#abstractposter
Text
This template kicks ass and has Madagascar in it

4 notes
·
View notes
Photo
Check out our Art Store, with new artworks added almost everyday. High quality prints in archival ink - #submersibletees #abstractart #posterart #posters #abstractposters #colourful #linework #pastels #painting #design #illustration #mural #abstractillustration #illus #instagramdesign #designoninsta #instaposters #posterartwork #drawing #sketching #fresco #adobe #artwork #archivalink #printshop #artstore (at Bandra West) https://www.instagram.com/p/Cjk8H1PKJB-/?igshid=NGJjMDIxMWI=
#submersibletees#abstractart#posterart#posters#abstractposters#colourful#linework#pastels#painting#design#illustration#mural#abstractillustration#illus#instagramdesign#designoninsta#instaposters#posterartwork#drawing#sketching#fresco#adobe#artwork#archivalink#printshop#artstore
0 notes
Text
Lupine Publishers | Post-COVID-19 GI Manifestations: Are We in for the “Long Haul”?
Abstract
Post-COVID-19 gastrointestinal (GI) disease management remains a clinical challenge as the medical literature continues to evolve and expand. Reports of excess GI disease burden across the population, as well as prescribed use of pharmaceuticals for symptom relief, have proven “long-haul” GI disease is prevalent across the population. This article will help to summarize the current medical literature as it pertains to post-COVID-19 GI clinical presentations, dysbiosis, functional disorders and evidence of lasting liver and biliary injury implications. Increased awareness of the GI implications for this paradigm hopefully will lead to a better understanding of the pathophysiology, as well as natural history and potential therapeutic approaches.
Keywords:COVID-19; post-covid manifestations; long covid; gastrointestinal disorders; dysbiosis; dyspepsia; microbiome; probiotics
Introduction
Early medical research into coronavirus disease 2019 (COVID-19) focused predominantly on the acute presentation, management, and treatment of what was initially viewed to be only a respiratory illness. However, progressive case analysis demonstrated that the COVID-19 clinical presentation frequently included gastrointestinal (GI) manifestations, diarrhoea being the most common by affecting up to 33.7% of COVID-19 positive patients [1,2]. Also known as SARS-CoV-2, this variant was found to have a similar prevalence of GI symptoms as SARS-CoV-1 and MERS-CoV [3]. Additionally, this disease was associated with frequent reports of nausea, vomiting, and abdominal pain often preceding the respiratory sequela or in some cases, evident as the only symptom. [1,2,4]. Typically, these GI symptoms last between 1-14 days after acute onset [5]. Longitudinal follow-up of patients has demonstrated a notable subset with a wide-range of persistent COVID-19 symptoms, maintained for extended time after the initial acute presentation. Collectively, this has been defined in the literature as long-haul covid (or long-covid) [6]. Evidence of longcovid has emerged recently in the medical literature. In a multistate telephone survey of 272 patients at 3 weeks after initial diagnosis, 35% of respondents indicated that they had not returned to their usual state of health with greater than 50% of those reporting at least one unresolved symptom [7]. Another study of 177 patients had approximately 30% of their cohort reporting persistent symptoms up to 9 months after diagnosis [8]. In a larger cohort of 1733 patients, looking at 6 month follow-up from diagnosis found that the most common persisting symptoms included fatigue or muscle-weakness, loss of sense of smell or taste, sleep disruption, and anxiety or depression [9]. These symptoms were found to be evident even in patients with relatively mild initial symptoms [8]. The clinical course also varied over time from recurrent and relapsing to constant symptoms. With extended follow-up of these “long haul” COVID-19 infected patients, there is increasing awareness of persistent GI involvement. A study of the national healthcare databases of the US Department of Veterans Affairs analyzing the 6-month data beyond the first 30 days of COVID-19 diagnosis showed significant evidence of excess GI-disease burden per 1000 patients compared to non-COVID patients with an increase in diagnosed esophageal disorders, gastrointestinal disorders, and abdominal pain [10].Furthermore, there was noted to be an increased use of laxatives, antiemetic agents, histamine antagonists, antacids, and antidiarrheal agents [10]. Thus, many of the GI complaints and disorders that healthcare providers have recently encountered or will see in the office through this COVID-19 era may be related to COVID-19 manifesting disease and must be considered in this context. This paper will discuss the current understanding of long-covid related GI-disease.
