#oxygen therapy
Text



Thinking about these views for the weekend… 😉
#braced babe#med fet#neck brace#oxygen#brace aesthetic#medical aesthetic#ng tube#catheter#soft collar#wrist brace#oxygen mask#oxygen therapy#tubie babe#braced and tubed
61 notes
·
View notes
Note
How would pneumonia have been treated in the mid to late 1930s, during the Great Depression?
This actually varies a LOT depending on where the person was, what their socioeconomic status was, whether they were getting hospital care or being cared for at home, etc...
At the highest level of care, someone could be in a hospital paying to be in a private room (which at the time meant paying for a private doctor (not just the hospital resident) and private nurse (not just the student nurses training at the hospital) to care for them, plus either family members or servants to provide basic direct care), on continuous oxygen therapy, getting arterial blood gas readings (super duper high tech), and receiving the most effective antibiotic of the day- sulfanilamide.
At the "lowest" level of care, someone was probably going to be cared for at home by a family member. To be clear, home nursing was still common at this time and there would have still been generational knowledge about how to feed, clean, and otherwise care for an ill person- knowledge that is largely lost today. If someone had access to a medical text aimed at home caregivers, it likely had advice to purge the body by taking medications designed to make the ill person sweat or vomit. This, and placing a mustard plaster against the person's chest.
You can see that these are two extremely different approaches to care, and most people would be somewhere in the middle- potentially able to afford a doctor's visit or prescription for sulfanilamide, but not private hospital care.
Or, if they did need hospital care (usually just those who didn't have someone to care for them at home, or those who needed oxygen), they would be on a public ward, probably cared for mostly by student nurses and the hospital resident (literally a doctor just out of training who lived and worked full time at the hospital for a year or so before setting up their own practice).
Oxygen therapy would have been available in hospitals at this point in pressurized tanks stored near patient beds. Pneumonia was one of the first uses of medical oxygen, which was titrated to the patient's level of cyanosis and level of consciousness.
Oxygen delivery mechanisms were developed in WWI and resembled just about what we have now in the way of cannulas and masks. Interestingly enough, there was a bitter debate at this time about whether continuous or intermittent oxygen was best. Continuous eventually won out, but not until the 1970's.
47 notes
·
View notes
Text
Just some random pic of these two lovely men
#house md#gregory house#james wilson#banter#voldemort#oxygen therapy#hilson#robert sean leonard#hugh laurie
43 notes
·
View notes
Text
Hyperbaric Medicine (HBO)
I'm sorry, what is that?

I have a side hustle as a hyperbaric medicine provider and I am here to give you the down and dirty!
Sometimes referred to as HBO (hyperbaric oxygen), hyperbaric or dive medicine is a specialty that utilizes oxygen at high pressure to treat a variety of conditions, primarily things involving wounds. We place a patient in a chamber, deliver 100% oxygen to them, pressurize the chamber, and keep them in there for about 120 minutes. Since oxygen is the number one thing you need to heal a wound, we use a lot of it to try and speed up the process.
The Basics
Wait - what? HOW? Try not to have PTSD from your days in chemistry, but remember these?

The treatment physiology of hyperbarics relies on gas laws. Recall that it takes a lot of pressure to dissolve a gas into a liquid.
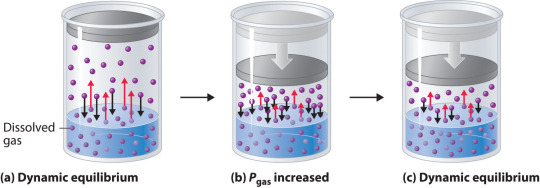
We use pressure to force oxygen into the blood stream at high rates to facilitate wound healing. For reference, most of your oxygen content is bound to hemoglobin (~98%). You do have dissolved oxygen in your blood, represented by your PaO2/PvO2 in a blood gas. However, this makes up a fraction of O2 content (~2%: if you want a clinical soap box, you should hear me talk about blood gases to students lol). A normal ABG would have a PaO2 of 65-100. An ABG acquired during hyperbaric treatment would be well over 2,000.
