#MEN2A
Photo
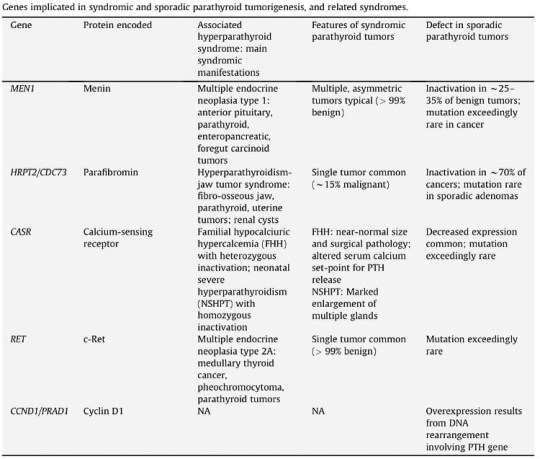
Genetic syndromes that have reported an association with parathyroid cancer cases include hyperparathyroidism-jaw tumor syndrome (HPT-JT), MEN1, MEN2A, and isolated familial hyperparathyroidism. https://doi.org/10.1016/j.beem.2010.01.003 (at Mount Sinai Medical Center of Florida) https://www.instagram.com/p/Cf-ig_gtTU2/?igshid=NGJjMDIxMWI=
0 notes
Text

No text posts we vent like men
#this isnt even all the problems i have#its just what i could remember offhand#honestly im surpised im still functioning lol#the past three years have been rough#funny#memes#meme#comics#funny comics#illness#autoimmunedisease#disease#diseases#costrocondritis#lupus#scleroderma#sacroiliitis#limbus vertebrae#back problems#MEN2a#thyroid surgry#thyroid problems#cancer#cancer survivor#medicine#medical#medical stuff#medical tumblr#myositis#rheumatoid arthritis
11 notes
·
View notes
Photo
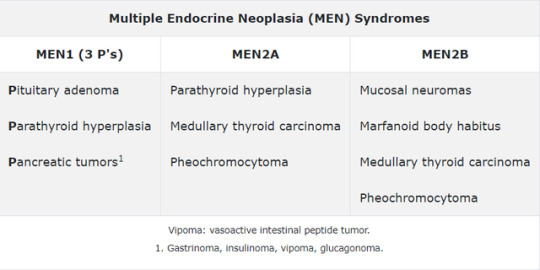
Bottom Line: Multiple endocrine neoplasia type 1 consists of the three P's: Pituitary adenoma, Parathyroid hyperplasia, and Pancreatic involvement. Prolactinomas are the most common pituitary adenoma and can cause bitemporal hemianopsia, if large enough, due to optic chiasm compression. Gastrinomas (eg, Zollinger-Ellison syndrome) are the most common pancreatic tumors, which are treated with high-dose proton pump inhibitors.
1 note
·
View note
Text
Day 2 - Healthy Anime
Continuing with Multiple Endocrine Neoplasias (MEN). We will continue with the men of Kuroko no basket and tackle MEN2A.
MEN2A aka Sipple’s Syndrome has 2 P’s: Parathyroid tumors and Pheochromocytomas (tumors of adrenal glands). So these patients get hyperparathyroidism, adrenal medullary tumors (pheochromocytomas) that produce catecholamines, and as a bonus can get medullary thyroid carcinomias.

To remember MEN2A - think Himuro. He always sticks together with Murasakibara - so they’re always 2 men ie MEN2. He loves pheochromocytoma with all the catecholamines, metanephrines, palpitations, and sweating. It’s almost like he has a thyroid problem. He also gets PARAnoid (parathyroid - kidney stones and increased amyloid) when he’s away from his boo Murasakibara.
In summary:
MEN2A = Sipple’s Syn
Parathyroids
Pheochromocytoma
Medullary thyroid cancer
Inc amyloid and inc calcitonin
#MEN2A#multiple endocrine neoplasia#kuroko no basket#himuro#Sipple Syndrome#100 days of healthy anime
1 note
·
View note
Text
Sorry I have bee so incognito as of late. I’ve still been following all of your wonderful Tumblr updates, just not posting myself. It’s been a busy few weeks, let me tell you.
I finally went to my doctor and talked to her about all of my anxiety. I have finally accepted that I need more help than just breathing exercises.