Underlying mechanisms for “long haul” GI COVID
The GI mucosa consists of mucin producing goblet cells as well as a protective barrier of intestinal epithelial cells to protect from exogenous harm and to prevent infection [11,12]. The breakdown of this natural barrier and persisting inflammation are hallmarks of SARS-CoV-2 GI manifesting disease. These are thought to be implicated in systemic disease manifestations, multi-organ involvement and possibly play a large role in “long-haul” COVID.2 Angiotensin converting enzyme 2 (ACE2) receptors are evident in many locations in the body including the renal tubules, lungs, brain, heart, luminal GI tract, and the liver [13]. Notably, the majority of the body’s ACE-2 receptors are found in the brush border of intestinal epithelial cells.2 SARS-CoV-2 infects epithelial cells through binding of its spike glycoprotein (S protein) to the ACE2 receptor [2,11- 12]. The binding causes fusion of the cellular membranes and a downstream effect that allows for internalization of the virus into the host cell. This subsequently leads to viral replication, viral shedding, and release of inflammatory cytokines [2].
Importantly for the gut, this binding has wide-ranging effects. The intestinal ACE2 receptor has a unique role in the stabilization of neutral amino acid transporters (e.g., B0AT1) which are responsible for uptake of amino acids (e.g., glutamine and tryptophan), the downstream metabolic products of which are important in maintaining immunity and healthy gut microbiota [13,14]. It has been shown in murine models that ACE2 receptor deficiency resulted in high susceptibility to intestinal inflammation through epithelial damage [15]. Thus, when either deficient in ACE2 or when bound by something such as COVID-19 glycoproteins, this down regulation effect has been shown to be associated with increased gut leakage and an increase in inflammatory markers such as IL-6 and fecal calprotectin [13–15].
The relationship between the systemic effects of COVID-19 and GI disease is complex and likely multifactorial. For example, the well reported respiratory effects of COVID-19 and the robust inflammatory reaction is associated with increased IL-2, IL-7, interferon gamma, tumour necrosis factor alpha, granulocyte colony stimulating factor. These wide-ranging systemic effects include infiltration of these inflammatory cells in the intestinal tract [11- 16]. Similarly, a study of SARS-CoV-2 infected non-human primate models showed either intranasal or intragastric virus inoculation resulted in pathologic changes in both respiratory and digestive tissues [17]. Thus, they concluded that inflammatory cytokines can play a role in development of both disease pathologies without direct inoculation of each respective tissue. To the contrary however is a recent article that analyzed human intestinal biopsy tissue samples from COVID-19 positive patients and found the absence of a pro-inflammatory response in the GI tract despite detection of SARS-COV-2 in the samples.18 This paralleled their results of reduced mortality in COVID-19 patients that had presented with GI symptoms [18]. Clearly, further studies are needed to better understand the pathophysiologic mechanisms, but it seems GI tract integrity and immune response play a large role in COVID-19 outcomes, severity, and likely long-term GI health.
