#ovarian tissue
Text
Me: not bothered by the smell of sweat, on me on other people it's whatever I don't mind (I will even be a freak about it when the situation calls for it iykwim)
Also me: my deodorant isn't working anymore I can smell myself and I bet you could smell me a mile away I cannot go to work until all of this is neutralized (I go to work anyway, because I don't know how to 'fix' it because I don't know what's 'wrong' and why I'm seemingly sweating through stuff so easily it feels)
Throttles my brain aggressively
#I have one ovary (or ovarian tissue) and no tubes anymore#(I've been fixed :) )#so it's probably hormonal and I'll see about getting to the right doc for those questions#but also like what the hell#am I supposed to be putting deodorant on 2+ times a day? is that 'normal'#cream talks#I hate societies obsession with people smelling nice and neutral but I also completely understand not liking the smell#so if I can cover it for people then I will it's nbd
3 notes
·
View notes
Text
soooo that pain in my side has become constant and that side of my stomach is swollen so if i keel over and fucking die thats probably why
#monolith mumbles#its either an ovarian cyst or irritated scar tissue from when i got my appendix out#probably#unless i have some other thing#or my appendix fuckin grew back
8 notes
·
View notes
Text
Who Should Undergo Fertility Preservation And How?
View On WordPress
#age#AMH#bloganuary#cancer#chemotherapy#dailyprompt#egg freezing#embryo freezing#Fertility#Fertility preservation#health#infertility#IVF#ovarian reserve#Ovarian stimulation#ovarian tissue cryopreservation#pregnancy#radiotherapy#semen freezing
0 notes
Text

Exploring Cryopreservation: Unveiling the Frozen Frontier
Cryopreservation involves the freezing of biological material to temperatures below freezing to halt metabolic processes and safeguard cellular integrity. The primary aim is to minimize damage caused by ice crystal formation, dehydration, and chemical reactions during freezing and thawing. Cryoprotectants, like glycerol and dimethyl sulfoxide (DMSO), are crucial, preventing ice formation within cells and tissues while maintaining structural integrity. Achieving the right balance between cryoprotectant concentrations and freezing rates is essential for optimal outcomes, as deviations can lead to cellular injury and reduced viability post-thaw.
The principles of cryopreservation encompass meticulous management of temperature gradients, cooling rates, and cryoprotectant concentrations to preserve cellular viability and functionality. Researchers delve into cryobiology, studying molecular mechanisms underlying cellular responses to freezing and thawing stresses. By understanding biochemical pathways involved in cryoinjury and devising innovative strategies to mitigate its effects, scientists aim to optimize cryopreservation protocols and enhance success rates of organ transplantation.
Recent advancements in cryopreservation techniques, like vitrification, rapidly cool tissues to avoid ice crystal formation entirely. Vitrification holds promise in preserving delicate structures such as embryos and oocytes more efficiently and with lower toxicity compared to traditional methods. By refining vitrification principles for organ transplantation, researchers strive to overcome challenges and transform regenerative medicine.
Current Applications: Navigating the Frozen Landscape
While cryopreservation is widely used in reproductive medicine and cell banking, adapting it to organ transplantation presents unique challenges due to organ complexity. Yet, significant progress has been made in cryopreserving organs like kidneys, livers, and blood vessels for transplantation.
A notable success is cryopreserving ovarian tissue for fertility preservation in cancer patients. By freezing ovarian tissue before chemotherapy or radiation therapy, women can preserve fertility. Similarly, cryopreservation is vital in banking umbilical cord blood stem cells for treating diseases like leukemia and lymphoma.
Advances in organ perfusion technology expand cryopreservation's scope in transplantation. Machine perfusion techniques maintain physiological conditions in donor organs, reducing ischemic injury and preserving function during preservation. Integrating cryopreservation with organ perfusion aims to prolong organ viability, expand organ availability, and improve patient outcomes.
