#what is acute inflammation and chronic inflammation
Text
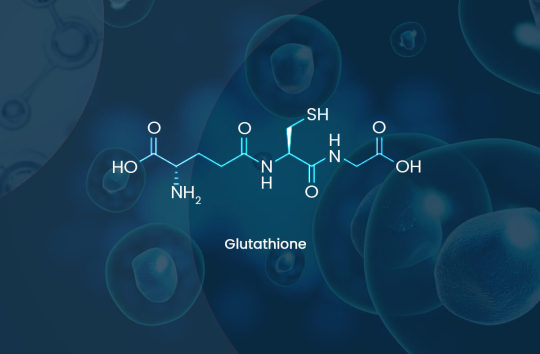
What is Glutathione
Glutathione (GSH) is often termed the “master antioxidant”. This tripeptide is ubiquitous in nature and is produced by every organism from bacteria, to plants to animals that derives energy from oxidative phosphorylation and respiration. Glutathione is synthesized in the cytosol of each cell by the action of two enzymes in an elegantly regulated system that allows it to be maintained at different homeostatic levels in different tissue types, with the liver, given its detoxification role, having the highest amounts. Glutathione plays a pivotal role in most key physiological functions including but not limited to maintenance of cellular redox, neutralising free radicals, cell cycle regulation, proliferation, apoptosis, xenobiotic metabolism, and the recycling of other cellular antioxidants such as Vitamins C and E. Glutathione depletion and a corresponding increase in reactive oxygen species (ROS) during microbial infection is a key driver of the immune response and inflammation. Most chronic diseases are related to oxidative stress arising from the affected tissue losing the capacity to maintain glutathione at adequate healthy levels. The severity of many poisonings from drugs, alcohol, heavy metals and environmental toxins are related to an acute depletion of cellular glutathione. Progressive depletion of cellular glutathione is also used as a mechanism by many viruses to control their replication cycle during infection.
https://www.glutathionereporter.com/what-is-glutathione/
#Glutathione Reporter#Glutathione and it’s importance to Life#The importance of glutathione#importance of glutathione in the body#How do cells produce Glutathione?#gamma-glutamylcysteine#Measuring cellular Glutathione concentration#What is Gamma-Glutamylcysteine#Gamma-Glutamylcysteine (GGC)#GGC supplement#gamma glutamyl cysteine supplement#gamma glutamylcysteine#Gamma Glutamyl Cysteine#glutathione boosting supplements#what is acute inflammation and chronic inflammation#what is acute and chronic inflammation#what is the difference between acute and chronic inflammation
0 notes
Link
#Measuring cellular Glutathione concentration#What is Gamma-Glutamylcysteine#Gamma-Glutamylcysteine (GGC)#gamma glutamylcysteine#Gamma Glutamyl Cysteine#glutathione boosting supplements#what is acute inflammation and chronic inflammation#what is acute and chronic inflammation#what is the difference between acute and chronic inflammation#glutathione and chronic inflammation#chronic glutathione depletion#glutathione & inflammation
0 notes
Text
[3/24] if anyone can help me with even 10ish usd. iv had to use all my medication on medications, and still can't afford my lexapro. after an ER determined that there was inflammation across my entire body, if you've ever seen me before around you'd know iv been experiencing severe physical pain for a long time now. it capsized into something much worse than i anticipated. other doctors are pointing to neuromuscular or neurological. i'm going to need help maintaining my medications and my appointments. i'll be actively updating this post as i get more info on my condition. i will be working as much as i can, trying to get more hours and pushing thru the unspecified acute pain in my lower back and right leg as i'm working to be able to afford a walker. if anyone is dealing with chronic pain that effects your ability to move, and know anything about what mobility tools that could help me move please dm me n let me know.
please, if you can, share and refrain from dono tags. i need a little help.