“Long-haul” COVID, the Microbiome, and Dysbiosis
The gut microbiome has been shown to be a key regulator of bidirectional signaling between the enteric nervous system (ENS) and central nervous system (CNS), suggesting that gut function is controlled through a microbiota-gut-brain (MGB) axis [19]. It has been shown that gut bacteria produce metabolites, such as serotonin, tryptophan, and short chain fatty acids, that can influence gut-brain signaling through the MGB axis. Accordingly, disruptions in the microbiota composition have been shown to impact neurodevelopment, mood, and GI motility [2,19]. Dysbiosis, defined as significant shifts in the diversity of commensal microbiota compared to that of healthy individuals, is a common finding in patients with acute diagnosis of COVID-19 [20–22] . A study of saliva samples from 392 COVID-19 patients found that infected patients had less butyric acid-producing bacteria and more lipopolysaccharide-producing bacteria within the oral cavity compared to that of healthy controls [22]. Several fecal studies found similar microbial imbalances within the gut [2,23- 24]. It has been suggested that gut bacteria develop metabolites to modulate the inflammatory response and potentially influence the severity of COVID-19 infections.19 Gu et al. found that patients infected with SARS-COV-2 have enriched microbial communities of Streptococcus, Rothia, Veillonella, and Actinomyces, all of which correlated with elevated levels of the inflammatory markers C-reactive protein (CRP) and D-dimer [19-23].The related longterm effects of COVID-19 and gut dysbiosis is not yet well defined. Yeoh et al. found a correlation between gut microbiota composition and levels of cytokines and inflammatory markers [25] .Relative to healthy controls, COVID-19 patients had depleted commensal and opportunistic bacteria known to be anti-inflammatory and pro-inflammatory, respectively[25] .They noted this change through serial stool samples collected from patients up to 30 days post-diagnosis and found that gut composition remained significantly altered when compared with non-COVID-19 patients. Notably, this gut microbiota composition of 27 patients remained significantly distinct, regardless of whether they had received antibiotics (although, those that did receive antibiotics were more dissimilar). Species found to be significantly altered compared to healthy controls include an increase in Bifidobacterium dentium and Lactobacillus ruminis and a decrease in E. rectale, R. bromii, F. prausnitzii, and Bifidobacterium longum [25] . A small longitudinal study analyzing fecal microbiota samples taken at the time of diagnosis, at 2 weeks after hospital discharge, and at 6 months post-discharge found that microbiota diversity was still limited 6 months after recovery[26]. Interestingly, the patients were found to have lower gut microbiota richness at 6 months as well as higher levels of CRP indicating a relationship between the inflammatory response and the gut dysbiosis observed in COVID-19[26]. Further studies with a larger sample size are needed to better clarify these associations. Although research indicates an association between dysbiosis and the severity of COVID-19 infections, the pathogenic mechanism(s) by which SARS-COV-2 causes microbiota imbalance remains largely unknown [2-4]. As noted previously it is likely that virus effects a dysbiosis by downregulating ACE2 to promote inflammation and inhibit gut immunity. ACE2 controls expression of B0AT1, an apical neutral amino acid transporter whose substrates are responsible for down-regulating pro-inflammatory cytokines, maintaining tight junctions between cells, and promoting release of anti-microbial peptides. Therefore, low ACE2 expression ultimately compromises gut immunity, allowing for opportunistic microbiota to multiply, invade, and activate cytokine storms [2-4].
“Long-haul” COVID and Functional GI Disorders
Functional GI disorders (FGID) are conditions consisting of chronic or recurrent abdominal pain, such as dysmotility or visceral hypersensitivity, that develop through dysregulation of the MGB axis. Irritable bowel syndrome (IBS) and chronic dyspepsia are considered FGID [26,27]. Studies have found that more than 10% of individuals with infectious enteritis develop post infectious-IBS (PI-IBS) [2,28]. Although COVID-19 has been found to cause bowel inflammation, there is currently a paucity of studies regarding the incidence of post-acute FGID in COVID-19 patients [29]. Research has shown incidences of acute ileus (53%), diarrhea (28.8%), and constipation (39.4%) in infected patients who are critically ill [30]. Based on prior modeling data, COVID-19’s median length of 12 days increases the risk of PI-IBS development by 10-fold [2,31]. Taken together, a wave of FGID cases as a by product of the COVID-19 pandemic should be anticipated [2,29].