Challenges and Limitations: Navigating the Frozen Terrain
Despite its potential, cryopreservation in organ transplantation faces challenges. Ice crystal formation within tissues can damage cells and compromise organ viability upon thawing. Cryoprotectants carry the risk of cytotoxicity, affecting cellular function and viability.
Infrastructure and expertise for cryopreservation are essential, including specialized equipment and skilled personnel. Logistics of transporting cryopreserved organs pose challenges, requiring careful temperature regulation and transit conditions.
Research across disciplines seeks to overcome these challenges, with advancements in cryoprotectant formulations, storage technologies, and organ perfusion. Genetic editing and regenerative medicine offer prospects for rejuvenating cryopreserved tissues and organs, extending their functional lifespan and improving patient outcomes.
Doctors suggest undergoing a full body health checkup before organ transplantation and cryopreservation. You can undergo a regular full body health checkup at Jaslok Hospital Mumbai, which is one of India's best hospitals.
#full body health checkup#regular health checkups#health checkup packages#cryopreservation#organ transplant#organ transplantation#fertility preservation#ovarian tissue freezing
0 notes
Text
Pain to Possibilities: Understanding Endometriosis!
Endometriosis is a complex and misunderstood medical condition affecting millions of women worldwide. It’s a condition that can cause excruciating pain, disrupt daily life, and even lead to infertility. Yet, despite its prevalence and impact, endometriosis remains underdiagnosed and frequently under-discussed. In this blog post, we will be understanding endometriosis, from pain to possibilities.…

View On WordPress
#Adhesions and scarring#Empowering endometriosis management#Endometrial implants#Endometrial tissue#Endometriosis awareness#Endometriosis causes#Endometriosis complications#Endometriosis diagnosis#Endometriosis infertility#Endometriosis pain#Endometriosis symptoms#Endometriosis treatment#Gynecological conditions#Hormonal influence#Laparoscopy#Menstrual cramps#Ovarian cysts#Pelvic pain#Retrograde menstruation#Women&039;s health
0 notes
Text
Have you heard about mole genders?

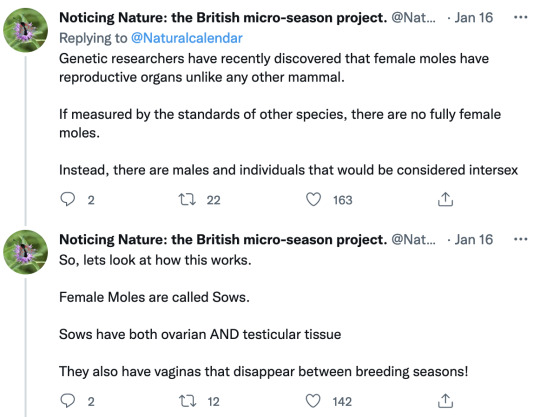








I’ve heard of this concept in sci-fi, but thought it was absolutely made up. I know some fish and frogs can change genders, but not in cycles like this. Wild. If I slapped this down in some alien world without explanation, I’d laugh in my own face. But no, real biology IS that bizarre.
Image descriptions:
A series of tweets from @NaturalCalendar that say:
Hello lovely Nature Noticers. It is time for today's thread! Follow me, and we'll delve deep into the subterranean and subversive world of Talpa europaea, the common European mole. We'll begin with a bombshell - there are no female moles.
Genetic researchers have recently discovered that female moles have reproductive organs unlike any other mammal. If measured by the standards of other species, there are no fully female moles. Instead, there are males and individuals that would be considered intersex.
So, lets look at how this works. Female Moles are called Sows. Sows have both ovarian AND testicular tissue They also have vaginas that disappear between breeding seasons!
Most of the year, female moles look and behave like males. They have masculinised genitals, with no external vagina + an enlarged clitoris. When this point in the year arrives, mating season begins. At this point the Sow's testosterone levels drop + they develop a vagina.
