#Somatic Involuntary
Text

#Musculo#Muscle#Fibra Estriada#Striated Fiber#Fibra Lisa#Smooth Fiber#Involuntario Somático#Somatic Involuntary#Sistema Nervioso#Nervous System#Tendon#Epimisio#Epimysium#Perimisio#Perimysium#Sarcomero#Sarcomere#Miofilamentos#Myofilaments#Miosina#Myosin#Actina#Actin#Núcleo#Core#Nucleus#Sarcolema#Sarcolemma#Miofibra#Myofiber
1 note
·
View note
Text
Arousal and Attraction: How They Coexist with Asexuality
I haven’t posted anything informational in a while, and I’m working on some bigger posts, so I thought I would make a post about these topics as I’ve been thinking a bit about it recently. I will be discussing arousal in the sexual context, making distinctions between the different types of sexual arousal, talking about attraction, and explaining why arousal is not the same as attraction all with a sprinkle of asexuality. One of the motivations for this post was to explain how one can be asexual but also experience arousal and sexual attraction; I wanted to talk about these topics in an asexual context.
Obviously, disclaimer if you’re
uncomfortable reading about this type of thing. I don’t say anything very graphic, but if it makes you too uncomfortable, please don’t read. I am also by no means an expert. I just read some stuff and know some things and want to communicate it to y’all. Without further ado, let’s dive in.
Arousal
Now, arousal in psychology refers to more than sexual kind, namely a physiological reaction to any stimulus, but this post will be focusing on sexual arousal and is meant anytime I use the word arousal.
Arousal can be split into two kind of arousal: physiological arousal and subjective arousal.
Physiological arousal is self-explanatory; someone becomes warmer, their heart starts to race, and blood flow to their genitalia increases amongst other things in order to prepare for sex. This type of arousal is regulated by the autonomic and somatic nervous system. The autonomic nervous system deals with automatic functions, and the somatic nervous system deals with both voluntary and involuntary functions meaning that physiological arousal is uncontrolled and involuntary.
Subjective arousal on the other hand deals more with the mental and psychological aspect of arousal. This is when one’s mind and emotions are positively engaged in sexual activity.
Sexual attraction
Sexual attraction on the other hand is most simply defined as actively wanting to have sex when a specific person. It differs from libido or sex drive which is the general hunger for sex. Someone may feel sexual attraction for a variety of reasons, but they’re taking sexual interest in a specific person.
Arousal versus attraction
Arousal and sexual attraction are not the same; arousal is a physical or mental response to a stimulus, getting turned on whereas sexual attraction took is not merely feeling sexually excited but wanting to have sex with a specific person because they are drawn towards them. It is entirely possible to get turned on by someone and have a physical response but not experience attraction and vice versa. This is called arousal non-concordance.
I also want to make a quick note—sexual arousal and attraction are not the same as sexual desire which is motivation and want to have sex. Being aroused doesn’t mean wanting sex, and even if you were sexually attracted to someone, that doesn’t necessarily mean you actually desire to have sex with them.
Asexuality, arousal, and attraction
Someone can be asexual and be aroused. The definition of asexual is someone who experiences little to no sexual attraction. Arousal is not the same as sexual attraction.
Using the argument of arousal in the physical sense against asexuality does not work as physiological arousal can be completely disconnected from the mental experience. Our bodies are programmed to behave a certain way to certain things and circumstances even if we feel very differently about the matter. Just because asexual people or anyone for that matter experience certain bodily reactions does not mean they’re enjoying an experience, are experiencing sexual attraction or want sex. This argument demonstrates a lack of understanding of asexuality, attraction, and arousal.
Furthermore, if someone experiences sexual attraction, that doesn’t nullify their asexuality. Being asexual is defined as experiencing little to no sexual attraction. That definition allows wiggle room for those who are demisexual, fraysexual, graysexual, whatever. Experiencing sexual attraction still falls under the umbrella of asexuality.
I hope you were able to learn something from this and it didn’t feel too disconnected! It’s my wish that this helps people to better understand these terms, exactly what they mean, and how asexuality intersects with these topics! I would definitely encourage researching anything talked about here more on your own if it interests you, but I have linked some resources and articles covering what I’ve discussed here in more detail.
Resources:
American Psychological Association definition of sexual arousal
NCBI Understanding Arousal
AVEN Defining Arousal vs attraction
itsbido Sexual arousal vs. attraction: what’s the difference?
Embrace Sexual Wellness, LLC. Arousal Non-Concordance: It’s More Common Than You Would Think
AVEN: The Gray Area, Sex and Related Discussions subforum post regarding arousal non-concordance and asexuality
The truth about unwanted arousal Emily Nagoski TED Talk
AVEN post on the Frequently Asked Questions Thread about what sexual attraction took is and more
Sex Positive Psychology: Sexual Desire and Arousal - Same or Different?
#asexual#asexuality#acespec#asexual spectrum#ace spec#aspec#ace#asexual info#sort of#the content is not just for aces#but i geared it towards aces
9 notes
·
View notes
Note
i wish you the best in your journey forward ... and i hope that though watching you i can convince myself that i'm not a lost cause. i haven't been able to play the piano for a very long time due to nerve damage in my arms. when i do play now, it's slow and clumsy. i hate it. it does feel like an existential betrayal, but my body didn't do this to me on purpose. i think i just have to take it day by day. have the same patience my teachers had with me when i was a child. take care of yourself, and thank you for being open about your experiences. 🤍
i believe with all my heart that you are not a lost cause, that with some time and patience (and limitless amounts of kindness to yourself) that you can make progress in your playing again.
toward the end of my master's degree, i developed a startle response in my voice, in my vocal onset. an involuntary throat constriction that ultimately took my ability to sing, to produce any sound at all. it spread from my auditions and performances until even the thought of my practice began to produce this response in my body. eventually the thought of singing brought me more grief than joy and i lost the desire completely. i felt like a ghost, an imitation of myself because i had no self separate from my identity as a singer/musician.
it's different, of course, from this past year of infections that have affected my body and reduced my ability to sing. but how i have approached my practice is the same: my therapist reminds me that whether it is a self-protective somatic mechanism or whether it is from illness: my body is constantly working to heal, my mind is capable of rewiring neural pathways, and what cannot be healed (or returned to its previous state) can be managed with adapting. either the situation can change, or how i approach the situation can change. approaching my practice with the mindset that i am not here to judge my progress, only to make some progress.
a huge bridge between me and singing was reaching out to some voice teachers who were recommended to me by someone in the classical music world that i trusted. i explained that i was rehabilitating my voice after some time away and once we met in person, was able to explain in more detail what had happened. they were able to approach my lessons in a way that gave me the safety i needed to make progress. i was drowning alone. i don't know if reaching out to some local teachers is possible for you — whether you have the financial stability to spend some extra money every few weeks or whether you have anyone you can trust. but if you can, i cannot overstate how much support it gave me to have a mentor again, to have someone to guide me back.
sending you all my love. i am right here with you in this. and thank you so much for sharing this with me. it means the world to me <3
31 notes
·
View notes
Text
I might just be being sensitive here, but I really dislike it when people make jokes about lobotomies, hysteria, and other such psychiatric practices considered outdated in the present day. I feel like people feel comfortable making these jokes because they believe psychiatric abuse to be a thing of the past, and that anyone who claims to have experienced it in the present is either lying or “crazy” (and therefore deserved it).
