#hla b27
Video
youtube
Be like Detective Pikachu, but don't forget Shin Chan!
Anterior Uveitis & Axial SpA - HLA-B27 Testing, Features, Support?
· • —– ٠ ✤ ٠ —– • ·· • —– ٠ ✤ ٠ —– • ·· • —– ٠ ✤ ٠ —– • ·
The most common type of Uveitis (inflammation in the eye) is anterior uveitis, or iritis, and almost 50% of patients with this condition test positive for the genetic marker HLA-B27.
Having a positive result could potentially help establish the diagnosis, guide treatment, and provide information about prognosis. It can help avoid unnecessary diagnostic workup too. But it's a grey area as both false negatives and false positives can happen. Asking questions is key and results should be interpreted in the context of the full clinical picture.
#uveitis#axialspa#ankylosing spondylitis#hla b27#pikachu#pokemon#detective pikachu#shin chan#spondylitis#house md#hugh laurie#axial spondylarthritis#iritis#scleritis#psoriasis#ibd#inflammatory bowel disease
1 note
·
View note
Text

[ID: the “wait, it’s all [blank]” meme of one astronaut pointing a gun at the other, edited to read “wait, it’s all celiac?” / “always has been.” with the word celiac in a groovy pink font. end ID]
happy celiac awareness month 💓🖤💓 folks expressed interest in my #Controversial Opinion, so here we go:
as someone who “has” non-celiac gluten intolerance, i don’t believe it exists.
this, as with all of my diagnostic opinions, is built from both health research & sociology, specifically the genealogy of (my) disabilities – how the labels we use & the divides we create between diagnoses are socially constructed. conditions don’t announce themselves as discrete entities; instead, labels are given based on, at best, current medical understandings of symptoms + clinical visualization measures (imaging, bloodwork, genetic testing, etc). conditions that were once considered two separate things may eventually be restructured under the same diagnostic label, & what was once considered one singular disease may be divided into separate categories, in response to new information or the new recognition / respect of existing information.
the issue with this system, though – with access to healthcare which is predicated upon diagnosis, which is itself predicated on checklists of symptoms & clinical visibility – is that we don’t know shit. our bodies are not required to present symptoms in accordance with the ICD 10, & chronic illnesses are very much an “ask four doctors, get five answers” situation.
for example: without any of my symptoms, imaging, or bloodwork changing, i’ve been diagnosed with active ankylosing spondylitis, ankylosing spondylitis that is in remission, fibromyalgia, & spondyloarthropathy. the only difference is the doctors: their belief or lack thereof in my symptoms, their familiarity with current research, & the diagnostic systems they abide by. under the NHS, it was definitionally impossible for me to have ankylosing spondylitis that was not visible on an MRI, therefore i must have been in remission, even as my symptoms were just as debilitating as before & treatable by immunosuppressants.
how this pertains to celiac: as with all chronic illnesses, symptoms of celiac disease are a broad spectrum. some people have severe growth impairment from a young age; others may only have minor skin manifestations. other common symptoms are vague & potentially attributable to any chronic illness, such as fatigue, depression, & gastrointestinal issues. crucially, though, damage to the small intestine is still occurring even in people with celiac who do not flare after consuming gluten.
following this,
the diagnosis of non-celiac gluten intolerance has nothing to do with symptom presentation or severity. it doesn’t even mean there is no clinically visible damage to the small intestine. rather, it just means you didn’t pass the test:
in my case, not only was the (notoriously unreliable) antibody blood test negative, but so were subsequent tests for the genetic markers associated with celiac.
two people with the same exact experiences can get put into two different boxes, solely based on bloodwork – but that’s not how genetics works. it’s pretty much impossible that only those two markers dictate whether or not someone has celiac, or any given disease, because genetics are infinitely more complex than that; equally, plenty of autoimmune disorders can have a genetic component but are not exclusively found in people with that particular marker (ankylosing spondylitis & HLA-B27, for example).
therefore, i firmly believe non-celiac gluten intolerance is celiac disease, just influenced by other genetic factors and/or antibodies we haven’t yet identified.