As an aside, recall that ambient air is 21% oxygen. Also, as a reminder, we exist at 1.0 ATA of pressure (one atmosphere).
How is it done?
Delivering oxygen this way requires delivery of a lot of pressure. We utilize dive chambers for this purpose. There are two types of chambers:
Monoplace: literally looks like a class coffin. Holds one patient and delivers oxygen at pressure through the entire chamber. These are very popular at wound centers.

Multiplace: literally looks like a submarine. Holds 2+ patients and delivers oxygen at pressure to individual patients hooked up to hoods or masks. These are found at tertiary care/academic medical centers.

Literally, the multiplace hoods make you look like a silly space person.

The reason oxygen is delivered this way in a multiplace chamber is to reduce the risk of fire. Oxygen at pressure can go boom. Having an entire chamber full of O2 is a big risk. So, we deliver the gas individually to each patient.
How did it start?
Dinking around with gases at pressure has been a thing for 400 years. However, it didn't become a more focused endeavor until the first dive suits started to be a thing in the 1870s. The specialty itself is relatively new, developed in the 1930s due to advent of decompression illness with divers. Things really progressed in the 1950s.
One pivotal study was "Life without Blood" in 1959. Dr. Boerema proved that he could keep a pig alive with HBO alone. The ethics of this experiment are questionable but he exsanguinated a pig under hyperbaric conditions (3.0 ATA, 100% FiO2). Plasma was left behind. By doing this, he proved that, at pressure, an organism does not need hemoglobin to live. Kind of a radical thing to prove! Don't worry, the pigs did get their blood back and recovered without issue.
What is treated with HBOT? (hyperbaric oxygen therapy)
Anything related to wound healing can be treated with HBOT. We also treat carbon monoxide poisoning, air gas embolism, and decompression sickness with HBOT. I'll start with those since they are (imo), the most clinically interesting. ;-D
Carbon monoxide poisoning: The physiology of using HBOT to treat CO poisoning is based on the binding affinity of CO to hemoglobin. CO has 200 x the binding affinity for hemoglobin than O2 or CO2 does. Because the binding sites are taken up by CO, hemoglobin cannot pick up O2. It also can't offload whatever O2 is already bound. The goal with HBOT is to bombard the blood with massive amounts of O2 to force CO off.

For reference, it would take about 6 hours for CO to offload on its own from hemoglobin on room air. It would take half as long at 100% FiO2 delivered at standard air pressure (1.0 ATA). CO is rapidly forced off within 30 minutes with HBOT. With very severe CO poisoning, particularly in cases of LOC, this is vital for limitation of hypoxia and neurological sequelae of exposure. Treatment is 1-3 "dives" depending on clinical context. The patient is treated at 2.8 ATA (60 feet of sea water) for about 120 minutes.
Air gas embolism: This occurs when gas is accidentally introduced into circulation. It can either be venous or arterial. The venous system has much more flexibility in tolerance for air bubbles. 15 cc or less of gas introduction is probably not going to result in symptoms. Higher volumes go to the lungs and can result in local lung infarction.
The real danger with this is air introduced into arterial circulation. Depending on where it is introduced, it can go directly to the heart causing an MI, or to the brain causing a stroke. Any volume of air introduced into arterial circulation is bad news bears. Treatment is usually 1 "dive" but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? If we ascend too quickly, the air bubble will reform.
Decompression sickness: This occurs primary with scuba divers who ascended too quickly. Scuba divers generally breath mixed gas, most commonly air (21% O2, ~79% N2) or nitrox (35% O2, ~65% N2). As someone is diving, the nitrogen they breath is also dissolved into their blood since they are at a pressure greater than 1.0 ATA. If a diver ascends too quickly, the nitrogen dissolved in the blood will rapidly reform air bubbles in the blood. We just mentioned how that is problematic.
Since air bubbles can go everywhere in circulation, the symptoms are variable ranging from headache, vertigo, nausea, joint pain, chest pain, stroke symptoms, loss of bowel/bladder function, etc. The treatment for this is to recompress the patient and very slowly ascend in the HBO chamber. Treatment is usually 1 dive but could be more based on the context. The patient is treated at 2.8 ATA for 30 minutes and then the ascent is extremely slow. The whole dive takes about 5 hours. Why so long? Again, if we ascend too quickly, the air bubble will reform.
