#What is the new variant of Covid?
Text
I've had anxiety pretty much all my life and having my fears/concerns brushed off is not a new thing for me and sometimes it's justified, but it is uniquely annoying in this case because I keep being right, repeatedly, throughout the pandemic, and people are still acting like I'm just being my panicky self and it's not as big a deal as I'm making it.
#for months my mom kept getting on my case about masking in the common areas of her complex#'everyone here is elderly they don't go out! why are you still wearing a mask here?'#and then suddenly what do you know two of her neighbors have covid and I was right#everyone: why are you still isolating and masking so much the pandemic is over!#me: it is not fucking over and it's gonna get worse again because of this#a couple months later: oh god there's a new variant that resists vaccines we couldn't possibly have predicted or prevented this#ironically I got covid somewhere highly improbable back in 2022 and it promptly made my anxiety like 5x worse so now I'm even more annoying#I also just kinda. got worse at spelling and keeping track of information#it's deeply frustrating but at least I never lost taste/smell and meds have helped with the anxiety so eh#still this could have been avoided if people would just take the goddamn thing seriously#and I'm gonna be salty about it for the rest of my life
20 notes
·
View notes
Text
Oh dear God, hazbin hotel and covid are both trending hastags- ARE WE BACK IN 2020?!?!?
#covid 19#why are they both trending#i get hazbin#but what about covid#why covid?!?#why is it back?!?#i had it a week ago#does it have a new variant?#hazbin hotel#i clicked the wrong hastage at first so now theyre out of order#darn
9 notes
·
View notes
Text
i really fucking hate being the only person in my friend/family group that gives a flying fuck about covid
#it's band practice night at our house#i made dinner#half an hour ago my husband says his bass player is sick#well he's not invited i say <- actual exact quote totally ooc#what if he tests negative#that doesn't mean shit anymore something like 80% of home test test negative these days#they aren't meant for the new variants#fifteen minutes ago: he tested negative#I still don't care. in fact i don't care if its covid or not. I don't want to get regular sick or possibly cognitively impaired 4 life sick#guess who just walked into the motherfucking band shed#the small enclosed unventilated space where the band practices?#and i have nowhere to go#no other friends or family who could i could be 100% are safe
5 notes
·
View notes
Text
something bad is happening to my spine
#i don't know what but#this is super fucked up#i can't be sat up for more than like 10#minutes without a specific bit of my spine feeling like it's almost like. burning#it feels like there's a sparkler in there just fucking going at it#i really want to mention it to my dad but i also don't because . ugh#k really need to go to a doctor about this#but also he's probably going to tell me that covid cases are rising and there's a new variant#and we can't afford to get covid i know that but it fuckinf hurts so bad#luckily lying down makes it go away but. gos
3 notes
·
View notes
Text
Plagueblogging / covid nursing 2023
#Unexpected development in covid nursing this season#Generally the intensity of covid itself seems to be less#Compared to this time last year#I guess different variant plus widespread vaccination in the older demographic especially#So now rather than high octane respiratory nursing#It's worked out now that we've got room and there's a rolling forever outbreak#That now we are getting send all the cancer oncology renal haematology patients that test positive#So now instead of general medical nursing#It's leaning much heavier towards oncology nursing#Which is. Idk there's a shift#Usually with medical it's a really obvious decline as people go towards end of life and we can make it relatively graceful#But man brain mets are another beast#There's a patient I never met but was just there for the edges of#And I think it will be a while before they don't linger in my mind#I'm so glad the family were onto it and we're accepting and understood her journey#And she was able to pass peacefully with them there#But man I'm glad I wasn't the one who had to make those calls#I was guiding the new grad with advice but they ultimately made different choices than I would#Luckily the patient and family's wishes were able to be followed#But imagining the what ifs of me being in that position had me bursting into tears again#Good practice#I'd have to know to find my voice and ask the question - do you want me to call a medical emergency or do you want some quiet?#That's not a question we usually have to ask because it's not usually so quick so the goals of care can be updated#Cancer cw
4 notes
·
View notes
Text
i cannot believe five days ago a doctor told me to take these two anti-inflammatory medicines together after i specifically asked if i should do that and then today another doctor was like ur doing what? don’t do that. absolutely do not do that.
