus infection may impair the body’s ability to circulate serotonin.
Depleted serotonin disrupts the vagus nerve system, which transmits signals between the body and the brain, the researchers said. Serotonin plays a role in short-term memory, and the researchers proposed that depleted serotonin could lead to memory problems and other cognitive issues that many people with long Covid experience.
“They showed that one-two-three punch to the serotonin pathway then leads to vagal nerve dysfunction and memory impairment,” Dr. Iwasaki said.
There are caveats. The study was not large, so the findings need to be confirmed with other research. Participants in some other long Covid studies, in which some patients had milder symptoms, did not always show depleted serotonin, a result that Dr. Levy said might indicate that depletion happened only in people whose long Covid involves multiple serious symptoms.
What’s Next: A clinical trial of Prozac.
Scientists want to find biomarkers for long Covid — biological changes that can be measured to help diagnose the condition. Dr. Thaiss said the new study suggested three: the presence of viral remnants in stool, low serotonin and high levels of interferons.
Most experts believe that there will not be a single biomarker for the condition, but that several indicators will emerge and might vary, based on the type of symptoms and other factors.
There is tremendous need for effective ways to treat long Covid, and clinical trials of several treatments are underway. Dr. Levy and Dr. Thaiss said they would be starting a clinical trial to test fluoxetine, a selective serotonin reuptake inhibitor often marketed as Prozac, and possibly also tryptophan.
“If we supplement serotonin or prevent the degradation of serotonin, maybe we can restore some of the vagal signals and improve memory and cognition and so on,” Dr. Levy said.
4 notes
·
View notes
Text
Book of the Day - The Self-Talk Workout
Today’s Book of the Day is The Self-Talk Workout, written by Rachel Goldsmith Turow in 2022 and published by Shambhala.
Dr. Rachel Goldsmith Turow is a psychotherapist, a researcher, an adjunct faculty member at Seattle University and the Icahn School of Medicine at Mount Sinai, and a mindfulness teacher. She is a renowned expert in teaching how to use mindfulness, self-compassion, and cognitive…

View On WordPress
#Book#Book Of The Day#book recommendation#bookstagram#booktok#Rachel Goldsmith Turow#Raffaello Palandri#Shambhala#Shambhala Publications#The Self-Talk Workout
12 notes
·
View notes
Text
Columbia University Irving Medical Center: A Systemic Response to Systemic Racism
Columbia University Irving Medical Center: A Systemic Response to Systemic Racism.
The death of George Floyd at the hands of police—combined with the disparities highlighted by the COVID-19 pandemic—spurred a racial awakening across the United States in 2020. The flurry of activity that started then at VP&S has not abated. VP&S students, faculty, and staff have initiated more than a dozen efforts to chip away at the massive undertaking of dismantling the effects of systemic racism in medical education.
Maya Jalbout Hastie, MD, associate professor of anesthesiology, and her fellow faculty in anesthesiology developed virtual improvisation sessions—inspired by true events—to help department members handle racist microaggressions in the workplace. Devon Rupley, MD, assistant professor of obstetrics & gynecology, along with two medical students, Stephanie Granada'21 and Cibel Quinteros-Baumgart'22, conducted one of the first studies to understand the birthing experiences of Spanish speakers during the early days of the pandemic in New York City. And medical student Jeremiah Douchee joined the Columbia chapter of White Coats for Black Lives, an organization run by medical trainees that aims to end racism and systems of oppression in health care.
Despite these efforts by members of the VP&S community, racism remains a systemic problem and demands a systemic solution. So in October 2021—as VP&S welcomed its most diverse medical student class in history—Hastie, Rupley, Douchee, and a dozen other stakeholders joined forces to form the executive coalition of the school's Anti-Racist Transformation (ART) in Medical Education project, perhaps the most comprehensive effort yet to undo systems of racism and bias in education at VP&S.
"Gathering a group of individuals across the workplace spectrum has been instructive on what it means to be inclusive," says Monica L. Lypson, MD, vice dean for education. "Having students, staff, and faculty working in collaborative fashion to create an anti-racist educational environment is key to future success."