114 notes
·
View notes
Text
well i actually went to the hospital earlier this week after dealing with chronic diarrhea and acute dizziness for the past couple of months and i ended up staying there for two and a half days! turns out i was borderline dangerously low on blood and had to have four blood transfusions! the reason being is there was microscopic bleeding coming through the diarrhea that i didn't know about! anyways after a chest x-ray, a ct scan, multiple tests, and a colonoscopy, i got diagnosed with ulcerative colitis! and while you'd think that would be something to get overwhelmed and feel downtrodden about, i just can't get over the elation of finally getting a diagnosis! cause it turns out that it's also probably the source of the inflammation that's been causing my chronic pain! not what i was expecting to come out of all this but i'm so fucking happy it's unreal
#ulcerative colitis#chronic pain#chronic fatigue#chronic illness#disabled#inflammatory bowel disease#swift-tricker's posts
65 notes
·
View notes
Note
Hi! I've read somewhere on your blog that icing swellings impedes the healing process - does that mean one shouldn't do that at all if healing speed is prioritized and pain can be managed otherwise? When doctors say to ice a body part after a surgery, is that also for pain management only?
Yes- icing swelling impedes healing. So does the use of NSAIDs and basically the entirety of the "RICE" acronym. You actually want swelling and inflammation (and, honestly, fever- though fever can be a sign of infection, and the infection needs to be treated even though the fever itself really shouldn't be).
But these things work well for pain management, so med pros keep recommending them.
Part of this is that all pain management has side effects. THe mainstays of pain management include the following:
We have acetaminophen but it's not really that strong and even slightly too much of it causes liver damage. We have RICE which is moderately effective but prolongs healing time. We have NSAIDs (including prescription ones much stronger than ibuprofen) which can be very effective but they prolong healing time and taking them for too long causes kidney damage. We also have opioids which are effective in the short term but most doctors haven't found a way of prescribing them that avoids the moderate-high risks of death from respiratory depression and addiction.
That being said, people still need pain management. And while we do have some other modalities for chronic pain, acute pain is pretty much a remix of the above.
So what do we as med pros do? We continue to recommend acetaminophen, RICE and NSAIDS because they spread out the side effects and allow a lower dose of opioids.
69 notes
·
View notes
Text
Vaccines that protect against severe illness, death and lingering long Covid-19 symptoms from a coronavirus infection were linked to small increases in neurological, blood, and heart-related conditions in the largest global vaccine safety study to date.
The rare events – identified early in the pandemic – included a higher risk of heart-related inflammation from mRNA shots made by Pfizer Inc, BioNTech SE, and Moderna Inc, and an increased risk of a type of blood clot in the brain after immunisation with viral-vector vaccines such as the one developed by the University of Oxford and made by AstraZeneca Plc.
The viral-vector jabs were also tied to an increased risk of Guillain-Barre syndrome, a neurological disorder in which the immune system mistakenly attacks the peripheral nervous system.
More than 13.5 billion doses of Covid vaccines have been administered globally over the past three years, saving over 1 million lives in Europe alone. Still, a small proportion of people immunised were injured by the shots, stoking debate about their benefits versus harms.
The new research, by the Global Vaccine Data Network, was published in the journal Vaccine last week.
The research looked for 13 medical conditions that the group considered “adverse events of special interest” among 99 million vaccinated individuals in eight countries, aiming to identify higher-than-expected cases after a Covid shot.
Myocarditis, or inflammation of the heart muscle, was consistently identified following a first, second and third dose of mRNA vaccines, the study found.
The highest increase in the observed-to-expected ratio was seen after a second jab with the Moderna shot. A first and fourth dose of the same vaccine was also tied to an increase in pericarditis, or inflammation of the thin sac covering the heart.
Researchers found a statistically significant increase in cases of Guillain-Barre syndrome within 42 days of an initial Oxford-developed ChAdOx1 or “Vaxzevria” shot that wasn’t observed with mRNA vaccines.
Based on the background incidence of the condition, 66 cases were expected – but 190 events were observed.
ChAdOx1 was linked to a threefold increase in cerebral venous sinus thrombosis, a type of blood clot in the brain, identified in 69 events, compared with an expected 21.
The small risk led to the vaccine’s withdrawal or restriction in Denmark and multiple other countries. Myocarditis was also linked to a third dose of ChAdOx1 in some, but not all, populations studied.
