#Prematurity
Photo

https://www.hippocraticpost.com/australasia/stillborn-and-preterm-statistics-for-covid-19-first-wave/ Interesting research. The research of 52 million births from 26 countries, published in Nature Human Behavior, reported a 3-4 per cent reduction overall in preterm births, averting almost 50,000 preterm pregnancies during the first month of lockdown alone. But the decrease in preterm births was limited to only high-income countries including Australia. The International Perinatal Outcomes in the Pandemic (iPOP) Study, one of the largest such studies of its kind, involved 167 collaborators across 42 countries. Murdoch Children’s Research Institute co-led the project alongside The Children’s Hospital Research Institute of Manitoba, University of Manitoba, The University of Edinburgh and UNSW Sydney. #preemiefamily #preterm #prematurebabiesawareness #neonatolgy #neonatal #prematurity #earlybaby #earlybabies #premature #research #nicuparents #nann #NICU https://www.instagram.com/p/Cpvrxnaqzb2/?igshid=NGJjMDIxMWI=
#preemiefamily#preterm#prematurebabiesawareness#neonatolgy#neonatal#prematurity#earlybaby#earlybabies#premature#research#nicuparents#nann#nicu
8 notes
·
View notes
Text
#prejac#hot as fuck#sexy content#spicy content#big boody#big round butt#cutie w a bootie#girl butts#sexy titts#great body#premature ejaculator
47K notes
·
View notes
Text
#asexual#tozzyn13#big round butt#cutie w a bootie#girl butts#hot nude#hot as fuck#onlytease#curvy girls#premature ejaculator#sexy titts#lingerie sexy#sexy breast
10K notes
·
View notes
Text
November 17th - World Prematurity Day

#World prematurity day#Prematurity#Prematures#nicu#Medicine#Paediatrics#Awareness#Prematurity awareness#Healthcare#pregnancy#babies#infants
0 notes
Text
World Prematurity Day

On World Prematurity Day, let us unite in the spirit of compassion and hope for the tiniest fighters. Medikart Healthcare stands committed to nurturing precious beginnings, providing strength and care to the little ones who inspire us with their resilience. Together, let's build a world where every premature baby has a chance to thrive and flourish.
#worldprematurityday#MedikartHealthcare#prematurebaby#prematurity#prematurityawareness#prematurityawarenessmonth#pretermbirth#newborn#medikart#healthcare#gratitude#healthcareheroes#health#healthyliving#wellness#wellnessjourney#healthfirst
0 notes
Text

"It's important to me to support the whole family. No one's birth plan includes a NICU stay. No matter how uncomplicated a case might be, medically speaking, the stress and loss of anticipated moments can be challenging for the family. My job is not only to provide exceptional clinical care for the newborn, but also to keep the parents aware and involved so they can keep their sense of autonomy and place as the number one caregiver in their baby's life."
Joann Smith, Physician, Neonatology, Nationwide Children's Hospital - Toledo
0 notes
Text

if only he had noticed
#rewatched jjk zero and it was a big miss steak#i will never get over them#stsg#satosugu#sugusatu#sgst#satoru gojo#gojo satoru#gojo x geto#hidden inventory arc#premature death arc#jujutsu kaisen#jjk#fanart#geto suguru#suguru geto#arctvros
15K notes
·
View notes
Text
Gynecologist In Thane West - Dr. Sujata Rathod

Discover the critical insights about the potential risks associated with pregnancy over age 35, including miscarriage, birth defects, twins, high blood pressure, gestational diabetes, and potentially difficult labor. A wealth of information is at your fingertips, guiding you through the journey. Knowledge is power - be prepared and stay informed.
Call to Book an Appointment: +09869174139 or Visit Site : https://nurvinaari.com
#pregnancyrisksat35age#highriskpregnancy#pregnancy#pregnant#gestationaldiabetes#obgyn#prematurity#pregnancycomplications#weekspregnant#gynecologistthane#drsujata
1 note
·
View note
Text