Dad was doing a lot better at Christmas. He and Husband A spent the entire time in the kitchen having a full conversation. It did my heart happy to see that. Whenever we left, I could tell Husband A was excited that he got to have that time with Dad. It hasn’t happened it a while. He still has cancer and it’s not getting better, but we’re enjoying the time that we have left.
My niece was born. My SIL has a chronic pain disease that meant she had to continue with pain medicine throughout the entire pregnancy or lose Harlee, so Harlee came early at 36 weeks, but had to spend a week in the NICU. She was home for Christmas, though.
My Mom finally got Genetic testing done for MEN2a, but she came back positive. She will be having her thyroid removed this year. Her Calcitonin levels came back okay, though. They were elevated, but not cancer elevated. My brothers and I all have to get tested now. If I come back positive, then I will definitely be getting my Thyroid removed this summer. If I don’t, then I have a 98% chance of developing cancer. I’d rather take medication for the rest of my life than risk that.
Due to all of that stress, I’ve now started Paxil. It took about 2 weeks to get used to it, but I’m actually started to feel better.
With all of that, I think I’ve officially made my decision to stop TTC. I brought up the option to adopt from foster care to Husband A last night and he seemed open to the idea. I’m not going back on birth control, though. So, I think we’re officially Not Trying, Not Preventing. More on that later.
4 notes
·
View notes
Text
Medullary carcinoma of the thyroid (MTC) accounts for less than 5% of thyroid cancer. MTC arises from the C cells of the thyroid, which do not accumulate radioiodine, and it secretes calcitonin (Ctn), which is used as a tumor marker. Sporadic, or isolated, MTC accounts for 75% of cases and the remaining 25% are part of multiple endocrine neoplasia type 2 (MEN2), an autosomal-dominant syndrome caused by germline-activating mutations in the RET proto-oncogene. [1] These features allow early recognition of sporadic MTC using Ctn screening in patients with thyroid nodules and preclinical diagnosis of patients with MEN2 by RET gene analysis. Outcome depends on extent of disease, nature of tumor biology, and overall efficacy of surgical treatment.
Advances in genetic testing in have revolutionized the management of this disease, by allowing risk stratification of patients with inherited mutations and identifying molecular targets for therapy. Prophylactic thyroidectomy is indicated for patients who carry mutations that put them at risk for aggressive MTC.
Surgery remains the standard of care for localized disease and for oligometastatic disease. Several tyrosine kinase inhibitors are approved for use in progressive, metastatic MTC, and a variety of agents have entered clinical trials. External beam radiotherapy is used in certain situations.
Medullary thyroid cancer (MTC) is usually diagnosed on physical examination as a solitary neck nodule. Early spread to regional lymph nodes is common. Distant metastases occur in the liver, lung, bone, and brain.
Sporadic MTC usually is unilateral. MTC in association with multiple endocrine neoplasia (MEN) syndromes is always bilateral and multicentric, with presentation earlier in life. MTC typically is the first abnormality observed in both MEN 2A and 2B syndromes.
In addition to producing calcitonin, MTC cells can produce several other hormones, including corticotropin, serotonin, melanin, and prostaglandins. Moreover, paraneoplastic syndromes (eg, carcinoid syndrome, Cushing syndrome) can occur in these patients.
Etiology
Sporadic MTC occurs in 75% of patients, and inherited MTC constitutes the rest. MTC is the dominant component of the multiple endocrine neoplasia (MEN) type 2 syndromes, MEN2A and MEN2B. MEN2A accounts for 95% of the cases. The following four variants have been recognized:
Classical MEN2A - The most common variant. MTC is uniformly present; pheochromocytoma, primary hyperparathyroidism, or both occur less frequently.
MEN2A with cutaneous lichen amyloidosis (CLA) - CLA may present in young patients, before the onset of clinically evident MTC
MEN2A with Hirschsprung disease
Familial medullary thyroid carcinoma (FMTC) - MTC only, in the absence of a family history of pheochromocytoma or hyperparathyroidism
Mutations in RET, a transmembrane proto-oncogene located on chromosome 10q11.2, are responsible for MEN2. Although its function is still unknown, the protein produced by RET is critical during embryonic development of the enteric nervous system and kidneys. RET consists of 3 domains, including a cysteine-rich extracellular receptor domain, a hydrophobic transmembrane domain, and an intracellular tyrosine kinase catalytic domain.
