#if you tell your psych you’re still depressed and they just increase the dose so high they don’t make the pills in that size run AWAY
Text
honestly at this point i think i’m just trying to relearn how to enjoy things
#years of way too high a dose of antidepressants has fucked up my brain so bad#if you tell your psych you’re still depressed and they just increase the dose so high they don’t make the pills in that size run AWAY#you will NOT get less depressed by taking that much you will just get permanently sick#so yeah i’m just going and throwing myself into everything i’ve ever enjoyed desperately trying to feel something again
11 notes
·
View notes
Text
I shared my personal mental health story with my vet class
I shared my very personal story with my classmates for R U OK day in our private facebook group and I received so much love and support. This is a copy of my post:
Today was R U OK day. I thought I would take this opportunity to talk about my recent experience with mental health and trying to find help. Sorry in advance for rambling. Also, just a warning that this is a pretty full on post. I just want to share it because mental health is something that most vets and vet students will struggle with at some point. It is important to know that you’re not alone and to speak up if you think it might help someone.
A few months ago, I had suicide ideations. I knew I had to go to the hospital to remain safe. Starting that conversation with my mum was one of the hardest things I have ever had to do. I have attempted suicide in the past and my partner at the time convinced me to tell my mum, who reacted very badly. She didn’t understand depression or anything like that at the time and her mind went straight to my brother who died when I was younger. He had been in a car accident and spent his 19th birthday on life support before it was switched off. My suicide attempt brought all that back for my mum and she yelled, “How DARE you?! Your brother fought as hard as he could for his life and you just want to throw yours away?!”
The second reason I was scared to get help, was the way the mental health nurse in Armidale treated me last time. She did not appear to care at all and clearly didn’t believe me when she asked if I had been sexually assaulted as a child. She asked me that same question several times and then made a face when she finally wrote my answer (”no”) on her clipboard.
Thankfully, this time my mum and the hospital staff were much more supportive.
I was admitted to the low care mental health unit, which is a locked ward. It is a secure and safe place but it did nothing to actually help me mentally.
The first thing that I was required to do, was very confronting. The mental health nurse that I was assigned to, along with a student nurse, led me into a conference room to meet with the psychiatrist. There was also a psychiatrist registrar and 2 other students in the room. 6 strangers. We sat in a semi circle and everyone looked at me. I couldn’t make eye contact but I knew some people had their hands posed, ready to write or type. The psychiatrist asked me why I was there. I thought it was pretty damn obvious why I was there. I had already been interviewed by about 5 nurses who kept repeating the same questions. Surely someone had passed along the message. I mumbled that I wanted to hurt myself.
“Yes. And when you say you want to hurt yourself, what do you mean exactly?”
I told them that I wanted to end my life. He still wasn’t satisfied. He wanted to know all of the details. How. With what. When. How far into my plan had I got? So I tried my best to answer his questions while my answers got scribbled and typed down.
After that, I assumed I would be bombarded with help. Pamphlets for programs, mental health workers, counsellors, support programs, group therapy, art therapy.... but there was none of that.
The psychiatrist told me he would increase the dose of my anti-depressants to see if it made a difference. My nurse and the student nurse took me to my room. I had been scanned by a metal detector and had my phone taken away when I arrived. Everything was secured into place to prevent us from hurting ourselves. No electrical items were allowed inside. No shoelaces. No belts. No aerosols. We weren’t even allowed to keep shampoo in our rooms. There was hot water for de-caffinated tea. A sandwich press was brought out at breakfast for making toast and then locked away again.
My nurse asked if I was anxious (lol) and gave me some pills. I didn’t ask what they were. I went to sleep until someone woke me for dinner. I had a new nurse. Another consumer (that’s what they call patients in the ward, consumers) gave me a whirl-wind tour of the facility, not that I can even remember what her voice sounded like, I was too out of it. But I did learn that there is a whiteboard in the nurses station that has our room number, name and our nurses name on it. There were about 4 nurses on at a time and we had to go to them for every little thing. But they changed shift regularly, so if you had to arrange something like a CSU medical certificate, it was hard because once you got somewhere with the last nurse, you had to explain the whole thing over again to the new nurse.