In many feminist circles in particular, people often talk about hysteria as something that “normal” (non-disabled) women were diagnosed with because men understand nothing about the women’s bodies. On here a few months ago I saw someone respond to a 19th century psychiatric illustration depicting a “hysterical fit” by joking that the patient was probably just having an orgasm but the doctor didn’t know what that was. To those who make jokes such as these, I want to ask: what if some of the women diagnosed with “hysterical fits” or “hysterical paralysis” were genuinely having medically unexplained seizures or paralysis? What if the woman Charcot describes having episodes where she seems to see and talk to a person who wasn’t there was genuinely hallucinating? Then would you think it was okay to lock them up in hospitals indefinitely? To administer treatments without their consent? Would you even characterize this as “getting them the help they need”? I feel like feminists who have never experienced forced psychiatry firsthand want to identify with the victims of 19th and early 20th century psychiatry without having to think about the ways the abusive practices of that era persist in many of the psychiatric practices of today: involuntary holds, forced medication, discrediting the voices of people with psychiatric diagnoses, etc. That would require aligning themselves with people they’ve been taught to fear. People who experience delusions, who have been diagnosed with personality disorders, who hallucinate. On the whole, there is a failure on the part of many feminists to recognize the diagnosis of hysteria (and modern hysteria-adjacent diagnoses like somatic symptom disorder and many more) as a place where the oppression of women and the oppression of psychiatric patients intersects, in a large part because they don’t even believe the latter exists.
I realize that at the top of this post I mentioned lobotomies and hysteria and then only talked about hysteria. That’s mostly because hysteria is a topic I’ve read much more about, but maybe sometime when I’m more educated I will make a post about lobotomies. Anyways. Please read literally anything by Judi Chamberlin.
#to be clear i do consider myself a feminist. i criticize current feminism because i want it to improve.#psychiatry & antipsychiatry#patriarchy
5 notes
·
View notes
Text
My Favourite TS/Tics Facts from my Textbooks
((pdf links to the full text-books at end))
-The repertoire, frequency, and intensity of tics typically fluctuates over time. This helps distinguish between Stereotypies (Stimming; hand-flapping, rocking, etc) which are more stable in quality, time duration, and interference with motor behaviour.
-Typically, tics correspond to parts of learned automatic routines; clapping, blinking, exclaimations, shrugging, etc.,.
-Simple tics typically appear first, slowly progessing into Complex tics
-Tics tend to have a cranio (head) - caudal (tail) spread over-time. Often times tics first involve the cranial (head/face) and cervical (neck-shoulders) musculature first; occular (eye) movements, shoulder shrugging, neck jerking, etc.,. Later including involuntary movements in the truncal and limb areas.
-The most common sensory phenonmena in TS/Tics is Premonitory Urges. Premonitory urges are defined as unpleasant somatic (bodily) sensations that typically build up just before a tic, and are relieved after a tic is completed.
-Premonitory Urges are often described by patients as more distressing than the tics themselves, and are more commonly described by adult patients.
-Predominant sites for Premonitory Urgers are: palms, throat, shoulders, and midline abdomen.
-Some patients experience what is called the ‘Just Right’ phenomena. It is another form of sensory phenomena that is defined by the need to compulsively repeat sensory experiences until they feel ‘just right’.
-Patients with Echophenomenon (Echolalia, Echopraxia, Palilalia, Palapraxia, Coprolalia, Copropraxia) have a higher association with an increased tic severity.
-Coprolalia and complex tics seem to be a prominent features of Tourettes patients, suggesting that these are typical features of Tourettes Syndrome.
-Coprolalia may be up to as 3x as likely as copropraxia, typically onsetting around age 11 years.
-Some patients display NOSIBs (Non-Obscene Socially Innapropriate Behaviours) such as commenting on someones height, weight, appearence, etc.,.
-Many patients report that their tics are partly, or wholly, voluntary in character, and are performed in response to an irresistible urge to make the movement/sound.
-Tic severity tends to peak at 10-12 years old. Adolescents and early adulthood can lead to a decline in the severity of tics.
-There is evidence to support subtle structural changes in the Basal Ganglia and Corpus Callosum in the brain. It is hypothesised that this leads to changes in brain function, specifically within the corticostriatothalamocortical circuits.
-Frequently, tics are less pronounced at school compared to at home, albeit at the cost of reduced attention and increased irritability.
-----------------
Textbooks: Advances in the Neurochemistry and Neuropharmacology of Tourettes Syndrome and Canadian Guidelines for the Evidence Based Treatment of Tourette Syndrome
145 notes
·
View notes
Text
Secret Santa Gift: @inscrutable-shadow
This is a Secret Santa event so there will be a blanket trigger warning for all entries, so read at your own risk! Potential trigger warnings may include nsfw themes as well as gore and possible squicks.
TRANSCRIPT BEGINS:
[0:00:00] The click of a recorder turning on. Brief moment of silence, broken only by humming background noise.
[0:00:07] A voice begins to speak.
VOICE: Audio log begins. Current time 0600 hours, current date 43/30. Experimental subject: Dr. Fairbank, AKA myself. Blood pressure 115 over 73, pulse oximeter indicates a resting heart rate of 84-- higher than expected, but that's likely due to prior caffeine ingestion-- and oxygen saturation of 98. All within normal ranges. Experiment nature: vivisection of the peripheral nervous system, mainly the major motor nerves, of the lower left arm.
[0:00:28] A metallic sound-- source unknown.
DOCTOR FAIRBANK (DR.): I've chosen to give real-time updates on the experience of the surgery. Since all prior nervous system dissections have been performed on cadavers-- for obvious reasons-- an examination of the peripheral nervous system in the limbs in a living subject will provide valuable and potentially actionable biomedical information. Limb loss is uncommon, but the lack of regenerative potential in such situations does raise the question of developing effective prostheses should the occasion arise.
[0:00:53] A slow exhale.
