#Schizophrenia is an illness
Text
Given the (warranted) suspicion given towards the disease denialism found in both Christian Science and Scientology, it can be said that if the claims of the neurodiversity movement were attached to organized religion, they too would be constantly lambasted.
#Christian Science#scientology#church of Christ scientist#Mary Baker Eddy#l ron hubbard#church of scientology#neurodiversity#neurodiversity movement#Just because a movement does not claim to be religious does not mean it isn’t cultic.#Scientific denialism#Denialism#autism is an illness#ADHD is an illness#Dyslexia is an illness#Down syndrome is an illness#Schizophrenia is an illness#Not all victims of a given illness will have an equally easy or difficult time#Not all illnesses have viral or environmental postnatal causes#I know most of the conditions the ND crowd champions are inborn#That still doesn’t mean they aren’t illnesses
24 notes
·
View notes
Text
Things I'd love for the Internet to leave in 2023:
• misusing the word "delusional" or saying "delulu"
• public freakout videos that are just someone displaying psychotic symptoms
• "I'm in your walls" and other paranoia triggering "jokes"
• schizoposting
• misusing the word "psychotic"
• baiting and triggering people online who are openly psychotic or displaying psychotic symptoms
• excluding schizo-spec and psychotic people from any neurodiversity/mental illness awareness
Let's just all try to be better to schizo-spec and psychotic people. And hold others accountable as well.
#2024#new years eve#tw im in your walls#tw paranoia#mental illness#nd#schizophrenia#neurodivergent#schizophrenic#psychosis#actuallyschizophrenic#mental health awareness#pseriouslypsychotic#schizo-spec
27K notes
·
View notes
Text
it's never too late to start brushing your teeth again. i basically never brushed my teeth for a whole 10 years. a decade. A DECADE. i still struggle to brush my teeth once a week, but it all started with brushing my teeth once every few months. so i mean it when i say brushing your teeth once a week, a month, a year, or even a decade, is better than nothing.
and still, nothing is not shameful. it is not immoral to struggle with self care. and it is also not pointless to keep trying. anything you can do, even if its wiping plaque off with a towel, is enough. it is good to take care of yourself however you can, even if it's just trying to muster the will to. reading this post is good, too.
i believe in you and i am proud of you, even in the smallest of steps. it's okay. you can give yourself grace.
#softspoonie#disabled#disability#schizophrenic#schizophrenia#schizoaffective#depression#depressed#severe depression#self care#hygiene#self love#self help#mentally ill#mental health#physical health#chronic illness#chronically ill#mental illness#mental health support#spoonie#spoonie positivity#disability positivity#neurodivergent#adhd#neurodivergent positivity#disabled positivity
24K notes
·
View notes
Text
poor memory is a huge deal and i wish people wouldn't diminish it by saying "oh yeah i can't remember what i had for breakfast lol."
i can't remember the first 10 years of my life. i can't remember entire days, weeks, months at a time. i can't remember entire people, i can't remember names or faces. i can't remember when things are scheduled for, my calendar app on my phone is booked to the max with reminders and task checklists. i can't remember when i moved into what home when, i can't remember important milestone dates like when i got or lost certain jobs, or when i started a new hobby.
that's what i mean when i say i have poor memory. poor memory is so scary for the person who has it. it's not a quirky thing, everyone forgets small details. memory problems are scary because you can go through entire events or days with no memory, or plan for things in the future that you can't recall ever even looking into or scheduling. it's not a funny haha kind of thing, it's serious, and it affects a lot of people in very unavoidable ways.
not being able to plan for appointments or work schedules, not being able to remember people's names or faces, not being able to recall whether or not you were present for something or whether or not you met someone, not being able to keep track of what's happening on what dates and losing track of items because you can't remember where you put them are all very real problems, and anyone dealing with them deserves to be taken seriously, and not diminished when they choose to speak up about it.