Wound related conditions: there are roughly 15 approved diagnoses for HBO by Medicare in the USA. This is important to mention because if a condition is not covered, paying out of pocket is extremely cost-prohibitive. Insurance is billed $6,000 per treatment! Some of the most common conditions treated are osteoradionecrosis, soft-tissue radionecrosis, irradiation cystitis with hematuria, and refractory chronic osteomyelitis. Wounds created from radiation exposure have the best evidence to support the use of HBOT. These are considered outpatient conditions so patients come to be treated Monday-Friday. We dive to 2.4 ATA for 120 minutes. At minimum, patients are prescribed 20 dives but most treatment protocols for radiation induced injuries is at least 40 dives.
As you can see, this is a HUGE commitment for the patient. One dive is not enough for these wound related conditions. As a hyperbaric provider, I can say that we have patients with such significant symptom relief from HBO. For example, irradiation cystitis with hematuria is extremely debilitating. Patients are fatigued from chronic blood loss, deal with painful bladder spams and pelvic pain, pain with urination, and increased frequency. The blood can clot and obstruct their urethra or foley catheter. Symptoms like this limit quality of life. HBOT makes a huge difference for them.
Benefits
Anyone who has barriers to wound healing can benefit from HBO. Barriers include vascular disease, CKD, COPD, DM, heart failure, and immunocompromised status. The goal is symptom resolution/improvement or healing of the wound. Some patients get approved for far more treatments than we typically do. Usually the maximum insurance will cover is 60. However, in some situations, the clinical benefit of continued treatments is recognized by insurance and treatment is extended.
As a provider, I get to know these patients pretty well. They show up every day that I am staffing in HBO and it is rewarding to see them improve. Compared to my critical care role, this is a nice change of pace.
Adverse Reactions and Risks
There are risks and side effects to HBO. The most common are barotrauma, pneumothorax, seizure, temporary worsening of cataracts/vision, and abdominal distention.
Barotrauma of the ears and sinuses is by the most common issue we face in HBOT. If patients are not able to clear their ears as they descend ("pop" their ears), they can rupture their ear drums. Patients that cannot descend without extreme pain may need myringotomy tubes (ear tubes) to assist with equalizing pressure.
Seizure is a risk of HBOT and that primarily comes from oxygen reducing the seizure threshold. We mitigate this with "air breaks". These are 5 minutes intervals of the treatment where the patient is receiving air rather than 100% O2. Example, we treat at 100% for 30 minutes, have a 5 minute air break, repeat x 2. Obviously the people at highest risk are those with epilepsy or taking seizure threshold reducing medications.
HBOT can worsen cataracts and vision temporarily. The mechanism of this is poorly understood but we know it is reversible. Distance vision is affected the most.
Contraindications
The only absolute contraindication to HBOT is an untreated pneumothorax. There are many relative contraindications that require a risk benefit analysis. An example of this is pregnancy. HBOT has not been thoroughly studied in pregnancy and is not recommended EXCEPT in cases of CO poisoning where we know that the CO concentration is higher in fetal circulation than maternal. Always treat a pregnant person with CO poisoning.
Other potential contraindications include use of certain chemotherapy agents, COPD with blebs/bullae, severe heart failure, epilepsy, sinus/HEENT disease, claustrophobia, certain implanted devices, or active infection.
With certain chemo agents, they can lower the seizure threshold putting patients at higher risk of seizure in the chamber. People with COPD and blebs are at risk of those blebs popping under pressure and causing acute respiratory distress. People with heart failure can experience flash pulmonary edema after an HBO treatment. If people are claustrophobic, obviously spending time in a monoplace chamber can trigger panic attacks. At my center, we sometimes have people referred to our multiplace chamber for exactly that reason.
Most implanted medical devices are HBOT compliant. Generally, pacers and other devices are tested at 4.0 ATA of pressure. We double check with the manufacturer that the device is compliant. If it isn't, we cannot safely treat and have to deny the consult.