there are a whole host of issues created by the false divide of celiac vs non-celiac gluten intolerance, certainly including things i’ve never considered, but here are a few examples of what i refer to as diagnostic violence, the physical & social consequences of these forms of categorization:
celiac disease increases people’s risk for small bowel cancer. but if it’s been determined by the medical establishment that according to their criteria, you don’t have celiac disease, then you won’t receive cancer screening.
since a food intolerance is not considered an autoimmune disease, there is no medical evidence of an underlying cause of arthritis, for example, making it that much harder for people to receive diagnosis & treatment for autoimmune symptoms.
diagnostic paperwork & a letter from a doctor is almost always required to receive accommodations, & food-related accommodations are notoriously difficult to obtain at universities which require the purchase of a meal plan without sufficient gluten-free options, for example.
as a response to the dangerous ableism permeating societal attitudes toward gluten-free food, many people (diagnosed) with celiac fall back on communicating the seriousness of their needs at the expense of their undiagnosable peers. “it’s not just an intolerance!” i read over & over – never mind that gluten made me so sick i lost a significant amount of weight, my hair fell out, i had signs of multiple vitamin deficiencies, & i could only keep down liquids.
this is honestly the most blatant example i’ve come across of the complete arbitrariness of diagnostic categories, but it’s far from the only one, & i’d love to hear other folks’ controversial opinions – what physical disabilities do you tell people you have without a diagnosis? do you consider yourself to have that condition, or is this just for expediency of communication? how does your undiagnosability affect your interactions with community formed around that diagnosis?
your experiences are real, your symptoms are serious, & it is not your fault that white supremacy demands a categorizability which all bodies inherently fail. join the club – we’ve got plenty of gluten-free snacks. 💓🖤💓
#celiac#celiac disease#dietary restrictions#gluten intolerance#gluten free#sociology#disability studies#diagnosis is a form of violence#abolish the clinic#mac.txt#image described
79 notes
·
View notes
Text
Quick Health Update
I went to my new rheumatologist's office two weeks ago today. Instead of seeing the rheumatologist, I saw the PA. I honestly don't know how I feel about him.
My pediatrician who gave me my wheelchair prescription said we could probably ask the rheumatologist where we could fulfill it.
We asked the PA how we could fulfill it and instead of initially answering the question, he said "my job is to prevent patients from using wheelchairs by using biologics". 💀💀 Bro, that wasn't the question. What gets me is that I wasn't even asking him for a prescription. I already had one, which means a doctor has already confirmed that I need a wheelchair. My prescription literally has the words "needs a wheelchair" on it.
So red flag 1 was the PA trying to discourage my use of a wheelchair, even though my primary doctor clearly stated I needed one.
I had back pain that day, so he wanted to run a couple tests to see if I have ankylosing spondylitis. I got 12 vials of blood taken from me to check for the HLA-B27 gene marker. And I got an X-ray done on my SI joints. I tested negative for the gene, I have yet to see the results of my X-ray--my parents need to take me to pick it up this weekend, probably Thursday.
He didn't examine my back or my contractured arm, just grabbed my hands and put pressure on them all the way up my arms, asking if I had any pain. It was a weird examination ngl
He then gave me a week's worth of methylprednisolone (a corticosteroid) that has a specific regimen to follow seemingly and told me to "take it as needed". Those instructions are odd.
I'm going to go to my pediatrician next week to ask about the steroid because it technically can increase the risk of stomach bleeding since I'm taking naproxen. Which also gets me because the PA, when my mom asked if I could take the steroid and naproxen together, said that I could take them together, when it's not recommended to take them together if it's possible to avoid it. But, if you can't avoid it, definitely don't take it at the same time, which the PA seemed to imply that I could do.
He ordered the two tests, gave me steroids to "take a s needed" and told me to go back in two months.
It was a weird appointment 💀
5 notes
·
View notes
Note
I have realized that doctors and fat phobia thing is a universal experience .