#neurodivergence#mental health#adhd#did#ptsd#mental illness#schizophrenia#ocd#anxiety#generalized anxiety disorder#depression#bipolar disorder#bpd#borderline personality disorder#neurodivergent#autism#mental health awareness#dpdr#osdd#dissociative disorders#dissociative#depersonalization derealization#other specified dissociative disorder#memory problems#poor memory#learning disorders#chronic fatigue#neurological disability#neurological disorders#traumatic brain injury
7K notes
·
View notes
Text
If you advocate for mental health awareness, but joke about things like intrusive thoughts and schizophrenia, think it’s disgusting and lazy when people who are depressed can’t do things like showering or cleaning their room, use terms like “narcissistic abuse”, and believe that having ASPD, BPD, or NPD makes someone a bad person, you are not a mental health advocate. You don’t actually care about helping people or de-stigmatizing mental illness, you just want to make yourself feel like you do. You can’t pick and choose what disorders and symptoms are acceptable, and which ones make someone a bad person. Either you support everyone, or you support no one.
and if you’re neurodivergent/mentally ill and you do any of those things, you are part of the problem. there’s no such thing as “good/moral” disorders, or “bad/immoral” disorders. We all need to have each other’s backs.
#mental health#mental illness#tw abelism#npd safe#bpd#npd#aspd safe#aspd#ocd#schizophrenia#cluster b#neurodivergent
4K notes
·
View notes
Text

my anhedonia is eating me alive so i’m making these mental illness memes to cope
#actually aspd#actually npd#aspd#npd#clusterb#actually mentally ill#actually bpd#actuallyaspd#actuallynpd#cluster b#bpd#actuallybpd#actually schizophrenic#actually delusional#actually borderline#actually obsessive#actually autistic#actually antisocial#actually narcissistic#schizophrenia#schizospec#psychotic spectrum#did#osdd#ocd#actually pocd#mental illness#cluster b personality disorder#cluster b memes#npd meme
2K notes
·
View notes
Text
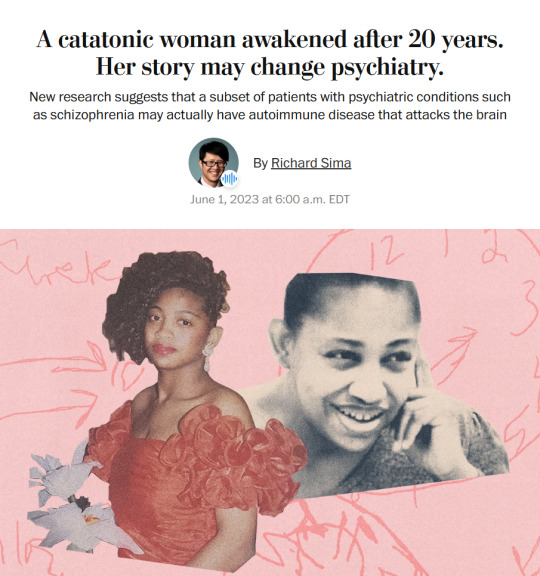
Story from the Washington Post here, non-paywall version here.
Washington Post stop blocking linksharing and shit challenge.
"The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.” ...
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries...
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments [for lupus] — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other people with similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients, the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.” ...
Waking up after two decades
The medical team set to work counteracting April’s rampaging immune system and started April on an intensive immunotherapy treatment for neuropsychiatric lupus...
The regimen is grueling, requiring a month-long break between each of the six rounds to allow the immune system to recover. But April started showing signs of improvement almost immediately...
A joyful reunion
“I’ve always wanted my sister to get back to who she was,” Guy Burrell said.
In 2020, April was deemed mentally competent to discharge herself from the psychiatric hospital where she had lived for nearly two decades, and she moved to a rehabilitation center...
Because of visiting restrictions related to covid, the family’s face-to-face reunion with April was delayed until last year. April’s brother, sister-in-law and their kids were finally able to visit her at a rehabilitation center, and the occasion was tearful and joyous.
“When she came in there, you would’ve thought she was a brand-new person,” Guy Burrell said. “She knew all of us, remembered different stuff from back when she was a child.” ...
The family felt as if they’d witnessed a miracle.
“She was hugging me, she was holding my hand,” Guy Burrell said. “You might as well have thrown a parade because we were so happy, because we hadn’t seen her like that in, like, forever.”
“It was like she came home,” Markx said. “We never thought that was possible.”
...After April’s unexpected recovery, the medical team put out an alert to the hospital system to identify any patients with antibody markers for autoimmune disease. A few months later, Anca Askanase, a rheumatologist and director of the Columbia Lupus Center,who had been on April’s treatment team, approached Markx. “I think we found our girl,” she said.
Bringing back Devine
When Devine Cruz was 9, she began to hear voices. At first, the voices fought with one another. But as she grew older, the voices would talk about her, [and over the years, things got worse].
For more than a decade, the young woman moved in and out of hospitals for treatment. Her symptoms included visual and auditory hallucinations, as well as delusions that prevented her from living a normal life.