RET germline mutations are present in virtually all patients with MEN2A and MEN2B, and somatic RET mutations are present in approximately 50% of sporadic MTCs. In sporadic MTC that is RET mutation–negative, mutations in genes involving the RAS pathway—HRAS, KRAS, or (rarely) NRAS—are often found.
Epidemiology
Thyroid cancer represents approximately 3% of new malignancies occurring annually in the United States, with an annual incidence of approximately 14 per 100,000. Of these cancer diagnoses, 2% to 3% are medullary thyroid carcinoma (MTC), which translates into approximately 1080-1620 new diagnoses per year. Unlike the rising incidence rates of papillary thyroid cancer and other differentiated thyroid cancers, incidence rates for MTC (as well as follicular) thyroidcancers have remained relatively stable over the past 30 years.The incidence rate of MTC in Europe is 0.11 per 100,000 person-years, with no noted substantial differences by race/ethnicity and sex. Peak incidence of isolated MTC occurs in the fifth or sixth decade of life. The peak incidence of MTC associated with multiple endocrine neoplasia (MEN) 2A or 2B occurs during the first to third decade of life.
Prognosis
Prognosis depends on patient age, histologic grade, and status of surgical resection. Patients with a worse prognosis tend to be older, have higher-grade lesions, and have undergone incomplete surgical resection of the lesion. The 5-year relative survival for stages I to III is about 93% compared to 28% for stage IV. [6]Isolated medullary carcinoma of the thyroid (MTC) typically demonstrates a relatively indolent biologic progression. While regional lymph node metastases are possible, the lesion may not spread outside of the cervical region until several months later. MTC associated with multiple endocrine neoplasia (MEN) syndromes may have a more aggressive course, which also depends on associated comorbidity (eg, pheochromocytoma).
Despite advances in genetic screening for the RET proto-oncogene, preliminary population studies have yet to show a definitive impact on disease prognosis.
A study by Rohmer et al concluded that disease-free survival (DFS) in younger patients (>21 y) with hereditary MTC was best predicted by TNM staging and preoperative basal CT level of less than 30 pg/mL. Basal CT findings, class D genotype, and age were the key factors in deciding peroperatively timely surgery.In a meta-analysis of 27 studies involving 984 MTC patients who underwent reoperation, Rowland and colleagues found that normalization of calcitonin after reoperation occurred in 16.2% of patients overall. Patients who underwent targeted selective lymph node removal procedures showed normalization of calcitonin in 10.5% of cases, while normalization was seen in 18.6% of those who underwent compartment-oriented procedures.
Permanent hypoparathyroidism and recurrent laryngeal nerve palsy reportedly occur in less than 2% of virgin neck dissections. Reoperation is associated with a considerably higher risk of these injuries.
Clinical picture
A specific constellation of symptoms of medullary thyroid carcinoma (MTC) is not usually noted; however, one or more of the following symptoms may be observed:
Patients may describe a lump at the base of the neck, which may interfere with or become more prominent during swallowing
Patients with locally advanced disease may present with hoarseness, dysphagia, and respiratory difficulty
Although uncommon, patients may present with various paraneoplastic syndromes, including Cushing or carcinoid syndrome
Diarrhea may occur from increased intestinal electrolyte secretion secondary to high plasma calcitonin levels
Distant metastases (eg, lung, liver, bone) may result in weight loss, lethargy, and bone pain
Physical Examination
Physical examination may demonstrate a dominant thyroid nodule at the base of the neck. Palpable cervical lymphadenopathy signifies disease that has progressed locally. Icterus, and rarely, bone tenderness may occur in patients with systemic metastases.
Cutaneous lichen amyloidosis in MEN 2A patients manifests as multiple pruritic, hyperpigmented, lichenoid papules in the scapular area of the back. Men2B patients may have a marfanoid habitus with mucosal neuromas.
Labile hypertension may be seen in those with an associated pheochromocytoma.
2 notes
·
View notes
Text
Multiple Endocrine Neoplasia
MEN 1 = Wermer’s Syn
Pituitary
Parathyroid
Pancreas (gastrinomas, peptic ulcers)
Make sure to check serum Ca++ esp if kidney stones/peptic ulcers

So for MEN1 I’m gonna relate it to Kuroko no Basket’s Akashi. He is has the Emperor’s Eye which means he is the EMPEROR and they have all the things - thus Akashi has all 3 P’s - Pituitary, Parathyroid, and PANCREAS THE FORBIDDEN ONE.