Possible safety signals for transverse myelitis – spinal cord inflammation – after viral-vector vaccines was identified in the study.
So was acute disseminated encephalomyelitis – inflammation and swelling in the brain and spinal cord – after both viral-vector and mRNA vaccines.
Seven cases of acute disseminated encephalomyelitis after vaccination with the Pfizer-BioNTech vaccine were observed, versus an expectation of two.
The adverse events of special interest were selected based on pre-established associations with immunisation, what was already known about immune-related conditions and preclinical research. The study didn’t monitor for postural orthostatic tachycardia syndrome, or POTS, that some research has linked with Covid vaccines.
Exercise intolerance, excessive fatigue, numbness and “brain fog” were among common symptoms identified in more than 240 adults experiencing chronic post-vaccination syndrome in a separate study conducted by the Yale School of Medicine. The cause of the syndrome isn’t yet known, and it has no diagnostic tests or proven remedies.
The Yale research aims to understand the condition to relieve the suffering of those affected and improve the safety of vaccines, said Harlan Krumholz, a principal investigator of the study, and director of the Yale New Haven Hospital Centre for Outcomes Research and Evaluation.
“Both things can be true,” Krumholz said in an interview. “They can save millions of lives, and there can be a small number of people who’ve been adversely affected.”
31 notes
·
View notes
Note
Okay but given Beach Vacay's glorious fit and accessories, what and how do chimeras smoke?
They smoke Marshmallow! Both in leaf and root form. It's not for any real buzz, but it's more of a way to soothe the lungs in cold/dry places. Outside of Mirum's hot and humid climate traditional chimera kind of struggle with some chronic respiratory discomfort. Chimera lungs are not fleshy expanding sacks like ours, but more so rows of bone arches within an inflexible air filled cavity. So any inflammation or swelling is acutely dangerous to them. Smoking was first started to soothe the lungs, but most mainly enjoy it for recreation with a few additional plants to get a true high going. Never Sleep is a favorite!

And as opposed to flavoring smoke like us, they color it instead! If you're extra fancy you can pack your pipe to burn through different colors as you smoke. Hella fancy.
Also since they have two distinct respiratory tracts, most chimera will have a favored side to smoke through. They inhale through placing the 'mouth piece' or well I guess nose piece? Into one nostril, which closes shut around it, and then inflating their bellows as normal. So they suck air in through the pipe. Smoke ALWAYS comes out of the trunk on the same side as they inhaled from.
#basically marshmallow is their tobacco#good ask!#made me do a LOT of googling#chimera#art#no true north#mirum
86 notes
·
View notes
Text
homegrown health literacy part 1.2: WTF is CRP?
hello and welcome back to my series about knowing when your doctors are full of shit! part 1 is about interpreting bloodwork results.
disclaimer: i’m Just Some Guy
CRP is a blood test that measures inflammation. it’s a general test, so it can’t say what chronic or acute condition is causing the inflammation, just that it’s there.
CRP stands for C-reactive protein, a type of protein in your blood. the amount of protein increases during (chronic or acute) inflammation, so a higher CRP indicates more inflammation. this could indicate an infection or an autoimmune disease, but CRP is also elevated during pregnancy. the average CRP for US Americans is estimated to be somewhere between 1 and 2 mg/L.
note: i use the units mg/L throughout this post, which is how CRP results are reported by Labcorp and Quest. some other providers report results in mg/dL, which would change the “normal” range by a factor of 10 (i.e., 0-1.0 rather than 0-10).
when used for cardiac disease screening, CRP results are interpreted as follows:
0-1 lower risk
1-3 average risk
3+ higher risk
a CRP greater than around 5 or 6 may indicate an underlying inflammatory condition. this should generally be followed by repeating the test about a month later, then conducting further screening if the result is still elevated.
while the reference range for CRP is often listed as 0-10 mg/L, meaning a lab report may not flag your result as abnormal unless it’s higher than 10, values lower than 10 can still indicate active autoimmune disease. my CRP was used in diagnosing me with ankylosing spondylitis when it was 8.0, and a range of values above 7 were consistently considered indicative of active disease.
additionally, a lower CRP should not be used to rule out autoimmune disease; as always, there is no one blood test and your doctor should consider the full clinical picture, particularly your symptoms, not just the test results. it’s relatively common to rerun ESR and CRP tests about 3 months later if they didn’t originally indicate inflammation but your symptoms still indicate you might have an autoimmune disease.