Obviously, if someone is sick, we don't want them in the chamber. Particularly colds, severe allergies, fever, or anything that is affecting HEENT. People with acute sinus infection are unable to clear sufficiently to dive. Even if they can clear, they feel miserable. No need to go through that.
Safety Issues
I mentioned that high O2 environments are at risk for explosion. Safety is the number one concern with any chamber. The goal is to reduce risk of fire by removing fabrics that create static (anything synthetic), removing electronic devices that are not HBOT approved, and going through multiple levels of safety checks for patients and for chamber preparation.
At our chamber, only 100% cotton is allowed in the chamber. All patients have special scrubs that they wear during treatment. No electronic devices can be brought in the chamber which includes phones, tablets, laptops, e-readers, watches, pagers, etc. We do have HBOT approved IV pumps and radio headsets that we use. These have been tested at 4.0 ATA. The radio headsets are for the attendant (staff member) who is in the chamber and this is also for safety purposes. Since we have a mulitplace chamber, a staff member is always in the chamber with the patient(s).
One thing I do want to address is that some people are concerned about putting a patient with active cancer into the chamber. There is concern that the high O2 environment will "feed" the cancer. There is simply not data to support this. Active cancer is not a contraindication to HBOT.
And there you have it! The down and dirty of HBOT! Hopefully you learned something cool. If you think you have a patient who would benefit, find your local HBOT provider. We are always happy to talk with you about the process. If you care about a soapbox of how insurance companies suck, see below. :-D
Soapbox: I will say, I have definitely been frustrated with insurance companies. They are the gatekeepers of this treatment. You can have several providers supporting the use of treatment and an insurance company can still say "no". Very frustrating.
A prime example of this are patients who have avascular necrosis that is steroid or chemotherapy induced. These are often younger patients (late teens, early 20s) who have/had leukemia of some kind. They end up having necrosis at a joint, usually the femoral head, that will likely result in complete joint replacement at a young age. No orthopedic surgeon wants to replace joints on a young person. It comes will all kind of problems and always needs revision later in life.
Insurance companies will say "we only cover radiation induced necrosis" because that is what the literature supports. Yes, they are correct that the vast majority of studies support HBOT for radiation induced injury. However, the pathophysiology of the tissue destruction, while a little different, ends up with the SAME problem. There are studies that support HBOT use in these situation but not nearly as many as radiation induced injury. The result is that patients suffer, get a joint replacement they could have avoided (or postponed until they are fully developed), and generally are shafted.
*end soapbox*
#pablr#medblr#nurblr#pharmblr#physician assistant#physician associate#doctor#physician#hyperbaric medicine#hbot#hbo#medicine#oxygen therapy
6 notes
·
View notes
Text
Respiratory Care: Promoting Healthy Breathing

Respiratory care encompasses a wide range of medical interventions aimed at promoting healthy breathing and optimizing lung function. From preventive measures to advanced treatments, respiratory care plays a crucial role in maintaining respiratory health and improving quality of life for individuals with respiratory conditions.
Preventive Education: One of the primary goals of respiratory care is to educate individuals about preventive measures to maintain healthy breathing. This includes providing information on avoiding exposure to respiratory irritants such as tobacco smoke, air pollution, and allergens, as well as promoting healthy lifestyle habits such as regular exercise and proper nutrition.
Early Detection and Screening: Respiratory care involves early detection and screening for respiratory conditions to identify potential problems before they progress. Screening tests such as pulmonary function tests, chest X-rays, and spirometry help healthcare providers assess lung function and detect respiratory abnormalities early, allowing for prompt intervention and treatment.
Smoking Cessation Programs: Smoking cessation is a key component of Respiratory Care, as smoking is a leading cause of respiratory diseases such as chronic obstructive pulmonary disease (COPD), lung cancer, and emphysema. Respiratory care professionals offer smoking cessation programs and support to help individuals quit smoking and reduce their risk of developing respiratory conditions.
