#oestradiol
Text

#the simpsons#homer simpson#marge simpson#marge bouvier#estrogen#oestradiol#new kid on the block#S04e08
544 notes
·
View notes
Text


Photo: October 2012.
I noticed over these years that estrogen treatment also had a rejuvenating effect on me.
Photo: octobre 2012.
J'ai constaté au cours de ces années que le traitement à base d'œstrogènes à eu aussi sur moi un effet rajeunissant.
15 notes
·
View notes
Quote
After making it through perimenopause and menopause, people's mood and cognition tend to stabilise — yet oestrogen levels remain low. Why is this? For the most part, our brain will adjust to lower oestrogen levels, and many symptoms will ease. But for some women, this new normal might make them more vulnerable to neurodegenerative conditions. For instance, two-thirds of Australians with dementia are women. No-one knows for sure why that is, but one theory points the finger at oestrogen. One of oestradiol's benefits is it has a protective effect on the brain, so take it away and you might increase brain inflammation — something that's implicated in conditions such as Alzheimer's disease, Dr Gurvich says. "But this is more of a hypothesis at the moment, and an area that's really just starting to be uncovered."
Belinda Smith, ‘How changes in oestrogen levels before, during menopause can affect how we think and feel’, ABC
#ABC#Belinda Smith#oestrogen levels#menopause#perimenopause#cognition#mood#neurodegenerative conditions#dementia#oestrogen#oestradiol#Alzheimer's disease#Caroline Gurvich
11 notes
·
View notes
Text
Oestradiol gave me mood swings
Oestradiol gave me hot flashes
Oestradiol gave me period craps
OESTRADIOL MADE ME A SIZE QUEEN
1 note
·
View note
Text
Hey wait a sec are your hormone levels not supposed to vary by like 1000 over the course of the month
#like in one of the routine checkup notes it says my ''oestradiol levels are fluctuating similarly to a natal female''#uh guys what does this mean what does this mean#i know they did a bunch of surgeries on me just after i was born Down There but no one tells me what#like i was all stitches for a few years#idk i uh#there may be some major revelations coming at me over the horizon real fast i Am Not ready for lmao
1 note
·
View note
Text
uh hello friends does anyone know if having high oestradiol and lutenising hormone levels + low testosterone levels might stop me from being able to go on T??
#ftm#transgender#transmasc#trans man#medical transition#got a copy of my bloods in preperation for a private appointment#realized my oestradiol and lh levels had 'H' next to them#and like according to google im JUST within the 'normal' testosterone levels for an afab person#but my bloods still has an 'L' next to my testosterone levels#im probably getting myself worked up over nothing but still...#og post //
1 note
·
View note
Text
A new research report titled "Global Oestradiol market" successfully exhibits the complete scenario of the global and an individual analysis of the various regional segments.
0 notes
Text
hello damon, i'd like to play a game. you’ve said before that gorillaz “might be the they/them parents” yet you yourself only have one earring and it’s on the straight ear. in front of you is one month’s supply of oestradiol
102 notes
·
View notes
Text
Invisible Women: Exposing Data Bias in a World Designed for Men (Caroline Criado-Perez, 2019)
"Digging deeper into the numbers, another issue the authors completely failed to address is whether or not the drugs were tested in women at different stages in their menstrual cycles.
The likelihood is that they weren’t, because most drugs aren’t.
When women are included in trials at all, they tend to be tested in the early follicular phase of their menstrual cycle, when hormone levels are at their lowest – i.e. when they are superficially most like men.
The idea is to ‘minimise the possible impacts oestradiol and progesterone may have on the study outcomes’.
But real life isn’t a study and in real life those pesky hormones will be having an impact on outcomes.
So far, menstrual-cycle impacts have been found for antipsychotics, antihistamines and antibiotic treatments as well as heart
medication.
Some antidepressants have been found to affect women differently at different times of their cycle, meaning that dosage may be too high at some points and too low at others.
Women are also more likely to experience drug-induced heart-rhythm abnormalities and the risk is highest during the first half of a woman’s cycle.