#crp#c reactive protein#bloodwork#chronic pain#chronic illness#spoonie#mac.txt#homegrown health literacy
58 notes
·
View notes
Text
Long Covid may be the body trying to fight off other viruses (Sarah Knapton, The Telegraph, April 08 2024)
"Dr Felicity Liew, from Imperial’s National Heart & Lung Institute, said:
“Even though the acute phase of illness resolves, there may be virus persisting in the body that could continually trigger the immune system and cause the ongoing inflammation that we found.
“It can also cause reactivation of herpes viruses or people that previously had glandular fever caused by Epstein-Barr virus, and it can cause that to reactivate and cause ongoing symptoms.
“Or it can result in autoimmunity, and all of those scenarios result in the types of inflammation that we see, and could result in chronic and ongoing abnormal inflammation represented by these proteins highlighted here.”
There are eight herpes viruses that routinely infect humans, and which lie dormant in the body.
Around 70 per cent of people in Britain carry the Herpes Simplex type 1 (HS1) virus, which causes cold sores, while 10 per cent have HS2, which can cause genital warts and is linked to cervical cancer.
Similarly, around nine in 10 people carry Epstein-Barr – also a type of herpes – which mostly causes no problems, but can sometimes lead to glandular fever, encephalitis, meningitis and trigger auto-immunity.
Usually dormant viruses are kept at bay by the immune system, but experts think Covid-19 requires so much attention that it may allow other viruses through the defensive cracks. (…)
Researchers believe long Covid may be similar, or the same, as post-viral syndrome which leads to people experiencing fatigue and brain fog after influenza and other viruses, and may be to blame for conditions such as ME/CFS.
The team say the sheer number of people suffering ongoing symptoms after Covid gives the opportunity to get to the bottom of what is causing these after-viral effects, and could lead to help for other long-term conditions."
9 notes
·
View notes
Text
Is Twilight really okay?
So I see tons of folks bring up how they are feeling sus out by if twilight is truly okay
No. He’s not okay, yet.
Warning: discussion of illnesses and injuries.
I get why folks are quick to be Sus of how twilight is. I will sort of explain this the best way I can. Using my own personal experience of what going okay. But note I am not invalidating anyone feelings on their thoughts of twilight and his finally seeming to be recovered.
I can say, I think he was given as much healing as they can provide him. He is not fully 100%. He probably got enough healing he can get. Over time it will heal more. However he is most likely poisoned by dink’s blade. But his wound will never truly heal. He will suffer from it till he last days. Something a lot like what Happened to Frodo in the Fellowship of the Ring. In the end Frodo does die once their task was completed and evil was banished from the land. I suspect this how it will got for Twilight.
More on a personal level, I suffer from chronic pancreatitis*. So I sympathize with how Twilight must be feeling. The aches and pains are unimaginable. However I kept going. Weakness can be strengthened slowly at my own pace. Which what he will have to do. You don’t just drink a potion, get heal with a life spell and can be spring chicken. It takes time. As we can see. There will be a struggle and frustration at every corner cause you want to not be a burden to anyone and be able to function the way you use too. The trauma of it will over time heal as well. He will have to relearn to do things. He won’t be able to fight the way he has done. Rest and recovery is a must. Not pushing too hard. Twilight and Time being related- they both share a stubbornness. So emotionally he will lash out a bit (or not). So I sort of get how Twilight must and will feel.