Asthma Management: Asthma is a chronic respiratory condition characterized by inflammation and narrowing of the airways, leading to wheezing, coughing, and shortness of breath. Respiratory care focuses on managing asthma symptoms through a combination of medication, trigger avoidance, and self-management techniques such as proper inhaler use and asthma action plans.
COPD Management: Chronic obstructive pulmonary disease (COPD) is a progressive lung condition characterized by airflow limitation and difficulty breathing. Respiratory care plays a crucial role in managing COPD symptoms, optimizing lung function, and improving quality of life through medication, pulmonary rehabilitation, oxygen therapy, and smoking cessation programs.
Pulmonary Rehabilitation: Pulmonary rehabilitation is a comprehensive program designed to improve lung function, exercise tolerance, and quality of life for individuals with chronic respiratory conditions. Respiratory care professionals develop personalized pulmonary rehabilitation plans that include exercise training, education, nutritional counseling, and psychosocial support to help patients achieve their respiratory goals.
Oxygen Therapy: Oxygen therapy is a common treatment for individuals with respiratory conditions who have low blood oxygen levels. Respiratory care professionals assess patients' oxygen needs and prescribe supplemental oxygen therapy as needed to improve oxygenation, relieve symptoms, and enhance quality of life.
Home Respiratory Care: For individuals with chronic respiratory conditions, home respiratory care plays a crucial role in managing symptoms and maintaining respiratory health. Respiratory care professionals provide education, training, and support for using home respiratory equipment such as nebulizers, oxygen concentrators, and positive airway pressure devices.
Patient Empowerment: Respiratory care empowers patients to take an active role in managing their respiratory health and making informed decisions about their treatment. By providing education, support, and resources, respiratory care enables individuals to understand their respiratory condition, adhere to treatment plans, and advocate for their respiratory needs.
In conclusion, respiratory care plays a vital role in promoting healthy breathing by providing preventive education, early detection and screening, smoking cessation programs, asthma and COPD management, pulmonary rehabilitation, oxygen therapy, home respiratory care, and patient empowerment. By addressing respiratory needs comprehensively and proactively, respiratory care helps individuals achieve optimal respiratory health and improve their overall quality of life.
Get More Insights On This Topic: Respiratory Care
#Respiratory Care#Lung Health#Breathing Therapy#Pulmonary Rehabilitation#Asthma Management#COPD Treatment#Oxygen Therapy#Smoking Cessation#Respiratory Conditions#Healthy Breathing
0 notes
Text
Types of Pigmentation Treatment offered by La Midas Aesthetics
BB Glow Treatment
Cosmelan
PRP (Platelet-Rich Plasma)
Oxygen Therapy
Laser Toning
Glow Booster Therapy
Meso Glow
Pigmentation Zap Therapy
Q Switch laser
Cell Restore Therapy
#hyper pigmentation treatment#pigmentation treatment#BB glow treatment#cosmelan#PRP#oxygen therapy#laser toning#glow booster#meso glow#pigmentation
0 notes
Link
While oxygen can offer significant benefits to our cells, the risks it can bring often require careful mitigation within any form of oxygen treatment. This is where hydrogen can play a crucial role: with antioxidant properties that can neutralise some of the oxygen’s harmful species and minimise the risk of oxidative stress, hydrogen ensures that oxygen’s healing properties are maximised while minimising the risk of unwanted side effects.
0 notes
Note
Hello! I need medication for life to prevent my lungs from collapsing, this implies permanent treatment with steroids, oxygen therapy, control of oxygen in the blood and antibiotics to prevent the development of bacteria in the lungs. I'm afraid I have to insist on this because it may be the only way to get my treatment.I need medication for life to keep my lungs from collapsing, this costs around $700 per month.Things are really tough on me, I can't afford. Please donate 🖤
.
0 notes
Text
#hyperbaric oxygen therapy#hyperbaric chamber#hyperbaric oxygen chamber#oxygen therapy#musculoskeletal therapy#hyperbaric oxygen therapy price brisbne
0 notes
Note
Hello, my name is Freddy, I am 26 years old and I have Cystic Fibrosis, a respiratory deficiency that limits my daily activities.
