#hemeonc
Text
im at that stage of my semi-hiatus/studying for a standardized test where im so burnt out i dont gaf anymore like my exams in 1 week to the dot and i canttt be assed to care but i still have so much to finish before i do more practice exams gawqhghshgsh
#my musings#i need tog et through renal#hemeonc#gi#msk ct and derm#and biostats and public healtht ho i imagine that one will take me 5 seconds
6 notes
·
View notes
Text
Blasts shouldn't be seen in peripheral blood.
Rule out leukemia, myelodysplastic syndrome, chronic myeloid leukemia.
Blasts may be other immature hematopoeitic cells. High monocyte count might actually be blasts, not monocytes.
If auto differential is abnormal, get a manual one.
Blasts newly elevated is more suggestive of acute leukemia. Pancytopenia suggests bone marrow failure. Febrile neutropenia is also concerning.
Make sure pt is stable with vitals, oxygen if needed, fluids.
Rule out emergencies and then contact heme/once.
APL is a subtype of AML. AML has 7 morphological categories using a system called fab. APL is the third subtype, M3. It has unique history and treatment. It presents with DIC and has early mortality. People hemorrhage and die. You can prevent it by giving all trans retinoic acid (ATRA). It helps APL cells differentiate into normal cells. APL is curable. Give all trans retinoic acid (ATRA). Diagnose by looking at source of the tumor cells. Look at peripheral blood smear. It separates ALL from AML. Auer rods are seen in AML. APL cells have multiple auer rods and folded nuclei that are very granulated.
CML has maturation of all the white cells, mature granulocytes, basophilia.
MDS (myelodysplastic syndrome) = elderly pts; hypogranular neutrophils, bilobed neutrophils, red cell shape/size changes (anisopoikilocytosis)*.
Do the peripheral blood smear first. Next do a peripheral blood flow cytometry or cell markers. It classifies cells based on the markers they express. Blasts express CD34. If CD34 is elevated, then the pt has increased blasts.
The definitive test to diagnose acute leukemia is a bone marrow biopsy. AML = more than 20% myeloblasts on bone marrow biopsy. ALL = more than 20% lymphoblasts on bone marrow biopsy.
APL has a characteristic genetic translocation--chromosome 15 and 17.
Before talking to heme/onc, also get bloodwork to rule out DIC (fibrinogen level, INR, PTT, d-dimer). If pt is febrile, work up includes blood culture, chest X-ray, urine culture for febrile neutropenia.
Also get CMP, phosphorus, magnesium, calcium, uric acid level to look for tumor lysis syndrome.
Transfuse platelets if platelets less than 10,000 and bleeding. If symptomatic anemia, transfuse RBCs.
Leukostasis = elevated WBCs such that blood flow to organs is impeded. Immature cells clog up the vasculature. Causes hypoxia, pulm infiltrates, SOB, AMS, HA, dizziness. WBC can be 50 to 100 or even less than that in leukostasis.
Other hematologic emergencies: cauda equina (spinal cord compression) is seen in lymphoproliferative disorders (lymphoma-> mass effect on spinal cord); myeloma (alters bone integrity-> compression fractures). Sometimes myeloma deposits can compress the spinal cord. So assess lower extremity reflexes, tone, Babinski sign, saddle anesthesia, rectal tone, bowel or bladder incontinence.
Top 5 clinical pearls
1) blasts are worrisome in peripheral blood, should not be in peripheral blood. Get heme/onc on board fast.
2) get a manual differential, review the film manually
3) acute leukemia can present with pancytopenia and no circulating blasts, OR with just circulating blasts. So either of those should be explored.
4) if you think the pt has acute leukemia, suspect APL, which is a medical emergency that can be treated with all trans retinoic acid immediately.
5) hematologic emergencies: severe cytopenia, febrile neutropenia, DIC, tumor lysis syndrome, leukostasis, cord compression. So screen for these.
*Anisopoikilocytosis is when you have red blood cells that are of different sizes and shapes.
The term anisopoikilocytosis is actually made up of two different terms: anisocytosis and poikilocytosis. Anisocytosis means that there are red blood cells of varying sizes on your blood smear. Poikilocytosis means that there are red blood cells of varying shapes on your blood smear.