I know people are quick to be like “angst, angst, angst.” But I think people don’t understand there’s something much deeper to a wound that won’t fully heal, but heals enough. It will be a chronic thing for him. Could he maybe get turned into a puppet for dink and turn on the chain. Maybe, but let’s be more logical and see it as he just won’t be fully healed. However he will continue to fight till their adventure ends and dink is defeated properly. So you are all valid in not trusting him being okay. It just may not be how angsty as you think. Just simply he will never be 100% and that now his struggle will be to learn to handle is medical situation and work around what he can and can not do any longer.
He will still be a down tight magnificent fighter, good hearted gent he is. How just now in a new phase in his situation where he will have to come to terms with his limitations. Which mentally is often hard to come to terms with. For me, I can’t eat a lot of my favorite stuff and knowing when I need to take it easy. Something along those lines. It’s an emotional, physical and mental journey. Which we will be watching as the comic progresses.
That’s my take on how he is and what we will expect as the comic progresses. More then welcome to disagree and think more into things. This just my own view of where things may go.
[* Chronic pancreatitis is similar to acute, but in this case, the inflammation is long-term and won’t get any better. In fact, over time, it tends to get worse and lead to permanent damage.
Chronic pancreatitis will often develop after an episode of acute pancreatitis has already occurred.
]
#linked universe#linkeduniverse#lu twilight#I Hope using my own medical situation#or invalidate how they think#cause I could be wrong#we shall see#doesn’t rub others the wrong way
55 notes
·
View notes
Link
#gamma glutamyl cysteine supplement#gamma glutamylcysteine#Gamma Glutamyl Cysteine#glutathione boosting supplements#what is acute inflammation and chronic inflammation#what is the difference between acute and chronic inflammation#glutathione and chronic inflammation#chronic glutathione depletion#glutathione & inflammation#glutathione and the immune system#Glutathione and Homeostasis#Glutathione Homeostasis#Glutathione and the human body
0 notes
Text
I wasn't sure if I was going to make a post about this, but this is something I feel like I need to do, especially for those who know and care about me (I know, people care on here? That's crazy.). I'm definitely going to struggle typing this all out, but...here it goes.
_____
So over the past month (and quite possibly earlier), Mom has been dealing some abdominal pain that radiates to her back. The pain would be so bad that it would cause her to throw up at times. She barely ate and slept while this was going on. On January 6th, things finally came to a head and we made the call to take her to the hospital.
When she first came in, she was diagnosed as suffering from pancreatitis (for those who don't know, it's inflammation of the pancreas that, if left untreated, can cause a high amount of pain and nausea to the person. There's two types of pancreatitis: acute, which is very treatable and will go away after a while, and chronic, which will last a lot longer and hurt more). They were able to treat her and she felt better for a while, discharging her after 3 days. When they released her, they wanted her to get a endoscopy test done up at a hospital in Royal Oak. With neither Mom or I having a car, this was difficult for us to do. But we would come to know why soon enough.
Mom came home and for a day or two, she seemed fine. She ate well and was able to sleep soundly, which I thought was the important thing. But the pain and nausea eventually came back with a vengeance We tried every the hospital doctors had told us: heating pads, soft to liquid diet, pain patches. Nothing was working. Her primary care doctor even had her go on some antibiotics and a stronger pain med than she had, but nothing seemed to help matters. We took her back to the hospital this past Saturday, January 20th.
When we initially got there, after they had done a CT scan on Mom, they said that the pancreatitis was gone. But what was left was a mass on her pancreas. Scared and unsure as to what it may be, they admitted her and has been in the hospital since. On Tuesday, they took her to the University of Toledo Medical Center for the endoscopy and see what the mass might be. They did the scope and drew fluid from the mass for testing.
On Wednesday, we get the news that it is cancer. More precisely, metastatic pancreatic adenocarcinoma. In layman's terms, it's Stage IV pancreatic cancer, not curable.
I could not believe it...
We don't really know how long she may have left, but the rough and harsh estimate is less than 6 months...
Needless to say, I broke down, not in front of Mom or my brothers (who have been with Mom and I throughout this whole thing).
I can't imagine being here on Earth without Mom and I'm somehow going to have to figure out how to...I panicked and wanted to run away...a moment of weakness...