SARS-COV-2 addresses many factors that contribute to individual susceptibility to post-infectious FGID, including gut inflammation, intestinal microbiota composition, and mood. FGID most commonly occurs after a bout of generalized gut inflammation, a condition associated with SARS-COV-2 infection [2,29,30-32]. A recent study looking at 347 adults (164 COVID-19 positive and 183 controls) identified persistent GI symptoms and chronic fatigue through a web-based questionnaire about 5 months after infection. They found that after resolution of infection, severity of abdominal pain, discomfort, diarrhoea, and incontinence were greater in COVID-19 recovered patients compared with controls (31.7 vs 13.7%, p<0.001). They postulated the MGB axis playing a large role in these patients [31]. While eliciting an inflammatory response, SARS-COV-2 potentially inhibits gut immunity and compromises epithelial integrity to allow for dysbiosis [2,4]. COVID-19 patients with altered microbiota composition are linked to elevated inflammatory markers, such as CRP and D-dimer, suggesting that dysbiosis may promote subclinical inflammation long after the course of COVID-19 [2,4,29]. Interestingly, a systematic review has recently shown that dysbiosis within the small bowel is associated with functional dyspepsia, which is a type of FGID [32]. COVID-19 and other coronaviruses can cross the blood-brain barrier to affect the brain and mood, thus increasing the risk of FGID. [2,33-34]. Approximately 30% of COVID-19 patients experience neurological symptoms such as dysgeusia, disorientation, nausea, and neuralgia. Mechanisms through which this occurs are currently poorly understood.34 Esposito et al. proposed that SARS-COV-2 could potentially infect the ENS and ascend vagal afferent fibers to reach the CNS [35].This proposal was substantiated by a histological study of post-mortem COVID-19 patients that discovered expression of ACE2 and TMPRSS2 by small and large bowel enteric neurons and choroid plexus epithelial cells [2,34].Other proposed pathways to CNS invasion involve the circulatory and lymphatic system.33 Regardless of the route of neurologic invasion, SARS-COV-2 poses a threat to the gut-brain axis and has been shown to alter mood.2,36 In a clinical study of patients 1 month after recovering from COVID-19, 31%, 28%, and 42% of patients scored within ranges diagnostic for depression, anxiety, and PTSD respectively.36 Because inflammatory dysregulation contributes to the pathogenesis of many mood disorders, these findings suggest that COVID-19 may have psychopathological consequences [36,37].There is a strong link between IBS and mood, given that IBS patients are three times more likely to have depression or anxiety when compared to healthy patients [19,38]. However, two-thirds of comorbid patients were diagnosed with IBS prior to experiencing mood symptoms, suggesting that both systems influence each other bidirectionally [19]. Although Ha et al. reported that serotonin levels are elevated in COVID-19 patients with diarrhoea, it is unclear whether elevated levels can be attributed to the effect of SARS-COV-2 on the CNS, gut, or both [4,36] .To further complicate the pathophysiological connection between SARS-COV-2 and FGID, gut microbes are also known to produce serotonin that can potentially influence gut motility [19].Therefore, much remains unclear as to the causality specifics between COVID-19 dysregulation of the MGB axis and resultant FGID.
“Long-haul” COVID, the Liver, and Biliary System
Liver injury is a common manifestation in patients with COVID-19, with up to 72% of patients with acute infection demonstrating liver impairment through transaminitis. Approximately 6% of patients develop severe liver injury, defined as alanine aminotransferase (ALT) >5x the upper limit of normal [39]. Severe acute liver injury has been associated with poorer disease outcomes, including increased intensive care unit admissions, mechanical ventilation, and mortality [39] . In addition to elevated aminotransferases, markers of liver function affected in severe liver injury include decreased albumin, elevated INR. Bilirubin typically is non-elevated to modestly elevated, overall suggestive of a hepatocellular pattern of injury [39]. Long-term effects of COVID-19 on the liver are still being elucidated. One study looking into liver tissue of 60 patients that died of COVID-19 found that with vascular injury from the disease and subsequent necrosis, there was an activation of intrahepatic stem cells and showed signs of aberrant regeneration [40]. Another study of 5 patients that recovered from infection showed residual viral antigens detected in both intestinal and hepatic tissues up to 180 days after testing negative for SARSCoV- 2 [41]. In addition to factors such as direct ACE2-mediated