Creating an anti-racist strategy
ART in Medical Education is a framework developed by the Icahn School of Medicine at Mount Sinai that brings a three-year, systemic approach to the effort, charging medical schools with creating a transformative, ongoing anti-racist strategy. (As opposed to being passively "not racist," the term "anti-racist" refers to taking an active approach in countering systems of racial prejudice.) By participating in the project's inaugural cohort of 11 schools in the United States and Canada, VP&S is building on the efforts of its anti-racism task force, which called for advances in curriculum, admissions, student support, and the learning environment.
The ART in Medical Education executive coalition at VP&S is led by Jean-Marie Alves-Bradford, MD, associate professor of psychiatry and inaugural director of the Department of Psychiatry's Office of Equity, Diversity, and Inclusion, and Hetty Cunningham, MD, associate professor of pediatrics and director of equity and justice in curricular affairs at VP&S. The ART project continues the work they did together to develop workshops for medical students processing racial trauma.
"It does really help to be a part of this team effort," says Alves-Bradford. "We're all coming from different disciplines, but with some similar experiences in those disciplines. Working together toward change, regardless of our area of expertise or particular focus, is not just bonding, it's motivating and strengthening and reinforcing that commitment."
When the project officially launched in October 2021, Cunningham says, the VP&S executive coalition began mapping out the disparate anti-racism efforts already taking place at Columbia to build a roadmap for organizational change. "What are the priorities of the institution that are documented, that have been expressed, that have been accepted? How can we work with those? Who are the main allies in this work? Who needs to be included? The idea is to come together and create a cohesive movement."
Guided by those findings, the coalition narrowed its focus to three core areas: curriculum, faculty retention, and integrated care.
Addressing the learning environment
To address curriculum, the executive coalition developed anti-racist learning objectives using a framework drafted by the Association of American Medical Colleges. The objectives aim to help students and faculty understand the term "anti-racist," says Alves-Bradford, and to define and operationalize what it means to create an anti-racist learning environment and health care system. Some of the objectives focus broadly on systems and practices, she says, while others drill down into specifics, such as how the medical school approaches basic sciences.
"We think about how the objectives would evolve over time throughout the curriculum," says Alves-Bradford, "to get deeper and more complex as students go from preclinical to clinical."
The learning objectives include understanding how a physician's personal biases and lived experience can influence clinical decision-making—and their interactions with patients, patients' families, and other members of the care team—and learning how to mitigate the effects of those biases. Another key element involves studying how societal structures might have played a role in a patient's health care experience. For instance, a person might have an increased risk of diabetes and heart disease if they live in a neighborhood that lacks access to affordable, healthy food. "Bias can creep in in lots of different ways," Alves-Bradford says, "even when we think it's far removed from the actual individual patient."
It's important to include anti-racist learning objectives as part of the curriculum, Cunningham says, because it means those skills will be formally assessed. "If something isn't assessed, then it's not taken seriously," Cunningham says. "We want our students to be able to be active in the space of anti-racism. Not only will they have the knowledge, but they'll know how to advocate for changes in medicine. The faculty are in agreement that that's something we want our students to be able to do, so we have to shift the curriculum."
Work toward an anti-racist medical education system also has implications for recruitment and retention, Alves-Bradford says. As workers nationwide reconsider their professional aspirations and work-life balance in wake of the pandemic, she notes, now is the time to consider systemwide structures that would help VP&S recruit and promote the best faculty, staff, and students.
Segregated care
Finally, while the idea of segregated health care might seem like a relic of the past, Alves-Bradford says a patient's health insurance coverage often dictates whether that person is treated at a faculty practice or a public clinic. Different providers work in these separate settings, and the differences don't end there. Faculty practices and public clinics have disparate resources, she notes, from technology to staffing ratios and even the ambiance of the setting in which patients receive care.
The Center for Clinical Medical Ethics at VP&S hosted a symposium in May on segregated health care. The center's director, Lydia S. Dugdale, MD, the Dorothy L. and Daniel H. Silberberg Associate Professor of Medicine at VP&S, gave the opening remarks. After public health experts outlined the history and policy that shapes how people receive care, a panel of physicians discussed ongoing efforts to desegregate care. Panelists included Julia E. Iyasere, MD, assistant professor of medicine and executive director of the Dalio Center for Health Justice at NewYork-Presbyterian. Kamini Doobay, MD, assistant professor of emergency medicine, closed the event by providing the attendees with ways to advocate for individual patients and for systemic changes.