They checked on us every hour. All through the night. It wasn’t very dark in my room but each hour a blast of fluorescent light invaded for a few moments, disrupting whatever sleep I had managed to find. The night staff started at 10pm and from then on, you could get sleeping pills. They helped a little.
I was woken early the next morning by a nurse who seemed to be running behind schedule. She didn’t wait for my eyes to adjust to the light, let alone for my brain to remember where I was before rolling down my sleeve.
“Just taking some blood,” she explained hastily.
“Oh, I had bloods taken yesterday.”
“Yeah, I can see that,” she replied, ripping the tiny, circular band-aid off.
Each morning, we were woken at 7 for breakfast, medication and we had our temperature and blood pressure measured. I don’t know what their obsession was with blood pressure but mine was measured several times each day. After breakfast, there was nothing to do. We could watch TV, colour-in (if we asked our nurse to get us the pencils etc) or we could pace the hallway. I just went back to bed and reassured the nurses each hour that I wasn’t dead. Eventually, it would be time for me to see my psychiatrist registrar. This was the only mental health care we received. He would ask how I was feeling, enquire about my appetite (nil), sleep (disrupted) and asked if I felt safe in the ward (I still don’t know if he meant safe from myself or from the other consumers but I just said yes each time).
On my first morning, my nurse brought me a bunch of paperwork to sign. She explained that I was an involuntary patient. Two days later, I told my brother that I still had no idea what I was supposed to DO in the ward. There was no stimulation whatsoever. It was just me and my own mind. And the nurses kept asking if I was hearing voices so many times that I actually started to question myself. My brother, who had been visiting me daily, asked my nurse how long I was going to be there. She explained that my psychiatrist would review me in a week. A week!!! A different psychiatrist comes each weekday (from Sydney or Melbourne) and the psychiatrist registrars communicate with them throughout the week. The registrar can grant leave for an hour each day but only once you’re a voluntary patient. Only the registered psychiatrist can formally discharge consumers.
The days dragged on after that. I was made a voluntary patient a few days later and the nurse brought me my new paperwork to sign. It turned out that the only real difference between voluntary and involuntary was that they could no longer give me ECT (electroconvulsive therapy) without my consent. So that was a plus. And yeah, they still do that. But it’s now done under anaesthetic. My ex used to complain about all the old people who get it done because their heart rates would suddenly shoot up dangerously high and sometimes it caused strokes.
The psychiatrist registrar asked how I felt about the prospect of returning home. I told him that I didn’t really care where I was but my family wanted me to have a plan and ongoing support. I also wanted to be connected with a counsellor or psychologist before I went home. The registrar and the nurses told me all of that would be arranged before I left.
But it wasn’t. I was discharged the day before my psych was due to see me and it all happened really quickly. I suspect it had more to do with the number of beds rather than an actual improvement in my mental health. Nothing had actually been done in the week I was there except for an increase in my anti-depressant dose. But I was so overwhelmed at the thought of being able to walk more than 10m without turning around and getting to see my animals that I didn’t think to ask about the support I had been promised.
They did put me in contact with a community health worker. I saw her once a week and she asked how I was sleeping, appetite, whether I had self-harmed etc. I told her that I wanted to see a psychologist and she said that was a great idea. She didn’t offer any further assistance. When I questioned her about it at our next meeting, she said that I needed to talk to my GP about getting a mental health plan. Her tone sounded impatient, as if I should have known that already. I started to get angry with the whole system. It had been three weeks since I had walked into the hospital and told them I wanted to kill myself and it still seemed so hard to access any help.
Two days later, I attempted suicide.
This time, I actually tried the method Leigh Ladd mentioned in class the other day - diazepam and alcohol. I had planned to get into the backyard swimming pool for good measure, but I didn’t make it that far. I actually felt validated for the first time when Leigh Ladd talked about this in class. Until then, all of the medical professionals had scoffed at my method and made remarks like, “Ha, that was never going to work. You could take 2000mg of valium and all you’d do is fall asleep.”