viral entry into cholangiocytes with cytokine-mediated damage, the use of medications during acute infection may confound the pattern of disease-related liver injury through drug-induced liver injury (DILI) [42,43]. Most commonly, acetaminophen/paracetamol is used to manage fever and body aches. COVID-19 therapies utilized, including hydroxychloroquine, antivirals (lopinavir, ritonavir, remdesivir), and JAK inhibitors (baricitinib), can all contribute to hepatocellular injury, and combination of multiple hepatotoxic medications with ongoing disease can potentiate this effect [43]. Population studies further out from COVID-19 diagnosis can help determine the long-term effects of liver injury and clinical implications at risk due to COVID-19 disease. Alternatively, about 12% of patients with acute COVID-19 develop cholestatic injury, with bilirubin > 3x upper limit of normal [44]. Some patients with cholestatic injury have persistence of jaundice and cholestasis following recovery from acute infection, suggestive of cellular damage to the biliary ductal cells in the pattern of secondary sclerosing cholangitis in critically ill patients (SSC-CIP) [45]. SSCCIP following COVID-19 has been referred to as post-COVID-19 cholangiopathy and has been associated with rapid progression to cirrhosis [46]. Various causes have been proposed for pathogenesis of this disease pattern, including DILI, hypoxic injury, direct viral effects, and damage from systemic inflammation (i.e. cytokine storm) [47]. Limited treatment options exist for SSC-CIP, with the exception of liver transplantation. One center has demonstrated successful orthotopic liver transplantation in a patient with post- COVID-19 cholangiopathy [48].
Therapeutic options for “long-haul” GI-COVID-19
Although there are currently no approved therapeutics preventing post-COVID-19 GI diseases or symptoms, there have been proposed options similar to those targeting the lungs, as the virus’ binding and internalization mechanisms are similar in both organ systems [2]. Promising drugs that are currently in clinical trials include recombinant human ACE2, Ang 1-7 agonists, monoclonal antibodies targeting the ACE2 receptor, and a TMPRSS2 inhibitor known as camostat mesylate [4,13]. As stated previously, the underlying mechanism of GI COVID-19 involves the ACE2 receptor which is important for viral invasion. Thus, utilizing pharmaceuticals to bind to these receptors may help alleviate the direct invasion and the systemic down-stream effects that the infection can cause the body. Currently, treatment of post-COVID-19 GI disease most aligns with rest, nutritional support, and case-bybase symptom management. As stated prior, there has been an increased use of laxatives, antiemetic agents, histamine antagonists, antacids, or anti-diarrheal agents seen recently, but care should be taken to ensure that the medications are not potentially prolonging infectiousness by modulating gastric pH or affecting the microbiome adversely [10]. Widespread treatment protocols using of these drugs have not been shown to have great efficacy. For example, a male COVID-19 patient with persistent diarrhoea successfully recovered while on a regimen of lopinavir-ritonavir, IFN-α2b, and acetylcysteine [49]. However, a clinical trial of 199 patients found lopinavir-ritonavir to have no therapeutic benefits for COVID-19 [50]. Given the role of the microbiome in the pathogenesis of postcovid dysbiosis, potential treatment options may include targeted probiotic treatment. The utility of these lies in the production of antiviral metabolites as well as the support of adaptive immunity [2,51]. The Chinese University of Hong Kong recently reported use of an oral microbiome formula which is targeted specifically for COVID-19. Although the formula is patent pending, and thus the contents is not public knowledge, the researchers working on it have mentioned that it contains several strains that were found missing from COVID-19 positive patients. Some of these strains may be Fecalibacterium prausnitzii, Lachnospiraceae bacterium, Eubacterium rectale, Ruminococcus obeum, and Dorea formicigeneran [52]. In an unpublished study, hospitalized patients with COVID19 showed resolution of symptoms and reduced proinflammatory markers in patients who received the reported formula [51]. Furthermore, Chinese National Health Commission has recently recommended probiotics to maintain intestinal microecological balance and prevent secondary bacterial infections [53]. Despite this, the rationale behind probiotic use is based on indirect evidence as animal studies failed to show changes in ACE 2 receptor expression after inoculation with lactobacilli and bifidobacterial [16]. More robust pre-clinical and clinical studies are needed to better define the role of probiotics and COVID-19.