I'm HLA-B27 positive and all my life dealt with arthritis . I used to be a very active kid , I still am despite me ending up in pain . I'm 5'8 and around 2018 I got diagnosed with pcod and I gain weight kinda ended up at 62kg . Which is definitely not a plus size person but I have never been over 56 kg in my entire life . During the same time my another classmate got diagnosed with pcos and she was 88kg at that time . The way that doctor didn't even told me to exercise and just prescribed me some meds and my friends repeatedly got told how if she lost weight the problem will be 90% over . It still bothers me. You know most people really don't care about your health . They just care about how you look . Pretty privilege as well as skinny privilege is real . Last year my health went really down hill and I lost a lot of weight . some of my friends complimented that stuff despite me telling them I couldn't leave my bed cause my joints were killing me . My whole body was giving up on me but They were like, at least you look great in all those outfits . I mean mate I had few asthma attacks , my hemoglobin was at 8 . I lost over 8kilo in few months by doing nothing just laying in my bed cause my body hurts . Unfortunately this kinda people ends up being doctors too . I truly hope people find good doctors who will listen to them . I'm grateful I found 2 really great docs who not only listened to me but also helped me feel emotionally better . Bro literally prescribed me fluoxetine . I would forever remain grateful for that . A good doctor can change so much in a person's life . I hope these people realize that their words can actually make or break many people's lives .
I swear to the almighty, if any doctor ever tries telling me to lose weight, I'm walking out of there without paying.
22 notes
·
View notes
Text
((So I saw my endocrinologist the other day and she has an idea about my 10 year + mystery back pain.
So she’s sending me for a blood test to look for a specific gene marker she called HLA-B27.
She asked me if there’s a family history of rheumatoid and/or psoriasis and yeah my grandmother on my mothers side has both and my mother has one because apparently this gene marker can present as one or both of those issues but can also potentially cause early onset arthritis and maybe even my ongoing mystery back pain.
So I might finally get an answer after all this time))
3 notes
·
View notes
Text
Not doing so hot tbh.
My Rheum thinks what I've got going on is inflammatory arthritis. Haven't narrowed it down quite yet but I can say, I'm pretty sure it's not rheumatoid, as my joints move fine usually (loss of ROM is from pain or stiffness, joints still move smoothly), I don't have psoriasis, or GI issues like crohn's or colitis, nor have I had an infection in any joints. So that basically narrows it down to: Ankylosing Spondylitis, or non-radiographic axial spondyloarthritis (sp?).
Which... My dad has AS with several fusions in his lumbar vertebrae. Partly surgical from an injury, but more Ankylosed further up after the damage.
I have the generally expected morning stiffness, can't stay still for long (though this doesn't mean I'm active, just fidgety and I move my legs/hips and pop/stretch my back a lot), and had pain in my shins and feet when I did walk and stand a lot. Not so much now but I don't spend much time standing. The tendons/ligaments in my hips are so tight it feels like steel cables. It's gross and it hurts. I don't have eye issues at the moment. And I am HLA-B27-. So I kind of suspect nrAxSpa rather than AS unless my SI joint is worse than I expect. I am getting xrays soon (again, in HD) of my spine, one shoulder that's swollen, and my SI joint.
I hope it's not AS, I don't want a degenerative autoimmune condition but considering my dad with AS and my sister with Lupus, it seems kind of inevitable.
I had been preparing myself for a fibromyalgia dx to be honest.
Anybody have tips? Meds that worked if you have AS? Tips for coming to terms with a scary diagnosis? I don't want my spine to fuse, it really scares me. I'm already in enough pain.
#ankylosing spondylitis#non radiographic axial spondyloarthritis#autoimmune disorders#Coping with chronic illness
24 notes
·
View notes
Text
awesome... just got a call back from my doctor with my autoimmune blood test results and evidently my HLA gene is fucked up and i'm HLA-B27 positive 👍
so now it's rheumatologist time to find out if my spine is fucking fusing itself together... wooo my bones ache so funnnnn
#chronic pain#chronic illness#disabled#physically disabled#actually disabled#ankylosing spondylitis#autoimmune#joint pain#back pain#yayyyy..... /s
10 notes
·
View notes
Photo

El primer sábado de mayo se celebra el Día Mundial de la Espondilitis Anquilosante, una patología inflamatoria, crónica y progresiva de origen inmunitario que afecta al 1% de la población a nivel mundial.