As is typical for mammals, Sows are equipped with two X chromosomes and Boars with an X and a Y chromosome. Unlike any other mammals Sows simultaneously develop functional ovarian and testicular tissues united in one organ, the 'ovotestis'. This is unique to Moles.
This testicular tissue does not produce sperm. It does however, produce large amounts of the sex hormone testosterone, meaning that Sows have similar testosterone levels to the Boars -except during mating season.
Scientists have hypothesized that these high levels of testosterone provide an adaptive advantage for the mole's underground life - providing added muscle mass for Sows who need to dig burrows and fight for resources for their offspring.
This is a dynamic process - the ovarian tissue that makes eggs and gets larger during breeding, then regresses. Outside of breeding season the testicular tissue, expands until it’s larger than the ovarian end - flooding the Sow's system with testosterone.
This explains why female moles have male-like genitalia... But it doesn't explain how patch of testicular tissue forms in female moles even though they do not have a Y chromosome. Up until recently the Y chromosome was thought to be fundamental to male sex determination.
In 2020 a team of molecular geneticists studied the female mole's ability to produce testicular tissue without a Y chromosome. They found that changes in the structure of the Mole's genome that lead to altered control of genetic activity.
But what does this mean? In short the female mole shows us that evolution doesn't work in the way that we have assumed since Darwin - their DNA changes within the living organism.
Since Darwin, it has been generally accepted that the different appearances of living organisms are the result of gradual changes in genetic makeup that have been passed onto subsequent generations - but Moles experience changes in the regulatory regions belonging to sex genes.
The researchers found that female moles do not have a Y chromosone but they do have a triple CYP17A1 gene. CYP17A1 is involved in the formation of steroid hormones + the triplication of this gene in the mole creates a dynamic sex regulatory system.
This dynamic process appends additional regulatory sequences to the gene and leads to an increased production of male sex hormones in the ovotestes of female moles, especially more testosterone.
What the intersexual mole shows us is how important the three-dimensional organization of the genome is for evolution. Nature makes use of existing developmental genes and rearranges them to create a characteristic such as intersexuality.
We see in the mole that evolution is not a linear process, arranged around the principle of Euclidian geometry. It is rather a topological process - a structure cast in rubber that is responsive and adaptive to the environment.
The mole also reminds us of the complexity of sexual development. The shifting sexual characteristics of the mole shows how the process of sexual development can, and does result in a wide range of natural variations.
#biology#gender#moles#fun animal facts#intersex#truth is stranger than fiction#yes I’ve read The Left Hand of Darkness#I’ve seen this idea elsewhere too#I had no idea it was based on something so exact#bonkers man#trans#mole genders
38K notes
·
View notes
Text
i need help with vet bills.
this is a remake of my original post which you can find here.

this is toos, she's a 10 year old miniature schnauzer who was recently diagnosed with stage 4 kidney failure. she is currently on medication to keep her stable, and she's steadly improving and getting better, but over the course of figuring out what's wrong with her, we accumulated thousands of pounds of vet bills, as well as now needing to keep up with her medication, which is not cheap. there's also hope that when she is more stable, she can undergo surgery to have ovarian tissue discovered over the course of her vet treatments removed, which will be costly.
i've emptied my savings trying to pay for this, and my parents have been taking from their pensions, but we are quickly running out of options for where to get more money. we're desperate.
please consider donating to my paypal, every little helps. thank you!
678 notes
·
View notes
Link
Ovarian Tissue Freezing Ernakulam
#Ovarian Tissue Freezing Ernakulam#Best Hospital For Infertility In Kerala#TESA Infertility Treatment In Kochi#Male Infertility Treatment In Kerala#ICSI Treatment In Kerala#Laser-assisted Hatching Process In Kerala
1 note
·
View note
Text
This deeper understanding of the ovary means researchers could potentially create artificial ovaries in the lab using tissues that were stored and frozen before exposure to toxic medical treatments such as chemotherapy and radiation.