MEN2A = Sipple’s Syn
Parathyroids
Pheochromocytoma
Medullary thyroid cancer
Inc amyloid and inc calcitonin

MEN2A = Himuro because 2B is the freaking giant Murasakibara. He loves the pheochromocytoma with all the catecholamines, metanephrines, palpitations, and sweating. It’s almost like he has a thyroid problem. He also gets PARAnoid (parathyroid), kidney stones and increased amyloid when he’s away from his boo Murasakibara.
MEN2B
Pheochromocytoma
Medullary thyroid cancer
Marfanoid body habitus
Mucosal neuromas - tongue tumors

MEN2B is definitely Murasakibara. He’s got the huge Marfanoid like body. He’s got the tongue tumors what with all the junk food he eats. He also loves the pheochromocytoma because Himuro like it. He also shares the possibility of getting that medullary thyroid cancer because he’s xoxoxo with Himuro.
MEN Syndromes are all Autosomal Dominant - thus all the dominant BB players that and they’re all MEN
MEN1: 3P’s = All the P’s = Emperor takes all
MEN2A: 2P’s = gets some parathyroid stuff and shares pheo and thyroid with 2B
MEN2B: 1P, Giant with an oral fixations but shares medullary thyroid cancer & pheo with 2A
0 notes
Text
There are various sorts of thyroid disease
Thyroid disease can be portrayed as by the same token:
Separated thyroid disease, which incorporates all around separated cancers, ineffectively separated growths, and undifferentiated cancers
Medullary thyroid disease.
Very much separated growths (papillary thyroid disease and follicular thyroid malignant growth) can be dealt with and can typically be relieved.
Ineffectively separated and undifferentiated growths (anaplastic thyroid disease) are more uncommon. These growths develop and spread rapidly and have a less fortunate possibility of recuperation. Patients with anaplastic thyroid malignant growth ought to have atomic testing for a change in the BRAF quality.
Medullary thyroid disease is a neuroendocrine growth that creates in C cells of the thyroid. The C cells make a chemical (calcitonin) that keeps a solid degree of calcium in the blood.
See the PDQ synopsis on Childhood Thyroid Cancer Treatment for data about youth thyroid disease.
Age, orientation, and being presented to radiation can influence the gamble of thyroid malignant growth.
Anything that expands Best Cancer Specialist in Delhi your gamble of getting an illness is known as a gamble factor. Having a gamble factor doesn't imply that you will get malignant growth; not having risk factors doesn't imply that you won't get disease. Chat with your PCP assuming you figure you might be in danger.
Risk factors for thyroid disease incorporate the accompanying:
Being somewhere in the range of 25 and 65 years of age.
Being female.
Being presented to radiation to the head and neck as a baby or youngster or being presented to radioactive aftermath Best Cancer Specialist in Delhi. The malignant growth might happen when 5 years after openness.
Having a past filled with goiter (amplified thyroid).
Having a family background of thyroid sickness or thyroid disease.
Having specific hereditary circumstances like familial medullary thyroid disease (FMTC), numerous endocrine neoplasia type 2A disorder (MEN2A), or different endocrine neoplasia type 2B condition (MEN2B).
Being Asian.
Medullary Best Cancer Specialist in Delhi NCR thyroid disease is at times brought about by an adjustment of a quality that is passed from parent to kid Best Cancer Specialist in Delhi NCR.
The qualities in cells convey inherited data from parent to youngster. A specific change in the RET quality that is passed Best Cancer Specialist in Delhi from parent to kid (acquired) may cause medullary thyroid malignant growth.
There is a hereditary test that is utilized to check for the changed quality. The patient is tried first to check whether the individual has the changed quality Best Cancer Specialist in Delhi NCR. In the event that the patient has it Best Cancer Specialist in Delhi NCR other relatives may likewise be tried to see whether they are at expanded risk for medullary thyroid disease. Relatives, including little youngsters, who have the changed quality might have a thyroidectomy (medical procedure to eliminate the thyroid). This can diminish the possibility creating medullary thyroid malignant growth Best Cancer Specialist in Delhi.
Indications of thyroid disease remember an expanding or bump for the neck.