I need your cock for a back shot 🍆💦💗💗💦💦💗 reblog if you wanna be that dude 🥵🍆🍆💙💦
telegram:@Alisonamy
Whatsapp: +1 (267) 724-7784
google chat: [email protected]
#prejac#premature ejaculator#hot as fuck#sexy content#great body#girl butts#sexy titts#spicy content#cutie w a bootie#big round butt
3K notes
·
View notes
Text
Inhibition of acute preterm labor:
●Candidates for treatment – For patients with preterm labor less than or equal to 34+0 weeks of gestation, we suggest tocolytic therapy (Grade 2B). A delay in delivery for 48 hours for administration of antenatal corticosteroids (ACS) can provide benefit to the newborn.
●Treatment goals – The goal of treatment is to delay delivery so that ACS can be administered and achieve the maximal effect; allow safe transport of the mother, if indicated, to a facility that can provide an appropriate level of neonatal care if the patient delivers preterm; and prolong pregnancy when there are underlying, self-limited causes of labor, such as abdominal surgery, that are unlikely to cause recurrent preterm labor. Treatment can be discontinued after these goals have been achieved.
●Choice of tocolytic drug
•First-line therapy less than or equal to 32+0 weeks
-For patients less than or equal to 32+0 weeks of gestation who are candidates for tocolysis, we suggest indomethacin as first-line therapy for labor inhibition (Grade 2B). It appears to be superior to placebo and has a relatively favorable maternal and fetal side effect profile and is compatible with concomitant neuroprotective administration of magnesium sulfate.
Contraindications to indomethacin use include maternal platelet dysfunction or bleeding disorder, hepatic dysfunction, gastrointestinal ulcerative disease, renal dysfunction, or hypersensitivity to aspirin. We avoid the use of indomethacin in gestations over 32+0 weeks and caution against their use for more than 72 hours because of concern about premature narrowing or closure of the ductus arteriosus.
-We suggest nifedipine for patients less than or equal to 32+0 weeks who have a contraindication to indomethacin (Grade 2B).
•First-line therapy greater than 32+0 weeks – For patients greater than 32+0 and less than or equal to 34+0 weeks of gestation who are candidates for tocolysis, we suggest nifedipine as the first-line therapy (Grade 2B).
•Second line therapy – If the first-line drug does not inhibit contractions, we discontinue it and begin therapy with another agent. For second-line therapy, we use nifedipine at less than or equal to 32+0 weeks and terbutaline at greater than 32+0 and less than or equal to 34+0 weeks, and for patients less than or equal to 32+0 weeks who received nifedipine as a first-line agent.
We avoid concurrent use of tocolytic drugs because of the increased risk of side effects and the absence of evidence of efficacy.
●Ineffective therapies – In patients with an acute episode of preterm labor, bedrest, hydration, sedatives, antibiotics, and progesterone supplementation are ineffective for preventing preterm birth.
I would just give nifedipine firstline whether the pt is 32 weeks or 34 weeks. I'm kind of confused as to why you would use indomethacin firstline for those less than or equal to 32 weeks. Aren't you worried about premature closure of the ductus arteriosus regardless of whether the pt is 32 weeks or not? I'll ask the attending. She said the older the pt is than 32 weeks, the likelier the risk of premature closure of the DA. You can do up to 48 hours of tocolysis with indomethacin if the pt is less than 32 weeks GA.
Antenatal corticosteroid therapy
Effects on newborn outcome – Antenatal corticosteroid therapy (ACS) reduces the incidence of respiratory distress syndrome, intraventricular hemorrhage, necrotizing enterocolitis, sepsis, and neonatal mortality by approximately 50 percent. These effects are not limited by sex or race; efficacy in multiple gestations is unclear as high-quality data are sparse.