#like what 😭😭#like why would the first one tell me to do that then#also apparently i’m a medical mystery#so that’s super fun super cool loving life#(i am very sad)#today i told him all my symptoms and he was really like huh. that’s weird#personally i think it’s long covid from one of the new variants bc i had NONE of these problems until i got covid :)#but he was like if it is that then we know nothing about it and we’re just gonna have to see what happens to u#again very fun very cool
2 notes
·
View notes
Text
Scientists at UC Riverside have demonstrated a new, RNA-based vaccine strategy that is effective against any strain of a virus and can be used safely even by babies or the immunocompromised.
Every year, researchers try to predict the four influenza strains that are most likely to be prevalent during the upcoming flu season. And every year, people line up to get their updated vaccine, hoping the researchers formulated the shot correctly.
The same is true of COVID vaccines, which have been reformulated to target sub-variants of the most prevalent strains circulating in the U.S.
This new strategy would eliminate the need to create all these different shots, because it targets a part of the viral genome that is common to all strains of a virus. The vaccine, how it works, and a demonstration of its efficacy in mice is described in a paper published today in the Proceedings of the National Academy of Sciences.
“What I want to emphasize about this vaccine strategy is that it is broad,” said UCR virologist and paper author Rong Hai. “It is broadly applicable to any number of viruses, broadly effective against any variant of a virus, and safe for a broad spectrum of people. This could be the universal vaccine that we have been looking for.”
Continue Reading.
18K notes
·
View notes
Text
.
#idk what the fuck is this new covid variant#but i got it at the vienna show and i swear it wants to kill me#like it’s been 2 weeks and it’s only getting worse#but i got some prescription pills with codeine today so pray for me to actually get a decent sleep
0 notes
Text
"A team of researchers at Washington University in St. Louis has developed a real-time air monitor that can detect any of the SARS-CoV-2 virus variants that are present in a room in about 5 minutes.
The proof-of-concept device was created by researchers from the McKelvey School of Engineering and the School of Medicine at Washington University...
The results are contained in a July 10 publication in Nature Communications that provides details about how the technology works.
The device holds promise as a breakthrough that - when commercially available - could be used in hospitals and health care facilities, schools, congregate living quarters, and other public places to help detect not only the SARS-CoV-2 virus, but other respiratory virus aerosol such as influenza and respiratory syncytial virus (RSV) as well.
“There is nothing at the moment that tells us how safe a room is,” Cirrito said, in the university’s news release. “If you are in a room with 100 people, you don’t want to find out five days later whether you could be sick or not. The idea with this device is that you can know essentially in real time, or every 5 minutes, if there is a live virus in the air.”
How It Works
The team combined expertise in biosensing with knowhow in designing instruments that measure the toxicity of air. The resulting device is an air sampler that operates based on what’s called “wet cyclone technology.” Air is sucked into the sampler at very high speeds and is then mixed centrifugally with a fluid containing a nanobody that recognizes the spike protein from the SARS-CoV-2 virus. That fluid, which lines the walls of the sampler, creates a surface vortex that traps the virus aerosols. The wet cyclone sampler has a pump that collects the fluid and sends it to the biosensor for detection of the virus using electrochemistry.
The success of the instrument is linked to the extremely high velocity it generates - the monitor has a flow rate of about 1,000 liters per minute - allowing it to sample a much larger volume of air over a 5-minute collection period than what is possible with currently available commercial samplers. It’s also compact - about one foot wide and 10 inches tall - and lights up when a virus is detected, alerting users to increase airflow or circulation in the room.
Testing the Monitor
To test the monitor, the team placed it in the apartments of two Covid-positive patients. The real-time air samples from the bedrooms were then compared with air samples collected from a virus-free control room. The device detected the RNA of the virus in the air samples from the bedrooms but did not detect any in the control air samples.