Currently, surgeons can implant previously frozen ovarian tissue to temporarily restore hormone and egg production. However, this does not work for long because so few follicles—the structures that produce hormones and carry eggs—survive through reimplantation, the researchers say.
Continue Reading.
68 notes
·
View notes
Text
Female reproductive health terms you should know!
(terfs not welcome)
Dysmenorrhea: Period pain that isn't normal, i.e. any pain more than Mild cramping.
Dyspareunia: painful intercourse
Oligomenorrhea: lighter, shorter menstrual flow.
Menorrhagia: heavier, longer menstrual flow.
Ovarian cysts: a mass on or in one's ovary, can be resolved on its own, or can remain and cause complications such as a rupture.
Polycystic ovary syndrome: a chronic condition causing cysts to reoccur on the ovaries and enlarging them. Symptoms include:
Irregular periods
hormonal imbalance
facial hair
weight gain
painful periods/ ovulation
infertility
People with PCOS are at higher risk for endometrial cancer, type II diabetes heart problems and high blood pressure.
Endometriosis: A chronic condition in which a tissue similar to, but different than, the endometrial lining grows outside of the uterus instead of inside. During menstruation this tissue sheds and has nowhere to go, thus irritating surrounding organs.
Symptoms include:
Irregular periods
Dysmenorrhea
Widespread pain
Painful ovulation
Vomiting, fainting, chills, sweating, fever and brain fog during menstruation
Infertility
Severe bloating
This also puts people at a higher risk for endometrial and ovarian cancer. There are four stages to Endo as it is a progressive disease, with 3/4 being more severe. The average time it takes to be diagnosed is 7 years.
Adenomyosis: A chronic disease similar and comorbid to endometriosis in which a tissue similar to the endometrial lining grows inside of the uterine wall. Symptoms are nearly identical to endometriosis but more difficult to detect.
Many people are diagnosed post menopause, by fault of the medical system, but it can and does develop much before then.
Ovarian cancer: cancer of the ovary(ies).
Endometrial cancer: cancer of the endometrium, the inner lining of the uterus.
Endometrial cyst, or chocolate cyst: cystic lesions from endometriosis.
Tilted uterus: the uterus is positioned pointing towards the back or severely to the front of the pelvis instead of a slight tilt towards at the cervix. Can cause painful sex and periods.
Pelvic floor dysfunction: inability to control your pelvic muscles. Comorbid with many things and is highly comorbid with endometriosis. Can cause pain and incontinence.
Vulvodynia: chronic and unexplained pain at the opening of the vagina.
Interstitial cystitis: a chronic condition where cysts form on the inside of the bladder and urinary tract and cause symptoms similar to that of a UTI.
Pre-eclampsia: a condition occurring in pregnancy where the blood supply between the fetus and the pregnant person is affected and can cause irregular blood pressure, swelling, and in more severe cases headache, nausea and vomiting, a burning sensation behind the sternum, shortness of breath and potentially death if untreated.
Endometritis: an infection or irritation of the uterine lining. Is not the same as endometriosis and is treatable but can cause pain, bleeding, swelling, general discomfort and fever, and more.
Pelvic inflammatory disease: an infection of the reproductive organs
Ectopic pregnancy: a pregnancy that is attached to the outside of the uterus. Can be fatal if left untreated.
There are many more I could probably add but if you see something missing, please add it!
#reproductive health#endometriosis#adenomyosis#pcos awareness#reproductive health awareness#chronic illness#polycystic ovarian syndrome#ovarian cancer#reproductive rights
180 notes
·
View notes
Note
when jen said she had abnormal sex anatomy i just assumed she was a transwoman but then she mentions not having to worry about periods anymore being a benefit of being a toy, am i wrong in my assumption then?
Jennifer is intersex! She has (or I guess had) an ovotestis (a gonad containing ovarian and testicular tissue). She also had an enlarged clitoris that formed a sort of pseudophallus. She was very self-conscious about it.