Maybe they were ignoring the fact that mixing it with a lot of alcohol depresses your respiratory system, maybe they didn’t hear the part about the swimming pool or maybe they were just trying to talk me out of trying it again, but it just made me feel like a complete idiot.
I woke up in the emergency room, crying and hugging my sister. My memory is very patchy due to the benzodiazepine-induced retrograde amnesia. I had a big bandage on my wrist from where I had self harmed. I don’t remember doing that but I think it was to distract myself from the mental pain during my attempt. My sister later told me that her and my mum had to leave the room when the doctor sutured my arm. Apparently, they didn’t give me any local before suturing it and I was screaming in pain for them to stop. I’m glad I don’t remember that at all.
I was taken back to the low dependency unit and back talking to a psychiatrist. This time, it was a woman. I expected to be spending another week in the unit but one of the first things this psych asked me was about going home. Apparently they didn’t want to “institutionalise” me. I spent just 2 days in the ward.
My family were looking into any and all kinds of programs for me to get help. I asked the registrar psychiatrist about any recommendations. He said there were programs but they were expensive if you don’t have private health insurance. He didn’t elaborate. A nurse signed my family up for some carers help program. They also referred me to a program called Wellways, which is about suicide prevention. Turns out that the only people who can be referred are those who have actually attempted suicide, not just thought about it, which is why I hadn’t been eligible before.
I was eligible for help from Wellways for 3 months. They could refer me to further help if I needed financial counselling, emergency accommodation and things like that. But not counselling or anything.The lady who I dealt with only worked 2-3 days a week and I didn’t find the program helpful at all.
My family were disgusted with the lack of help I got. My sister talked to some people at her work (in community health) and gave me the names of 2 private psychiatrists. I saw my GP and arranged referrals but they were booked out for months. One of them was finally able to fit me in earlier after I pleaded with the receptionist. It cost $800 for the appointment (I could reclaim some of that on medicare but I’m forever grateful that my family were able to lend me money). I wasn’t impressed with what I got for my $800. He asked why I was there. I told him my story and he asked why I had attempted suicide. I told him that I didn’t want to live anymore (it rolls off the tongue more easily the more you say it) but again, he asked why. Every answer I gave him, he said, “But why?”
I left with a script for a new medication that was supposed to help me sleep but has actually given me nightmares and made my sleep pattern worse. It’s also not on the PBS and costs a lot of money so I’m weaning myself back off it. When I told the community health worker about seeing the psychiatrist, she seemed annoyed that I had gone behind her back to get help and told me that there were community health psychiatrists who are very good at what they do. She asked me to get the private psych to forward her his notes. I would have gladly seen a free or cheaper psychiatrist but that was the first (and last) that she mentioned their existence. I again told her that I wanted to be connected with a psychologist and she basically told me to keep her in the loop if I make any more appointments.
I went back to my GP and asked for a referral to a psychologist. But when I rang to book an appointment with the one he recommended, the receptionist told me they no longer work there. They booked me in to see someone else. I was just happy that I was finally going to see someone who might actually help. I have seen her 3 times now and she is really lovely. I complained to her about my GP (I left those details out of this post because it’s already too long!!) and she gave me the name of another doctor that I have started to see. This new doctor is much more understanding and has been doing further tests to see if I have any underlying health problems. I’m now getting cosmetic injections to improve the appearance of the scars on my wrist, I’m getting an iron infusion for my anaemia and she is helping me combat my anxiety as well.
This is the first time in months that I can see a light at the end of the tunnel. I’m finally working with a psychologist and I’m willing to try anything. Over the summer, I’m hoping to do an 8 week recovery program. I’m also hoping to do some equine therapy in the future. The most important thing for me, is that people are finally listening.
I’m sorry that this is so long (and a bit confronting) but I didn’t want to censor it. I want people to know how hard it can be to get help. There are so many ads on the TV etc about getting help for depression but I swear most of their money must go into advertising and paying admin because finding actual help was so much harder than I would have imagined. I want people to know how long this road is - because one day you will probably have to be there for a friend, family member or yourself - and it’s not just a matter of making one phone call or having one conversation. It’s an ongoing process and it’s difficult. Some people who work in mental health are complete dicks and they just don’t get it.