In laboratory experiments that aerosolized SARS-CoV-2 into a room-sized chamber, the wet cyclone and biosensor were able to detect varying levels of airborne virus concentrations after only a few minutes of sampling, according to the study.
“We are starting with SARS-CoV-2, but there are plans to also measure influenza, RSV, rhinovirus and other top pathogens that routinely infect people,” Cirrito said. “In a hospital setting, the monitor could be used to measure for staph or strep, which cause all kinds of complications for patients. This could really have a major impact on people’s health.”
The Washington University team is now working to commercialize the air quality monitor."
-via Forbes, July 11, 2023
-
Holy shit. I know it's still early in the technology and more testing will inevitably be needed but holy shit.
Literally, if it bears out, this could revolutionize medicine. And maybe let immunocompromised people fucking go places again
Also, for those who don't know, Nature Communications is a very prestigious scientific journal that focuses on Pretty Big Deal research. Their review process is incredibly rigorous. This is an absolutely HUGE credibility boost to this research and prototype
#covid#covid 19#pandemic#plague#rsv#influenza#the flu#science and technology#medical research#medical technology#biochemistry#immunology#good news#hope#hope posting
6K notes
·
View notes
Link
The World Health Organisation (WHO) is keeping an eye on the XBB.1.16 COVID-19 subvariant, which has been spreading through India for a while and is now responsible for a recent uptick in cases there. According to WHO, there are more than 600 Omicron subvariants that are currently in circulation, including Covid XBB.1.16.
#what to know about the new covid-19 variant#COVIDXBB.1.1#Symptoms of Covid XBB.1.16#What is XBB.1.16 Variant?
0 notes
Text
Worldwide, there were more than 11,000 reported deaths from COVID between mid-December 2023 and mid-January 2024, and more than half of those deaths occurred in the U.S. In that same time frame, nearly one million cases were reported to the World Health Organization globally (although reduced testing and reporting means this is likely a vast undercount). In particular, epidemiologists are monitoring the newest variant of SARS-CoV-2, JN.1, and looking for any signs that it may be more severe than previous strains.
Although the WHO declared an end to the COVID public health emergency in May 2023, the organization has emphasized that the pandemic isn’t over—it’s just entered an endemic phase, which means that the virus will continue to circulate indefinitely.
[...]
How would you describe the overall state of COVID at this point in the pandemic?
COVID’s not in the news every day, but it’s still a global health risk. If we look at wastewater estimates, the actual circulation [of SARS-CoV-2] is somewhere between two and 20 times higher than what’s actually being reported by countries. The virus is rampant. We’re still in a pandemic. There’s a lot of complacency at the individual level, and more concerning to me is that at the government level.
[...]
"We understand you don’t want to hear about it. I don’t want to talk about it. But we need to because there’s more we can do. We cannot prevent all infections. We cannot prevent all deaths. But there’s a hell of a lot more that we can do to keep people safe and save them from losing a loved one"
2K notes
·
View notes
Text
#COVID new variant#BF.7 Variant#What are COVID variants?#COVID-19 variants#omicron subvariants BF.7#Covid variant BF-7#Covid new variant Precautions#Covid virus#Kauvery Hospital
1 note
·
View note
Text
The Swiss Cheese Model of Covid Prevention

An edited version of the swiss cheese model tailored towards the measures that you as an individual can take to minimize your risk of infection. Public health is ultimately what its name implies, public, but that doesn't mean you're powerless.
Covid prevention is not all-or-nothing. Think of it as risk reduction, rather than a binary.
Let's go through these step by step.
VACCINES
The current vaccines are meant primarily to reduce chances of severe illness, hospitalization, and death. They will reduce your chance of infection a bit--but not nearly as much as you might think. You should still get your boosters regularly, because avoiding severe illness is of course worth doing.
If you haven't gotten the updated monovalent vaccine yet, go get it. It is not a booster. Think of it as a new vaccine. It's targeted towards the XBB lineages, which are now the most common variants. Your last boosters were likely of the bivalent type, aimed at both the original Covid strain from 2020 and Omicron. The new vaccine is monovalent, meaning it targets one family in particular.