This can, of course, be fatal. (…)
Perhaps most galling from a gender-data-gap perspective was the finding that females aren’t even included in animal studies on female-prevalent diseases.
Women are 70% more likely to suffer depression than men, for instance, but animal studies on brain disorders are five times as likely to be done on male animals.
A 2014 paper found that of studies on female-prevalent diseases that specified sex (44%), only 12% studied female animals.
Even when both sexes are included there is no guarantee the data will be sex-analysed: one paper reported that in studies where two sexes were included, two-thirds of the time the results were not analysed by sex.
Does this matter? Well, in the 2007 analysis of animal studies, of the few studies that did involve rats or mice of both sexes, 54% revealed sex-dependent drug effects. (…)
It’s a tantalising finding that inevitably leads to the following question: how many treatments have women missed out on because they had no effect on the male cells on which they were exclusively tested?"
12 notes
·
View notes
Text
okayy i'll just copy-paste it onto here cuz i don't have a scanner lol.
i used the informed consent model to start hrt for male-oriented transition at 17 and this is the info i was given by my doctor, who is a trans specialist! i figured it could be a helpful resource for transmascs/trans men/etc or even a writing resource as it goes over a lot ^_^

A Guide to Testosterone Therapy for Gender Transition
Hormone therapy can have positive and important effects on trans people's quality of life, but it's important to know about the health risks and know what to expect, so that you can work with your doctor to maximize the benefits and minimize the risks.
The purpose of this booklet is to:
Explain how hormones work
Describe the changes to expect from testosterone
Outline possible risks and side effects of testosterone
Give you information about how to maximize the benefits and minimize the risks
This booklet is written specifically for people in the FTM* spectrum who are considering taking testosterone. It may also be a helpful resource for partners, family and friends.
* FTM is shorthand for a spectrum that includes not just transsexuals, but anyone who was assigned "female" at birth and who identifies as male, masculine or a man some or all of the time, including non-binary, genderqueer and androgynous people.
How Hormones Work
Hormones are chemical messengers produced by one part of the body to tell cells in another part of the body how to function, when to grow, when to divide, and when to die. They regulate many functions, including growth, sex drive, hunger, thirst, digestion, metabolism, fat burning and storage, blood sugar and cholesterol levels, and reproduction.
Sex hormones regulate the development of sex characteristics – including the sex organs that develop before we are born (genitals, ovaries, testicles, etc) and also the secondary sex characteristics that typically develop at puberty (facial/body hair, bone growth, breast growth, voice changes, etc). The three categories of sex hormones that naturally occur are:
androgens: testosterone, dehydroepiandrosterone (DHEA), dihydrotestosterone (DHT)
oestrogens: oestradiol, oestriol, oestrone
progestagens: progesterone
Generally, "males"* tend to have higher androgen levels, and "females" tend to have higher levels of ostrogens and progestagens.
Changing the levels of sex hormone in the body will affect hair growth, voice pitch, fat distribution, muscle mass and other features that are associated with sex and gender. This can help make the body look and feel lesrs "feminine" and more "masculine" – making your body more closely match your identity.
* The binary terms male, female, masculine and feminine don't accurately reflect the diversity of trans people's bodies or identities. But it is helpful to understand how hormones work in "typical" (non-trans or cis-gendered) men's bodies, and how ostrogen works in "typical" women's bodies.
What Medications Are Involved in FTM Hormone Therapy?
Testosterone (sometimes called "T") is the main hormone responsible for promoting male physical traits. It works directly on tissues in your body (e.g. stimulating clitoral growth) and also indirectly by suppressing ostrogen production. If your menstrual periods don't stop within 3 months of taking testosterone, a 3 monthly progesterone injection can be given until the testosterone kicks in.
Assigned at birth females who have androgen insensitivity syndrome (AIS) won't get any effects from taking testosterone. In AIS, the body's receptors don't respond to testosterone (whether produced naturally or taken externally). However speech therapy, chest surgery and genital surgery can still be used in FTMs with AlS.