So basically: get a peripheral blood smear, which let's you look at the cells. Flow cytometry can further differentiate the specific cell type that is elevated. Bone marrow biopsy is the definitive way to diagnose.
#heme#AML#APL#CML#febrile neutropenia#blasts#leukostasis#monocytosis#M3#leukemia#all trans retinoic acid#ATRA#Auer rods#Auer rod#hemeonc
3 notes
·
View notes
Text
Ganzoni Equation for Iron Deficiency Anemia

Use before dosing iron
0 notes
Photo

Working on the inpatient pediatric Hematology-Oncology service with my lovely colleagues, pediatrics resident Dr. Taryn Johnson (left) and child neurology resident Dr. Victoria Lorah (right) at Phoenix Children’s🩸🏥🩺 #MedPeds #IMPeds #InternalMedicinePediatrics #MedPedsResidency #InternalMedicine #Pediatrics #Residency #IM #Peds #IMProud #GME #GraduateMedicalEducation #Hospital #Medicine #Doctor #Physician #Resident #ResidentLife #UAPHXIM #PhoenixChildrens #PhoenixChildrensHospital #HemeOnc #HematologyOncology #JacksonReynolds #JacksonDavidReynolds #JacksonDavidReynoldsMD #JacksonReynoldsMD #Hematology #Oncology #PedsHemeOnc (at Phoenix Children's) https://www.instagram.com/p/CqQqW96pS-f/?igshid=NGJjMDIxMWI=
#medpeds#impeds#internalmedicinepediatrics#medpedsresidency#internalmedicine#pediatrics#residency#im#peds#improud#gme#graduatemedicaleducation#hospital#medicine#doctor#physician#resident#residentlife#uaphxim#phoenixchildrens#phoenixchildrenshospital#hemeonc#hematologyoncology#jacksonreynolds#jacksondavidreynolds#jacksondavidreynoldsmd#jacksonreynoldsmd#hematology#oncology#pedshemeonc
0 notes
Text
12th International Nursing, Healthcare & Patient Safety Conference
#CallforAbstract
Track 19: Oncology Nursing

UCG Committee invites authors to submit abstracts for the CME/CPD accredited 12th International Nursing, Healthcare & Patient Safety Conference, scheduled on 25-27, July 2023 in Dubai, UAE. For an interesting and enlightening educational experience. Interact with top speakers and researchers, and connect with colleagues from around the globe.
Note: Abstract Submission Deadline is November 10th, 2023.
Submit Abstract: https://nursing-healthcare.universeconferences.com/submit-abstract/
#oncologynurses #oncologynurse #oncologynursing #CallforPaper #Behaviouralhealth #globonc #hemeonc #Healthliteracy #Healthpromotion #publichealth #nursing #oncology #oncologist #cancerawareness #cancerpatient #oncopath
0 notes
Text
Juvenile Myelomonocytic Leukemia
Juvenile Myelomonocytic Leukemia (JMML) occurs when monoblasts start overproducing monocytes (absolute monocyte count >5000/microL). Patients present with fever, hepatosplenomegaly, lymphadenopathy, rash, and/or bleeding from thrombocytopenia due to crowding out of megakaryoctes in the bone marrow. Lab abnormalities include monocytosis out of proportion to other cytopenias, and the WBC differential includes immature and/or dysplastic cells that have been prematurely pushed out of the bone marrow. The stereotypical patient is a neonate with Noonan Syndrome or a 2-year-old boy with an NF1 mutation.
Pro-Tip: JMML can be difficult to distinguish from viral or bacterial infections, or from acute leukemia.
Source: Sivan Kassiff, "JMML/Pancytopenia," Children's Hospital of Pittsburgh Senior Morning Report (9 April 2020).