Don’t be scared about saying the wrong thing to a friend/family member. I don’t remember what my friends/family said to me - I just remember that they were there. That was the big thing, having my family supporting me and forcing me to keep seeking help even though I wanted to give up.
Please be there for your loved ones. And please feel free to come talk to me, even if we have never spoken before. Struggling with mental health isn’t something that I’m ashamed of (anymore). Hopefully sharing my story might help someone else, somehow.
I received so many private messages from people who shared their own stories and offered support. These were the comments left on my post:


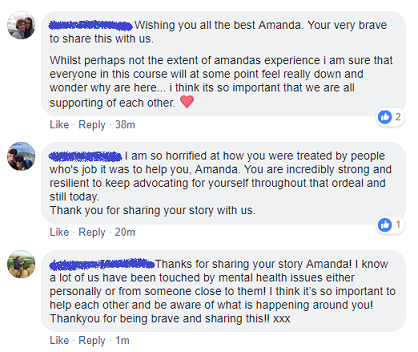
I'm a shy person and did not expect that kind of response. It is amazing how many people really do care and are more than willing to offer support ❤❤❤
82 notes
·
View notes
Text
Chronic Fatigue Syndrome
Even though I’m not sure if it’s going to do any good, I’m thinking of going back to my PCP and seeing if they’ll be open to exploring a diagnosis of chronic fatigue syndrome for me. I’ve been dealing with vague aches and pains and lack of energy on and off for years now, and it’s always been explained away by some other condition. At one point it was related to my allergies, and dosing on Flonase helped a lot. At another time it seemed to be a Vitamin D deficiency, and I was given vitamins that seemed to help me for a while. I’ve been checked for anemia and thyroid problems, and all tests have come back normal. I don’t have high blood pressure. I even thought it might be PCOS, and I had an ultrasound done on my ovaries and all the results- thankfully- came back normal.
So, what’s wrong with me? I’ll feel like I’m coming down with a cold, replete with mild sinus/head congestion, aches and pains, and an overwhelming desire to sleep. Sometimes I feel like it might be all in my head, a side effect of my depression and anxiety. When I look closely, however, there has been some physical exertion beforehand. The main marker of chronic fatigue syndrome is that you’ll be profoundly fatigued from what should be considered normal activity.
Case and point, driving to my mom’s house. It’s only a two-hour drive there and a two-hour drive back, but just getting there seems to take so much effort sometimes. So much so, that I rarely travel there and go back on the same day; I stay overnight. Also, when I went there and did the birthday party for my niece- which, was extremely enjoyable for me- I felt tired for days. The trigger of my current fatigue was an 8-hour shift at my job on Saturday, followed by a trip to the laundry mat on Sunday. After the 8-hour shift I slept for 14 hours, and last night I slept more than 10 hours, followed by a 3.5-hour nap today.
The kicker? I still feel tired.
An additional sign of CFS is not feeling rested…after resting. They are required to do tests to make sure it isn’t caused by a virus or some other underlying condition, including depression. CFS can cause depression, though, so this makes it extremely difficult to diagnose. The doctors must figure out whether the symptoms of CFS are really caused by the depression, or whether the chronic fatigue makes people depressed. Not being able to work or do other activities for as vague and undefinable a reason as just “being too tired” can be extremely stressful and frustrating, but at the same time depression by itself can be so discouraging that you can easily become too tired to function.
One marker that can help with diagnosis is that many other conditions that cause chronic fatigue can be improved by vigorous exercise a few days a week, whereas vigorous exercise makes chronic fatigue syndrome worse. People with CFS will exercise and instead of getting that “runner’s high” and all the good endorphins, will simply feel exhausted for days. I’ve experienced this to a certain extent, but not consistently. Sometimes exercise does pep me up, other times it just makes the other tasks I need to do even harder (note: mild exercise does seem to help when I can manage it).