DR.: Some introductory information. The peripheral nervous system is the portion of the nervous system that transmits information to and from the central nervous system, which consists mostly of the spinal cord and brain. It is divided into two subsections: the autonomic nervous system, which controls involuntary processes such as smooth muscle movement, blood pressure, breathing, etc., and the somatic nervous system, which controls skeletal muscle movement. I will be focusing on the three major motor nerves in the lower arm, which are components of the somatic nervous system.
I've chosen to use myself as the subject for this particular experiment. While this may compromise the experiment's objectivity, subjective observations are equally-- if not more-- useful in this case, and I doubt any other subject would remain lucid enough during this or any similar surgery to provide observations on the duration, quality, and level of pain. As this is the case, I will be performing the surgery unmedicated.
[0:02:27] A sigh.
DR.: This will be... a long process.
[0:02:30] Beat. They continue.
DR.: In order to assess the state of the peripheral nervous system in my lower left arm prior to this study, I performed several nerve conduction studies, intended to assess the speed at which electrical impulses currently travel. I placed the distal electrode in the center of my palm and the proximal electrode approximately 3 cm above my elbow, then measured conduction time and amplitude between the two. These results indicate my nerve conduction baseline and have been recorded in photo format.
For the following experiment, I have, for simplicity's sake, immobilized my arm utilizing a standard table vice. I suspect that I may need to change position during the surgery, but hopefully complications will be few.
I've decided that in order to gain useful information through this surgery, I would need to observe the nerves on a fairly large... canvas, so to speak, for better visibility of both the major motor nerves themselves and the effects of manipulating them. As that is the case, I will be beginning at points near the wrist and making several incisions, which will vary in positioning and length depending on the motor nerve I'm attempting to access.
I had initially planned at beginning at a more distal point-- the hand or possibly even the fingertips-- but those scenarios introduced significant limitations; most of the nerves in those areas are sensory nerves, and the motor nerves I'm most interested in are harder to access, so information would be sparse. Therefore, this is the method I chose. I've also used fluorescent peptides to tag the nerves in question, so that the visuals will be clearer and I won't risk more severe damage.
The time is currently...
[0:03:12] Brief beat, presumably a result of them turning to face the clock.
DR.: The time is currently 0604 hours. Mark beginning of surgery.
[0:03:17] The sound of a sterile instrument being removed from its package, followed by a quiet sound and an intake of breath.
--
[05:12:57] Heavy, rasping breaths for a moment, before commentary resumes. Their voice is breathy, but otherwise devoid of indicators of pain.
DR.: I've begun the surgery by exposing the median nerve, which is the main nerve controlling the first two fingers and thumb, as well as approximately half of the ring finger.
I've chosen the median nerve because it's the easiest of the three major motor nerves to access from my current position. The median and ulnar nerves both run through the underside of the carpal bones into the palm of the hand, but the median nerve runs through the carpal tunnel, which is a central area dense with tendons. It's also very close to the surface, hence why most compression of the median nerve happens at the wrist-- carpal tunnel syndrome. The ulnar nerve is somewhat deeper, so I've decided to save it for later.
[05:15:09] A long pause, with several somewhat wet noises, as they examine the surgical site.
DR.: I've restricted blood flow to the area using a tourniquet. Under normal lighting, I can see some red muscle tissue and yellow fat, as well as the tendons of the area, which are a very clean, shiny white. At the most distal edge of the cut, closest to the palm, the tendons disappear under the transverse carpal ligament, which stretches laterally across the carpal tunnel. The median nerve is slightly difficult to make out within the bundle of tendons, but I've set up an overhead blacklight prior to beginning this experiment.
[05:17:13] A click, presumably the sound of the blacklight turning on.
DR.: Switching it on tells me that the fluorescence has been very helpful indeed. The nerve is immediately obvious against its surroundings, glowing green under the UV light.
Current pain is typical of surgical cuts without anesthetic; the stinging pain of cutting skin, and the deeper ache of muscle and tissue being separated. It's not particularly notable, though interestingly as the cut is shallower the pain does feel somewhat... sharper. As always, descriptors are difficult.
I will now proceed to stimulate the median nerve via physical touch.
[05:18:25] Another noise, meatier than the others, followed by an inhale through teeth.
DR.: Oh. Ah. Well. I'd been expecting that, but it's still somewhat unpleasant.
[05:17:53] They clear their throat.
DR.: Even a slight compression of the median nerve creates a painful feeling of pressure extending both outwards, into the thumb and first three digits, and inwards towards the elbow. It also produces paresthesia, in a form that I would describe as a sort of tingling numbness-- not quite the pins and needles of restricted blood flow, but still uncomfortable. It cuts through the rest of the pain and creates a sensation that I would characterize as feeling near-freezing, though I have heard others describe it as a burning sensation.
[05:20:01] Their voice turns dry.
DR.: According to the traditional pain scale, my pain would rank as a 4; distracting, but I can continue my usual activities. I believe that accurately highlights the limits of the pain scale.
[05:20:56] Brief beat before continuing, in a more inquiring tone.
DR.: I wonder... I hadn't planned on stimulation via electricity, but given that I still have materials from my nerve conduction study on hand to be repurposed, and that the median nerve is so relevant for muscular control in the hand... One moment.
[05:23:23] The sound of cloth rustling, and a quiet clink, most likely the sound of a surgical instrument being laid down on a metal tray. Some other miscellaneous noises, including a quiet groan that cuts off abruptly into silence. Something being dragged over the ground.
[05:25:49] A moment of panting before they resume speaking, their voice clipped.
DR.: I've acquired the nerve conduction equipment from its prior position. I now plan to place the stimulating electrode directly at the median nerve and observe the effects.
[05:26:38] A grunt, and the sound of a switch flicking. They gasp, briefly.
DR.: The muscles in my thumb and first three fingers are-- are spasming, as are some of the minor muscles in my palm. I can see my tendons tensing as the fingers and wrist attempt to curl. There's the pain of the electricity; it's mild in comparison, but does twinge a bit. Interestingly, however, the pain mostly originates from the muscle spasms, rather than any new nerve pain or paresthesia. It's a strange feeling, almost cramp-like, and though they were initially mostly painless, the pain is increasing in intensity as I keep the electrode placed at my wrist. I will now turn off the current and remove the electrode.
[05:27:14] Another click, and several quiet, indistinct noises. When they speak next, their voice is tinged with relief.
DR.: Fascinating information so far. I'm going to use the free-standing magnification that I set up to take some pictures of the surgical site before I suture it, then reposition slightly and work on the ulnar nerve.
--
[11:47:19] Breathing has become more measured. In-between breaths, the quiet, wet sound-- presumably of the scalpel cutting through flesh-- can still be heard.