Having clothes that never come off and nothing between her legs is a blessing to her - she never has to see herself naked again. Perhaps in a better world where she had better parents and wasn’t taught to be ashamed of herself, she could have grown up to be proud and love herself.
52 notes
·
View notes
Note
wait until you find out there are plenty of people born with both ovarian and testicular tisssue
after a 2 second google search, i found that its called Ovotesticular DSD. "Ovotesticular disorder of sex development is the most rare form among all disorders of sex development and characterized by the simultaneous presence of both ovarian and testicular tissues in the same individual" which is what i believe you are referring to. As of 2019, it's only been reported in about 500 individuals. I read this here. you are misinformed; it is not "plenty" of people. (additionally, if you look in just the first sentence of the case report they describe the patient as "a 19-year old male.")
besides, what bathroom/prison/shelter/team/etc people with DSDs should enter is an entirely seperate question than if males without DSDs should enter those women's spaces
#radfem#radical feminist safe#sex based oppression#radblr#terfsafe#gender critical#gender abolition#not j a reblog tag
19 notes
·
View notes
Text
Gabriella Ferlita (February 23, 2024). "A third of trans men can ovulate after undergoing gender-affirming treatment, study finds." PinkNews. https://www.thepinknews.com/2024/02/23/do-trans-men-on-testosterone-ovulate/
tl;dr: This is about transgender men and other transmasculine people who had been on T for at least a year, and had stopped having a period. A third of these people continue to ovulate while they are on T, even though they don't have a period. The type or amount of T doesn't matter, so we don't know why this happens for some people and not others. It's more proof that being on T doesn't protect someone from getting pregnant. People who don't want to get pregnant need to use actual birth control or other methods of contraception.
Here's the full text of the study that the news article is about:
Joyce D. Asseler, Julieta S. del Valle, Susana M. Chuva de Sousa Lopes, Marieke O. Verhoeven, Mariette Goddijn, Judith A.F. Huirne, Norah M. van Mello (February 22, 2024). "One-third of amenorrheic transmasculine people on testosterone ovulate." Cell Reports Medicine 5, 101440. DOI:https://doi.org/10.1016/j.xcrm.2024.101440 https://www.cell.com/cell-reports-medicine/fulltext/S2666-3791(24)00063-6
#transgender#testosterone#hormones#contraception#birth control#pregnancy#ovulation#sex education#rated PG-13#PinkNews#relevant for transgender men and trans masculine nonbinary people and others on the female to male spectrum#relevant for people who can get pregnant#relevant for people who no longer menstruate#relevant for people in relationships where someone could get pregnant
14 notes
·
View notes
Note
do you know the general consensus on using the H-slur to refer to plants and/or animals? I know it shouldn't be used for people but I see a lot of people still using it to talk scientifically about animals or plants so I'm curious if I should be correcting them or not
It's entirely acceptable scientifically. There's no reason to correct! It is not usually offensive when being used towards animals or plants or the such. It is just the scientific term. It's okay if an intersex person feels uncomfortable hearing it, but it is okay to use. No need to correct!
Great question though! Totally valid concern.
However, it should only be used for organisms that are always hermaphrodites, if that makes sense. For example, slugs always have both functioning "male" and "female" reproductive systems. Gonochoric (meaning they function on a binary female/male sex system, like all mammals and birds) organisms are not ever hermaphrodites. They are intersex. A dog born with ovotestes would be intersex, not a hermaphrodite. Hermaphrodite is not only offensive when applied to gonochoric organisms, but scientifically incorrect.
For example, an animal like a male calico cat is intersex, and using hermaphrodite would be scientifically wrong and potentially offensive.
Intersexuality is not to be confused for hermaphroditism. They are not the same.
I'm actually going to school for zoology soon so if you have questions about animals I'd love to answer. I know lots about biology in non-human life forms as well.
To recap:
It's okay to call organisms that don't have different sexes hermaphrodites because that is what they are called. (This means an individual organism can and is "supposed" to sexually reproduce with both male and female gametes/sex cells.)