2 notes
·
View notes
Text
Introductions
Hey, so this is a new blog I’m starting up. I graduated in late May from a BSN program, passed my NCLEX in early June, and have been waiting for my job to start. I applied to many places and many different kinds of units. I went through undergrad not really finding my niche. I knew I didn’t like L&D, I love working with vulnerable populations, and I need to be kept very busy. I had attended many interviews, mostly for ICUs, but my SO of six years is getting his masters and would be placed with a hospital. This is why I applied so many places; I wanted to have an option near him. Two days after applying to the position I eventually accepted, I got a call for an interview in oncology. They had offered me a pick of any adult unit- no pedi onc for new grads. I spent some time shadowing on two drastically different units and decided that the hematology oncology/bone marrow transplant unit would be a great fit for me.
Anyways, my first day is Monday. I am nervous. My last semester I was selected out of my class with a few other students to work 1:1 with a preceptor who would help me become more independent and manage a pt workload alone, but this feels much more intimidating. I know it’s normal, but I am filled with self doubt. I was recognized by my program for providing outstanding care as a student, but none of that matters now. I’m in an unfamiliar city with unfamiliar peers. I just kinda feel alone.
#nurblr#nurse#nurse tumblr#nurse blog#hemeonc#hemeoncrn#heme oncology#oncology#oncology blog#oncology nurse#hematology oncology#new grad
1 note
·
View note
Photo
First month of fellowship ✔️ 2 weeks on the bone marrow transplant unit ✔️ 2 weeks of being on-call ✔️ • I already feel like I’ve learned so much about blood cancers and transplant. It’s been exciting and brain-exhausting, but I’m loving it. • I’m also REALLY excited to ditch this pager for the next few weeks and focus on studying for internal medicine boards. * * * * * #YesWeStillUsePagers #SomeonePleaseUpgradeUs #MDLife #DoctorLife #DoctorStruggles #PagerLife #Pager #OnCall #HemeOnc #LeukemiaAndLymphoma #Oncology #Hematology #LiveWell #CancerFree #BeatCancer #HeathyLife #HowToStayAlive
#livewell#mdlife#oncology#pagerlife#beatcancer#heathylife#doctorlife#howtostayalive#leukemiaandlymphoma#hematology#oncall#someonepleaseupgradeus#cancerfree#pager#doctorstruggles#yeswestillusepagers#hemeonc
3 notes
·
View notes
Text
Heme Onc is tough.
I wrote this after my first week in heme onc. The sadness on the floor is so pervasive, but it’s admirable how many people try to bring joy and carry on the best they can. I had to write down something to deal with the many thoughts and experiences that heme onc had generated in my mind...
I do not know what broke my heart first. Was it the yellowed man sitting up in bed, a stack of books next to him, a fruit basket crammed on the table. Next to that rests a water bottle labeled BOTTLE 2 FINISH BY NOON. A slender women, presumably his wife, is sitting in a chair next to the window. The blinds are pulled open to reveal a vast gray sky, an even drape of clouds creates a monochrome ceiling outside the fluorescent lit room. The wife is taking notes, vigorously, in a spiral notebook. The hair along the edge of her scalp is greasy enough to curl and stick to her face. She has a cardigan tied around her shoulders, she is wearing matching jewelry, but her eyes are wild and the pen in her hand is shaking. He thought he had a stomach bug 2 weeks ago at their New Years party. But he has metastatic lung cancer, clumped onto his pancreas and liver and with a haloed spot in his brain. He never smoked a cigarette.
Perhaps it was the sweet woman with dark hair and a sharp appearance, waiting outside her husbands door. “We need a family meeting today.” She too is polished, hands folded across her chest, nails done and pants with creases. But her eyes flicker too fast, she shoulders are too high.
“Yes yes” says the attending with his bowed head and compassionate nod. “We will do that. Now let’s see the patient.”
We walk into a room and are greeted by a man in restraints, his face is contorted and he growls at us. But my eyes can’t leave his neck, glittering with rows and rows of staples over scabbed gashes. As we move closer, I see the deep cuts across his neck, his arms. We lift his gown to check his abdomen where a checkered pattern of lacerations is sprawling to each corner of his torso, dappled with sutures and staples, glimmering at us while he writhes and grunts at us. The doctor gently pats the man, tells him he is doing better. The cuts are healing, but he has no white blood cells. He is psychotic, he cannot speak. The kind wife nods graciously as we leave, we will see them this afternoon to talk.