●Approach to treatment at 21+0 to 22+6 weeks of gestation – ACS can be considered at this gestational age when delivery in the next seven days is anticipated and the patient is requesting aggressive neonatal intervention. A key concept is that ACS may provide a survival benefit, but the risk of major long-term morbidity in survivors is high. Shared decision-making involving the parents, obstetrician, and neonatologist is particularly important at this gestational age.
●Approach to treatment at 23+0 to 33+6 weeks of gestation
•Candidates – Given the benefits of ACS, we recommend administration of ACS to pregnant patients who are at 23+0 to 33+6 weeks of gestation and at high risk of preterm birth within the next one to seven days (Grade 1A). In our practice, we restrict administration of the first course of ACS to patients who rupture membranes or are receiving tocolysis for active preterm labor, or in whom delivery for maternal or fetal indications is highly anticipated within the next seven days. Antenatal hospitalization does not necessarily mandate a course of ACS. This approach minimizes the need for salvage (rescue, booster) therapy while allowing most patients to receive a course of ACS prior to preterm delivery.
•Dose – A course of ACS consists of betamethasone suspension 12 mg intramuscularly every 24 hours for two doses or four doses of 6 mg dexamethasone intramuscularly 12 hours apart.
•Effect of timing on outcome – Observational data suggest neonatal benefits begin to accrue within a few hours of ACS administration. Maximum efficacy appears to occur when delivery occurs one to seven days after administration of the first dose of ACS. Efficacy is incomplete less than 24 hours from administration and appears to decline after seven days.
•Lower gestational age threshold for administration – We consider approximately 23+0 weeks of gestation as the lower limit for ACS administration since only a few primitive alveoli are present below this gestational age. Earlier administration in the 22nd week is reasonable if aggressive neonatal intervention is planned after thorough counseling about the limit of viability.
●Approach to treatment at greater than or equal to 34+0 weeks of gestation – In contemporary obstetric practice in the United States, patients delivered at 34+0 to 38+6 weeks of gestation for an obstetric indication are now delivered without amniocentesis to test for fetal lung maturity. The following approach reflects our concern that widespread use of ACS at greater than or equal to 34+0 weeks will result in treatment of many pregnancies that will not benefit or will derive only a modest clinical benefit (avoidance of neonatal intensive care unit admission for transient mild respiratory problems) while exposing them to the potential long-term hazards of steroid administration, particularly adverse neurodevelopment outcome in offspring.
•Planned cesarean birth at greater than or equal to 37 weeks – For patients scheduled for cesarean birth at greater than or equal to 37 weeks, we suggest not administering a course of ACS (Grade 2C).
•Planned cesarean birth at 34+0 to 36+6 weeks – For patients scheduled within seven days for cesarean birth at 34+0 to 36+6 weeks, we suggest holding a discussion with the patient regarding the administration of a course of ACS prior to their delivery. There is consensus that repeat courses of steroids are not indicated at this gestational age. For patients who have not received a previous course of steroids, data regarding the potential benefits and long-terms harms of an initial course are discussed using a shared decision-making approach, and some patients may choose to receive a course of steroids before their scheduled cesarean delivery as part of shared decision making.
•Vaginal birth at 34+0 to 36+6 weeks
-Vaginal birth within seven days uncertain – For patients at 34+0 to 36+6 weeks in whom a high risk of delivery within seven days is uncertain (eg, threatened preterm labor), we recommend not administering a course of steroids (Grade 1C). There is potential for long-term harm with no benefit if the patient does not deliver preterm. Importantly, a large proportion of patients with threatened preterm labor does not deliver within seven days when the effects of steroid administration are most likely to occur.