Some studies suggest that the Novavax vaccine, which is a more traditional protein-based vaccine, is more effective and safer than mRNA vaccines, and offers better protection against future variants. Of course, the data we have so far isn't 100% conclusive (the last paper I linked is a preprint). Make of these findings what you will, just something to keep in mind. The new Novavax vaccine's availability is still limited, especially outside of the US.
MASKS

Masking is one of the most effective ways to protect yourself. While it is true that masking and reducing Covid transmission protects those around you, the idea that masks can't protect the wearer is outdated information from the early days of the pandemic when medical authorities refused to acknowledge that Covid is airborne.
The key to protecting yourself is to wear a well-fitting respirator. You want to minimize any gaps where air might leak out. If your glasses get fogged up, that's a sign that air is leaking.
Headbands will always have a tighter fit than earloop masks (and therefore provide better protection). However, you can use earloop extenders to improve the fit of earloop masks. You can find these online. Your comfort in wearing a mask is important, but there are options for compromise.
The above graphic doesn't include elastomeric respirators. While some (like the Flo Mask) are expensive, they can be much more affordable than buying disposables--look for P100 respirators at your local hardware store, but make sure it fits your face well.
For more general information, see this FAQ. For mask recommendations (NA-centric, sorry!), see my list here or Mask Nerd's YouTube channel.
For situations where you need to hydrate but don't want to take your mask off, consider the SIP valve.
Not even N95s are foolproof (N95 means it filters at least 95% of particles--with the other 5% potentially reaching you). Most people will likely not have a perfect fit. There will be situations where you'll have to take your mask off. The key is risk reduction, and that's why the Swiss cheese model is crucial.
If you can't afford high-quality masks, look for a local mask bloc or other organization that gives out free masks. Project N95 has unfortunately shut down. In Canada, there's donatemask.ca.
AVOID CROWDED INDOOR SPACES
This is rather self-explanatory. Indoor transmission is much, much, much more likely than outdoor transmission. If it's possible to move an activity outdoors instead, consider doing so.
If possible, try going to places like stores or the post office during less busy hours.
Viral particles can stay in the air for a considerable amount of time even after the person who expelled them has left. Do not take off your mask just because no one is currently present, if you know that it was previously crowded.
A CO2 monitor is a decent proxy for how many viral particles may have accumulated in the air around you. The gold standard is the Aranet4, but it's expensive, so here are some more affordable alternatives.
VENTILATION AND AIR FILTERS
Ventilation is effective for the same reason that outdoors is safer than indoors. If it's warm enough, keep windows open whenever possible. If it's cold, even cracking them open occasionally is better than nothing. Try to open windows or doors on different sides of a room to maximize airflow.
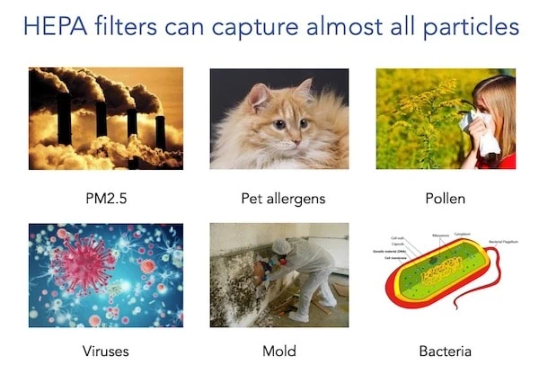
HEPA air filters can significantly reduce viral transmission indoors. Make sure to find one suitable for the room size, and replace the filters regularly. You want to look for devices with HEPA-13 filters.
You can use websites like these to calculate how long it takes for a device to change all the air in a room. Remember what I said about viral particles being able to hang around even after people have left? If an air purifier provides 2 air changes per hour, that means that after 30 minutes, any potential viral particles should be gone.
If you can't afford a commercial air filter, here's a useful DIY filter you can make with relatively simple materials. The filtration capacity is great--but due to being built with duct tape, replacing filters will be a challenge.