DR.: The speed of my work has increased somewhat as I become more comfortable with the surgery. Still, I have to exercise caution. Too fast and I might cause damage that would take too long to heal for my liking. Additionally, I suspect both my speed and my accuracy may decline as I continue to work.
[11:48:02] Swallowing sound.
DR.: I suppose we'll see.
[11:48:07] The sound stops, followed by a series of deliberately slow, even breaths.
DR.: Of the three major motor nerves of the lower arm, the ulnar nerve is the second most accessible at the wrist. Really, it would be easier to access at the elbow; it's very close to the surface there, as anyone who hits their quote-unquote "funny bone" would know. However, as I'm doing this surgery on myself, accessing the nerve at the cubital tunnel would require a very annoying angle, as well as impeding visibility. Hence, the wrist.
The ulnar nerve controls the pinky finger and the half of the ring finger that the median nerve doesn't control, as well as other minor muscles in the hand. Most often compression at the nerve happens at the elbow, a condition called cubital tunnel syndrome, but direct trauma can also cause ulnar nerve entrapment at the wrist.
[11:49:47] They click their tongue thoughtfully.
DR.: The incision I've made to examine the ulnar nerve is similar to that of the median nerve, but necessarily deeper. The median nerve is very close to the surface as it travels through the forearm and passes through the carpal bones, but the ulnar nerve passes through what's called Guyon's canal or the ulnar tunnel, which is somewhat deeper and harder to access. I briefly removed the tourniquet in the time between suturing the incision I made for the median nerve and beginning the ulnar nerve incision in order to avoid unintentional and unrelated numbness, but have now returned to restricting blood flow.
Due to the deeper cut, more muscle tissue and fat are visible around the tendons and ulnar tunnel-- more red, more yellow, less white. However...
[11:52:18] A click as the blacklight switches on.
DR.: ...the blacklight and fluorescent tagging still allows for a very visible ulnar nerve. That was a very good move on my part, if I should say so myself.
The pain of this incision in general lacks the sharp, stinging sensation of the shallower median nerve cut, instead being deeper and carrying the sense of... well. To get very subjective, it carries the sense of wrongness that all deep incisions have. Pain is a response to a great many things, but with particularly deep wounds there's also a feeling that something that should be a continuous whole no longer is, and while the body obviously doesn't like that it's also never sure exactly how to respond.
[11:54:58] Beat.
DR.: Now, moving on to the stimulation portion.
[11:55:06] More heavy, meaty sounds. When they speak, their voice is tight.
DR.: Ah. Hm. I had expected the pain to be similar in quality to the median nerve, but it seems I was too presumptuous. Palpating the ulnar nerve causes a somewhat similar pressure and paresthesia, but stronger and more noticeably painful, and while it does radiate into the fingers served by the ulnar nerve it's also extremely obvious at the elbow. Again, the feeling that I would describe as being temperature-adjacent, almost cold. If I tap on it--
[11:57:38] A quiet, muffled thump, followed by an intake of breath.
DR.: --I notice that it creates a shock, of the same quality that I would associate with hitting my elbow in a way that would temporarily traumatize the ulnar nerve. And, in retrospect, I wish I'd done the same to the median nerve.
Ah, well. It's too much work to undo the sutures now. Time for electric stimulation.
[11:59:10] The slick sound of the electrode being pushed into the incision, then a switch flips. Brief moment of silence broken only by the sound of teeth grinding.
DR.: Some results similar to electrical stimulation of the median nerve. The muscles in my hand are contorted, and my ring and pinky fingers have seized. Muscle spasm pain and electrical pain aren't noticeably different in quality or quantity in the hand and fingers. However, I am now experiencing pain in the elbow and in the lower parts of the upper arm, as my muscles have tensed in that area as well. I'm unsure as to why-- am I reacting to the pain I'm experiencing? Is the ulnar nerve stimulating nerves of the upper arm?-- but I'm making a note of it.
Turning off the electricity... now.
[12:02:37] Switch flips again.
DR.: Once again, photos, sutures, and then reposition for the radial nerve. We're nearing the home stretch now.
--
[15:34:39] Muffled cursing.
--
[15:52:44] A grunt of pain, cut off short. After a long period of silence, they begin to speak again.
DR.: We've-- ah-- we've run into an issue.
The radial nerve doesn't pass over the underside of the arm; rather, it passes through the outside of the arm, almost aligned with the thumb, and takes a more winding path. Accordingly, I had to reposition my arm and make yet another incision. The angle of approach would have been somewhat awkward no matter what I did, so I eventually decided to begin this portion of the surgery, and... well.
Mostly, the nerve is intact. However, as the radial nerve is responsible for straightening the wrist, damage to it-- in addition to being shockingly painful-- can cause something called "wrist drop", which is exactly what it sounds like.
[15:55:28] They let out an annoyed hiss.
DR: Given the current state of my arm, observation and palpation of the nerve in question is more... difficult... than I would like it to be. The natural state of the wrist is partially flexed, and the radial nerve is required to stimulate the extensor muscles enough to counteract the flexor muscles and straighten it. Due to the damage, my wrist is now partially contracted. In addition, the pain in my arm and hand has increased significantly, and while I'm not exactly a stranger to pain, it's still not what I would consider a good feeling.
[15:57:23] The sound of something tapping rapidly on a metal surface, accompanied by thoughtful sounds.
DR.: On the other hand... this may be good. I can assess what damage feels like in comparison to mere pressure and electrical stimulation. So, in that case...
[15:57:41] They sigh.
DR.: The sensation is a far, far more intense version of the paresthesia that I experienced with compression on the median and ulnar nerves, accompanied with significantly more numbness. It also lacks the sensation of pressure that palpating the median and ulnar nerves did.
A large portion of my arm has lost feeling almost entirely, and other portions are... painful. As noted, I can't fully straighten my wrist or bend it backwards, and while I can control most of my fingers as usual, I can't bend my thumb fully backwards.
It's unpleasant, and unfortunate, but I suppose at this point there's nothing to do but end the procedure and wait. Fortunately for me, time will heal all my wounds.
--
[17:09:38] They begin, once again, to speak. Their voice is more composed and slightly less strained overall.
DR.: I've been able to document several useful observations from this procedure.
First, as previously known, the Vitalichryne Engine provides some resistance to nerve damage. Despite the incident with the radial nerve, the degree to which nerve damage can be resisted did allow me to view more of the motor nerves than I may have otherwise been able to, all without serious issue. While the radial nerve was damaged, it was damaged far less severely in me than I suspect it would have been in someone entirely lacking regenerative abilities, and I suspect it will heal completely and quickly.
Secondly, and more importantly, examination of the median and ulnar nerves brought me to an interesting observation, which is that, if things weren't as they are, I would have carpal tunnel syndrome.