Conclusion
There is evolving data from extended longitudinal follow-up of patients affected by COVID-19, that there is a significant cohort with persistent GI symptoms (including abdominal pain, discomfort, diarrhoea, and incontinence) even after resolution of respiratory symptoms and outside the infectious window of acute disease. The spectrum of long-haul COVID-19 has not been well characterized in the medical literature, particularly as it pertains to gastrointestinal pathophysiology. It appears that COVID-19 virus enters a variety of different GI tissues including the liver, biliary tree, and epithelial cells lining the GI tract. The resulting dysbiosis of the GI tract leads to disruption to the MGB axis and can affect the acute illness, severity, and ability to recover from disease. It may also lead to wide-ranging clinical presentations of functional GI disorders, with symptoms persisting many months, hence a new recognition of “long haul” GI COVID. It is imperative for clinicians to be aware of post-COVID-19 GI manifestations in patients who have a history of either confirmed COVID-19 or a suspected clinical history. Recognizably, COVID- 19 infection may not have initial typical symptoms but it is unclear if these cases may still result in more “long haul” consequent effects. It is also unclear as to the duration of these “long haul” symptoms and pathophysiologic changes. Clearly some of the effects such as loss of gustatory or olfactory function can have major effects on quality of life. Future research is clearly needed, but at present, there is even more rationale for disease prevention by vac
cination!
For more Lupine Publishers open access journals please visit our website:
https://lupinepublishers.com/index.php
For more Current Trends in Gastroenterology and Hepatology articles please click here: https://lupinepublishers.com/gastroenterology-hepatology-journal/index.php
#open access journals#submissions#article#lupine publishers#lupine journals#gastritis#hepatology#endoscopy
0 notes
Photo

Big Deal 20% Off In All Our Prints From Website. Hurry Up and Don't Miss this Deal! Only For a Limited Time. #artprint #prints #printshop #posterdesign #posters #posterart #posterstore #vintageposters #minimalposter #minimalstyle #bohemian #blackabdwhite #abstractartwork #abstractposter #abstractprint #murellosart
0 notes
Photo

Color Wave 06
#designposter#visualgraphics#abstractposter#geometric#posterseries#graphicdesign#designinspiration#designfeed#posterart#posterdesign#posterchallenge#thedesignblacklist#minimalisticdesign#abstractdesign#postereveryday#blankposter#posterjam#dailyposter#printdesign#collectgraphics#posterdesigncommunity#manos_mankou#athens#greece
1 note
·
View note
Link
Visit Panda Avenue on Etsy.
Abstract Watercolour Wall Art, Earth Tones, Printable Digital Download, Bohemian, Abstract Art Download, Boho Art
https://www.etsy.com/ca/listing/772635188/abstract-watercolour-wall-art-earth?ref=tumblr
#digitaldownloadart#printabledownload#diywallart#midcenturymodern#abstractposter#abstractprintable#bohoposter#abstractdownload#midcenturyposter#printableart#art print#download art#etsy#etsydecor#etsydigital#artists on tumblr
3 notes
·
View notes
Text

Poster / cover design made by me & follow for more creative content
1 note
·
View note
Photo
2 notes
·
View notes
Photo

Prints are now available on my @society6 shop 👉 society6.com/leaboratory If you wish any prints, that you don’t see there, let me know. 🙌 #behance #graphicdesigndaily #designfeed #itsnicethat #tdkpeepshow #artposter #dribbble #graphicartists #abstractposter #visualdesigns #designinspo #artprints #printableart #printableartwork #printmaker #projectmono #editorialillustrations #printart https://www.instagram.com/p/CDYua97h_dF/?igshid=1ilvyvtpe2yml
#behance#graphicdesigndaily#designfeed#itsnicethat#tdkpeepshow#artposter#dribbble#graphicartists#abstractposter#visualdesigns#designinspo#artprints#printableart#printableartwork#printmaker#projectmono#editorialillustrations#printart
4 notes
·
View notes
Text

DRAMA #03
-
Poster / magazine cover. Thought it turned out pretty cool.