Thyroid malignant growth may not cause early signs or manifestations. It is some of the time found during a routine actual test Best Cancer Specialist in Delhi. Signs or manifestations might happen as the growth gets greater. Different circumstances might cause similar signs or side effects. Check with your primary care physician assuming you have any of the accompanying:
A knot (knob) in the neck.
Inconvenience relaxing.
Inconvenience gulping.
Torment while gulping.
Roughness.
0 notes
Text
Woman Undergoes Robotic Surgery For Rare Disease In Delhi
Woman Undergoes Robotic Surgery For Rare Disease In Delhi
A 31-year-old woman suffering from a rare form of hereditary disease was operated in Delhi.
New Delhi:
A 31-year-old woman suffering from a rare form of hereditary disease was operated through robotic surgery at a hospital in New Delhi.
The woman, who is from Kota, Rajasthan, suffered from multiple endocrine neoplasia type 2A (MEN2A), a rare inherited condition in which patients develop a…

View On WordPress
0 notes
Text
दिल्ली में दुर्लभ बीमारी के लिए महिला ने रोबोटिक सर्जरी की
दिल्ली में दुर्लभ बीमारी के लिए महिला ने रोबोटिक सर्जरी की
वंशानुगत बीमारी से पीड़ित एक 31 वर्षीय महिला का दिल्ली में ऑपरेशन किया गया।
नई दिल्ली:
नई दिल्ली के एक अस्पताल में रोबोटिक सर्जरी के जरिए वंशानुगत बीमारी से पीड़ित एक 31 वर्षीय महिला का ऑपरेशन किया गया।
महिला, जो राजस्थान के कोटा की है, कई एंडोक्राइन नियोप्लासिया टाइप 2A (MEN2A) से पीड़ित है, यह एक दुर्लभ विरासत वाली स्थिति है जिसमें मरीज दो ग्रंथियों, या तो थायरॉयड ग्रंथि, पैराथाइरॉइड ग्रंथि या…

View On WordPress
0 notes
Text
Adrenal
Low attenuation (HU<10), rapid washout (>50%) – adenoma
Higher attenuation (HU>18),<50% washout, heterogeneous - Adrenalcortical Carcinoma
Incidentaloma Resection if (Unilateral Laparoscopic Adrenalectomy):
Functional
>4cm
Malignant risk
<40yo, 1cm or more unilateral adrenal mass + symptoms of hyperaldosteronism —> Laparoscopic adrenalectomy
Pheochromocytoma- MEN2a, MEN2b. MRI T2 best scan. 131MIBG for localization. Clonidine normally suppresses plasma catecholamines, wont with Pheo. Needs Adrenalectomy. Phenoxybenzamine alpha blocker preop. 10% malignant, bilateral, extra-adrenal, familial
1 note
·
View note
Text
Medullary Thyroid Carcinoma (MTC)
Medullary Thyroid Carcinoma (MTC)
Medullary thyroid carcinoma (MTC) arises from:The neuroendocrine parafollicular C cells or C cells of the thyroid glandSporadic MTC accounts for about 75% to 80% of all cases of the disease:The remaining cases, 20% to 25% consist of inherited tumor syndromes, such as:MEN type 2A (MEN2A):Which is the most common typeMEN2BFamilial MTC:Is now viewed as a variant of MEN2ASporadic disease:Typically…

View On WordPress
0 notes
Photo


Hey, go check out my other blog @ifontwanttodrive where I post about my past year with me being diagnosed with overlap syndrome, MEN2a and a lot of fun and weird stories :) ( also here's some pics of my dog tenshi!)