Testosterone can be taken in different ways:
injection (intramuscular)
skin patch or gel (transdermal)
pill (oral)
The way you take testosterone seems to affect how rapidly the changes happen.
Transdermal application causes the same degree of masculinisation as injection, but takes longer to suppress menstruation and make facial/body hair grow. Oral testosterone is the least effective and most dangerous due to risk to the liver, so is not used.
With Transdermal testosterone, the daily dosing means a more steady blood level of testosterone. With injecting there is a peak right after the injection and a dip at the end of the injection cycle. This can increase side effects at both ends of the cycle (e.g. aggression when testosterone peaks, fatigue and irritability when it dips). This can be reduced by injecting a smaller dose every 7 to 10 days, or by switching to the long-acting injectable testosterone which gives a longer plateau of testosterone lasting up to 3 months.
What's a Typical Dose?
Clinical protocols vary greatly and there is no one right type or dose that is best to use. Deciding what to take depends on your health, what is available locally, and what you can afford. It also depends on how your body reacts when you start taking testosterone.
The right type or dose for you may not be the same as for someone else. Always discuss the pros and cons of different options with your doctor and voice any concerns you have.
This table summarizes the forms of testosterone most commonly used by FTMs in Australia. You may be started on a lower dose if you have chronic health problems or are at risk for specific side effects, or have had your ovaries removed.
Forms of Testosterone Commonly Used
(note from me: use this section more as a general guide, as it is particular to aus almost 5 years ago. still pretty helpful otherwise.)
Intramuscular Injection, short-acting: Brand – Primoteston. 150-250mg fortnightly. $10. Pros – Rapid changes. Cheap. Cons – More side effects at beginning and end of cycle. More injections.
Intramuscular Injection, long-acting: Brand – Reandron. 1000mg every 8 to 12 weeks. $40. Pros – Rapid changes. More stable T levels. Cons – Not able to be self-injected (you will need to see a nurse). (i take this! it's every 15 - 17 weeks now.)
Transdermal: Gel – Testogel, Axiron. Patch – Androderm. 5-10g per day. $30 per month. Pros – More stable levels, less ups and downs. No needles. Cons – Changes take longer to happen when first starting. More expensive. Daily treatment. Risk of gel getting onto partner or pets.
Costs vary depending on pharmacy. These costs are based on PBS subsidy which assumes the person has a Medicare card. Costs are higher without this subsidy.
Every person is different in terms of how their body absorbs, processes and responds to sex hormones. Some people have more changes than others; changes happen more quickly for some people than others. Taking more than the dose you were prescribed – or taking another kind of steroid as well as your prescribed dose (sometimes called "stacking") – is not a good way to speed up changes. Taking a higher dose can actually slow down the changes you want: extra testosterone can be converted to oestrogen by an enzyme in your body called aromatase.
Taking more than your prescribed dose also greatly increases your health risks. If you think your dose is too low, talk to your doctor about your concerns. It may be better to try a different type rather than increase the dose.
Obtaining anabolic steroids through other means (such as through gyms or the internet) is a really bad idea, as these are often veterinary grade steroids which have not gone through the same rigorous quality assurance process that is applied to human pharmaceuticals, and it is very easy to overdose and cause serious liver damage. If you are taking these steroids please tell your doctor so that they can monitor your health.
If you have had your ovaries removed your body will producing a much smaller amount of oestrogen, so the dosage of testosterone is usually reduced. However you will need to stay on testosterone for the rest of your life to preserve bone strength.
What Changes Can I Expect, and How Soon?
Hormone therapy has important psychological benefits, helping to bring the mind and body closer together and easing dysphoria. People often describe feeling less anxious, less depressed, calmer and happier when they start taking hormones. For some people this psychological change happens as soon as they start taking hormones, and for others it happens as physical changes progress.
The degree and rate of change depends on factors that are different for every person, including your age and how sensitive your body is to testosterone. There is no way to predict how you will respond before you start.