Devine was eventually diagnosed with schizoaffective disorder, which can result in symptoms of both schizophrenia and bipolar disorder. She also was diagnosed with intellectual disability.
She was on a laundry list of drugs — two antipsychotic medications, lithium, clonazepam, Ativan and benztropine — that came with a litany of side effects but didn’t resolve all her symptoms...
She also had lupus, which she had been diagnosed with when she was about 14, although doctors had never made a connection between the disease and her mental health...
Last August, the medical team prescribed monthly immunosuppressive infusions of corticosteroids and chemotherapy drugs, a regime similar to what April had been given a few years prior. By October, there were already dramatic signs of improvement.
“She was like ‘Yeah, I gotta go,’” Markx said. “‘Like, I’ve been missing out.’”
After several treatments, Devine began developing awareness that the voices in her head were different from real voices, a sign that she was reconnecting with reality. She finished her sixth and final round of infusions in January.
In March, she was well enough to meet with a reporter. “I feel like I’m already better,” Devine said during a conversation in Markx’s office at the New York State Psychiatric Institute, where she was treated. “I feel myself being a person that I was supposed to be my whole entire life.” ...
Her recovery is remarkable for several reasons, her doctors said. The voices and visions have stopped. And she no longer meets the diagnostic criteria for either schizoaffective disorder or intellectual disability, Markx said...
Today, Devine lives with her mother and is leading a more active and engaged life. She helps her mother cook, goes to the grocery store and navigates public transportation to keep her appointments. She is even babysitting her siblings’ young children — listening to music, taking them to the park or watching “Frozen 2” — responsibilities her family never would have entrusted her with before her recovery.
Expanding the search for more patients
While it is likely that only a subset of people diagnosed with schizophrenia and psychotic disorders have an underlying autoimmune condition, Markx and other doctors believe there are probably many more patients whose psychiatric conditions are caused or exacerbated by autoimmune issues...
The cases of April and Devine also helped inspire the development of the SNF Center for Precision Psychiatry and Mental Health at Columbia, which was named for the Stavros Niarchos Foundation, which awarded it a $75 million grant in April. The goal of the center is to develop new treatments based on specific genetic and autoimmune causes of psychiatric illness, said Joseph Gogos, co-director of the SNF Center.
Markx said he has begun care and treatment on about 40 patients since the SNF Center opened. The SNF Center is working with the New York State Office of Mental Health, which oversees one of the largest public mental health systems in America, to conduct whole genome sequencing and autoimmunity screening on inpatients at long-term facilities.
For “the most disabled, the sickest of the sick, even if we can help just a small fraction of them, by doing these detailed analyses, that’s worth something,” said Thomas Smith, chief medical officer for the New York State Office of Mental Health. “You’re helping save someone’s life, get them out of the hospital, have them live in the community, go home.”
Discussions are underway to extend the search to the 20,000 outpatients in the New York state system as well. Serious psychiatric disorders, like schizophrenia, are more likely to be undertreated in underprivileged groups. And autoimmune disorders like lupus disproportionately affect women and people of color with more severity.
Changing psychiatric care
How many people ultimately will be helped by the research remains a subject of debate in the scientific community. But the research has spurred excitement about the potential to better understand what is going on in the brain during serious mental illness...
Emerging research has implicated inflammation and immunological dysfunction as potential players in a variety of neuropsychiatric conditions, including schizophrenia, depression and autism.
“It opens new treatment possibilities to patients that used to be treated very differently,” said Ludger Tebartz van Elst, a professor of psychiatry and psychotherapy at University Medical Clinic Freiburg in Germany.
In one study, published last year in Molecular Psychiatry, Tebartz van Elst and his colleagues identified 91 psychiatric patients with suspected autoimmune diseases, and reported that immunotherapies benefited the majority of them.
Belinda Lennox, head of the psychiatry department at the University of Oxford, is enrolling patients in clinical trials to test the effectiveness of immunotherapy for autoimmune psychosis patients.
As a result of the research, screenings for immunological markers in psychotic patients are already routine in Germany, where psychiatrists regularly collect samples from cerebrospinal fluid.
Markx is also doing similar screening with his patients. He believes highly sensitive and inexpensive blood tests to detect different antibodies should become part of the standard screening protocol for psychosis.
Also on the horizon: more targeted immunotherapy rather than current “sledgehammer approaches” that suppress the immune system on a broad level, said George Yancopoulos, the co-founder and president of the pharmaceutical company Regeneron.