That’s another fact about CFS- it can come and go, but generally it should last for 6 months or more before it can be diagnosed. I haven’t tracked it enough to see exactly when the symptoms began and ended. Sometimes my mood can increase without a corresponding increase in energy, but of course if you’re happy you tend to have a little more energy, so I don’t know for sure. I figure that these are things that I can discuss when I go to the doctor.
Ideally, I’ll be able to get up in time to make my appointment, but with the way I’ve been feeling I really don’t know. A huge part of getting a diagnosis for me is having legal standing if I need to ever defend myself regarding my missed work/activities. I guess just having schizoaffective disorder and taking psych meds could explain the fatigue to some extent but having a formal diagnosis of CFS could help me to get more treatment covered by insurance, although there is no specific treatment for CFS.
My boyfriend told me today “You are worth more than the labor you can put out, more to me than words can even describe” and that meant so much to me. I do my best to show up and work hard, and sometimes because of the nature of this illness I feel like I’m weak for not being able to just “suck it up” and “push through.” I would be so happy if this were just something that I could treat with a specific diet or treatment plan, but like I said, there is no specific treatment for CFS- assuming that is even the cause of these mysterious illnesses. We did have some weather changes, which typically do make it much worse for me, but that still doesn’t explain the underlying cause.
I don’t know if anyone will see this and respond, but if you do, please tell me about your experiences. This is unexplored territory for me and I would love to have some input.
#chronic fatigue syndrome#chronic fatigue#cfs#getting diagnosed with chronic fatigue syndrome#diagnoses#i feel tired all the time#always tired#exhausted#fatigued all the time
4 notes
·
View notes
Text
so uhh chaboy is...... having a real bad time
SO the backstory is that among various other maladies i have been working for Several Years on trying to combat the combination of depression and narcolepsy that makes me physically exhausted at all times and keeps me from performing basic maintenance of my physical form, let alone doing any of the things an adult in a capitalist country needs to do.
so in our monthly gambit to trick my body into Cutting That Shit Out, my psychiatrist recommended that we drop one of my current medications (which may be causing weight gain and tiredness) and increase the dose of my narcolepsy meds to compensate. which i’m excited about! i’m willing to try anything that might give me even a tiny bit of energy, i’m dying squirtle
HOWEVER the pharmacy refused to fill the script for the increased dose, because even though i’m already on the damn medication, they need a prior authorization from my doc to get the increased dose. which is bullshit, but whatever, i don’t make the rules, so i call my psych and tell her i need a prior auth.
and i hear. Nothing
so i call again a few days later and leave a slightly bitchy message, and almost immediately get a call back from her secretary saying they tried to call me back day of but my voicemail wasn’t set up, and anyway since my sleep doctor is the one who originally prescribed the narcolepsy meds he’s the one who’s gotta give the prior auth.
which. okay. first of all. i immediately have my mom call my phone and successfully leave a message in my very-much-set-up voicemail box. so there’s fuckin that. but more importantly my sleep doctor is kind of a dick who doesn’t listen to a word i say so i’m not excited about calling him. But. I want to be able to shower and do laundry. so i suck it up and i call his office and leave a nice message about how my psych recommended a dose increase, and i’d REALLY LOVE IT if he could just call that into the pharmacy please, but i understand if i need an appointment, just give me a call back and we’ll work it out.
and iiiiii call again two days later when i dont hear a fucken peep
and meanwhile im off the med she recommended dropping, which was a boost for my antidepressant, and without the corresponding increase i am Suffering in a way i haven’t in a couple fucken years. but i don’t hear a Goddamn Peep from the sleep doctor. I have my parents call my phone from a billion different sources in a billion different ways, so that’s not the Fucking problem. so finally i call the psych again and say Hey, we’re probably going to be switching sleep doctors because he won’t Fucking call me, what should i do in the meantime?
AND I HEAR,,, UHHHHH,,,,, NOTHING?????