I don't know what will happen between now and the inevitable day, but we all agreed that we're going to try and make the most out of the days she does have left. I know that there will be bad days ahead, and there'll be good days as well.
But it's tough, knowing that the last few years I've been taking care of her (and complaining about her behavior, which is making me feel guilty about, now that this is happening) and it's going to come to an end.
_____
I know this isn't the greatest of things to post on here, but I needed some therapeutic way to get some of the emotions I am feeling right now out and to inform you all of what has been going on. I thank you all for the thoughts and positive vibes before and coming in the future. It's going to be a rough time ahead and I hope you will all bear with me in the meantime.
I love you all.
6 notes
·
View notes
Text
I teach patho to nursing students. Every semester since spring of 2020, I have taught about Covid. And every semester to have to change my lecture to keep up with new data. I was teaching Covid this semester and I told them that if nothing else, understand the science.
I explained how Covid attaches to ACE2 receptors in the nose, throat, heart, kidneys, and gut first. That’s why you see a runny nose, sore throat, myocarditis and acute kidney failure first. There aren’t as many ACE 2 receptors in the lungs, so Covid hits the lungs later.
That’s why you see lag time between initial infection and respiratory symptoms. More importantly, I explained that Covid is not just a lung disease, it is a massive systemic inflammatory response to the virus. Covid also upregulates a protein called bradykinin, causing clots.
If nothing else, I told them to think of Covid as huge inflammatory process that causes injury, scarring and clots to form everywhere. That’s why we are seeing so many strokes, MIs, weird liver failure in peds, bowel ischemia, and long Covid.
It all points to chronic inflammation. There is no immunity as the variants keep changing, kind of like the flu, which is why we get flu shots every year. We’ve just let this run rampant, so a slew of Covid variants keep popping up, rendering treatments less effective.
The worst part of this was when one student said that their parents had gotten Covid and asked how to keep them safe from the complications. Another student piped in and said she had Covid 3 times and was she at risk too? It was my moment of reckoning.
I realized that there wasn’t much I could say except to protect themselves with masks, vaccinations, and to try not to get Covid again. I told them that if they had Covid, they were at higher risk of long Covid and lantern complications. There was nothing to be done.
Except to protect themselves going forward. After that there was silence. One of my students then said how disappointed in government and public health leaders he was. Another told me she was disappointed in her professors and her school for not being more vigilant.
I told them that as long as they understood the patho of the disease, they could guard against misinformation. I told them to educate their families and patients about the science, not the rumors. This left me feeling so sad. What have we done?
If I can teach this to first semester nursing students, why couldn’t we have taught this to everyone? People do not understand the disease and no one bothers to explain it. Perhaps that’s why we have failed so miserably.
We need to backtrack and explain the disease before we start talking about immunity debt (a non issue) and endemicity. My students are so young. It’s heartbreaking.
via Kali
54 notes
·
View notes
Text
Title: Hypermobility, the Ehlers-Danlos syndromes and chronic pain
Date: September 2017
Published in: Clinical and Experimental Rheumatology
Publicly available? Yes (pdf will download)
Citation: Syx, D., De Wandele, I., Rombaut, L., & Malfait, F. (2017). Hypermobility, the ehlers-danlos syndromes
and chronic pain. Clin Exp Rheumatol, 35 (5), 116–122.
Abbreviations:
ECM: extracellular matrix
EDS: Ehlers-Danlos syndrome (lowercase letters in front indicate the subtype; e.g., hypermobile EDS = hEDS)
GJH: generalised joint hypermobility
HSD: hypermobility spectrum disorder
JH: joint hypermobility
JHS: joint hypermobility syndrome
MSK: musculoskeletal
Article Summary
Abstract
Hypermobility, joint hypermobility syndrome, and Ehlers-Danlos syndromes
Joint hypermobility (JH) is a range of movement in a joint that exceeds what is normal (accounting for the age, gender, and ethnicity). JH can be localised or generalised with GJH being defined by a score of at least 5 on the Beighton scale.