Maybe it was the man in bed, his breathing heavy, his eyes closed. A tube comes from his nose and green juice pours out of it, liters each day. He has conformed to his bed, hasn’t gotten up in days. His arms look red and puffy today. Under his gown is a similar redness, hot to the touch. It’s a new rash. It’s called as cellulitis, he is started on more medication. A plump women with freshly curled short hair sits next to him. She is enthusiastic to see us, bubbling with news to share. Her husband really wants to go home, she can tell. He also made a droplet of urine, she saw it in the bag. He doesn’t like when the nurses roll and rotate him, but oh boy he likes it when the TV is on! Her eyes glimmer. We shake his shoulders gently, we call his name. He slits open his eyes and groans at us, it’s a high pitched sound, his mouth doesn’t move and his eyes close again. “Oh he’s just a riot!” She laughs at her husbands humor, then looks at us suddenly. “He wasn’t like this at home. He never complained. I think this got him.” And tears pour out of her eyes, her forehead wrinkles and she sobs. We hand her tissues. The kind doctor tells her that her presence is indeed felt by him. He tells her we all hope for the best, but this will be a long recovery. We walk to the next one.
Or maybe it was the family hopeful that their father was stepped down from the ICU. He was breathing on his own, he was moved into his new room. But then his heart began racing, the beats were irregular, and he started to breath so fast. “Call the family” the attending ordered. He gasped for breath and the gurgles from within his chest were so loud. We all had to wear yellow gowns and gloves and masks since he was positive for a respiratory virus. We try to hold his hands with our latex hands, stroke his shoulder, but he is panicked and could only breath with all his might, fluid seeping into his lungs. He tried to pull out his cannulas, his tubes, his IV. We soothe him while holding down his arms. His eyes glaze over. We all watched the monitors, the oxygen saturation just went down and down. The family came in. They sobbed and told him it’s okay to go, it’s alright to leave them behind. He was DNR, we gave him morphine and lots of oxygen and unplugged his tubes and cords. We ripped off our gowns and gloves and masks as we left the room to see the next one. Later that day he died.
That was Day One.
25 notes
·
View notes
Photo
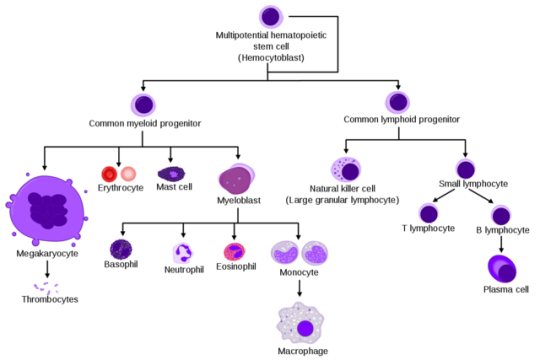
Finishing up Heme-Onc week and then it will be 2.5 weeks of neuroscience. I can’t wait to get these comp exams over with.
#medblog#medblr#med student#doctor#MD#medstuff#hematology#oncology#hemeonc#hemeoncweek#comp#STEP1#MS2#med school
8 notes
·
View notes
Text
It’s my first call shift tonight.
Please let my night be calm and my patients healthy and asleep.
9 notes
·
View notes
Text
How do you get ‘Dick’ from ‘Richard?
You ask nicely.
submitted by /u/Hemeonc
[link] [comments]
5 notes
·
View notes
Text
Nurse practitioner oncology
Come join HemeOnc and TCT learning group in Facebook, the link is here https://m.facebook.com/groups/291961305059530/?ref=group_browse
1 note
·
View note
Text
Humoral Hypercalcemia of Malignancy (HHM)
Associated with squamous cell carcinoma of the lung
HHM is a paraneoplastic syndrome that causes hypercalcemia due to the release of PTHrP by malignant cells. It acts on PTH -1 receptors and causes increased bone resorption and reabsorption of calcium in the distal renal tubule.
#HHM#humoral hypercalcemia of malignancy#paraneoplastic syndrome#squamous cell carcinoma of the lung#lung cancer#endocrine#pulm#respiratory#hemeonc#hypercalcemia#PTHrP#hyperparathyroidism
0 notes
Photo

Multiple Myeloma
youtube
0 notes