Effects and Expected Time Course of Masculinizing Hormones*
Typical changes from testosterone
Skin oiliness/acne. Onset: 1-6 mth. Maximum effect: 1-2 yr.
Facial/body hair growth. Onset: 3-6 mth. Maximum effect: 3-5 yr.
Scalp hair loss. Onset: >12 mth. Maximum effect: variable.
Increased muscle mass. Onset: 6-12 mth. Maximum effect: 2-5 yr.
Body fat redistribution. Onset: 3-6 mth. Maximum effect: 2-5 yr.
Menstruation (period) stops. Onset: 2-6 mth.
Deepened voice. Onset: 3-12 mth. Maximum effect: 1-2 yr.
Clitoral enlargement. Onset: 3-6 mth. Maximum effect: 1-2 yr.
Vaginal dryness. Onset: 1-6 mth. Maximum effect: 1-2 yr.
Testosterone affects the entire body.
It's not possible to pick some changes and not others.
* Adapted from WPATH Standards of Care version 7
(note from me: the onset and "maximum effect" of these changes are not set in stone or fused to a certain timeline. after a certain period of time if you continue hrt your body will take on the characteristics of a typical cis male's and what you are genetically predisposed to. everybody's body changed as they age, like how a 20 year old cis man and his 30 year old self are wildly different, and this will happen to you too! also, for example, i started growing facial hair around 6 months, true, but i'm 5 years in now and it's only just started actually growing in properly, and that's also because i'm... 22 and not a teenager anymore, y'know? my (cis) brother's beard only filled in when he was 26, a lot of it's just genetics!)
Most of the effects of hormones happen in the first two years. During this time, your doctor will want to see you one month after starting hormones, then 3-4 times in the next year, then every 6 months. At appointments in the first two years your doctor will:
order a blood test to check hormone levels, liver function and red cell count
ask you about physical changes
ask you how you feel about the changes that have happened thus far
Are These Changes Permanent?
Most of the noticeable changes caused by taking testosterone are not fully reversible, even if you stop taking the hormone.
Irreversible: deeper voice, male-pattern baldness, facial hair, clitoral growth
Reversible: menstrual periods, muscle/fat/skin changes
The long-term effects on fertility are not fully understood. There is a chance you will be permanently sterile after taking testosterone for some time, in other words, you may not be able to become pregnant if you stop taking testosterone.
What Won't Change?
1. Hormone therapy won't solve all body image problems.
The point of hormone therapy is to make you feel more comfortable with your body which can increase self-esteem and make you feel more confident and attractive. It can be hard to separate out gender dysphoria from body image problems.
Counselling (therapy) can be helpful to sort out your expectations about your appearance, and to work towards greater self-acceptance.
2. Hormone therapy won't make you into somebody else.
Many people experience positive emotional changes with hormone therapy. But after the excitement wears off, and you've incorporated the changes into your daily life, you'll likely find that your personality remains unchanged. Whatever you see as your strengths and weaknesses will still be there. Hopefully you will be happier and more accepting of yourself, but if you re expecting all of your problems to disappear you're probably going to be disappointed.
This extends to mental health concerns as well. People who were depressed because of gender dysphoria may find that taking hormones greatly alleviates their depression. However if you have depression caused by biological factors, the stresses of transphobia, or unresolved personal issues, you may still be depressed after you start hormones.
3. Hormone therapy won't provide you with a perfect community.
For some trans people, hormone therapy is a ritual affirming that they are who they say they are. Making physical changes is a way to bring who you are to the rest of the world so that other people can see it. This process of self-emergence can be very liberating, but it does not guarantee that you will find acceptance or understanding.
When starting hormones there can be a drive to find other people who have gone through similar experiences. There are a lot of very cool trans people to talk with about hormones, but having taken hormones doesn't automatically make trans people welcoming, approachable or sensitive. Being realistic about the likelihood that you will at times feel lonely and alone after you start taking hormones is part of emotionally preparing for hormone therapy.