JH has a strong genetic basis and is affected by gender, age, and ethnicity but can also be affected by environmental factors including weight, training, trauma, surgery, and medical conditions.
JH does not necessarily lead to symptoms and is not a disease or permanent diagnosis
The history and historical classifications related to GJH are detailed and the overlap with connective tissue disorders including Marfan syndrome, osteogenesis imperfecta, and notably Ehlers-Danlos syndromes (EDS)
EDS is a group of disorders that mainly affect the soft connective tissues but that are varied in their genetic and phenotypic (observable characteristics) presentations. Major characteristics include skin hyperextensibility and fragility; vascular fragility with easy bruisability and a variable bleeding tendency; joint hypermobility (usually generalised) and manifestations of generalised connective tissue fragility. The severity of symptoms can be varied.
There are now 13 EDS subtypes (expanded from the 6 originally identified in 1997) with molecular defects identified in 19 different genes. The effects are briefly discussed and Table III details these defects.
One of the most prevalent subtypes of EDS, hypermobile EDS (hEDS), is still molecularly unexplained. hEDS shows considerable overlap with JHS and it has been considered that they may be the same and/or can be used interchangeably. Hypermobility syndrome and JHS have therefore been combined into the single HSD diagnosis to be used for patients with symptomatic JH who do not meet the new criteria for hEDS or another form of EDS. This review uses JHS instead of HSD as it is a review of old literature (consider them interchangeable).
The natural history of pain in JHS and EDS
The compromised structural integrity of connective tissues, people with EDS and JHS are prone to joint instability, and as a result, joint disclocations (full displacements and subluxations), and articular and soft tissue injuries. This commonly causes acute and reccurent pain which can evolve to chronic widespread musculoskeletal (MSK) pain.
Approximately 3.3% of women and 0.6% of men experience chronic pain but these numbers are likely an underestimation since clinicians are generally unaware of GJH-related pain. More recent studies have found incidences of chronic pain over 90% in hEDS patients -- higher than that in cEDS. Clinicians report that pain is the primary reason fro seeking medical help and the most frequent complaint but more studies are needed.
Most studies focus on hEDS and many do not distinguish between hEDS and JHS.
Pain usually starts in early life and is often triggered by an apparent external factor such as an injury, surgery, psychological distress, or by a comorbidity. The pain is initially felt as an acute and localised symptom or as 'growing pains' related to the trauma. Muscle cramps, pariarticular inflammation, enthesopathies, and nerve entrapment syndromes can add to the localised MSK pain.
The pain later becomes widespread, most commonly presenting as arthralgias and myalgias (joint and muscle pains) in young adult and adult patients. The pain is most frequently localised in the neck, shoulders, forearms, fingers, hips, knees, and feet and may, at first, be localised to a few joints or muscles with a migratory pattern. The pain will gradually become more widespread and additional symptoms including burning sensations, peripheral paresthesias, generalised hyperalgesia, allodynia, and hypersensitivity to various stimuli (e.g., light, sound, and odors) become apparent. Pain in non-articular regions (e.g., headaches, gastro-intestinal, pelvic) as well as fatigue often appear. The underlying cause of the fatigue is unclear.
The pain is generally resistant to the use of analgesics (painkillers), surgery, and physical therapy. This can have a negative effect on physical, social, and emotional wellbeing.
The pathogenesis of pain in hypermobility and EDS
The underlying causes and mechanisms of pain in JHS and EDS are poorly understood.
Pain caused by an injury or damage (nociceptive pain) is often present, especially in early stages and neuropathic pain may also contribute to the pain (and account for parasthesias) and be exacerbated by dislocations and subluxations. Central sensitisation may also contribute to the pain becoming chronic.
It has been proposed that lack of proprioceptive acuity (ability to sense joint position and movement) and muscle weakness play a role in generating chronic pain. The fear of pain is common in people with JHS and hEDS and can cause deconditioning and exercise intolerance which leads to a cycle.
It is hypothesised that abnormalities in the extracellular matrix (ECM) can contribute to the generation and chronification of pain. The ECM has a clear role in the general detection of noxious stimuli (nociception) and painful injuries have been shown to alter the the ECM at acute and chronic time points after the injury. The ECM also has a role in neuroplasticity and connectivity of the central nervous system.