SO. that was yesterday. so today i called the sleep doctor and went through to the receptionist like. Hi :’) I’m Just Wondering If You Got The Messages I Left Two Times Last Week :’) What’s Up and she looks through her files and is literally like. ‘huh. well it looks like your request went through but i don’t have any record that your doctor filled it, that’s weird’ and i’m over here like 8′) OH. NICE. GREAT.
and the other Nice and Great thing is that my parents, who are lovely and supportive people, still..... they uhhhhh........ like. when i say ‘i literally cannot do this thing, i am too exhausted to stand for any period of time’ they’re like Yeah We Understand You’re Sick. Until. The thing needs to get done???? and then they’re like. welp, nothing else for it, you’ll just have to do the thing! and like. IF THE THING BEING NECESSARY. GAVE ME THE ABILITY TO DO THE THING. I WOULD HAVE DONE LAUNDRY A FULL WEEK AGO MY DUDES.
so uhhhhhh That’s Where We’re At Atm. thanks for reading and uhhhhhh kill me maybe
#mental illness#health#ask to tag#i kind of..... can't overstate how bad i feel rn#i just.... i don't Fucking understand what the fuck's up w/ my sleep doctor. i am feeling angry
1 note
·
View note
Text
lude-n-lascivious replied to your post:
Ok so here’s the thing about my Mental Illness™...
I’ve been there. I’m there now. I am only guaranteed one day a week, sometimes I work more. My grandma doesn’t understand why I can’t get a second job, because I’m basically on call for the first. I really don’t want to burst your bubble. But sometimes, psychiatric help doesn’t help. There’s no magical pill that’s going to make it go away. If anything it just causes more problems. I was on medications for 15+ years and I only got better when I quit them.
I’ve done my psychiatric nursing rotation. I know all about psych meds. lol
It’s a long and complicated process. You’re right - there is no magical pill to make it all better. Most of the time it’s a delicately concocted dosage of multiple medications all mixed together. It takes weeks for it to work, if it works, and then like all things there’s tolerances that can build up and adjustments that need to be made accordingly and then that week long process of waiting for the meds to work right is reset every time the dosage changes. What worked one time might not work ever again etc. etc.
It works for some people, it doesn’t work for all people. Some people swear by their medications, for some people it really does work. Others, like you and I, perhaps aren’t so lucky. Maybe we’ve just not found the right balance of the right ones. Maybe our body’s makeup just doesn’t care what we want to do.
I’ve tried three different meds in the past. Mind you - I suffer anxiety and depression. I told my DR about the anxiety. NOT the depression. I was too afraid to. This was my error.
WHAT SHOULD HAVE HAPPENED: I should have told him about both. I should have been given a SSRI/SNRI combination to tackle BOTH disorders simultaneously.
WHAT ACTUALLY HAPPENED: I told him about the anxiety. I was given one SSRI to combat the anxiety. During the 2-3 week adjustment period (in which the med starts to build up and the brain starts to go WE’RE UNDER ATTACK) my anxiety was being handled by the med but my depression spiked because before the anxiety and depression worked as a team to run my brain but now the anxiety was shoved into the corner by the med and my depression got control. I stopped taking the med during this period because my suicidal idealizations naturally increased. So I told the DR. He switched my med to another SSRI. This time the reverse happened. Depression was kicked in the balls by the med but my anxiety (and trichotillomania which is a product of my anxiety) got worse (and I was bald). So I stopped taking that med. I told the DR the med wasn’t working. He gave me a third SSRI. I tried it - a few days later my body felt like I was burning from the inside out and it was made worse by laying down. I thought I was going into like toxic shock from the meds, which psychiatric meds have HORRID side effects that will permanently affect you, and I knew this, and I am a hypochondriac, so I almost ended up in the ER at 3am. But I didn’t. And when the med left my system because I skipped the next dose I told my DR. I was told not to take it anymore.
So what was my next option? My ins. would only cover one more SSRI before I’d run out of options. But after that episode I was too scared to try another one. So really, I was screwed.