To explain further, carpal tunnel syndrome is caused by a variety of things. Among them, repetitive hand or wrist motions rank very highly. I do nothing but repetitive hand and wrist motions, and though my left hand gets slightly less of it, it would still make sense for the tunnel in question to be irritated, potentially enough to put pressure on the median nerve. And, in fact, I could see some inflammation, but it was extremely minor and hasn't been affecting my nerves or my work at all.
[17:08:41] A touch of amusement enters their voice.
DR.: I suspect that, in the hypothetical universe where I could or wanted to take more breaks, the issue would heal completely with no issues.
[17:09:01] Tone switches back to brisk, businesslike.
DR. Both of these observations bring me to some further questions about the means by which acute and chronic nerve damage is prevented and the degree to which minor and major trauma impact the nerve in question, but also have implications for the potential future development of prosthetics in the event of limb loss. As nerves are resistant to damage and experience easier regrowth, it may be possible to create bio-synthetic prosthetics that have a far less limited range of motion and even sensation than currently suspected.
[17:10:25] Their voice changes again, this time sounding pleased.
DR.: This study was both satisfying and enlightening. But, as I suspected it would, it raised more questions than it answered, and these questions can't be answered by auto-vivisection. Though it means sacrificing some subjective data on sensations, I'd really need other patients to gather truly extensive data on the peripheral nervous system.
Or, depending on where my research takes me, the central nervous system. We'll just have to see.
[17:11:38] A click, and the recorder turns off.
TRANSCRIPT ENDS.
7 notes
·
View notes
Text
am i concerned enough about other people? am i concerned enough about lives, experiences, and existences that aren’t my own? if i can’t relate, do i enjoy listening? have i been projecting my experiences onto everyone as if they’re universal? is that childish and naive? am i a cynic? am i skeptic? are my experiences universal? am i wise? what does it mean to be concerned about another person? what makes concern different than worry? is concern a choice? is worry involuntary? is anything really voluntary (life itself?)? do i believe i should be more concerned with other people: should i be more concerned with other people? how concerned am i about other people? how much does intention matter? is every answer an individuated perspective? am i seeking the universal through the particular? what is the universal? are my experiences? are other people universal? what constitutes the universe? is space part of the universe? is the galaxy the universe? Is the universe all the galaxies? aren’t we from one singular galaxy most of us haven’t had the chance to explore outside the atmosphere of? how did humans begin to start using the word “universal?” what is the etymology of the word universal and when did it become common language? how does vernacular rise to popularity? does specificity have a value (positive or negative?) will specific answers receive specific questions? what is the relationship between a question and an answer? how many ways are there to answer this question? how can i become more concerned about other people? how can i feel more connected to other people? how can i express my love to other people? do i love everyone? who do i love? why do i love them? do they love me? why do they love me? does love ever stop? what really is an ending? is everything always ending or is it always going? is the top of a circle no different than the bottom of a circle? is a circle a physical thing or is the only physical thing a representation of a circle? is a sphere a circle? why is math important? would knowing math improve my life? how do i show other people I’m concerned about them? am i concerned about them? do i care about myself more than anything else? is that bad? do i want to be good? why do i want to be good? how often do i think about other people? how often do i think about strangers? is there a reason to think of strangers? is there a reason to think of people you haven’t spoken to in months and don’t plan to speak to in the future? is there a reason to think of people you’ve never spoken to and can never speak to verbally? how abstract are your thoughts? how does one express concern abstractly and how does one express concern physically? how does absurdity make you feel? what does freedom mean to you? are you connected with other people? do i scare you? do you feel anything for me? do you know what love feels like? do you miss being in love? do you know who you are? do you think i’m pretty to look at? do you think i’m doing something for you? does it make you happy to please other people? how do you know what pleasure is? can you describe how you know something feels good? somatically? abstractly? can you tell me where the feelings start in your body? how do you feel about words? how do you feel about using your mouth to say words? how do you feel about using your mouth to eat? do these things matter to you? what matters to you? do you want to smoke right now? do you want to order food? do you want to watch a movie? how do you pick movies you like? how do you watch them (computer, tv, cinema?) do you like to review movies? why? do you like to read other people’s opinions? why? does it make you feel more connected to other people? does it make you feel more connected to your self? do you use other people to understand your self? am i you? am i using you? am i guilty? am i wrong? am i bad? am i good? how can i be better?
1 note
·
View note
Text
Psychopathology, Ch 2 pt. 1
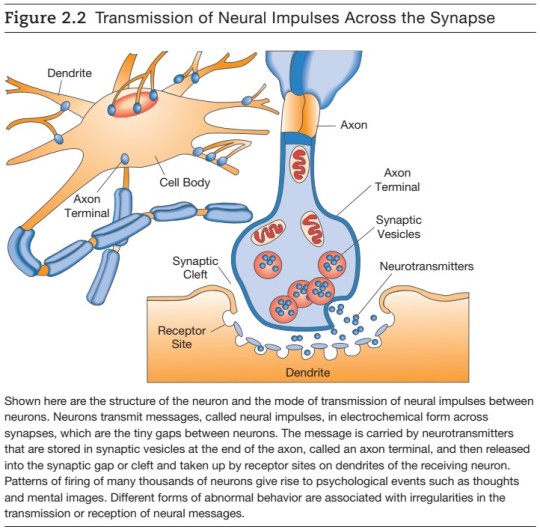
Identify the major parts of the neuron, the nervous system, and the cerebral cortex. Describe their functions.

Neurons: nerve cells.
Dendrites: the rootlike structures at the ends of neurons that receive nerve impulses from other neurons.
Axon: the long, thin part of a neuron along which nerve impulses travel.
Terminals: the small branching structures at the tips of axons.
Myelin sheath: the insulating layer or protective coating of the axon that helps speed transmission of nerve impulses.
Neurotransmitters: chemical substances that transmit messages from one neuron to another.
Synapse: the junction between one neuron and another through which nerve impulses pass.
Receptor site: a part of a dendrite on a receiving neuron that is structured to receive a neurotransmitter.
Central nervous system: the brain and spinal cord.
Peripheral nervous system: the somatic and autonomic nervous systems.

Medulla: an area of the hindbrain involved in regulation of heartbeat, respiration, and blood pressure.
Pons: a structure in the hindbrain involved in body movements, attention, sleep, and respiration.
Cerebellum: a structure in the hindbrain involved in coordination and balance.
Reticular activating system (RAS): brain structure involved in processes of attention, sleep, and arousal.
Thalamus: a structure in the forebrain involved in relaying sensory information to the cortex and in regulating sleep and attention.
Hypothalamus: a structure in the forebrain involved in regulating body temperature, emotion, and motivation.