Con la creación de esta efeméride se pretende visibilizar las causas e impacto de esta enfermedad autoinmune. Asimismo, sensibilizar a la población acerca de la importancia de efectuar un diagnóstico oportuno o en fases tempranas.
¿Qué es la Espondilitis Anquilosante?
La Espondilitis Anquilosante (EA) es una enfermedad de origen inmunitario e incurable, asociada con un alelo HLA-B27. Se caracteriza por una degeneración e inflamación crónica, de los tejidos de las articulaciones de la columna vertebral y sacroilíacas.
Causa dolor e incapacidad, así como el endurecimiento paulatino de las articulaciones. Ocasiona una flexibilidad reducida en la columna vertebral, generando una postura encorvada hacia adelante.
Esta enfermedad reumatológica puede tener una predisposición genética y suele manifestarse en adultos jóvenes, con edades comprendidas entre los 20 y 30 años. Es más común en hombres que en mujeres.
Algunos de los síntomas y manifestaciones más frecuentes de la Espondilitis Anquilosante son los siguientes, tomando en cuenta que los mismos disminuyen con el movimiento. Es recomendable acudir a consulta médica para descartar esta enfermedad:
Dolor agudo en la parte baja de la espalda por más de tres meses.
Rigidez matutina, con al menos una hora de duración.
Limitaciones para expandir la caja torácica.
Dolor e inflamación en hombros, rodillas, talones, tobillos y cuello.
¿Sabías Que?
Conoce algunos datos importantes acerca de la Espondilitis Anquilosante (EA):
Se estima que en América Latina la prevalencia de esta enfermedad es de 10,2 por cada 100.000 habitantes.
Al no detectarse y tratarse a tiempo, esta enfermedad puede derivar en discapacidad física, pérdida de la independencia, angustia emocional y disminución de la integración social.
Entre el 5 y el 10% de los pacientes presentan una patología intestinal inflamatoria sistemática y generalmente asintomática.
No se ha establecido una cura definitiva para esta enfermedad, la cual debe ser controlada por un médico reumatólogo y un equipo de especialistas para mejorar el desempeño físico y emocional del paciente.
Se estima que en España más de medio millón de personas padecen esta enfermedad.
¿Cómo se celebra este Día Mundial?
En la celebración del Día Mundial de la Espondilitis Anquilosante se llevan a cabo eventos, charlas y conferencias presenciales y virtuales, con la participación de especialistas de salud, investigadores, pacientes y público general para dar a conocer información acerca de los alcances de esta enfermedad reumatológica.
Algunas edificaciones públicas y otras instalaciones se iluminan de color azul, como símbolo de solidaridad con los pacientes que padecen de esta enfermedad y sus familiares.
Comparte información útil e interesante sobre el Día Mundial de la Espondilitis Anquilosante en las redes sociales. Utiliza los hashtags #DíaMundialEA #EspondilitisAnquilosante #diamundialespondilitisanquilosante #WorldASDay
2 notes
·
View notes
Text
https://www.maxlab.co.in/blogs/hla-b27-test-overview-procedure-result
HLA-B27 Test: Overview, Procedure And Result
The HLA-B27 test detects the presence of the HLA-B27 antigen to help diagnose & manage autoimmune disorders like ankylosing spondylitis, and reactive arthritis. Know more about the HLA B27 Test.
0 notes
Text
The US Axial Spondyloarthritis market is anticipated to reach a ~USD 2.3 Bn. industry by 2028: Ken Research
The United States Axial Spondyloarthritis market which currently has a market size of ~USD 1.3 Bn. is projected to grow at a CAGR of ~9.5% in the next five years as per the findings of Ken Research.
Story Outline
Rising cases of Axial Spondyloarthritis pose as a demand for the correct diagnosis and treatment of AxSpA which helps in the growth of US AxSpA market.