4. Hormone therapy won't remove all female aspects of your body.
Some physical characteristics aren't changed by hormone therapy, or are only slightly changed. This includes things that have developed before birth (vagina, chromosomes) and also physical changes that occurred during puberty.
Testosterone does make your voice pitch drop, but it does not change intonation and other speech patterns that are associated with gender socialization rather than hormones.
Testosterone does not make breast tissue go away, you will need surgery for this change to occur.
Once your bones have stopped growing after puberty, testosterone won't change the size or shape of your bones. You will not grow taller or get bigger hands or feet.
Since effects on fertility are unpredictable, there is a chance you could still become pregnant. Depending on how you have sex, you may need to use birth control.
Testosterone is toxic to the developing foetus and you cannot take it whilst pregnant.
Testosterone tends to make the vagina drier and the cervix more fragile, so if you have vaginal sex you should add extra lubricant to avoid breaking latex or tearing your vaginal lining.
What are the Possible Side Effects/Risks of Testosterone?
The long-term safety of testosterone is not fully understood. Most of the studies on hormone therapy involve cis-gendered men taking testosterone. There may be long-term risks that are not yet known.
1. Testosterone can increase the risk of heart disease, stroke and diabetes.
Testosterone tends to:
Decrease good cholesterol (HDL) and increase bad cholesterol (LDL)
Increase fat deposits around internal organs and in the upper abdomen
Increase blood pressure
Decrease the body's sensitivity to insulin
Cause weight gain
These changes may increase the risk of heart attack, stroke and diabetes. The risks are greater for those who smoke, are overweight, or have a family history of heart disease. Many of the contributing factors to these conditions can be reduced by creating a care plan that is tailored to your specific situation. Stopping smoking, exercising, eating well and having periodic blood tests are all key steps in reducing your risks.
2. Testosterone can increase red blood cells and haemoglobin.
The increase is usually only to the average male range, but a higher increase can cause potentially life-threatening problems such as stroke and heart attack.
Blood tests will check on this.
3. Testosterone can cause or worsen headaches and migraines.
If you are getting frequent headaches/migraines or the pain is unusually bad, tell your doctor.
4. Cancer risk is not significantly affected.
Breast cancer, ovarian cancer and uterine cancer are all sensitive to ostrogen, and there is evidence that some testosterone is converted to ostrogen. Studies have not however found a definite increase in rate of cancers in trans men on testosterone. However risk is likely to be increased if you have a family history of these cancers, are aged >50, or are overweight. It is important to discuss screening tests that may be appropriate.
5. Testosterone can negatively affect mental health.
In some people testosterone can cause increased irritability, frustration and anger. People with bipolar disorder or schizophrenia may be destabilized. Using daily Transdermal testosterone can help with mood swings.
6. There can be social consequences to taking testosterone.
Being visibly trans in a transphobic society carries risks. Harrassment, violence, discrimination, loss of employment, loss of support from loved ones can all occur.
Peer support and counselling can be very helpful.
7. Pelvic Pain in Trans Men.
Some people develop pelvic pain after being on testosterone for some time. This can be like period pain and can occur monthly or in a random fashion. If this happens to you be sure to tell your doctor so it may be properly investigated.
Health Checkups While You're Taking Testosterone
As long as you are taking testosterone (possibly for the rest of your life) you need to have regular physical exams and lab tests to monitor your overall health. Initially these checkups will be every few months. Expect your doctor to:
Ask about your overall health
Check your blood pressure, weight, heart rate
Order blood tests to check red blood cells, blood sugar, cholesterol, liver health and hormone levels
Recommend other tests such as bone density tests or heart tests as needed, depending on your health and any signs of problems
Routine breast and cervical cancer checks (mammograms, Pap smears) as per the usual screening guidelines (generally every 2 years)
There are some health problems that make it dangerous to take testosterone (eg uncontrolled heart disease) – your doctor will do everything possible to control the disease so that you are able to take hormones, but may need to change the dose and type of testosterone to protect your health.
Maximizing the Benefits, Minimizing the Risks
What can you do to ensure your therapy is safe and effective?