“I think we’re at the dawn of a new era. This is just the beginning,” said Yancopoulos."
-via The Washington Post, June 1, 2023
#mental illness#schizophrenia#schizoaffective#psychotic disorders#psychology#neurology#autoimmune#autoimmine disease#neuroscience#medical news#medical research#catatonia#immunotherapy#immune system#clinical trials#good news#hope
6K notes
·
View notes
Text
told someone i'm schizophrenic and they ask "are you sure it's not just your mind playing tricks on you" bro what the fuck do you think schizophrenia is
#schizophrenic#schizophrenia#actually schizophrenic#neurodivergent#neurodiverse#actually neurodivergent#mentally ill#actually mentally ill#hallucination#hallucinations
24K notes
·
View notes
Text
hey i just wanted to give a shout out to people with personality disorders real quick. your disorder doesn't make you evil, it doesnt make you an abuser, and it doesnt make you unlovable. you're just as deserving of respect, care, and support as people without personality disorders. stay safe, i love you and i hope you have a happy holiday season. we're in this together <3
#also i hope you remember it's not your fault#i love you so much muah#bpd#borderline personality disorder#npd#narcissistic personality disorder#schizophrenia#aspd#histrionic pd#ocd#bpd positivity#npd positivity#ocd positivity#personality disorder#mental health#mental health awareness#mental health positivity#mental illness positivity#not mlm#dantes talking again
2K notes
·
View notes
Text

Fridge Light Stay On.
A comic coming out in December - an investigation of liminal space, dissociation, lost time, and hauntings.
#art#my art#digital art#comic#web comic#visual poetry#words#journal#diary#mental illness#schizophrenia#Gumroad#a fridge light in the dark
1K notes
·
View notes
Text
If you don't judge people for saying "sorry adhd brain" in public, then don't judge people for saying "sorry schizophrenia brain" in public
If you correct people when they misuse the term "ocd" then you need to correct people when they misuse the terms "psychotic", "delusional", "hallucinating" and "schizophrenic"
If you don't stare, laugh at or fear a stranger in public flapping their hands, then you need to do the same for a stranger in public talking to someone who isn't actually there.
If you give a trigger warning to sensitive topics then you need to give a trigger warning to unreality and false information as a prank.
If you want to normalize medication like antidepressants you also need to normalize medications like antipsychotics.
If you don't like people without your disorder joking about it online and report it as harassment, then you need to do the same for the tons of nonschizophrenics making "schizoposting" memes to make fun of us.
Just please include schizo-spec and psychotic acceptance into your mental illness/neurodiversity acceptance. We are part of your community whether you like it or not. We are constantly stigmatized, misrepresented and made fun of. We do what we can to help you, please return the favor.
Mental illness/neurodiversity acceptance is an ongoing action. We will get nowhere in the long run if we split the community into the "in" group and the "out" group. We could all accomplish so much if we worked together. But you need to include the "weird" people that don't fit into your aesthetic and don't fit the social norms.
Us psychotics and schizo-specs have been struggling for years and have been the only people fighting for ourselves while the people we plead to barely see us as human. If you are nonpsychotic and nonschizo-spec, you can help us more than you realize. Please include us and stick up for us the same way we have been including and sticking up for you.
#mental illness#nd#schizophrenia#neurodivergent#schizophrenic#psychosis#actuallyschizophrenic#mental health awareness#pseriouslypsychotic#neurodivergent community#neurodiversity#mental illness acceptance#neurodiversity acceptance#mental health#sanism
21K notes
·
View notes
Text
my heart goes out to you if you're a disabled person who has a complicated or negative relationship with sleep. if you need to sleep a lot but can't due to life circumstances, or sleeping extra causing other symptoms to flare up. if you can't sleep enough due to pain, or nightmares, or psychosis, or bipolar, or depression. if you sleep way too much and find it hard to stay awake. if you can't fall or stay asleep. if you need medication in order to be able to sleep. if you don't feel rested from sleep. if you wake up a lot in the night. if you have bladder or bowel accidents while asleep. if you twitch or convulse or move too or get injured in your sleep. if you can't control your sleep schedule no matter what. if you can't sleep during "normal" sleeping hours. if you can't sleep for 8+ hours straight but can sleep for shorter amounts of time. if sleep is what you need but for one reason or another you just can't or refuse to do it.
i care about you. your disabilities deserve to be seen and acknowledged
#actually disabled#chronic pain#cripple punk#fibromyalgia#crip punk#insomnia#troubled sleep#trouble sleeping'#sleep disturbances#sleep disorder#sleep disorders#narcolepsy#depression#bipolary#psychosis#schizophrenia#autism#adhd#ptsd#did#dissociative identity disorder#osdd#mental illness#disability#madpunk#]our writing#cpunk#disability culture#cripplepunk#c punk
901 notes
·
View notes
Text
it's okay if you get confused easily. it's okay if you forget things easily. it's okay if you lose track during conversation easily. it's okay if you have to ask for clarification often. it's okay if you struggle to parse information or sensory unit. you're not "playing dumb" or "doing it on purpose". it's okay to be disabled, some people just refuse to be accommodating.