#posterdesign#abstractposter#graphic design#magazine cover#art#typeposters#my art#my design#photoshop#posterart
1 note
·
View note
Photo

"Lynx." Swipe left for details ➡️ Let me know your thoughts in comments. #postercolor #helveticaposter #digitalarchive #typeinspire #slantedpublishers #posterdesigncommunity #nicogscollection #generaleclectics #graphicdirectory #graphicindex #designergrafico #posterveryday #posters #betype #albumart #posterlabs #communicationdesign #abstractposter #wallposter #postershop #posterstore #fruitsartclub #visualgraphc #mukeshbasu https://www.instagram.com/p/CPdSi-nAGzK/?utm_medium=tumblr
#postercolor#helveticaposter#digitalarchive#typeinspire#slantedpublishers#posterdesigncommunity#nicogscollection#generaleclectics#graphicdirectory#graphicindex#designergrafico#posterveryday#posters#betype#albumart#posterlabs#communicationdesign#abstractposter#wallposter#postershop#posterstore#fruitsartclub#visualgraphc#mukeshbasu
0 notes
Photo


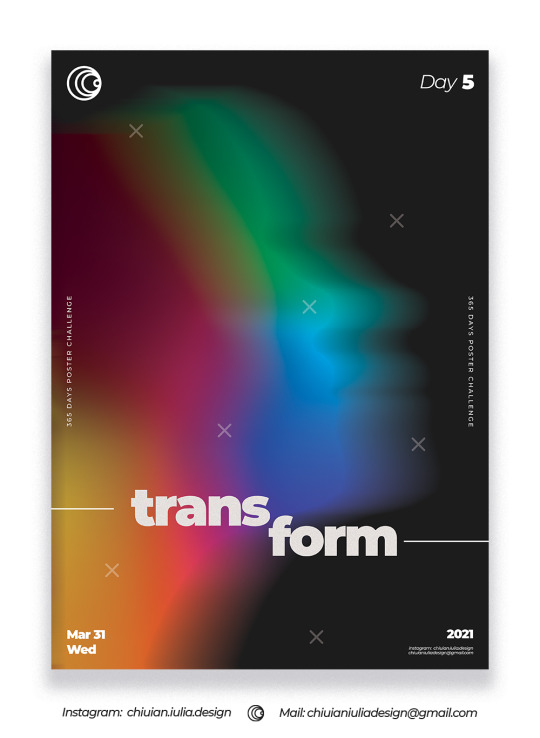


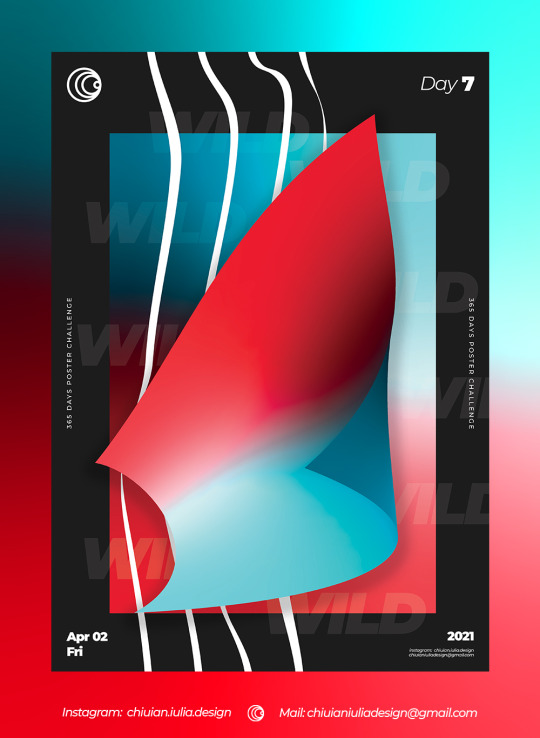
A Poster a Day Challenge- C.I. Design
First week of posters :)
365-day challenge - poster design by Chiuian Iulia.