NOW - what needs to be done is this:
I’ve tried controlling my mental illness without medication. I can’t do it. I might get slightly better for a week or two but then it comes back full swing and Hello Lethargy My Old Friend, How’s Suicidal Thoughts Doing Is He Coming? (by fall out boy)
But I need more options. I need a PSYCH doctor (not my family practitioner) and I need to TELL THEM whats wrong with me. I can’t skip over the fact I have depression because I’m scared of the “well do you have suicidal thoughts” exam that follows that statement. Because the truth is I need a cocktail to control this. Not just one type made for one of my problems. I need to be more truthful and they need to be more knowledgeable and I need to have affordable access to this help.
Or maybe, if the medication route genuinely doesn’t work for me, I still need some sort of professional help to guide me into being alright. Because, like I said - I can’t do this on my own. I’ve tried. It’s not worked.
So yeah, I know the meds can be nasty. I know it’s a challenge to get them to work. I know that they’re not going to work for everyone. But I also know I can’t function on my own the way I’m going. I need to try to do something about it.
1 note
·
View note
Note
mom are you okay?
Hey bby!
The short answer is yes, I’m okay, just really bogged down with course work and life!
But I also want to give a longer answer/what’s been going on in my life because I like to be honest and open about the stuff I go through, since I think that’s more helpful to me and to my kiddos, so you guys know that no one has a perfect life and that struggles don’t mean you’ll never feel okay again.
The main reason I haven’t been on is because I have no time, or when I have a bit of time I have no energy thanks to grad school. It’s really demanding and, as much as I love it, I sure miss being able to pop on and answer questions regularly! :(
But some other stuff has been going on, too, that also makes it even more difficult for me to find the energy/time to answer asks and write anything that isn’t for school, STCNTA, or one of my other Hamilton mini-series.
Around December my therapist and I decided to increase the dose of the medication I’m on because I was feeling depressed. By the time it reached full effect I was even more depressed, and we became worried that the medication was causing my depression (I’d started it for anxiety, but it works for both).
So my therapist told me I should see a psychiatrist, since psychiatrists are better able to monitor psych. meds than a primary care doctor. I recently did just that (that’s why I was making those phone calls... oh how I hate phone calls to offices!!) and am in the process of switching over to a different medication that will hopefully still work for my anxiety and not make me depressed/worsen my depression.
I wanted to tell you kiddos this because there’s no shame in it. For the longest time I have felt ashamed and that’s made it all worse. It doesn’t mean it’s easy now–– my anxiety is way higher because of the change in meds (which is to be expected)–– but why make something that’s already difficult to go through even worse by adding shame into the mix? There’s just no need.
So this is to all of my kiddos who also have mental illness(es). Please get all of the help you need. Make sure you find a good therapist, and if they recommend adding a psychiatrist to your team, listen to that advice. Your mental health is just as important as your physical health and you deserve to feel healthy and happy.
I love you kiddos so much. You have given me so much strength, especially through these darker times. I need to get back to my homework now, but if you guys have any questions do feel free to send them in as long as you’re okay with waiting for a response! I’m hoping to answer a bunch over my upcoming winter break.
Keep on being your beautiful selves, bbys! I love you!!!
30 notes
·
View notes
Note
Hey, so I got diagnosed with EUPD and ASPD yesterday and I don't really know how to come to terms with it. I saw Danny has BPD/EUPD and was wondering if you've tried DBT yet? I'm on the list and really freaking out about it. Also, what mess have you been put on? I asked them for sleeping pills cause I really struggle sleeping but they refused to give it to me. Idk what to do, can you help me?
Person talking about the EUPD - I forgot to add, I also got diagnosed with depression and anxiety - is this normal? I’ll be honest, I don’t know how to feel about the diagnosis so wanted to know how you’re getting on, I guess. So yeah, thank you guys.
Hey!
Welcome to the BPD/EUPD club!
I’ll be honest, I never really understood why I was diagnosed with BPD until I read up on what it actually is. Mind and the Royal College of Psychiatrists both have a good section on BPD/EUPD which is worth a read if you get the chance. I was suggested to read these by the psych I was diagnosed by as it would supposedly help me figure things out and understand what I’d been diagnosed with better. If you’re interested, the links I was given are here:
RCPsych‘Personality Disorders’‘Personality Disorder Facts’
Mind‘Borderline Personality Disorder’
Okay, onto the questions!!