Limbic system: a group of forebrain structures involved in emotional processing, memory, and basic drives such as hunger, thirst, and aggression.
Basal ganglia: an assemblage of neurons at the base of the forebrain involved in regulating postural movements and coordination.
Cerebrum: the large mass of the forebrain, consisting of the two cerebral hemispheres.
Cerebral cortex: the wrinkled surface area of the cerebrum responsible for processing sensory stimuli and controlling higher mental functions such as thinking and use of language.
Somatic nervous system: the division of the peripheral nervous system that relays information from the sense organs to the brain and transmits messages from the brain to the skeletal muscles.
Autonomic nervous system (ANS): the division of the peripheral nervous system that regulates the activities of the glands and involuntary functions.
Sympathetic nervous system: the division of the autonomic nervous system whose activity leads to heightened states of arousal.
Parasympathetic nervous system: the division of the autonomic nervous system whose activity reduces states of arousal and regulates bodily processes that replenish energy reserves.

Epigenetics: the study of heritable changes in processes affecting gene expression that occur without changes in the DNA itself, the chemical material that houses the genetic code.
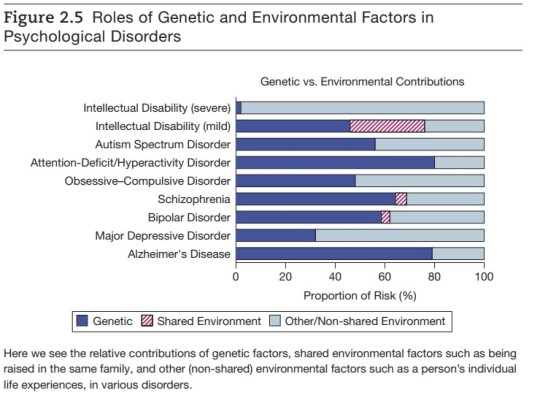
Things to Remember in the “Nature vs. Nurture” Debate
Genes do not dictate behavioral outcomes.
Genetic factors create a predisposition or likelihood - not a certainty - that certain behaviors or disorders will develop.
Multigenic determinism affects psychological disorders. Scientists have yet to find ANY psychological disorder that can be explained by defects or variations of a single gene.
Genetic factors and environmental influence interact with each other in shaping our personalities and determining our vulnerability to a range of psychological disorders.
2 notes
·
View notes
Text
hate the perception of anxiety disorders, of panic disorders, somatic disorderes. cops came by today due to the involuntary screaming during them. i feel embarrassed
0 notes
Note
Tw - about flashbacks and SA and little details of SA
Looking for: opinions but also just venting.
Call me Jaguar.
I don’t even know WHAT SOME OF MY TRIGGERS ARE!!! I LEGIT HAVE TO GUESS. I think certain things revolving around night time had triggered a certain somatic flashback before so I try to make sure to avoid what I think triggered me?
I haven’t had that particular flashback in awhile so maybe I can self trigger and see if it is what I think it is… I’m scared thinking about experiencing it again but I wanna see…
I can’t pin triggers at all. Never know where it comes from, some triggers are obvious like seeing abusers in person.
Some episodes I get idk what they are or if they’re just depressive/other episodes. Like I can get into intense depressive episodes that make me feel odd emotions I can’t describe. Idk where they come from or why they’re there. It’s like an intense sadness mixed with feeling dissociated and out of place, gross, in a way. Idk what this even is!
There are flashbacks I haven’t had in a long time and I’m really trying to figure out was it even a flashback? Why did they show up and why haven’t I seen them in a while? I was told it was a somatic one because of the SA hallucinations and how real they were on my body… the things I felt were obviously SA I thought someone was in bed with me but nobody was. One of those flashbacks was SA of vaginal somatic experiences…
…Was I triggered by thinking about the trauma memory from my childhood? Bc it was on my mind at the time the somatic flashback hit me and I was contemplating certain details from the memory…I typically avoid all memories even though they intrude on me.m but it had me thinking…
was I triggered by certain things revolving around night time? Bc I am avoiding those things atm in case it is. I think certain things about night time trigger me so I don’t go near it.
But I seem to have no experienced particular flashbacks in awhile?
I had to rearrange my room and do so many things differently at night to not feel so depressed or awful which has helped with bad episodes like that.
I really don’t know what these experiences even are. I don’t know how to label them. Or if it’s just a type of depression, Idk…
Hey Jaguar,
Please know that it's normal to not fully know what your triggers are. Sometimes our brains will recognize something as a threat that, on a conscious level, we aren't even aware of. While it can be helpful to try and figure out what your triggers are, self triggering is a dangerous way to go about this.
It's possible that the sudden onset of intense emotions could be an emotional flashback, which can be described as a rush of intense emotions related to a past traumatic event that occur without any visual memories or images. Alternatively, experiencing a flashback in which you can physically feel certain sensations related to the traumatic memory can be a somatic or sensory flashback. It's important to distinguish this from a hallucination because a hallucination is typically a perception of something that is not present in reality, while a flashback is a vivid and involuntary recollection of a past event or experience. There is some overlap, but I think that distinguishing flashbacks from hallucinations can be validating.
It's possible that things such as thinking about traumatic childhood memories or certain things about nighttime could've influenced being triggered at that time, but it's ultimately up to you to make that determination.
If you can access or afford it, a mental health professional such as a therapist can help explore your trauma in a safe and controlled setting, as well as navigate these flashbacks and collaborate with you to construct some healthy coping mechanisms that you can take with you along your healing journey. In the meantime, I do hope that I could help name some of your experiences, and please know that we're here for you if you need anything.
-Bun
0 notes
Text
Effects of Sleep Deprivation and How to Fix It?

Sleep deprivation-a term that describes a state or situation caused by insufficient quantity or quality of sleep taken by an individual. An inadequate amount of sleep or insufficient sleep makes you feel drowsy throughout the day and affects your mental and physical health.
Lack of sleep can be either due to circadian rhythm sleep disorders or involuntary and voluntary sleeplessness it eventually affects you. Short-term effects of sleep deprivation include somatic pain, emotional disorders, and performance deficits.
According to the Centres for disease control and Prevention, a quality sleep of 7 hours is essential for every individual. Occasional interruptions to sleep can be a nuisance and lead to sleep deprivation.
An ongoing lack of sleep affects a person’s productivity and mental health; to know more about the effects of sleep deprivation on your brain, go through the complete article.
Effects of Sleep Deprivation on the Brain
One of the most treacherous effects of sleep deprivation on the brain is that it not only affects cognitive but also emotional issues. This results in conflicting feelings of depression and euphoria.
If you are encountering constant yawning, grogginess while waking up in the morning, and the tendency of dozing off throughout the day, these are relatable sleep deprivation symptoms.