The ART in Medical Education coalition at VP&S plans to use its platform to publicize the issue and educate the Columbia community about segregated care. "What are some of the pitfalls when things are structured in that way?" Alves-Bradford asks. "What is the context? How did those systems evolve to be that way? There were regulations that led it to be one way or another: How does that happen?"
The coalition has joined ongoing efforts, including White Coats for Black Lives and the NYC Coalition to Dismantle Racism in the Health System, to push for an end to this divided system. "We're advocating for not having those systems segregated," says Alves-Bradford, "to integrate and have people seen in similar settings, regardless of their insurance or payment."
Beyond their work on curriculum, faculty retention, and integrated care, the VP&S coalition is considering ways to support and recognize students involved in anti-racism work. Also on the horizon: involving more participants from the greater VP&S community and the city at large.
As the ART in Medical Education project enters its second year, the VP&S coalition and the rest of the inaugural cohort of schools are moving into the next phase of the project: implementing and sustaining change at their various institutions. While each of the 11 medical schools aims to embed change, learn from feedback, and course correct to develop transformative, ongoing anti-racism strategy, the cohort also plans to come together to learn from each other.
"The cohort allows us to partner with institutions around the country that are doing very exciting things," Cunningham says, "We're sharing our challenges and solutions. That allows us all to move forward more quickly and adopt best practices."
#A Systemic Response to Systemic Racism#systemic racism#disparities in society#racism#change#anti racism work
3 notes
·
View notes
Text
Taking out tumor-associated macrophages allows the immune system to target tumors
According to findings published earlier this month in Cancer Immunology Research, researchers from the Icahn School of Medicine at Mount Sinai report a new means of counteracting therapeutic resistance in cancer cells: Take out their goons. Chimeric antigen receptor (CAR) T cells can be made to target the tumor-associated macrophages that protect cancer cells from the rest of the immune system.
CAR T cells have been used to treat cancer before, but always by targeting the cancer cells themselves. Here, researchers found that targeting TAMs instead could produce an even more pronounced effect. TAMs usually infiltrate the tumor and physically block the channels that immune cells would otherwise use to enter and attack it. By taking out the TAMs, the CAR T cells allows the rest of the immune system to bring its weight to bear.
“Our initial goal was just to use the CAR T cells to kill the immunosuppressive macrophages, but we discovered they were also boosting tumor immunity by releasing this powerful immune-boosting molecule,” said study co-author Brian Brown. Dr. Brown is Director of the Icahn Genomics Institute.
Another co-author, Dr. Miriam Merad, pointed out that this new technique addresses a perennial problem in cancer treatment: “Our molecular studies of human tumors have revealed macrophage subsets present in human tumors and not in normal tissues and are similar across tumors and across patients. So macrophage-targeting CAR T cells could be a broad way to target different types of solid tumors and improve immunotherapy.”
The research team tested this process in an in vitro model of lung cancer and in vivo mouse models of lung, pancreatic, and ovarian tumors. In all cases, the CAR T cells infiltrated the lesions, blockaded PD-1, and destroyed TAMs without any toxic side effects.
Sánchez-Paulete A, Mateus-Tique J, Mollaoglu G, Nielsen S, Marks A, Lakshmi A, et al.; Targeting Macrophages with CAR T Cells Delays Solid Tumor Progression and Enhances Antitumor Immunity. Cancer Immunol Res 2022; doi: 10.1158/2326-6066.CIR-21-1075
Life Science Editing
2 notes
·
View notes
Text
El cuco de cristal
Ficha Técnica
Nº de páginas: 488
Editorial: Suma
Idioma: Castellano
Encuadernación: Tapa blanda / eBook / De bolsillo
ISBN: 9788491293552 / 9788491296089 / 9788466374637
Año de edición: 2023
Plaza de edición: ES
Fecha de lanzamiento: 01/02/2023
Alto: 23.4 cm
Ancho: 15.5 cm
Grueso: 3.5 cm
Peso: 632 gr
Colección: Suma
Sinopsis
Un trasplante de urgencia. Un donante lleno de secretos. ¿Que esconden los latidos de tu corazón?