Be informed. Understanding how testosterone works, what to expect, possible side effects/risks, and guidelines for care gives you the tools to be in charge of your health and make informed decisions.
If you smoke, stop or cut down. Smoking greatly increases risks. If you are a smoker, your testosterone level may have to be kept low. Your doctor can help you to quit.
Find a health care provider you trust and can be honest with. You need to be able to talk openly about what you want, and any concerns or problems. You also need to be able to talk openly about drug and alcohol use, supplements and anything else you are taking.
Deal with problems early on. If caught early most problems can be dealt with so that you don't have to stop your hormones. Waiting can worsen your health to the point where you can't safely take testosterone.
Don't change medication on your own. Check with your doctor if you want to stop, start or change the dose. Taking more frequently or at a higher dose increases health risks and can slow down the effects you want.
Take a holistic approach to your health. Health involves more than just hormone levels.
Know where to go for help. There are peer support groups and counsellors who can play a role in assisting you.
This brochure has been modified from "Hormones: A Guide for FTMs" by Vancouver Coastal Health.
Testosterone Informed Consent Information
Testosterone treatment will cause some permanent and many reversible changes in your body. Some of these changes you may want (like facial hair and a deeper voice) but some you may not (like baldness). Before you start taking testosterone, it is important that you have a good understanding of these effects as well as the risks involved in taking testosterone. If while reading this form you have questions, make sure you discuss them with your doctor so you have a realistic expectation of what will happen and what may happen.
It is also important that you understand that testosterone is not the only way that all FTM transgender patients choose to be treated. Just as chromosomes and genitals do not define your gender identity, neither does which hormones are in your body or what surgeries you choose to have. So it is important that you decide what goals you would like to achieve in your treatment and discuss these with your doctor. Deciding not to take testosterone, to delay taking testosterone, or to take a lower dose than others are all valid choices and do not make you "less trans". Gender identity can only be determined by you based on how you feel inside, not the choices you make about your medical care.
Permanent Changes
These will not go away if you stop taking testosterone:
Will happen:
Increased facial and body hair. Not just on your face, chest and stomach. You may also get hairs on your back, buttocks, and even in your ears.
Deepened voice. How deep your voice will get is variable from one person to the next.
Enlargement of the clitoris to an average of 4-5cm (< 2 inches) after 1-3 years.
May happen:
If you have not finished puberty, you might have a growth spurt and closure of growth plates.
Male pattern baldness (may be partially treatable), genetic.
Changes in your ovaries that may make it difficult or impossible for you to produce eggs or get pregnant even if you stop taking testosterone.
Changes in your uterus (like fibroids) or ovaries (like cysts) that may make hysterectomy (removal of uterus) and oophorectomy (removal of ovaries) more difficult if you eventually choose to have these surgeries.
Rarely, benign or malignant liver tumours or other liver disease (usually only in those who take oral testosterone)
Possible but uncertain increase risk of developing osteoporosis (thinning and weakening of bones) that may become worse after ovary removal or if you stop taking testosterone.
Reversible Changes
These occur with testosterone treatment but generally will go away if you stop taking testosterone:
Increased libido (sex drive) and changes in sexual behaviour.
Increased muscle mass (especially upper body strength)
Redistribution of fat to a more typical male pattern (to the stomach instead of hips and thighs)
Increased sweat and changes in body odour.
Increased appetite, weight gain, and fluid retention.
Acne of the face, back and chest, especially in the first few years of treatment (which if severe, may cause permanent scarring).
Prominence of veins and coarser skin.
Emotional changes (both good and bad).
Worsening of blood cholesterol levels which might increase your risks of heart attacks and strokes.
Increase in red blood count (which rarely if severe and untreated can make you more likely to have strokes, heart attacks or blood clots).
Stopping menstruation (periods). This may take several months or may be immediate.
Vaginal dryness and itching that may make vaginal penetration painful.
Interference with other medications that you may take.