Sleep deprivation symptoms may vary in children and adults like children experiencing irritability, temper tantrums, hyperactive behavior, and reluctance to get off the bed.
Let’s discuss the major effects of sleep deprivation of which you need to be aware:
Hypertension: It is already proven that sleep controls body hormones by regulating stress and the metabolism. A continuity of poor sleep can cause swings in hormone and eventually leads to high blood pressure and another risk for heart disease.
Heart Attack and Stroke: Continuous sleep apnea can affect your heart health too. It affects the amount of oxygen we take during sleep and causes several health issues and heart failure.
Immune system deficiency: A healthy and quality sleep is hypothesized to have a restorative function on the immune system of your body. Severity disorder in sleep accordingly correlates with the decline of cellular immunity that is associated with the alterations in the complex cytokine network.
Depression and Anxiety: Undoubtedly, lack of quality sleep affects your mental health and reduces your productivity. Sleep Apnea also leads to temporary changes in mood and cognition and is also associated with reduced cerebral metabolism.
Psychiatric disorder: Lack of sleep is ultimately linked to a number of unfavorable health consequences under which psychiatric disorders. A long-term sleep deprivation tends to several consequences that eventually led to symptoms like disorientation, hallucinations, and paranoia.
Weight gain and Obesity: Several studies show that an inadequate quantity of sleep leads to obesity. As sleeplessness drop down the leptin level in one’s body triggers hunger and makes you feel less satiated after eating. Poor sleep tends to increase fat storage in the belly area and also higher the mass index of the body with decreased insulin sensitivity.
Decreased fertility: Sleep deprivation produces a commensurate effect on the health of women by reducing their fertility rate. Inadequate sleep in women suppresses melatonin production and excessively activates HPA. This results in failed embryo implantation, amenorrhea, early pregnancy loss, and anovulation.
Faulty Brain function: One of the major effects of sleep deprivation is a fault in brain function. It makes you moody and irritable and impairs the functions of the brain. If the brain is not getting enough rest and sleep, it drastically affects the overall health of an individual and tends to the effects of sleep deprivation in psychology.
Diabetes: Diabetes is one such prolonged condition with no cure, it is treated with medication. Studies show that long-term sleep may disrupt the body’s method of processing glucose. It gradually increases insulin resistance and accelerates blood sugar in the body.
As the condition tends to have a drastic effect on one’s life it is important for us to know how to fix sleep deprivation. There are a lot of factors that one can consider to fix the concern and get restful sleep of 7-9 hours.
How to Fix Sleep Deprivation?
Indulging some lifestyle changes in daily routine may results in promoting good sleep and eliminate the symptoms of sleep deprivation. After keeping a few things in mind and adopting a healthy lifestyle you can fix the sleep deprivation. These are:
Avoid Caffeine later in the day
Don’t end up your day with alcohol
Do regular physical activity
Make a pleasant sleep environment
Do not take large meals within 2 hours of sleep time.
Create a sleep-wake routine
Avoid using blue light devices before naptime
Try to take a light dinner
Include Sleep boosting supplements in the diet
In order to get restful sleep, practicing these lifestyle changes on a regular basis surely delivers the expected outcomes. However, combining the best sleep-boosting pills can also be an option.
Noocube Sleep Upgrade is one such sleep supplement that enhances the quality of sleep. It’s a melatonin-free supplement that naturally promotes the production of the hormone to improve sleep quality. In order to consider the supplement in your routine, prefer to know Noocube sleep upgrade reviews to know further about its effectiveness and the working mechanism.
Conclusion
The above blog helps you to get to know the far-reaching effects of sleep deprivation, which you have to consider. A healthy sleep not only helps you in keeping fresh throughout the day but also boosts your performance. It also sharpens the memory and selfheal some minor health issues and mental issues like anxiety.
However, considering changes in daily life activities may improve the overall sleep cycle and help you eliminate the effects of sleep deprivation.
In addition to this, combining pills like Noocube Sleep Upgrade can be the best aid to get rid of the concern naturally. As the supplement comprises only natural supplements it’s completely safe to combine in the diet. Noocube Sleep Upgrade Results are amazing. Upgrade your sleep with the best sleep aid booster.
0 notes
Text
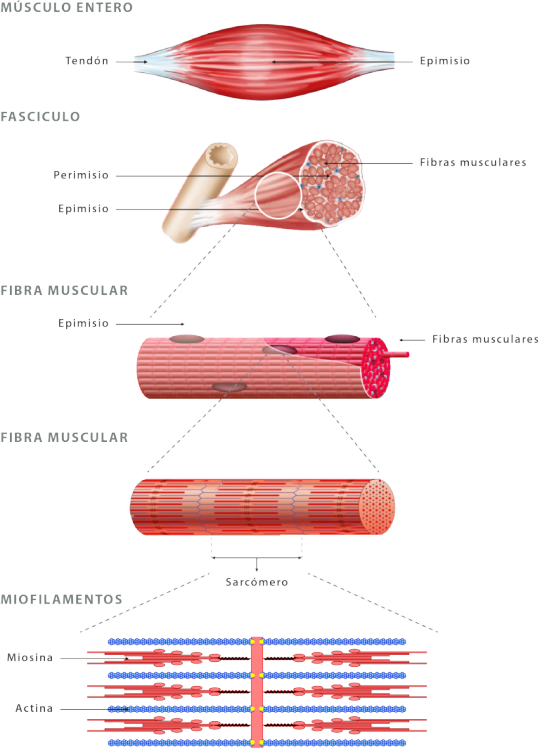
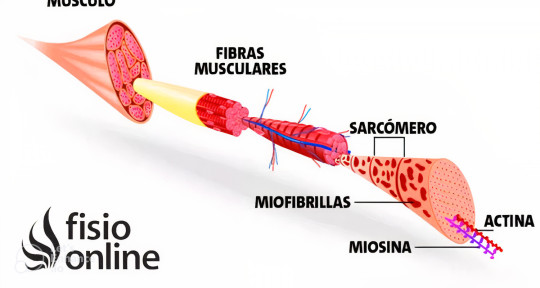
The Different kinds of Muscle Tissue
There are three primary types of muscle tissue found in the human body:
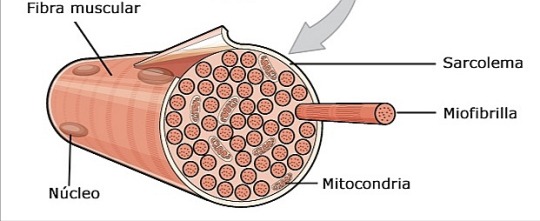
Skeletal Muscle:
Description: Skeletal muscle is attached to bones and responsible for voluntary movements.