Nueva York, 2017. Cora Merlo, medico residente de primer año, sufre un infarto fulminante que la obliga a un trasplante de corazón. Aún convaleciente la joven recibe la visita de una extraña mujer con una enigmática oferta: pasar unos días en Steelville, un pequeño pueblo de interior, para conocer la vida de su hijo Charles, el donante de su corazón.
Cora se adentra así en un hogar lleno de secretos, en un misterio que se extiende durante veinte años y en un pueblo hermético en el que, justo el día de su llegada, desaparece un bebe en un parque público.
Fragmento
"Me desperté sintiendo el corazón en llamas, como si un incendio estuviese arrasando el interior de mi pecho. Tenía frío, me temblaban las manos, me faltaba el aire. Pero todo era peor por dentro. El fuego devastador que ardía bajo mi esternón parecía agotar el oxígeno que inhalaba y yo sentía cómo me devoraba sin control. Mi madre estaba postrada a los pies de la cama, con la mirada perdida en el suelo y unas ojeras que insinuaban una larga vigilia. Lloraba. Escuché sus sollozos entremezclados con el pitido de un monitor cardiaco que invadía la habitación y que marcaba, sin yo ser consciente aún, el inicio de mi caída.
Una alarma comenzó a sonar y mi madre me miró asustada. Me fijé en la pantalla y, al ver que marcaba treinta y seis pulsaciones por minuto, sentí cómo toda la esperanza se desvanecía. Me había despertado para morir. Miré con pánico a mi madre y conseguí exhalar un «te quiero» antes de que fuese demasiado tarde. No se merecía esta despedida.
—¡Cora! ¡Cora! —chilló aterrorizada—. ¡Ayuda! ¡Que venga un médico!
Yo no tenía fuerzas para decir nada más. Cerré los ojos y..., de repente, me caí al vacío engullida por las llamas en mi corazón.
Todo había comenzado un mes antes, justo el primer día de mi residencia médica en el hospital. Había sido admitida con beca a uno de los programas más importantes del país y llegaba tarde a la reunión de presentación del decano, el doctor Mathews, en la que se suponía que me asignarían el primer grupo de trabajo. Yo aspiraba a la especialización en oncología de radiación, un destino que me recordaba el brillo de las lágrimas de mi madre. Así que subí corriendo las escaleras. Al llegar a la tercera planta sentí como si estuviese participando en la maratón de Nueva York, batiendo las tres horas cuarenta de mi mejor marca personal el año anterior. Notaba el corazón desbocado y tosí como ya casi me había acostumbrado desde hacía unas semanas.
—¡Cora! —chilló una voz que reconocí al instante. Era Olivia, mi compañera de la facultad de Medicina y con quien lloré de felicidad el día en que nos admitieron—. ¡Estamos aquí! ¡Lo hemos conseguido! ¿Cómo me queda? —Posó delante de mí sonriente y luciendo la misma bata blanca que yo en la que se podía leer el nombre de la Icahn School of Medicine del Monte Sinaí bordado en el pecho, junto a dos montañas de color azul y magenta—. ¿No es increíble? ¡Las dos juntas en la residencia!"