-Vaginal birth within seven days likely – For patients at 34+0 to 34+6 weeks in whom vaginal delivery is expected within seven days (eg, planned induction, preterm labor with substantial cervical change, preterm prelabor rupture of membranes), we suggest not administering ACS as the neonatal respiratory problems described in the ALPS trial are less common after labor and vaginal birth than after planned cesarean (Grade 2C).
However, this is a controversial area, and some national obstetric organizations have taken a more liberal approach to steroid administration at this gestational age.
●Use of repeat (rescue or salvage) courses in patients who do not deliver after the first course – The absence of consistent and long-term data precludes making a strong recommendation for the number of courses that are safe for the fetus, the appropriate time interval between courses, the optimal dose for repeated courses of therapy, or the full ramifications of the single course approach to therapy. Given the potential for harm from repeated courses of ACS:
•We suggest a course of salvage (rescue, booster) therapy only if the patient is clinically estimated to be at high risk of delivery within the next seven days, more than two weeks have elapsed since the initial course of ACS, the gestational age at administration of the initial course was less than or equal to 28 weeks of gestation, and membranes are intact (Grade 2C).
•We also suggest that providers who elect to give a course of salvage (rescue, booster) therapy use one rather than two doses of 12 mg betamethasone and limit treatment to this one additional dose (Grade 2C) before 34 weeks of gestation. One dose appears to be effective and may minimize complications related to steroid use; however, a two-dose course is also reasonable. No more than one salvage dose or course is recommended over a single pregnancy.
●Mechanism of action – ACS leads to improvement in neonatal lung function by enhancing maturational changes in lung architecture and by inducing lung enzymes involved in respiratory function.
I was confused as to why it said they don't recommend ACS for pts at 34 weeks because my pt is 34 weeks and we gave her steroids. But then I finished reading it. So basically, a vaginal delivery means the baby will get squished and have more stress so they're less likely to have pulmonary issues compared to a baby that doesn't get squished through the birth canal and who comes into the world via C-section instead. But I don't know yet whether this woman's baby will be NSVD or C-section. Probably the latter, but it makes sense we gave her steroids anyway.
1 note
·
View note
Text
#prejac#hot as fuck#sexy content#spicy content#sexy titts#big round butt#girl butts#great body#gorgeous#premature ejaculator#eliza rose watson
27K notes
·
View notes
Text
#asexual#tozzyn13#big round butt#cutie w a bootie#girl butts#hot nude#hot as fuck#onlytease#curvy girls#premature ejaculator#sexy titts#sexy breast#lingerie sexy#çok güzel
7K notes
·
View notes
Text
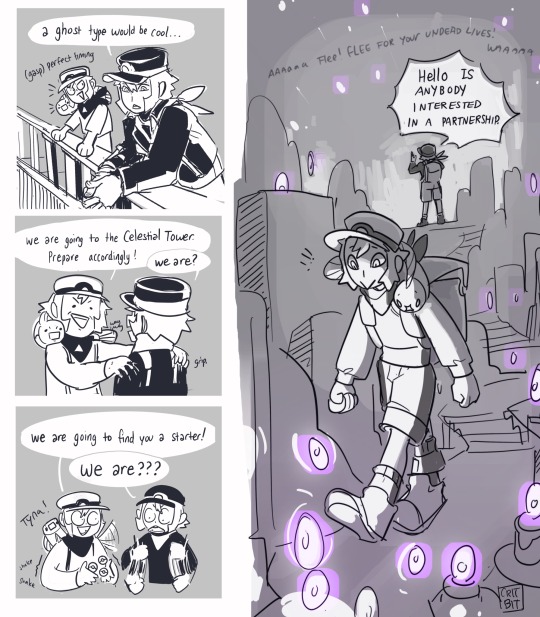

Meet Ingo’s partner!
The one and only!
A Litwick!


Litwick’s a panic capture and she knows it.
As a firm believer of half the depot agents in BW2 being either ghosts or pokemon (or both), a litwick with vague telepathy isn’t too out of question, me thinks.


Bonus:

Feel free to add any headcannons! This is lawless lands now.
(click here for submas masterpost!)
#art#sketchbook#submas comic#baby submas#pokemon#ingo#subway boss ingo#subway boss emmet#subway bosses#pokemon ingo#pokemon emmet#litwick#tynamo#litwick’s on the payroll to drive ingo prematurely grey#(this is a lie ingo loves shenanigans when they arent happening to him)#ghost pokemon are weird#the art of candle domestication (80 percent of it is bribery)#fanart#submas
5K notes
·
View notes