I need medication for life to prevent my lungs from collapsing, this implies permanent treatment with steroids, oxygen therapy, control of oxygen in the blood and antibiotics to prevent the development of bacteria in the lungs.
kindly consider donating anything, donation link is available on my pinned post
hi! i unfortunately can't donate anything but i'll share your story by answering this ask! i hope you can raise enough! best of luck!
0 notes
Text
Portable Oxygen Concentrator: Deciding Between Buying and Renting

A portable oxygen concentrator, or POC, is a medical device that helps individuals with respiratory conditions receive supplementary oxygen on the go.
These small and lightweight devices are essential for those who require oxygen therapy but still want to maintain an active lifestyle.
However, many individuals face a common dilemma when it comes to POCs: whether to buy or rent one. This decision can be overwhelming, as there are various factors to consider.
In this blog post, we will explore the aspect of buying and renting a POC, helping you make an informed decision that best suits your needs and budget.
Reasons to Consider Buying a POC
Investing in a portable oxygen concentrator (POC) is a significant decision, and you can consider the following reasons to buy a POC:
Reason I: Long-term cost-effectiveness
When comparing the cumulative costs of renting a POC over several years to the one-time purchase price, buying outright often emerges as the more economical choice.
This is particularly true for those who depend on oxygen therapy daily. While the initial outlay for a POC may seem substantial, it negates the recurring rental fees, which can accumulate significantly over time.
Additionally, owning a POC eliminates the need for ongoing rental contract renewals, further streamlining the financial aspect of oxygen therapy management.
Potential buyers need to conduct a thorough cost-benefit analysis, factoring in their specific oxygen needs and projected length of therapy, to ascertain the most financially viable option.
In many cases, the investment in purchasing a POC pays dividends in the long run, not just in monetary savings, but also in the assurance of uninterrupted access to oxygen therapy, a critical component of their healthcare regimen.
Reason II: Customization and personalization options
Manufacturers offer a range of models with varying capacities, sizes, and features, allowing buyers to select a POC that caters to their specific oxygen therapy requirements. Furthermore, some models come with customisable skins or cases, enabling users to personalise their devices to reflect their style.
This level of customisation is particularly beneficial for individuals who rely on their POC daily, as it ensures both functionality and personal satisfaction with the device.
Reason III: The convenience of ownership and access
Owning a portable oxygen concentrator ensures that the device is readily available whenever needed, offering unparalleled convenience for users. This constant access is crucial for those who rely on oxygen therapy regularly, removing the hassle of arranging rentals in advance or dealing with potential delays in obtaining a unit.
Additionally, ownership allows users to become fully acquainted with their device's features and operation, fostering a sense of confidence and independence in managing their health condition.
Reason IV: Possible insurance coverages or tax deductions
Some health insurance plans may partially or fully cover the cost of a POC, significantly reducing the financial burden on the user. Additionally, in certain jurisdictions, individuals may be eligible for tax deductions for medical equipment, including oxygen concentrators. It's prudent to consult with a healthcare professional or financial advisor to understand the specific benefits you're entitled to. This exploration can reveal financial support that makes purchasing a POC more feasible.
Reasons to Consider Renting a POC
Renting a portable oxygen concentrator (POC) offers a pragmatic solution for those requiring oxygen therapy for a short period. Following are the reasons to rent a POC:
Reason I: Ideal for short-term use or travel
Renting a portable oxygen concentrator is an excellent option for individuals who need oxygen therapy for a brief period or those who travel frequently and do not wish to carry their own equipment.
It provides a flexible and convenient solution, allowing users to access oxygen therapy without the commitment of a purchase. This option is particularly beneficial for travellers, as it alleviates the need to transport personal POCs on long journeys, ensuring that oxygen therapy does not impede the travel experience.
Renting can offer peace of mind by adapting to temporary needs or holiday plans without the complexities of ownership.
Reason II: Lower upfront costs
Opting to hire a portable oxygen concentrator can significantly reduce the initial financial outlay compared to buying the device outright. This choice is particularly advantageous for individuals who may be facing temporary respiratory challenges or those on a tight budget.