Read the full article
0 notes
Text
Postdoctoral Fellow in Neuroscience at Mount Sinai NYC - Xiaoting Wu Lab
Icahn School of Medicine at Mount Sinai
We're seeking a #neuroscience postdoc to join us @XiaotingWuLab at Mount Sinai NYC
See the full job description on jobRxiv: https://jobrxiv.org/job/icahn-school-of-medicine-at-mount-sinai-27778-postdoctoral-fellow-in-neuroscience-at-mount-sinai-nyc-xiaoting-wu-lab/?feed_id=74014
#autism #neural_circuits #neuromodulation #neuroscience #optogenetics #ScienceJobs #hiring #research
0 notes
Text

Another Vulnerable Population
Study of different cell types in Parkinson's disease-affected brains reveals, in addition to dopaminergic neurons, another type called RIT2 neurons that are vulnerable to Parkinson's-associated molecular changes
Read the published research article here
Image from work by Qian Wang, Minghui Wang and Insup Choi, and colleagues
Icahn School of Medicine at Mount Sinai, New York, NY, USA
Image originally published with a Creative Commons Attribution 4.0 International (CC BY-NC 4.0)
Published in Science Advances, January 2024
You can also follow BPoD on Instagram, Twitter and Facebook
#science#biomedicine#immunofluorescence#neuroscience#parkinsons#parkinson's disease#neurons#dopamine#brain
5 notes
·
View notes
Text
Too Dumb for Harvard? Lemon's Too Dumb for Twitter

Interviewing Elon Musk this week, former CNN host Don Lemon demonstrated the real-life consequences of affirmative action.
Interestingly enough, Lemon himself is an affirmative action beneficiary who miraculously hung on at CNN despite committing one moronic gaffe after another (maybe he's just got television magic!). The only CNN on-air personality to handle himself worse was Jeffrey Toobin.
Lemon was baffled by Musk's claim that "if we lower standards for what it takes to become a board-certified surgeon ... then more people will die than if we don't lower the standards, therefore we should not lower the standards."
This was apparently Lemon's first encounter with the logical sequence known as a "syllogism."
Lemon's response: "Do you understand how by saying just that standards are being lowered that you're implying that they're being lowered because people are less skilled and less intelligent, and you're talking about people of color?"
What on Earth do liberals think "affirmative action" is? (And when I say "liberals think," of course, I'm speaking figuratively.)
Does Lemon understand that when universities fight like wildcats to hide their black students' SAT scores, they are also kind of implying blacks are less skilled and less intelligent?
Last year, during the part of a multimillion-dollar lawsuit known as "discovery," Harvard University finally coughed up the data. If -- you'll pardon the expression -- "newsman" Lemon had followed the news, he would know precisely how much standards had been lowered for black students.
Applicants in the top "academic decile" (GPA plus standardized test scores) were accepted in the following percentages: Asians: 13%; Whites: 15%; Blacks: 56%. Perhaps more jaw-dropping, in the fifth academic decile -- not quite Harvard material -- the percentages were: Asians: 2% (musicians); Whites: 3% (football players and Jared Kushner); Blacks: 22%.
Recommended
People who've been paying attention were shocked. Good lord, who are the 44% of blacks in the top academic decile who DON'T get into Harvard? What kind of horrendous character defect do they have? Do they all submit "Cill My Landlord" as their personal essay? How can it not be 100%?
Nonetheless, Lemon asked Musk, "Why do you think they're lowering the standards for minority doctors?" To his credit, at no point did Lemon cry out, "I thought we agreed there'd be no math during this interview!"
The Manhattan Institute's Heather Mac Donald has been documenting the total abandonment of standards at medical schools for years. Before choosing your heart surgeon, you might want to review the statistics she's laid out most recently in her book, "When Race Trumps Merit."
In 2021, the average white score on the MCAT was at the 71st percentile. The average black score was at the 31st percentile.
Whereupon medical schools began dropping the MCAT altogether. Henceforth, some students (guess who?) would be offered admission on the basis of their "strong appreciation of human rights and social justice," as The Icahn School of Medicine at Mount Sinai puts it. In other words, would-be physicians can now skip those chapters on chemistry and physiology as long as they watch the Source Awards.
The lowered standards persist throughout medical training. Step 1 of the United States Medical Licensing Exam (USMLE), given after the second year of medical school, allows students to begin practicing medicine and "matches" them to a residency. But it seems that the average score for black students is a full standard deviation below the score for whites and Asians.
Although the test is multiple-choice and graded by computer, in January 2022, the USMLE dropped grades for Step 1 and converted it to "pass/fail."
So now, instead of medical students being matched to specialties that play to their strengths, they are randomly assigned to residencies for which they may have little aptitude or interest. You know, the same way they assign on-air talent at CNN. It's a brilliant way for training the next generation of doctors.
Also, starting next year, open-heart surgery will be graded "pass/fail."