You shouldn't call a gonochoric organism a hermaphrodite, this is offensive. (Gonochoric means that the organism functions on a system of two sexes, male and female. "Opposite" of hermaphrodites.)
Intersex is usually only applied to gonochoric organisms. It is used to refer to an organism that has mixed sex characteristics in an otherwise understood binary sex system of male and female. You may occasionally see it used in reference to hermaphroditic organisms, but this is usually wrong. (There are hermaphrodite organisms that have intersex individuals as a large portion of their population. There are also animals that frequently have intersex individuals as a part of their population. Some scientists believe that these should be classified as another sex, though, as it's a "natural"/"intended" part of the population.)
Examples of organisms you shouldn't call a hermaphrodite:
A female lion who developed a mane later in life. This is intersex.
Female hyenas. Female hyenas have a pseudopenis, very high testosterone/androgens, and are highest in their social caste. This is just how female hyenas are. They are not inherently intersex, either.
Examples of organisms that are hermaphrodites:
Many molluscs, like snails and slugs.
Most plants that flower
Clown fish. Even though they are born as male and become female later on, they are all still hermaphrodites as they don't function on a binary sex system and possess both female and male gametes at one point. (This is called sequential hermaphroditism.)
There are Wikipedia articles on everything I mentioned, but some of the information may be incorrect or misleading. It says that all female moles of certain species are intersex, which I and many others disagree with. Female moles have both ovarian and testicular tissue, but this is an "intended" part of their biology, meaning it isn't a variation of their "intended" sex. It is okay to use the word intersexual to describe this, as intersexual is used to refer to an organism that has sex traits that we usually consider mixed or androgynous (such as ovarian and testicular tissue), but it is something they are "supposed" to have. Such as in a few mole species. However, some people think it is correct to use intersex for animals like this. There is no common consensus. It is important to understand the nuance of how intersex can be used in a given organism and in non-human biology, as it can refer to different things than in humans.
Sorry for answering so much! Zoology is a special interest of mine and I'm planning to go to school for zoology. I also love biology and sexology.
TLDR; There are organisms that are called hermaphrodites because they have male and female gametes. This is not offensive and scientifically correct. Gonochoric organisms (ones that function on a binary male female sex system, like mammals) are not ever to be called hermaphrodites and should be called intersex.
If I made any scientific mistakes and anyone sees, please correct me!
If you have more questions please ask I love talking about biology and zoology.
36 notes
·
View notes
Text
If you have boobs, listen to them.
I’m not great about listening to my body - chronic pain and working manual labor jobs for thirty years mostly make me want it to shut up, because pain is very loud sometimes.
But last June when I was at the doctor for something else (which we still haven’t figured out) that hurt a lot more, he asked if I was having other problems, because he doesn’t often see me.
‘Eh, my left breast has been kind of uncomfortable for a little while?’
Fortunately, he not only listens, but takes things seriously. Diagnostic mammogram, several years before I should have needed them for routine testing.
‘Hmm,’ said the mammogram techs. ‘Let’s biopsy that.’ (‘That’ was an abnormality in my left breast that appeared to be shaped like a piece of macaroni. Amused concern about boob noodles abounded.)
As much as I try to ignore my body is roughly how successful my body actually is at ignoring lidocaine. The biopsy - which was mammogram guided and from a medical technology standpoint, really cool! - hurt like blue blazing fuck.
‘Hmm,’ said the folks who examined the biopsy. ‘That’s weird but doesn’t appear to be cancerous, at least?’
(It still hurt. It continued to hurt worse as time went on.)
It turns out - because there was a history of ovarian cancer from my father’s side of the family and gene testing was done to check for other factors - that I’m also positive for a BRCA 2 mutation that increases my lifetime risk of breast and ovarian cancers to roughly stratospheric levels.
Thanks, dad.
So. Boobs off? Boobs off.