By hiring, users avoid the substantial upfront cost of buying a new unit, making oxygen therapy more accessible. Rental agreements often include the flexibility to adjust the rental period according to personal needs, providing an economically viable solution for short-term oxygen therapy requirements.
Reason III: Flexibility to upgrade
Renting a portable oxygen concentrator (POC) grants users the unique advantage of upgrading to newer models as they become available. This flexibility is particularly beneficial for those who wish to utilise the latest technology in oxygen therapy without committing to a single device. As innovations emerge, renters can easily switch to a model with advanced features, ensuring they are always at the forefront of oxygen therapy technology. This adaptability is an appealing aspect of renting, allowing individuals to benefit from the latest developments in the field without the financial implications of purchasing each new model.
Reason IV: Rentals include maintenance and repairs
This provision means that users can enjoy peace of mind knowing that should their device encounter any issues or require servicing, the rental company is obligated to address these concerns at no additional cost to the renter. This benefit not only alleviates the stress associated with potential device malfunctions but also reduces the risk of unforeseen expenses related to device upkeep.
Renters can confidently use their POC, secure in the knowledge that they have support for maintenance and repair needs, allowing them to focus solely on their health and well-being without the worry of added financial or logistical burdens.
How much does it cost in Australia?
The cost of a portable oxygen concentrator (POC) in Australia varies widely based on the model, features, and capabilities of the device. Prices range from approximately $1,099 for basic models to up to $5,896 for high-end units equipped with advanced technology and greater oxygen delivery capacity.
Consider the following:
This price variation reflects the diversity in POCs available on the market, catering to a broad spectrum of oxygen therapy needs and preferences.
Prospective buyers or renters should consider the specific requirements of their oxygen therapy, including flow rate, battery life, and portability, when evaluating different models.
It's also advisable to explore various suppliers and compare prices, as some may offer competitive deals or bundle packages that include accessories and extended warranties.
Engaging with healthcare professionals and seeking recommendations can also guide individuals towards making a cost-effective choice that ensures they receive the necessary oxygen support without compromising on quality or functionality.
Where to buy it?
When looking to purchase or rent a portable oxygen concentrator in Australia, there are several reputable suppliers to consider. One notable provider is Mega Medical, known for its wide range of oxygen devices tailored to meet various needs and preferences. Beyond this, online marketplaces and specialised medical equipment stores offer a plethora of options.
Have a look at following pointers:
It's important to research and compare the services and products of different suppliers.
Many of these companies provide detailed product information, customer reviews, and comparison tools on their websites, making it easier for consumers to make an informed decision.
Additionally, consulting with healthcare professionals can provide valuable insights and recommendations based on your specific medical and lifestyle requirements.
Ensure to enquire about after-sales support, warranty options, and any additional services such as training on how to use the device effectively.
By carefully evaluating your options, you can find a reliable supplier that meets your oxygen therapy needs.
Conclusion
Deciding between buying or renting a portable oxygen concentrator (POC) ultimately hinges on your individual oxygen therapy needs, lifestyle preferences, and financial considerations.
Purchasing a POC may be more cost-effective for those requiring long-term oxygen therapy and seeking the convenience of ownership, along with the ability to customise and personalise their device.
On the other hand, renting offers flexibility, lower upfront costs, and the advantage of upgrading to the latest models without the commitment of a purchase, making it ideal for short-term needs or frequent travellers.
Whatever your choice, it's crucial to undertake thorough research, consult healthcare professionals, and weigh the benefits against your specific circumstances. In doing so, you ensure that you select the option that not only meets your oxygen therapy requirements but also supports your overall quality of life.
You have to keep in mind that the ultimate goal is to maintain your health and independence, and so select the option that aligns best with your lifestyle and medical needs.
0 notes
Text




Spending my Saturday in bed 🖤
#braced babe#med fet#neck brace#oxygen#wrist brace#nasal cannula#medical aesthetic#brace aesthetic#catheter#aspen therapy collar#oxygen therapy#braced and tubed
97 notes
·
View notes
Text
1 note
·
View note
Text

Actual photo of me in the hyperbaric oxygen. For this therapy, you enter a special chamber to breathe in pure oxygen in air pressure levels 1.5 to 3 times higher than average. The goal is to fill the blood with enough oxygen to repair tissues and restore normal body function.