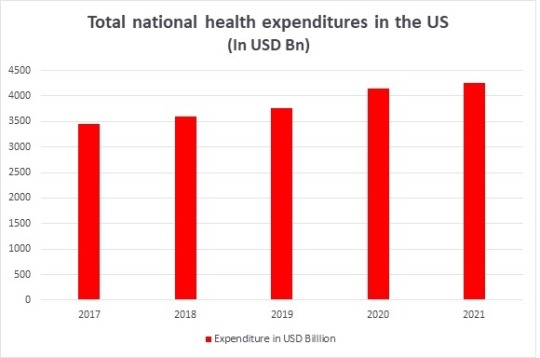
Increasing US health expenditure allows hospitals, research institutes and pharmaceutical company to research, diagnose, and treat AxSpA thereby accelerating the US AxSpA market.
Technological advancements in diagnosing AxSpA such as MRI, CT scan, and ultrasound can provide early and correct diagnosis which pumps the US AxSpA market.
Availability of various treatment options also help in the effective and efficient treatment of AxSpA which contributes in the growth of US AxSpA market.
A fast growing industry, rising cases of Axial Spondyloarthritis, increasing health expenditure, and technological advancements along with the availability of many treatment methods are the various reasons that are contributing to the growth of US Axial Spondyloarthritis market. This market is projected to grow at a CAGR of ~9.5% in between 2022-2028.

Click to read more about US Axial Spondyloarthritis market
Rising cases of Axial Spondyloarthritis: accelerating the US AxSpA market

Click to Download a Free Sample Report
Axial Spondyloarthritis is group of inflammatory disorders which have the traits of autoimmune diseases. It is primarily of two types, i.e., Ankylosing Spondylitis and Non-radiographic Axial Spondyloarthritis. The prevalence of Axial Spondyloarthritis is very high in the United States. It ranges in between 0.9% to 1.4%. Moreover, in the United States, more than 3 million people suffer from Axial Spondyloarthritis.
It’s one of the most common subtype, i.e., Ankylosing Spondylitis almost affects 1% of the US population. Its second type, i.e., Non-Radiographic Axial Spondyloarthritis affects about 0.5% of the US population. Speaking of its incidence rate, it was 0.39 in 2007 and rose from 0.39 to 0.57 in 2017. It is clear that the cases of Axial Spondyloarthritis is only rising in the United States and we will be seeing more cases of it in the near future.
Axial Spondyloarthritis is primarily caused by the presence of HLA-B27 gene and a high number of people in the US have this gene which increases their chances of developing Axial Spondyloarthritis in the future.
Overall, the prevalence of this gene is 3.5% in overall US population. Almost 7.5% of the Hispanic-White people have this gene. This gene is present in about 4.5% of the American-Mexican people. Lastly, 1% of Black-Non-Hispanic people have this gene. With such high prevalence of Axial Spondyloarthritis, there becomes a greater need to correctly diagnose the patients and furthermore, correctly treat them which ultimately helps in the growth of US Axial Spondyloarthritis market.
Rising health expenditure: contributing in the growth of US AxSpA market
Click to Download a Free Sample Report
The national health expenditure in the US has been constantly rising in the United States. The rising health expenditure helps hospitals, research institutes and pharmaceutical companies in correctly diagnosing and treating AxSpA. It also helps pharmaceutical companies in developing more medicines and therapies to help in the effective and efficient treatment of AxSpA.
In 2017, the US government made a health expenditure of ~USD 3.4 Tn. In 2018, ~USD 3.6 Tn. worth of expenditure was made in the healthcare sector. In 2019, this amount rose to ~USD 3.7 Tn. In 2020, a healthcare budget worth of ~USD 4.1 Tn. was allocated. Lastly in 2021, the US government made a healthcare expenditure of ~USD 4.2 Tn.
As it is evident, that the healthcare expenditure in the United States have only been rising and it is projected to rise further in the upcoming years. The rising expenditure would allow hospitals, diagnostic laboratories, pharmaceutical companies and research institutes to research, diagnose, and treat Axial Spondyloarthritis along with develop first line medicines and alternative therapies to effectively treat Axial Spondyloarthritis.