If you have to hold meetings or meet with people at work, having a smaller filter on the desk between you will also reduce chances of infection.
As a bonus, HEPA filters will also filter out other things like dust and allergens!
REDUCE LENGTH OF EXPOSURE IF EXPOSURE IS UNAVOIDABLE
Viral load refers to the amount of virus in a person's blood. If you've been exposed to someone with Covid, how much you've been exposed matters.
You might escape infection if the viral load you've been exposed to is very small. Or, even if you get infected, there will be less virus in you overall, leading to milder illness--and crucially, a lower chance of the virus penetrating deep into your body, creating reservoirs in your organs and wreaking long-term havoc.
A low viral load is also less contagious.
This is the same reason that wearing your mask most of the time, but having to take it off for eating, is still much better than not wearing your mask at all.
RECHARGEABLE PORTABLE AIR FILTERS
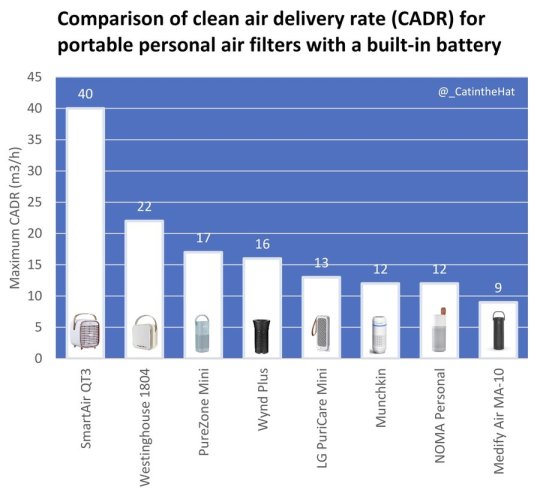
You might attract some odd looks. But if you're at high risk or just want to be as protected as possible, small portable air filters can help. Try to find models small enough to take with you on public transportation, to school, or while traveling.
These devices will be far too small to clean the air in the whole room. The goal is to have it filter air in your immediate vicinity. Be sure to angle the device so that the air is blowing in your face.
Unfortunately, rechargeable devices are much rarer and harder to find than normal air filters, and many are also expensive.
The best option at the moment, apart from DIY (which is possible, but you need to know what you're doing), seems to be the SmartAir QT3. The size and shape are a bit clunky, but it fits in a backpack. Its battery life isn't long, but it can be supplemented with a power bank.
NASAL SPRAYS
There's some research that suggests that some nasal sprays may be effective in reducing risk of infection by interfering with viruses' ability to bind to your cells.
These sprays are generally affordable, easy to find, and safe. The key ingredient is carrageenan, which is extracted from seaweed. So there are no potential risks or side effects.
Be sure to follow the instructions on the packaging carefully. Here's a video on how to properly use nasal sprays if you've never used them before.
Covixyl is another type of nasal spray that uses a different key ingredient, ethyl lauroyl arginate HCI. It also aims to disrupt viruses' ability to bind to cell walls. Unfortunately, I think it's difficult to obtain outside of the US.
CONCLUSION
None of the methods listed here are foolproof on their own. But by layering them, you can drastically reduce your chances of infection.
The most important layers, by far, are masking and air quality. But you should also stay conscientious when engaging with those layers. Don't let yourself become complacent with rules of thumb, and allow yourself to assess risk and make thought out decisions when situations arise where you might have to take off your mask or enter a high-risk indoor area, such as a hospital.
Remember that the goal is risk reduction. It's impossible to live risk-free, because we live among countless other people. But you can use knowledge and tools to keep yourself as safe as possible.
1K notes
·
View notes
Text
now that I got covid all I have is my Gerard Way fanfics and the Hot Topic website /hj
#tw covid#covid 19#i got the new covid variant#it feels like strep throat#also yes im look at far too expensive stuff on Hot Topic#I'm sick I'll do what i want man#i'm not okay (i promise)
0 notes
Link
Is the BA.2.75 subvariant more transmissible and does the COVID-19 vaccine protect against it? CNA looks into the new variant and the concerns surrounding it.