It increases the oxygen supply to tissues, promotes tissue repair and regeneration, reduces swelling and inflammation, and enhances the immune system's ability to fight infection. These factors are all essential to the healing process following surgery.
1 note
·
View note
Text
Breathe In, Bliss Out: The Unbeatable Benefits of Fresh Air at Home

Hey there, cozy dwellers and fresh-air enthusiasts! In the fast-paced world we live in, it's easy to overlook the simple joys, like opening a window and letting in a breath of fresh air. Today, let's cozy up and chat about the incredible benefits of inviting the great outdoors into our homes. Spoiler alert: it's not just about getting a lungful of oxygen; it's about unlocking a treasure trove of well-being and tranquility.
The Power of Oxygen:
Let's kick things off with the OG of fresh air benefits: oxygen. Your body craves it like your morning coffee, and no, that's not an exaggeration. Fresh air oxygenates your blood, giving you a natural energy boost that even the strongest espresso can't quite replicate. So, throw those windows open and let the oxygen infusion begin!
Mood Makeover:
Feeling a bit "meh" lately? A dose of fresh air might be just the pick-me-up you need. The great outdoors is like nature's mood enhancer, releasing those happy hormones and bidding adieu to stress. It's like a magic spell for turning 'meh' into 'heck yeah!'
Beauty Sleep 2.0:
Say hello to the unsung hero of a good night's sleep: fresh air. A well-ventilated room can do wonders for your beauty sleep, turning your bedroom into a cozy cocoon of serenity. It's like Mother Nature herself is tucking you in for the night.
Brainpower Unleashed:
Need to boost your brainpower? Look no further than the sweet embrace of fresh air. Open windows equal increased circulation, and increased circulation equals a sharper mind. So, the next time you're feeling a bit foggy, step outside or crack a window – your brain will thank you.
Detox for the Home:
Our homes deserve a detox session too, right? Fresh air isn't just for us; it's a breath of relief for our living spaces. It sweeps away those stagnant vibes, leaving your home feeling lighter, brighter, and oh-so-refreshing.
Practical Tips for Infusing Fresh Air Bliss:
Daily Dose of Vitamin D: Take a few minutes each day to soak in the sun. Whether it's a morning coffee on the porch or an afternoon stroll, let the sun kiss your skin and your spirits.
Window Wonderland: Make it a habit to crack open those windows daily. Even in colder months, a few minutes of fresh air can do wonders for your indoor air quality.
Green Allies: Bring the outdoors in with some leafy companions. Indoor plants not only add a touch of greenery but also contribute to better air quality.
So, there you have it, my fellow fresh-air aficionados – the secret sauce to a healthier, happier home. It's as simple as opening a window, stepping outside, and letting nature work its magic. Your body, mind, and home will thank you for this easy and cozy upgrade. Now, go ahead, take a deep breath, and let the good vibes flow.
#restoration wellness#health and wellness#naturopathy#healthy lifestyle#wellness#reduce stress#fresh air#oxygen therapy#ayurveda#ayurvedicmedicine
0 notes
Text
Hyperbaric Oxygen Therapy Tested for Post-Covid Conditions - Technology Org
New Post has been published on https://thedigitalinsider.com/hyperbaric-oxygen-therapy-tested-for-post-covid-conditions-technology-org/
Hyperbaric Oxygen Therapy Tested for Post-Covid Conditions - Technology Org
High-dose pressurized oxygen can stress out old immune cells, leaving behind a younger, better-functioning immune system. It helped with acute COVID, and now Anders Kjellberg is also testing the post-covid method.
An example of a hyperbaric chamber. Image credit: Steve Simpson via Flickr, CC BY 2.0
You can offer your link to a page which is relevant to the topic of this post.
#Aging news#Biotechnology news#Cells#covid#Featured life sciences news#Health & medicine news#hyperbaric oxygen therapy#immune cells#immune system#it#Link#Medical devices#Method#oxygen#oxygen therapy#stress#Studies & experiments#technology#testing
0 notes