Contact for purchase :
Mail: [email protected]
Whatsapp: +40 755 665 437
Fiverr: www.fiverr.com/iuliachiuian
Branding/Rebranding: https://www.fiverr.com/iuliachiuian/do-branding-or-rebranding
Logo Design: https://www.fiverr.com/iuliachiuian/design-an-awesome-unique-minimalist-logo
Social Media Design: https://www.fiverr.com/iuliachiuian/design-premium-social-media-posts
Portfolio: www.behance.net/iuliachiuian
0 notes
Photo
6 11 20
Série /
JoceOffice
0 notes
Photo

Dark green abstraction. . . . . . . . #lirosastore #poster #posterlovers #posterart #abstractart #abstractposter #greeneryinterior #greendecoration #livingroominterior #greenartdecoration #livingroomdecoration #livingroominspirations #livingroomidea #livingroomideas #livingroomdecorideas #livingroomdecormalaysia #livingroomdecorating #livingroomdeco #homeinspiration #apartamentdecore #apartmentideas #apartmentideas https://www.instagram.com/p/CCJ5bl9p6SD/?igshid=dj1eldi7alzz
#lirosastore#poster#posterlovers#posterart#abstractart#abstractposter#greeneryinterior#greendecoration#livingroominterior#greenartdecoration#livingroomdecoration#livingroominspirations#livingroomidea#livingroomideas#livingroomdecorideas#livingroomdecormalaysia#livingroomdecorating#livingroomdeco#homeinspiration#apartamentdecore#apartmentideas
0 notes
Photo
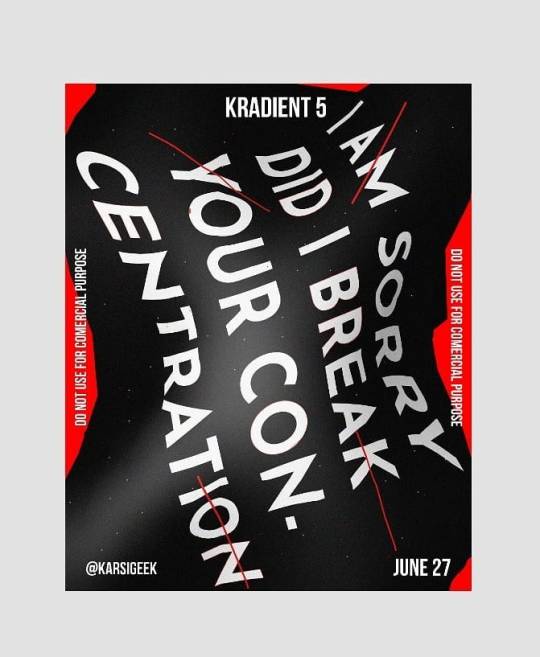
Post - Kradient 5! . People tagged in this Post are selected RANDOMLY.... . Clothing Effect Poster Softwares used - Adobe illustrator & Adobe Photoshop Time Consumed - 1-2 Hours (For Creating This)! . If you like it you can support me by sharing these posts to others :) . Swipe =====> ! . YouTube - KarsiGeek ! Facebook - facebook.com/KarsiGeek.official/ ! Pinterest - Goalsachievers ! Email - [email protected] ! . #karsigeek #karsi #baugasm #cinema4d #photoshop #share #creative #art #digitalart #poster #abstractposter #abstractart #abstract #clothingeffect #effects (at Cinema 4D Studio) https://www.instagram.com/p/CB7TPq8HVGc/?igshid=1hg01uke8nz2v
#karsigeek#karsi#baugasm#cinema4d#photoshop#share#creative#art#digitalart#poster#abstractposter#abstractart#abstract#clothingeffect#effects
0 notes
Link
Visit Panda Avenue on Etsy.
Printable abstract poster. DIY print. Abstract art. Digital download art print. Collage wall art.
https://www.etsy.com/ca/listing/791995223/printable-abstract-poster-diy-print?ref=tumblr
#digitaldownloadart#printabledownload#diywallart#linedrawing#lineartprint#midcenturymodern#lineartposter#abstractposter#abstractprintable#minimalistposter#bohoposter#abstractdownload#collageposter#Etsy#PandaAvenue#Interior Design#Home Decor#Wall Art#Wall Decor#Printable Art#Art Download
2 notes
·
View notes