Responding to Musk's claim that the "probability that someone will die I think at some point is high," Lemon said, "but that's a hypothetical that doesn't mean it's happening."
In fact, it already has happened, countless times, all over the country -- but notoriously, to the most famous affirmative action doctor of all: the black applicant who took Allan Bakke's place at the medical school of the University of California at Davis. Here was an incompetent black doctor whose medical errors couldn't be brushed under the rug, though affirmative action proponents did their best.
Dr. Patrick Chavis openly admitted that he never would have gotten into medical school without UC Davis' affirmative action program. Sen. Teddy Kennedy, The New York Times and the Nation magazine all touted Chavis as an affirmative action success story! Unlike Bakke, who went to work at the Mayo Clinic, Chavis was serving a disadvantaged community and "making a difference in the lives of scores of poor families," as Sen. Kennedy said.
Yes, he was making a difference in his patients' lives, mostly by shortening them. Dr. Chavis' liposuction surgery left one patient bleeding, vomiting and urinating uncontrollably. But instead of taking her to a hospital, he let her bleed in his home for another 40 hours. By the time she managed to escape and check herself into a hospital, she'd lost 70% of her blood. (To be fair, she looked amazing when bikini season rolled around!)
Miraculously, she lived, as did most of his other liposuction patients who ended up in the emergency room. One, Tammaria Cotton, did not.
But the affirmative action cover-up can never end: It took the California medical board a year to suspend Dr. Chavis' license, with patient advocates screaming bloody murder at such a pathetically slow response.
You think Bakke could have killed a patient to so little fanfare?
The New York Times took no notice of the affirmative action doctor's grisly liposuctions, except a brief notation in his obituary years later, after he was gunned down in an attempted carjacking. In paragraph 7, the Times extravagantly described Chavis' medical malpractice thus: "He was accused of mistreating eight liposuction patients, one of whom died."
Or, as Lemon repeated on autoplay: "There's no actual evidence of what you're saying."
Then there was Martin Luther King Jr. Hospital in South Central Los Angeles -- or "Killer King," as the locals dubbed it. A "symbol of justice and political power to many black people," as the Los Angeles Times put it in a Pulitzer Prize-winning story, "the majority of its staff has always been black."
"Entire departments," the Times investigation found, "are riddled with incompetence, internal strife and, in some cases, criminality. Employees have pilfered and sometimes sold the hospital's drugs; chronic absenteeism is rampant; assaults between hospital workers are not uncommon."
Despite having "abnormally high salaries for ranking doctors," Killer King paid out "more per patient for medical malpractice" than any of the state's 23 other public hospitals or medical centers.
So there's loads of "evidence" that affirmative action kills, despite the best efforts of our universities, medical system and media to hide it. Of course, if you mention the evidence, you'll be called a "white supremacist."
See? No evidence.
0 notes
Text

Humpback Whales are known for their magical songs, which likely serve to communicate with others and attract potential mates. Photograph By Karim Iliya
Whales Can Sing Underwater Without Drowning—Now We Know How
Scientists Have Discovered New Insights into Baleen Whales’ Anatomy That May Also Make Them Vulnerable to Human Noise Pollution.
— By Melissa Hobson | February 21, 2024
Scientists have long wondered how baleen whales can sing while holding their breath. That’s because a whale’s larynx both makes sound and closes off their airway so they don’t drown. Try closing your mouth, holding your nose, and trying to hum—it won’t work.
“If you can't let the air flow, the system is pressurized. When it's pressurized, and flow stops, sound stops,” says Joy Reidenberg, a professor at Icahn School of Medicine at Mount Sinai in New York City who studies whale anatomy.

An Illustration of a Humpback Whale Shows Its Pink, U-shaped Larynx. Painting By Patricia Jaqueline Matic
Experts already knew that whales have a special larynx with a bagpipe-like sac that enables them to sing, but they didn’t know exactly how they produced sound.
“You can't just take an endoscope down a baleen whale and see what they're doing when they're singing,” says Reidenberg who was not involved with the new study. But three strandings close to his lab enabled lead author Coen Elemans, professor of bioacoustics at the University of Southern Denmark, to collect fresh vocal tracts from a recently deceased humpback, minke, and sei whale.