#puppy#disease#overlap syndrome#story#me#mcga#voltron#bookrants#steven universe#pjo#jacksepticeye#markiplier
3 notes
·
View notes
Photo
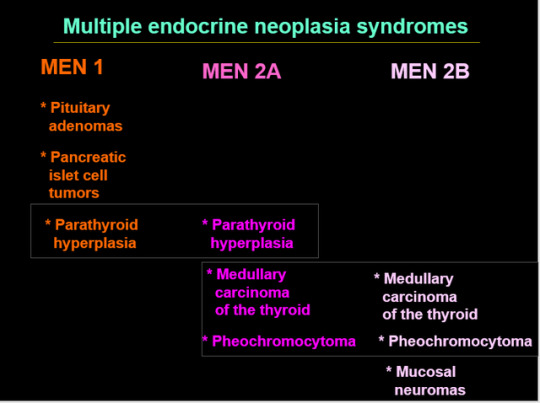
MEN1 = PPP
MEN2A = PPM
MEN2B = PMM
Pts with MEN2B often have marfanoid habitus. Pheochromocytomas occur in MEN2A and 2B; they occur anywhere along the sympathetic chain from neck to bladder. Must screen pts with medullary CA for pheochromocytoma before and after doing surgery. That’s because if you have medullary CA, you can have MEN2A or MEN2B, in which case you would have a pheochromocytoma. You don’t want the pt to have a HTN crisis during surgery. Also screen for pheochromocytoma periodically afterward. Plasma metanephrines must be obtained before surgery to evaluate for possibility of pheochromocytoma
8 notes
·
View notes
Text
Hi crush, Alam mo yung Men2A? Multiple Endocrine Neoplasia Type 2A diba? E yung Men2B? Tayo yun. We're Men2B. Hahaha 👑🌈💕
1 note
·
View note
Text
Kanserde genetiğin yeri
Genetik yapı: Bir insanın sağlığı, görünümü, kişiliği ve yetenekleri, genetik yapısı ve içerisinde yer aldığı çevresinin etkileşimi ile belirlenir. Genler ailemizden bize geçen özellikleri taşıyan, ve kromozomlar üzerine yerleşmiş, DNA dizininden oluşan en küçük yapı taşlarıdır. Kişinin genleri onun potansiyelini oluşturmakta, çevresi ise bu potansiyeli sınırlamada veya ortaya çıkarmada yardımcı olmaktadır. Örneğin bazı ilaçların kullanımı, enfeksiyonlar, beslenme bozukluğu ve kanser kişinin genetik potansiyeline göre farklı sonuçlar ortaya çıkarır. Ayrıca aile bireyleri arasında bir kişide genetik hastalıklardan birisinin ortaya çıkarılması, ailenin diğer fertleri için risk getirebilir, bu nedenle kan bağı olan kişilerde tarama yapılaması gerekir.
Kanserde Genetik: Kanserde genetik alt yapı yüzde on civarında sorumludur, çoklu faktörlere bağlı (genetik ve çevresel faktörlerin karşılıklı etkileşimi sonucu) olduğunu bilinmektedir. Özellikle yaşlanma, doğal ortamlardan uzaklaşma, doğal gıdalar tüketmeme, genetiği değiştirilmiş gıdaların fazla tüketilmesi, fazla alkol tüketilmesi, sigara ,elektro manyetik ortamlar, yaşamdaki önemli travmalar ve stres etkilemektedir.
Kanserle İlişkili Genler:
Tümör baskılayıcı genler: Bunlar koruyucu genlerdir. Vücudun iyi ustalarıdır, hasarlanan yeri hemen tamir ederler. Bu genler normalde hücre bölünme hızını sınırlar, hasarlı DNA’yı tamir eder ve hücre ölümünü kontrol eder. Bu genler mutasyona uğradığında hücreler büyümeye devam eder ve sonunda tümör oluşur. BRCA1, BRCA2(meme kanseri), ve p53’ü genlerini içeren 30’a yakın tümör baskılayıcı gen tanımlanmıştır. Tüm kanser vakalarının yaklaşık % 50’sinde p53 geni ya yoktur ya da hasarlıdır. Bu önemli genin mutlaka baktırılması gerekir.
Onkogenler: Sağlıklı hücreyi, kanseröz hücreye dönüştüren genlerdir. Bunlar da vücudumuzun kötü ustalarıdır. HER2/neu (meme kanseri) ve ras, en yaygın iki onkogendir.
DNA Tamir Genleri: DNA’nın çoğalması esnasında oluşan hataları tamir eder. Tamir edilmeyen hatalar, mutasyona yol açar ve sonunda kanser gelişir.
Prof. Dr.Duran Canatan
Çeşitli genlerdeki mutasyonlar sonucuna kanser gelişir, ancak kanserlerin pek çoğu belirli bir tip genle ilişkili değildir.
Günümüzde; meme, over, kolon ve uterus kanserlerinin %10 unun bilinen genetik mutasyonlardan kaynaklandığı saptanmıştır. Belirli genler, diğer genler veya çevresel faktörlerle Meme, yumurtalık (over), kalın barsak (kolon) ve diğer nadir kanserlerde uygulanabilir 900′ den fazla genetik test vardır.