As it turned out, boobs off was going to take a length of time that was becoming increasingly unbearable since the pain in my breast was continuing to get worse.
‘Can we just get the noodle out?’ I asked, rather despairingly, and apparently we could!
Having a section of my boob the size of half a deck of cards excised did not hurt at all, despite my worries following the biopsy.
It did, however, show that I had cancer.
So, boobs are coming off - in a week and a half, actually, which is engendering very complicated emotions (none of them about gender, funnily) followed by chemo, possibly radiation, then reconstruction, since I’m getting it done with my own tissue rather than implants.
It’s going to be a really long year.
So, yeah, listen to your boobs, regardless of sex and gender. Breast cancer hits plenty of men, too.
And if anyone wants to help make my recovery a little easier I have a wishlist?
12 notes
·
View notes
Note
What’s YOUR personal experience with these disorders? :-)
Hello anon! I know I’ve made this post before but it’s buried somewhere. So here it is! Buckle up folks!
I always struggled with bad periods. Heavy flow, horrific cramps, irregular timing. I just thought that’s what it is and everyone deals with it. I figured the pain I experienced trying to use tampons was all in my head, some psychological fear due to my religious upbringing.
It wasn’t until college that I realized maybe my experience wasn’t normal. Maybe people aren’t supposed to be in this much pain. Maybe something was wrong. My pain got to be so overwhelming that I went to the emergency room. After a rather traumatic experience, I was eventually told that I had ovarian cysts and one of them had ruptured, and just go to my OBGYN and take some Advil. (Great advice, wonderful care. /s)
PCOS was in my family history, and my aunts and sisters all struggled with it. My then OBGYN diagnosed me with it, but basically said the same thing as the ER nurses. Take some ibuprofen and birth control and get over it. A diagnosis doesn’t do anything.
I had another episode with cysts about two years later, after I was out of college. I knew what it was this time, and I knew they’d only tell me the same thing. Take Advil and stop crying. So I didn’t bother going to the ER, and I tried to deal with the pain on my own. My (much nicer) OBGYN monitored the two softball sized cysts on my right ovary, and said we’d just keep an eye on them until they went away. That worked for a while, but not for long. One night my mother insisted on taking me to the ER because I was practically screaming in pain. After another traumatic visit, I was, you guessed it, told to take Advil and go home. It was probably another rupture.
Except it wasn’t. The next day I visited my OBGYN for an ultrasound so she could see what was going on. I was called back later that night and told to come in for emergency surgery. The cysts were torsing my ovary and cutting off the blood supply. Very scary situation, I’d never had a big surgery before. I was rushed in for the laparoscopy. This procedure usually takes less than a half hour. For me, I was on the table over two and a half hours. The reason being, not only did I have two huge cysts, but I was discovered to also have endometriosis. The cysts and all my organs had lesions, and everything was fused together. My OBGYN had to scrape the extra tissue from all my organs, she said it was the worst case of endo she’s ever seen, and I must have the highest pain tolerance ever to not be screaming my head off all day long. It was during this surgery I lost my right ovary, dead from having no blood supply.
Recovering from that surgery took me six months. It was brutal and at times, humiliating. My insides were raw and my muscles felt like goo. The only good thing to come out of it was meeting my lovely physical therapist, whom I still talk to today.
Today, five years later, I still deal with PCOS and endo. I have it mostly under control with the depo shot and many other medications. But… I struggle to lose weight, I have high blood pressure, I have major chronic fatigue, I’m at risk for diabetes, I still have migraines and flare ups and GI problems. My health is always going to be a problem for me. I am always going to be battling my hormones. I am going to struggle getting pregnant, if I even can. I am always going to have the risk of losing my other ovary and going into early menopause. I can only pray that these two disorders don’t take away more from me.
#my story#endometriosis#pcos#chronic illness#invisible illness#pcos awareness#endo awareness#pcos symptoms#endo symptoms#chronic pain#chronic fatigue#shitty doctors
11 notes
·
View notes