0 notes
Text
You might be forgiven for thinking it’s been a very quiet few months for the Covid-19 pandemic. Besides the rollout of new boosters, the coronavirus has largely slipped out of the headlines. But the virus is on the move. Viral levels in wastewater are similar to what they were during the first two waves of the pandemic. Recent coverage of the so-called Pirola variant, which is acknowledged to have “an alarming number of mutations,” led with the headline “Yes, There’s a New Covid Variant. No, You Shouldn’t Panic.”
Even if you haven’t heard much about the new strain of the coronavirus, being told not to panic might induce déjà vu. In late 2021, as the Omicron variant was making its way to the United States, Anthony Fauci told the public that it was “nothing to panic about” and that “we should not be freaking out.” Ashish Jha, the Biden administration’s former Covid czar, also cautioned against undue alarm over Omicron BA.1, claiming that there was “absolutely no reason to panic.” This is a telling claim, given what was to follow—the six weeks of the Omicron BA.1 wave led to hundreds of thousands of deaths in a matter of weeks, a mortality event unprecedented in the history of the republic.
Indeed, experts have been offering the public advice about how to feel about Covid-19 since January 2020, when New York Times columnist Farhad Manjoo opined, “Panic will hurt us far more than it’ll help.” That same week, Zeke Emanuel—a former health adviser to the Obama administration, latterly an adviser to the Biden administration—said Americans should “stop panicking and being hysterical.… We are having a little too much [sic] histrionics about this.”
This concern about public panic has been a leitmotif of the Covid-19 pandemic, even earning itself a name (“elite panic”) among some scholars. But if there’s one thing we’ve learned, three and a half years into the current crisis, it’s that—contrary to what the movies taught us—pandemics don’t automatically spawn terror-stricken stampedes in the streets. Media and public health coverage have a strong hand in shaping public response and can—under the wrong circumstances—promote indifference, incaution, and even apathy. A very visible example of this was the sharp drop in the number of people masking after the CDC revised its guidelines in 2021, recommending that masking was not necessary for the vaccinated (from 90 percent in May to 53 percent in September).
As that example suggests, emphasizing the message “don’t panic” puts the cart before the horse unless tangible measures are being taken to prevent panic-worthy outcomes. And indeed, these repeated assurances against panic have arguably also preempted a more vigorous and urgent public health response—as well as perversely increasing public acceptance of the risks posed by coronavirus infection and the unchecked transmission of the virus. This “moral calm”—a sort of manufactured consent—impedes risk mitigation by promoting the underestimation of a threat. Soothing public messaging during disasters can often lead to an increased death toll: Tragically, false reassurance contributed to mortality in both the attacks on the World Trade Center and the sinking of the Titanic.
But at a deeper level, this emphasis on public sentiment has contributed to confusion about the meaning of the term “pandemic.” A pandemic is an epidemiological term, and the meaning is quite specific—pandemics are global and unpredictable in their trajectory; endemic diseases are local and predictable. Despite the end of the Public Health Emergency in May, Covid-19 remains a pandemic, by definition. Yet some experts and public figures have uncritically advanced the idea that if the public appears to be tired, bored, or noncompliant with public health measures, then the pandemic must be over.
But pandemics are impervious to ratings; they cannot be canceled or publicly shamed. History is replete with examples of pandemics that blazed for decades, sometimes smoldering for years before flaring up again into catastrophe. The Black Death (1346–1353 AD), the Antonine Plague (165–180 AD), and the Plague of Justinian (541–549 AD), pandemics all, lacked the quick resolution of the 1918 influenza pandemic. A pandemic cannot tell when the news cycle has moved on.
Yet this misperception—that pandemics can be ended by human fiat—has had remarkable staying power during the current crisis. In November 2021, the former Obama administration official Juliette Kayyem claimed that the pandemic response needed to be ended politically, with Americans getting “nudged into the recovery phase” by officials. It is fortunate that Kayyem’s words were not heeded—the Omicron wave arrived in the US just weeks after her article ran—but her basic premise has informed Biden’s pandemic policy ever since.