Features:
Long, cylindrical cells called muscle fibers.
Multinucleated cells with striations (stripes) due to the arrangement of actin and myosin filaments.
Allows for conscious control over movements.
Contracts rapidly and forcefully.
Works in pairs or groups to produce coordinated movements.
Under the control of the somatic nervous system.
Smooth Muscle:
Description: Smooth muscle is found in the walls of internal organs and blood vessels.
Features:
Non-striated, spindle-shaped cells.
Each cell has a single nucleus.
Involuntary control (under autonomic nervous system regulation).
Contracts slowly and rhythmically.
Functions in a variety of processes such as propulsion of food in the digestive tract, regulation of blood flow, and control of airway diameter.
Can exhibit plasticity and stretch without damage.
Cardiac Muscle:
Description: Cardiac muscle is specific to the heart.
Features:
Branching, striated cells with intercalated discs (specialized cell junctions).
Each cell has a single nucleus.
Involuntary control (regulated by the autonomic nervous system).
Contracts rhythmically to pump blood.
Possesses high endurance due to continuous contraction.
Exhibits an intrinsic conduction system that coordinates contractions.
Can generate and conduct electrical impulses.
Each type of muscle tissue has unique characteristics and functions, enabling the body to perform various movements, maintain organ function, and circulate blood effectively.
0 notes
Text
Biology 10 (3rd Quarter)
!!!(Pics not mine)!!!
Topic 1 | The Nervous System
- Controls body activities.
02/14/23 D1
Major Divisions and Parts of the Nervous System
1. Central Nervous Systems (CNS)
- The CNS serves as the main processing center for the entire nervous system.
Consists of 2 main components:
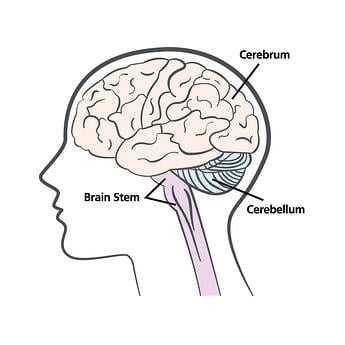
A. Brain
- An organ located within the skull that functions as organizer and distributor of information for the body.
• Cerebrum
- Large, upper part of the brain that controls activity and thought.
• Cerebellum
- The part under the cerebrum that controls posture, balance, and coordination.
• Brain Stem
- The part that connects the brain to the spinal cord and controls automatic functions such as breathing, digestion, heart rate, and blood pressure.

B. Spinal Cord
- Serves as a channel for signals between the brain and the rest of the body, and controls simple musculoskeletal reflexes without input from the brain.
2. Peripheral Nervous System (PNS)
- The PNS connects the central nervous system to the organs and limbs.
It has 2 main divisions.

A. Somatic Nervous System
- This system is associated with the voluntary control of body movements and has 2 main parts:
• Spinal Nerves
- The nerves that carry motor and sensory signals between the spinal cord and the body.
• Cranial Nerves
- The nerve fibers that carry information in and out of the brain stem.
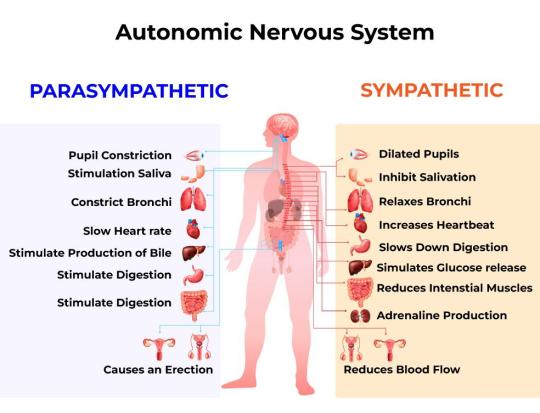
B. Autonomic Nervous System
- This system is associated with the involuntary control of body movements and has 2 subdivisions.
• Sympathetic
- It's activated when the body is in a dynamic role or stress.
E.g. Increased heart rate and breathing, dilation of pupil, sweating, etc.
• Parasympathetic
- Maintains body functions and restored the body to normal or relaxed mode.
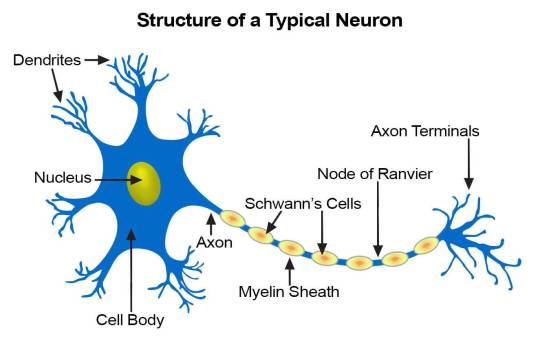
Nerve Cell A.K.A. Neuron
- Transmits or carries the information.
- Basic unit of the Nervous System.
- Billions of it in a human Nervous System.
Video: https://youtu.be/imw6GyZfttY
*️⃣Main Parts: (I think)
- Cell body (Soma)
- Dendrites
- Axon
*️⃣Neurotransmitters:
- Melatonin
- Seratonin
- Dopamine
- Adrenaline
- Acetylcholine
*️⃣Types:
- Sensory
- Motor
- Inter
❗Parts
1️⃣Cell Body
- Root-like structures.
2️⃣Dendrites
- Carries Impulses towards the cells body.
3️⃣Axon
- Carries impulses away the cell body.
- Longest extension from the soma.
4️⃣Myelin Sheath
- Protects the Axon.
- Made up of protein & fatty substances.
5️⃣Synapse
- A small gap at the end of a neuron.
Allows a signal to pass from one neuron to another.
- Where electrical signal (action potential) is converted into a chemical signal (neurotransmitter release).
❗3 Types of Neurons
1️⃣Sensory Neuron
- Nerve cells that are activated by sensory input from the environment.
2️⃣Motor Neuron
- Specialized type of neuron that allow us to move, speak, swallow, and breathe by sending commands from the brain to the muscles that carry out these functions.
3️⃣Interneuron
- The one in between.
- Connects the spinal motor and sensory neurons.
- Found exclusively in the central nervous system.
❗Neurotransmitters
1️⃣Melatonin
-A hormone that our brain produces in response to darkness.
2️⃣Serotonin
- Happy hormones.
3️⃣Dopamine
- Allows us to feel calmness, pleasure, satisfaction and motivation.
4️⃣Adrenaline
- A hormone that helps us react very quickly in a fight/flight scenario.
5️⃣Acetylcholine
- Regulates cardiac contradictions and blood pressure, intestinal peristalsis, and glandular secretion.
0 notes