Kanserde genetik testler: Genetik testlerin çoğu, yaşamın herhangi bir döneminde kanser gelişme olasılığının tahmin edilmesine yardımcıdır. Kişide % 100 kanser gelişeceğini belirten hiçbir genetik test bilinmemektedir, ama bu testler toplumun geri kalanına oranla kanser gelişme riski daha yüksek olan kişileri işaret edebilir. Kanserle ilişkili olan genlerin hepsi kansere yol açacaktır diyemeyiz; örneğin meme kanseri gelişme riski genine sahip kadınların % 75′ i sağlıklı kalırken; sadece % 25′ inde meme kanseri ortaya çıkmaktadır.
Aile üyelerinde genç yaşta kanser teşhis edilen birey olanlarda, üç veya daha fazla kuşakta aynı tip kanser öyküsü bulunanlarda, anne veya baba tarafından üçten fazla kanser olgusu bulunan kişilerde ve aile bireylerinden birinde iki veya daha fazla farklı tip kanser bulunan bireylerde kanser gelişme riski yüksektir.
ASCO (Amerikan Klinik Onkoloji Derneği); aile öyküsünde veya kişisel öyküsünde genetik kanser şüphesi bulunanlarda, genetik durumu yeterince yorumlanarak, genetik testlerin tanı ve tedaviye yardımcı olacağı vakalarda genetik testlerin yapılmasını önermektedir.
Genetik Testler:
Kolon kanseri (APC Geni-Dizi Analizi)
Meme kanseri (BRCA1 ve BRCA2 MLPA)
Meme kanseri (BRCA1, BRCA2, p53 Tüm Gen-Dizi )
Malign Melanoma (P16 Tüm Gen-Dizi Analizi)
Tüm Kanserler (P53 Geni-Dizi Analizi)
Kolorektal Kanser, PapillarTiroid Kanseri (BRAF)
Kolorektal , Akciğer, Pankreas Kanseri (KRAS) Kronik MyeloidLökemia (ABL1)
Kolorektal, Akciğer NSCLC, Meme Kanseri (EGFR)
Familyal Medüller Troid Kanseri (FMTC) RET (Ekzon 10-11-13-14-15 ve 16)
Multiple Endok NeoplaziTip2 (MEN2A ve MEN2B),
Aile Non-Polipo Kol Kan (MLH1,MSH2,MSH6,PMS2)
Mesane ve serviks Kanseri –( FGFR3 Geni-Dizi)
Gastrointestinal Kanser (C-KIT :9,11,13,17 Ekz)
JAK2 Geni (V617F mutasyonu)
Genetik danışmanlık: Genetik testler, kanser nedenini, gelecekte kanser gelişme riskinin olup olmadığını ve/veya kanserin çocuğunuza geçip geçmeyeceğini anlamaya yardımcı olacaktır.Bu testleri yaptırmak, aile bireyleri ve doktorunuzla yapacağınız işbirliğiyle alınmış kişisel karara bağlıdır.
Bu testleri yaptırmakla, kanser gelişme riski yüksekse daha sık tarama testlerinden geçmek, belli risk faktörlerinden kaçınmak, yaşam biçiminizi değiştirmek yoluyla kanser gelişim riskini azaltmak, koruyucu medikal tedavi alma şansını artıracaktır.
Ailede birden fazla bireyde genetik mutasyonla geçen kanser öyküsü var ve genetik tarama testi negatif ise; bu durum kişiyi rahatlatacaktır.
Koruyucu hekimlik açısından kanser genetik testleri ve genetik danışmanlık oldukça önemlidir. Sosyal Güvenlik Kurumunun test bedellerini karşılaması gerekir. Birey kanser olduğunda ailenin harcamalarını bir kenara bırakırsak, hastanın medikal tedavisi, cerrahi ve ışın tedavilerine Sosyal Güvenlik Kurumu çok para ödemektedir.
Koruyucu hekimliğe harcanan para tedavi edici hekimliğe harcanan para yüz birimdir. Örneğin kanser de bir kanser genetik testi bir birim ise, kanserin tedavisine ödenen para yüz birimdir. Kişinin yaşadığı travmayı, manevi çöküntüyü, ailesinin çektiklerini, iş gücü kayıplarını para ile ölçmek mümkün değildir.
source https://saglik.kocaali.com/kanserde-genetigin-yeri-3/
0 notes