For the first time, Elemans could use these three larynxes to replicate what happens when the animals produce sound. That led to a surprising discovery: The animals’ vocal cords vibrate in an unexpected way to produce noise.
Party Balloons—For Science
Each of the three species create very different noises: humpbacks sing complex songs, minkes quack like ducks, and sei whales create low frequency booms. But how?
After conducting CT scans, the team situated the three larynxes in a laboratory air space and slowly blew air through the system to see if they could mimic a whale’s gigantic lungs.
“We ended up using party balloons to power the setup,” Elemans says.
They’d assumed that the inner edges of the whales’ vocal cords rub together to make sound, but the experiment revealed the vocal cords instead rub together against a fat pad at the back of the larynx.
“No other animal does vocalizations in that way,” says Reidenberg.
Reidenberg wonders if the two vocal cords can vibrate at different frequencies against the fat cushion, or whether they can also vibrate against each other. This could explain how a whale can make more than one sound at once.
Elemans thinks these adaptations arose when whales' land ancestors returned to the ocean around 50 million years ago. Because baleen whales needed to communicate with other whales while using their larynx for food and airway separation, they evolved this unique system.
“These animals physiologically made up a totally new evolutionary novelty to make sound underwater with this weird larynx,” he says.

A Mother Humpback Whale swims with her calf off the coast of Rarotonga, the largest of the Cook Islands in the South Pacific. Humpbacks are among the species of whale known to partake in "kelping"—or playing with seaweed they find floating in the ocean. Photograph By Brian Skerry National Geographic Image Collection
More Investigation Needed
Reidenberg cautions the sample size of the study—just three animals—is too small for such a generalization, and that scientists need to examine more specimens first.
Heidi Pearson, professor of marine biology at University of Alaska Southeast, who was also not involved in the study, agrees. She’d like to see a different family of whales examined for comparison, as the three individuals studied were all juvenile rorqual whales. Elemans says he wants to study an adult male, which are known for their singing.
But the experts acknowledge the inherent challenge in doing so. “Just getting those samples is a triumph in its own right,” says Pearson.
Controlling Noise Pollution
The researchers also used 3-D computer simulations to mimic what happens when the whales’ larynx muscles are activated. They discovered these structures cannot produce sound at higher frequencies than 300 hertz (Hz), or below depths of about 330 feet.
Unfortunately, that “depth and frequency range overlap almost perfectly with what humans make,” says Elemans, meaning they may struggle to compete with noise generated by shipping vessels, which emit sounds between 30 and 300 Hz.
“It's what you and I might call a cocktail party effect,” says Reidenberg. When your vocal range overlaps with everyone else’s, it becomes harder to hear each other without raising your voice.
That’s why the study highlights an urgent need to decrease noise pollution by limiting vessel traffic, implementing slow zones, protecting areas with lots of vocalizing whales, and making ships quieter, says Pearson, and using real-time data in conservation plans.
Reidenberg has a good example of how to do that: If an offshore wind farm in New York conducted a seismic survey during winter, it wouldn’t interfere with whale vocalizations, she says, because “the singers are all down having spring break in the tropics.”
#Whales 🐋#Humpback Whales 🐋#Singing 🎵 🎶#Underwater#Baleen Whales’ Anatomy#Vulnerable#Human Noise Pollution#Melissa Hobson
0 notes
Text
New approach to tackling bacterial infections identified.
Researchers at the Icahn School of Medicine at Mount Sinai have identified a new approach to controlling bacterial infections. The findings were described in the February 6 online issue of Nature Structural & Molecular Biology [DOI # 10.1038/s41594-024-01220-x].
The team found a way to turn on a vital bacterial defense mechanism to fight and manage bacterial infections. The defense system,…
View On WordPress
0 notes
Text
7 Signs of Lung Cancer You Might Be Ignoring – Koperacija
“Coughing up blood is never a good sign. Right then and there, go see your doctor,” says Raja Flores, MD, professor and chairman of thoracic surgery at Icahn School of Medicine at Mount Sinai in New York City. Although cancer may not necessarily be the cause of your bloody coughs, you should definitely get tested, he says.
1 note
·
View note