Worsening of or increased risk of getting certain diseases. If you think you have or are developing these diseases, it is important to tell your doctor. They can be treated and having them doesn't necessarily mean you have to stop taking testosterone: Type 2 diabetes, Liver disease, High blood pressure, High cholesterol, Heart disease, Migraine headaches, Sleep apnoea, Epilepsy
#🐾#feel free to rb#my 5 year anniversry is actually on the 31st so heh... cool#if there's mistakes uh sorry i was just copying it from photos with the iphone thing
13 notes
·
View notes
Text
98% of adolescents who started puberty suppression and subsequently hormone treatment, continued with gender-affirming medical treatment at follow-up around age 20.
In the Netherlands, treatment with puberty suppression is available to transgender adolescents younger than age 18 years. When gender dysphoria persists, testosterone or oestradiol can be added as gender-affirming hormones in young people who go on to transition. We investigated the proportion of people who continued gender-affirming hormone treatment at follow-up (approx. 3-6 years) after having started puberty suppression and gender-affirming hormone treatment in adolescence.
720 people were included in the study. 704 (98%) people who had started gender-affirming medical treatment in adolescence continued to use gender-affirming hormones at follow-up.
Age at first visit, year of first visit, age and puberty stage at start of GnRHa treatment, age at start of gender-affirming hormone treatment, year of start of gender-affirming hormone treatment, and gonadectomy were not associated with discontinuing gender-affirming hormones.
#transgender#transsexual#trans#transmed#transmedicalist#hormone blockers#puberty blockers#transition#science
24 notes
·
View notes
Text

In this photo from November 2011, I'm 43 years old, it has already been 8 years since I started my feminizing hormone treatment and 5 years since I underwent my sexual reassignment surgery in the clinic of a magician, doctor Supporn in chonburi.
Sur cette photo de novembre 2011, j'ai 43 ans, cela fait déjà 8 ans que j'ai commencé mon traitement hormonal féminisant et 5 ans que j'ai subi ma chirurgie de réattribution sexuelle dans la clinique d'un magicien, le docteur Supporn à Chonburi.
#transgender#transwoman#transisbeautiful#transfemme#male to female#dr supporn#oestrogen#oestradiol#srs#happy woman
10 notes
·
View notes
Quote
One reason for changes in mood and cognition may be wild fluctuations and an eventual permanent drop in the production of the sex hormone oestrogen. There are two main types of oestrogen implicated in menopause. The most potent form we produce is called oestradiol. It is generally made during reproductive years, and can drop by 85 to 90 per cent during menopause. Then there's a weaker form of oestrogen called oestrone, which decreases by around 65 to 75 per cent. "They both fluctuate rapidly during perimenopause, and reduce after menopause, but oestradiol reduces the most, which makes oestrone the predominant oestrogen post menopause," Dr Gurvich says.
Belinda Smith, ‘How changes in oestrogen levels before, during menopause can affect how we think and feel’, ABC
#ABC#Belinda Smith#menopause#mood changes#oestrogen production#oestrogen#oestradiol#oestrone#perimenopause#Caroline Gurvich
1 note
·
View note
Text
Turns out my doctor is extremely happy with how the transening is happening. My abnormally high testosterone is now way lower than the minimum a cis man should have, but still a little bit higher than what cis women typically have. And my already high oestradiol is now very high.
Going to wait a few more months and get another blood test done, but it looks like I may not need to take any testosterone blockers in the future. My body seems to be cooperating with what I want, even though there's no real changes yet
9 notes
·
View notes
Text
also lrb is why hypotheticals about "bathtub insulin" are wild to me bc bathtub oestradiol (& to a lesser extent bathtub testosterone) is literally a major way trans people get their hrt in this country (britain). there are a few pretty well-known homebrewers with good reputations in the trans community here and it's already a pretty normalised and accepted way we get around the state's deprivation of our bodily autonomy (as well as the exploitation of trans desperation from private trans healthcare providers + pharmacies that sell hrt online). but it's not a hypothetical; it's real and it's already here. it is not as safe as lab-synthesised hrt and any homebrewer who claims that it is is lying to you, but it can be done safely enough for the purposes of the people who need it, and it's not some absurd hypothetical for people to compound their own drugs... people already do that because the "official" channels want us dead.