Q1. DBT
The simple answer to that is no. I’m still on the list and have been waiting since the end of January this year which is when I was diagnosed with BPD.
Just for you guys who don’t know what DBT is, it’s dialectical behavioural therapy, which is a therapy usually used to ‘treat problems associated with borderline personality disorder’ and works on both behaviour (like CBT) and accepting who you are, apparently.
See more HERE
Q2. Medication
Back last year, I think it was January sort of time, I was put onto Citalopram (I can’t remember the mg) and was on that until around October time, increasing the dose every couple of months I think (dates aren’t any good for me so don’t expect much) when I was switched to Sertraline 50mg, and am now on 150mg of that, but knowing my doc, when I go back in a few weeks, he’ll switch them once again, so lucky me..
All I’ve been on is antidepressants so far, but I’ve heard mood stabilisers are better for BPD rather than antidepressants. I don’t exactly know why this is, and haven’t got any experience of them to share, but from what I heard, they are better with dealing with the ‘emotionally unstable’ part of the disorder and help to well, I guess stabilise your mood. According to Mind, they also help with any psychotic symptoms. It would definitely be worth possibly talking to you doc about different medications they would suggest for you and what they feel is the best option for you and your diagnosis.
Here is some info from Mind on mood stabilisers, hope this helps!
Q3. The issue of the sleeping pills
You’re not the only one which won’t be given sleeping pills. I think doctors are reluctant to give sleeping pills to those with BPD purely because of the impulsive side to the disorder.
For me, my doc/psych won’t give me sleeping pills because I have a history of ODs, which of course, hasn’t helped my case trying to get medication. I think that’s a worrying side to BPD, you know, the impulsiveness, which means GPs are reluctant to give them over, especially if you are under 18.
I think it’s definitely worth trying to talk to your doc about the sleeping pills, but maybe it’s also a good idea taking another adult with you and tell the doc that they’ll keep hold of the meds for you. I know that’s what one of my friends have had to do, so it’s an option you could consider too.
Here are some sleeping techniques which may help in the mean time:
a) breathing exercises from Dr Weil - [HERE]b) Meditation works wonders when trying to sleep! You can find videos/audio online which can assist you with this!c) Hypnosis can be another suggestion which helps me and my friend, and you can find videos/audio online, like the meditation.
One hypnosis video that both me and my friend use are the ones from LiberationInMind which helps you to relax your breathing before starting the hypnosis and actually really helps us to sleep, so hopefully that can help you too!
Another are some apps (I don’t know if they’re available on the Apple Store as I have an Android phone) such as ‘Sleepo’, ‘Sleep Sounds’ and ‘Atmosphere’ which all allow you to create your own relaxing mix to help you sleep, and includes lots of nature sounds which I love!
Q4. Other diagnoses alongside BPD/EUPD
Like you, I am also diagnosed with depression and anxiety, as well as mild PTSD (but that’s nothing to go into here), and I think if you’re diagnosed with BPD, you’re likely to be diagnosed with those two too, well, from my experience anyway. Lots of the people I know with BPD have these diagnoses too. I would say it’s completely normal to have several diagnoses and I wouldn’t go worrying about it, but if you are, definitely try to talk to your doc or a psych about it if you’re able to, as although they can be pains in the ass sometimes, they are ultimately there to help you, so make the most of that.
One more little thing!!
‘I Hate You, Don’t Leave Me’ is a book based solely around BPD, which I admit, I haven’t read yet, but it’s on my list to read and it has very good reviews.It’s suggested for many with BPD and lots of people I know both with and without BPD have recommended it, so that’s another thing too.
I really hope I was able to help and sorry it took so long to reply to your message!
If you want to talk more, I’m here and so is Daria, so just drop us a message.
Have a great day!
- Danny x
#oh jeez that was long#bpd#eupd#mental health#borderline personality disorder#emotionally unstable personality disorder#dbt#therapy#tw: overdose#depression#anxiety#sleeping tips#breathing tips#DJ#medication
0 notes