Technological advancements: a boon for the US Axial Spondyloarthritis market
Visit this Link: – Request for custom report
Various technologies are used in the effective and correct diagnosis of Axial Spondyloarthritis. Some of the most common technologies used in the diagnosis of Axial Spondyloarthritis include Magnetic Resonance Imaging (MRI), Ultrasound, Gene Testing, and Computerized Tomography (CT) scan.
A Magnetic Resonance Imaging (MRI) is the most common method of diagnosing Axial Spondyloarthritis. This technology works by taking the cross-sectional images of your body parts with the help of radio waves and magnetic field.
It has a success rate of almost 80 to 97%. It helps in AxSpA diagnosis as it has the ability to detect early changes happening in the Sacroiliitis.
Ultrasound is another technology that is primarily used to diagnose AxSpA. It works by sending the body sound signals or ways as the internal body is examined. It is primarily used to take a look at the inflammation of Sacroiliac Joints to diagnose Ankylosing Spondylitis. The success rate of ultrasound ranges from 90% to 97%.
A Computerized Tomography (CT) scan is another technology that is used to diagnose AxSpA. It provides valuable information in regard for osteoporosis, ankyloses, erosion etc. which extremely helps in making the correct diagnosis of AxSpA. This scan has a success rate of almost 85%.
Thus, technology is indeed a boom for the US AxSpA market as the task of correctly diagnosing ankylosing spondylitis and non-radiographic Axial Spondyloarthritis has become greatly easier. With these technological advancements, early diagnosis is made which accelerates the US AxSpA market.
Availability of many treatment methods:
Request free 30 minutes analyst call
There are many treatment options when it comes to Axial Spondyloarthritis. NSAIDs, Biologics, Analgesics, and Glucocorticoids are primarily used in the effective treatment of Axial Spondyloarthritis.
NSAIDs is an initialism for Non-Steroidal Anti-inflammatory drugs. These drugs are the first line treatment of AxSpA which causes high pain and inflammation. These drugs reduce the pain and inflammation. The most common NSAIDs used in the treatment of AxSpA include Ibuprofen, Naproxen, and Diclofenac.
Biologics are another set of medications that are primarily used to treat Axial Spondyloarthritis. These medicines are generally given to such patients who do not respond to NSAIDs. Common biologics used to treat AxSpA include Adalimumab, Etanercept, Infliximab, Crtolizumab pegol, etc.
Sulfasalazine is a type of anti-rheumatic drugs which is primarily given to patients who complain of pain in other joints than the spine and pelvis ones. Moreover, this drug also has is known to make your back less painful and stiff.
Glucocorticoids can be best described as a type of steroids which are generally given for pain relief. These are anti-inflammatory and generally come in the form of injections.
Thus, there are many treatment options available for the treatment of Axial Spondyloarthritis. As the treatment options are widely present, more and more patients widely benefit from them which ultimately accelerates the US AxSpA market.
Conclusion
Axial Spondyloarthritis is an inflammatory health condition which is of two types, Ankylosing Spondylitis and Non-Radiographic Axial Spondyloarthritis. The US AxSpA market is associated with the diagnosis and treatment of AxSpA.
There are various factors responsible for the growth of this market which include rising cases of Axial Spondyloarthritis, increasing health expenditure, and technological advancements along with the availability of many treatment methods. As per Ken Research, this market is projected to grow at a CAGR of ~9.5% in the next five years.
0 notes
Note
Wait holy shit
AS describes exactly the pain I have
oh boy okay as i’ve mentioned i’ve got an extensive document on AS symptoms & mythbusting coming soon but i’ve been wanting to do a quick summary of “wtf is that?” for a while and this is the perfect opportunity! most stats in this post from this 2022 summary article (link) but note that their gender stats are questionable as recent studies show equal prevalence regardless of ‘sex’. so!
wtf is AS?
ankylosing spondylitis is a systemic autoimmune disorder characterized by inflammatory back pain. it’s estimated to be 1.5 times as common as rheumatoid arthritis and over 6 times as common as lupus (SLE) but is incredibly underdiagnosed, which is why i’m super loud about it!