5 notes
·
View notes
Text
Ovaries [Anatomy]
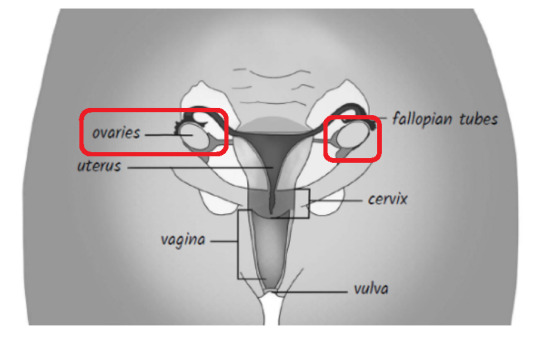
The ovaries are gonads, which are the primary reproductive organs. The male version is the testicles—the balls. Gonads have two jobs: to produce sex hormones and sex cells.
Women and other people with female sex organs generally each have two ovaries. About the size and shape of almonds—tiny considering how much work they do!—they get larger during the reproductive years and shrink again after menopause. They’re situated on either side of the uterus (a.k.a. the womb), attached by thin ligaments.
People with female sex organs are typically born with all the sex cells we’ll ever produce, while those with male sex organs continue to produce new sperm throughout their lives, although the amount and quality of sperm decreases with age.
The female sex cells are called eggs, or oocytes. At 20 weeks’ gestation—about halfway through our development as a foetus—our bodies are storing about seven million follicles that contain immature eggs. By the time we’re born, that number will be down to about two million follicles (and unmatured eggs) stored in our ovaries, waiting to be developed and released. When we start having a period we have about 400,000 eggs left. So where do they all go?
Well, the eggs we’re born with aren’t yet mature. Each month our ovaries develop the eggs we’re born with into mature eggs ready to participate in the fertilisation process with sperm—but the ovaries don’t just choose one egg to develop at a time. Initially, all eggs are surrounded by a sac called a follicle, basically a single layer of cells. During every cycle, cells will divide—so one cell becomes two, then they become four and so on—as the egg within it matures and follicles grow progressively bigger. Some follicles can’t cope with this rapid development and die off.
Eventually, one follicle dominates and a mature egg is released by one ovary each month—this is what happens when we ovulate. Just as thousands of sperm compete to merge with an egg as it travels along the fallopian tubes, a battle of eggs takes place within the ovaries to produce the fittest possible one for release. From the time we’re born our ovaries do this each month, but until we’re menstruating they don’t receive a hormonal signal from the brain telling them to release an egg, so those follicles and eggs just die. Think of it as a dress rehearsal: they’re getting ready for puberty and reproduction.
Producing oocytes, eggs or sex cells is the first job of the ovaries. Their second job is to produce sex hormones. In women and other people with female reproductive organs, the main sex hormones are oestrogen and progesterone but they also produce a small amount of testosterone.
Oestrogen is produced by everyone but is more important for women. The oestrogen produced in the ovaries is called oestradiol, and its main aim is to look after the female reproductive system, including the organs and other sex characteristics such as the uterus, vagina, breasts, hips and pelvis.
Progesterone, which means ‘for pregnancy’, prepares the lining of the womb for implantation, produces nutrients for an early embryo and prepares a mother’s breasts for milk production during pregnancy. It also influences levels of sexual desire.
Both oestrogen and progesterone play an important part in the menstrual cycle.
Pain and Prejudice — Gabrielle Jackson
#long post#Pain and Prejudice#Gabrielle Jackson#endometriosis#adenomyosis#women's health#female anatomy#female physiology#menstruation#menopause#hysteria#chronic pain#pelvic pain#autoimmune#chronic illness#perimenopause#atypicalreads#anatomy#health#sexism#misogyny#negative#female health#feminism
2 notes
·
View notes