#mad pride#madpunk#mad punk#schizophrenia#mentally chill#mentally ill#mental illness#mental health#adhd#did#ocd#ptsd#autism#brain fog#neurodivergent#mental heath awareness
32K notes
·
View notes
Text
The young woman was catatonic, stuck at the nurses’ station — unmoving, unblinking and unknowing of where or who she was.
Her name was April Burrell.
Before she became a patient, April had been an outgoing, straight-A student majoring in accounting at the University of Maryland Eastern Shore. But after a traumatic event when she was 21, April suddenly developed psychosis and became lost in a constant state of visual and auditory hallucinations. The former high school valedictorian could no longer communicate, bathe or take care of herself.
April was diagnosed with a severe form of schizophrenia, an often devastating mental illness that affects approximately 1 percent of the global population and can drastically impair how patients behave and perceive reality.
“She was the first person I ever saw as a patient,” said Sander Markx, director of precision psychiatry at Columbia University, who was still a medical student in 2000 when he first encountered April. “She is, to this day, the sickest patient I’ve ever seen.”
It would be nearly two decades before their paths crossed again. But in 2018, another chance encounter led to several medical discoveries reminiscent of a scene from “Awakenings,” the famous book and movie inspired by the awakening of catatonic patients treated by the late neurologist and writer Oliver Sacks.
Markx and his colleagues discovered that although April’s illness was clinically indistinguishable from schizophrenia, she also had lupus, an underlying and treatable autoimmune condition that was attacking her brain.
After months of targeted treatments — and more than two decades trapped in her mind — April woke up.
The awakening of April — and the successful treatment of other peoplewith similar conditions — now stand to transform care for some of psychiatry’s sickest patients, many of whom are languishing in mental institutions.
Researchers working with the New York state mental health-care system have identified about 200 patients with autoimmune diseases, some institutionalized for years, who may be helped by the discovery.
And scientists around the world, including Germany and Britain, are conducting similar research, finding that underlying autoimmune and inflammatory processes may be more common in patients with a variety of psychiatric syndromes than previously believed.
Although the current research probably will help only a small subset of patients,the impact of the work is already beginning to reshape the practice of psychiatry and the way many cases of mental illness are diagnosed and treated.
“These are the forgotten souls,” said Markx. “We’re not just improving the lives of these people, but we’re bringing them back from a place that I didn’t think they could come back from.”
– A catatonic woman awakened after 20 years. Her story may change psychiatry.
#block JavaScript in site settings if article is paywalled#April burrel#disability#schizophrenia#lupus#mental illness#catatonia#chronic illness#institutionalization#psychiatry#medical science#healthcare#autoimmune disease#Washington post#knee of huss
3K notes
·
View notes
Text
good morning to these people and these people only: autistic people who constantly put their foot in their mouth, bitches with NPD, undiagnosed freaks who bamboozle the DSM, bipolar or mood disorder girlies and non-girlies in a manic rage, low- or no-empathy weirdos, and psychos (reclaimed). please survive.
#npd#narcissistic personality disorder#bipolar mood disorder#schizophrenia#schizoaffective#mental illness#cluster b#autism#autistic spectrum#empathy deficit disorder#mood disorder#mental disability
3K notes
·
View notes
Text
#“Disabled allies” when people with disabilities actually suffer and it's not just some kind of romanticized version with watered down#symptoms they see on TikTok and people with “bad” mental illness and disabilities more often than not actually need support and care#It's anti ableism until it's not convenient for them.#Leftist#Leftism#Bpd#Borderline#borderline personality disorder#schizophrenia#schizo spectrum#Actually autistic#Bipolar#Bipolar disorder#antisocial personality disorder#Narc abuse#Narc abuse isn't real#NPD#narcissistic personality disorder#Personality disorders#Mood disorders
1K notes
·
View notes