Patients with EDS have defects in different components of the ECM which can lead to a devastating impact on the nervous system. Defective connective tissue can also inhibits the body's ability to react protectively to stretching or pressure of peripheral nerves.
The abnormal ECM may contribute to the central sensitisation that causes the chronification of pain.
The complex nature of pain in JHS and EDS patients, fragmented understanding of the underlying mechanisms, and lack of reported effectiveness of treatments highlight the fact that the management of pain in JHS and EDS patients.
Management requires pharmacological and psychological therapy.
Conclusion
#summary#medical#chronic pain#ehlers danlos syndrome#eds#hypermobile ehlers danlos syndrome#heds#hypermobility spectrum disorder#hsd#hypermobility syndrome#hms#joint hypermobility syndrome#jhs#clinical and experimental rheumatology#generalised joint hypermobility#gjh
2 notes
·
View notes
Text
Deepak Chopra says inflammation is ‘the number one pandemic of our times.’ He suggests these 5 habits to help reduce it
My mom emailed me this and said "I'm not a big Deepak Chopra fan, but the idea that runaway inflammation is the root cause of most ailments has been my theory for decades.......get proper sleep, hydrate, eat well, don't overthink - and check in please! xo"
From the article:
When the body’s immune system is alerted to anything foreign, like pollen or microbes, it triggers an inflammatory response. Acute inflammation protects the body and helps it heal. However, when inflammation persists, and becomes what’s known as chronic inflammation, serious health consequences can follow.
“Stress, inflammation, depression, anxiety, and chronic disease go together,” Chopra said. “Inflammation is the culprit in all these diseases.”
Constant stress can put the body in a state of chronic inflammation, which increases the risk for mental health problems like anxiety and depression along with heart disease and Alzheimer’s, according to the Cleveland Clinic.
“The reason for that is trauma. Anyone who's had trauma is likely to be inflamed,” Chopra said. The rise in mental health problems and chronic stress is related to the body’s response to trauma, which can stem from generational trauma, isolation, or the stress of the news cycle, Chopra explained.
5 notes
·
View notes
Text
"How to Combat Inflammaging, the Aging Side Effect No One Talks About"
Article Date: April 7, 2024.
Article Excerpt:
It may sound like a made-up word, but “inflammaging” is a medical term coined more than 20 years ago to describe the chronic inflammation that happens in our bodies as we get older. “It’s a word that combines ‘aging’ and ‘inflammation’ to describe a low-level inflammatory process,” says Linda Herrmann, Ph.D., a clinical associate professor and aging expert in the Division of Advanced Nursing Practice at Rutgers, the State University of New Jersey. “It’s systemic throughout the body, but occurs in the absence of an acute illness or injury.”
[...]
It turns out that inflammaging is a risk factor for cardiovascular diseases, kidney disease, diabetes, cancer, depression and dementia. “The rise in rates of these conditions are the by-products of a longer life span,” says Nicole Ehrhart, V.M.D.,
[...]
Potential triggers may include genetic susceptibility, obesity, changes in the microbiome and chronic infections.
Another cause seems to be cellular senescence, which is when cells stop replicating, but they don’t die. “Instead, they go into a sort of ‘undead’ state, secreting inflammatory factors and inducing neighbor cells to do the same,” says Ehrhart. [...]
“as we age, our immune system gets less specific to what it’s reacting to. After a while, this cumulative sort of chronic response actually becomes this low-grade chronic inflammation,” says Ehrhart. “It doesn’t’ function like it used to when we were younger.” The result is inflammaging. [...]
How can you prevent inflammaging? [...]
Get moving
Work on your balance
"Eat right"
Manage stress
Spend quality time with others
Get good sleep
[Note: more information in article, take with a bit of skepticism - "a grain of salt"]
#am getting sense that there really isn't much that's known about it to have such vague broad advice n blaming obesity (vague)#text post#o post#magz upload
6 notes
·
View notes