key symptoms of inflammatory back pain:
most frequent onset in early 20s but can be juvenile or later. articles say onset is prior to age 40 but seeing as i’m deeply skeptical of all things medical establishment i wouldn’t rule later onset out
either no history of mechanical trauma or unrelated (for example, i have a herniated disk but had AS symptoms for years before then)
pain gets worse with rest and better with movement - most sources say “exercise” but in the experience of me and other folks with AS i’ve talked to that’s debatable at best. my pain gets worse after remaining in the same position and better with rotating, stretching, etc; sitting upright is most painful for me, but on typical days i need to alternate laying down and standing / walking briefly
morning stiffness and back pain that wakes you up at night
alternating buttock (butt) pain
articles say inflammatory back pain improves with NSAIDs but i’ve never met any chronically ill person whose pain has been made manageable with NSAIDs
AS can also include (usually asymmetrical) joint pain in other locations (especially large joints like the hips, shoulders, neck, and knees - juvenile AS commonly starts with pain in one or both knees prior to spine involvement), fatigue, peripheral neuropathy, and enthesitis (inflammation of tendon insertion points, especially plantar fasciitis).
testing and diagnosis:
CRP and ESR for inflammation. 40-50% of people with AS do not have elevated inflammatory blood markers.
HLA-B27 gene marker. less common in people with non-radiographic AS (doesn’t show up on an x-ray) and more common in white people. only 6-10% of people who are HLA-B27 positive develop AS and plenty (10-30%) of people with AS are negative for HLA-B27 - myself included!
x-ray and MRI for spine inflammation. both of mine were negative; the absence of clinically visible inflammation does not rule out AS. there is a growing body of literature and education about non-radiographic AS; my rheumatologist put me on 20mg prednisone for a week while waiting on my bloodwork and scan results and when that helped my back pain immensely, said “yep it’s definitely inflammatory then” and that this is the standard of diagnosis/care rheumatological associations are advocating for
i wish you the absolute best of luck in finding an explanation and treatment for your pain 💕 if you (or anyone reading this who suspects they have AS!) have any questions feel free to reply, send me an ask, or dm me!
#ankylosing spondylitis#chronic pain#back pain#lower back pain#chronic fatigue#knee problems#knee pain#mac.txt#asks
158 notes
·
View notes
Link
0 notes
Text
The Journey of a Patient with Ankylosing Spondylitis and Crohn's Disease
1. Both Ankylosing Spondylitis and Crohn's Disease are chronic inflammatory diseases that affect the body's immune system.
2. Both conditions can cause abdominal pain, diarrhea, and weight loss.
3. Ankylosing Spondylitis and Crohn's Disease are associated with the HLA-B27 gene, which increases the risk of developing these conditions.
4. Both conditions can cause inflammation in the joints, leading to pain and stiffness.
5. Treatment for Ankylosing Spondylitis and Crohn's Disease may involve the use of anti-inflammat...
Read More.
https://statesandcounties.com/2023/06/22/ankylosing-spondylitis-and-crohns-disease-ankylosing-spondylitis-and-crohns-disease-co-occurrence/?feed_id=5831&_unique_id=649b29b02675f
0 notes
Text
((Just got my blood test to check for HLA-B27.
If it weird I hope the results come back positive?
I mean in one hand positive bad because it means one of my genes is fucky.
But on the other hand I’d finally have an answer to wtf is going on with my chronic back pain and apparently there’s stuff that can be done if this is it. Also it’d be undeniable proof that it’s not all in my head which is something I wonder about at times given literally no other test has shown up anything so what if I’m just imagining it?
If it does come back positive I think I’ll ask if it’s hereditary and a chance other family may have it too and if so I can let relatives know if they wanna get checked.
At the very least if it is positive it’s not something that could kill me. Apparently it just affects the ID markers on cells so some cells will incorrectly display their ID markers and the immune system attacks because of mistaken identity and/or said cells do display correctly but the immune cells incorrectly read the ID markers…))
0 notes
Text

HLA-B27 - Finger painting on canvas, 2023
#art#artists on tumblr#artwork#illustration#creepy art#horror art#horror illustration#chronically ill#illness#finger painting
0 notes