Perhaps even less responsibly, the physician Steven Phillips has called for “new courageous ‘accept exposure’ policies”—asserting that incautious behavior by Americans would be the true signal of the end of the pandemic. In an essay for Time this January, Phillips wrote: “Here’s my proposed definition: the country will not fully emerge from the Covid-19 pandemic until most people in our diverse nation accept the risk and consequences of exposure to a ubiquitous SARS-CoV-2, the virus that causes Covid-19.”
This claim—that more disease risk and contagion means the end of a disease event—runs contrary to the science. Many have claimed that widespread SARS-CoV-2 infections will lead to increasingly mild disease that poses fewer concerns for an increasingly vaccinated (or previously infected) population. In fact, more disease spread means faster evolution for SARS-CoV-2, and greater risks for public health. As we (A.C. and collaborators) and others have pointed out, rapid evolution creates the risk of novel variants with unpredictable severity. It also threatens the means that we have to prevent and treat Covid-19: monoclonal antibody treatments no longer work, Paxlovid is showing signs of viral resistance, and booster strategy is complicated by viral evolution of resistance to vaccines.
But these efforts to manage and direct public feelings are not just more magical thinking; they are specifically intended to promote a return to pre-pandemic patterns of work and consumption. This motive was articulated explicitly in a McKinsey white paper from March 2022, which put forward the invented concept of “economic endemicity”—defined as occurring when “epidemiology substantially decouples from economic activity.” The “Urgency of Normal” movement similarly used an emotional message (that an “urgent return to fully normal life and schooling” is needed to “protect” children) to advocate for the near-total abandonment of disease containment measures. But in the absence of disease control measures, a rebound of economic activity can only lead to a rebound of disease. (This outcome was predicted by a team that was led by one of the authors [A.C.] in the spring of 2021.)
A pandemic is a public health crisis, not a public relations crisis. Conflating the spread of a disease with the way people feel about responding to that spread is deeply illogical—yet a great deal of the Biden administration’s management of Covid-19 has rested on this confusion. Joe Biden amplified this mistaken perspective last September when he noted that the pandemic was “over”—and then backed that claim by stating, “If you notice, no one’s wearing masks. Everybody seems to be in pretty good shape.” The presence or absence of health behaviors reveals little about a threat to health itself, of course—and a decline in mask use has been shaped, in part, by the Biden administration’s waning support for masking.
Separately, long Covid poses an ongoing threat both at an individual and a public health level. If our increasingly relaxed attitude toward public health measures and the relatively unchecked spread of the virus continue, most people will get Covid at least once a year; one in five infections leads to long Covid. Although it’s not talked about a lot, anyone can get long Covid; vaccines reduce this risk, but only modestly. This math gets really ugly.
The situation we are in today was predictable. It was predictable that the virus would rapidly evolve to evade the immune system, that natural immunity would wane quickly and unevenly in the population, that a vaccine-only strategy would not be sufficient to control widespread Covid-19 transmission through herd immunity, and that reopening too quickly would lead to a variant-driven rebound. All of these unfortunate outcomes were predicted in peer-reviewed literature in 2020–21 by a team led by one of the authors (A.C.), even though the soothing public messaging at the time called it very differently.
As should now be very clear, we cannot manifest our way to a good outcome. Concrete interventions are required—including improvements in air quality and other measures aimed at limiting spread in public buildings, more research into vaccine boosting strategy, and investments in next-generation prophylactics and treatments. Rather than damping down panic, public health messaging needs to discuss risks honestly and focus on reducing spread. Despite messages to the contrary, our situation remains unstable, because the virus continues to evolve rapidly, and vaccines alone cannot slow this evolution.
In the early months of the pandemic, many in the media drew parallels between the public’s response to Covid-19 and the well-known “stages of grief”: denial, bargaining, anger, depression, and acceptance. The current situation with Covid-19 calls for solutions, not a grieving process that should be hustled along to the final stage of acceptance.
833 notes
·
View notes