#both of them later developing fevers as their symptoms worsen
Text


(≧///﹏ ///≦) 💦 💫
#the sopping wetcat detective caught in the pouring rain#and the workaholic ceo that doesn’t know the meaning of the word “rest”#I couldn’t have asked for a better pair of blorbos to put through hell#thank you rain code I am blessed#i love them both dearly <3#cropped out doodles#pixeldoodles#rain code#rain code spoilers#whumpcode#yuma would catch a cold and makoto would get a headache#both of them later developing fevers as their symptoms worsen#yep thats how it goes its canon to me#inb4 they get sick at the same time because they're twins#my precious clone whumpees <3#my art#makoyuma#they are so screwed by the time im through with them >:3#whumpee#sick whump#illness whump
65 notes
·
View notes
Note
can i request yoongi and jin taking care of hobi and namjoon with high fevers and colds, but they start paying more attention to hobi than namjoon so namjoon just starts to get more and more sick until someone notices
Here it is. Hope you enjoy.
Tw high fever
Turtles and Walruses
It was a brisk fall morning for the members of Bangtan. The maknae line had already left for their schedules and the two oldest were trying to convince the 94 liners to stay home for the day.
"Namjoon and Hoseok, for the last time you're both sick and should be in bed." Yoongi was losing his patience with his two eldest dongsaengs, as they were seemingly refusing to listen to reason.
"Hyung, it's just a little cold. I'm fine to go to sche-" Namjoon was abruptly cut off by a fairly intense coughing fit that had him doubled over for a good minute. Once he recovered Yoongi spoke up. "Joon-ah, you can't dance, rap, or sit through whatever meetings you may have if you're coughing like that. Your body is telling you to rest, so rest."
Namjoon knew his hyung was right, so he sat down on the couch and watched Hoseok be the next one to be lectured. “Seok-ah, you haven’t been able to say anything above a whisper all morning and you nearly fell asleep in your breakfast. How do you intend to get anything done if you can’t speak and you’re nodding off every five minutes?” Yoongi gave Hoseok a pointed look and gestured for him to join Namjoon on the couch.
Hoseok sighed, knowing his hyung was right and he went to the couch. Shortly after, Jin joined the others in the living room carrying a tray with four mugs of tea. The two older men then watched as Namjoon called the manager to tell him that he and Hoseok were too sick to attend the day's schedule. Seokjin and Yoongi already had the day off, so it wasn’t any problem for them to stay and look after their dongsaengs.
As soon as Namjoon finished his phone call with the manager, Seokjin gave the younger two the tea he had made, while Yoongi went to grab the thermometer. A quick scan of the forehead revealed that Namjoon barely had a fever with a temperature of 100.6, while Hoseok definitely had a fever of 102. The moderate fever coupled with the fact that he couldn’t speak, put Yoongi’s and Seokjin’s worry for Hoseok a little into overdrive.
Once the younger two had been given tea, Yoongi gave them each medicine. He gave Namjoon a cough suppressant and Hoseok a fever reducer and cough suppressant. He then ushered the two back to bed, in hopes they could get some sleep.
After about an hour, harsh coughing could be heard from the hallway as Hoseok and Namjoon emerged from their respective rooms. Upon reaching the couch Hoseok doubled over in a coughing fit that was even harsher than Namjoon’s. Almost sounding like he was gasping for breath in between coughs.
Seokjin was quick to start pounding the younger on the back in hopes of aiding him in expelling whatever was irritating his lungs or throat. “Yoongi-yah, please go get the humidifier and set it up out here.” Yoongi nodded and left the room to get the requested device.
By the time that Yoongi had returned with the humidifier, Hoseok had finished coughing and was now drinking some more tea. Both Seokjin and Yoongi were fairly concerned about the elder of the two sickies. He was seemingly getting worse by the hour, but he was adamant about not going to the doctor.
“Hyung, can I please do some sort of work? I’m bored.” Namjoon whined to no one in particular. Seokjin sighed. “Joon-ah, If you want you can work on writing some songs, but no going on the computer.” Jin was speaking with his no nonsense voice and gave Namjoon a ‘don’t test me look. Namjoon was quick to agree and retired back to his room where he kept his notebooks.
Namjoon had decided to stay in his room while he wrote some lyrics. At one point he began to develop a headache and left his room to see if he could get his hands on some pain reliever. On his way to the living room, he found himself coughing for the millionth time that day.
Namjoon groaned a bit loudly as he entered the living room. “Hyungs” Namjoon whined, “I have a headache, can I get some medicine?” To Namjoon’s surprise, he was met by a glare from Seokjin instead of Sympathy.
“Namjoon.” Jin said with a harsh tone. “You probably disobeyed me and went on your computer, that’s why you’ve got a headache. Furthermore, Hoseok was asleep and you decided to be loud, which woke him up.” As if on cue, Hoseok began coughing rather harshly again.
“You don’t need pain meds for a headache you got from staring at a screen, you need rest. Go back to bed and take a nap.” Namjoon dejectedly turned to go back to his room and heard Jin say as an afterthought, “By the way Yoongi went to the store to restock on soup and medicine.”
Back in his room, Namjoon was feeling bad about the fact that he had unintentionally woken up Hoseok. He also was unhappy that Seokjin assumed his headache was from staring at his computer, when he didn’t even power it up. Namjoon put on a heavy sweater and crawled underneath his blankets, wishing he had more, because he was now really cold and wasn’t really sure why.
When Namjoon woke up, he wasn’t entirely sure what time it was, so he looked out the window. He noticed the sun was still out, but he also noticed something rather peculiar on the balcony. A turtle hovering above the chair that was always there.
Namjoon knew the turtle wasn’t supposed to be there and also knew there was only one way to get rid of it. He needed to fight the turtle to assert his dominance over his territory. He left his room to get the necessary supplies.
When Namjoon walked past the living room, he noticed that Yoongi and Seokjin had both passed out on the couch. Hoseok, on the other hand, was wide awake. Namjoon quickly waved at him then made his way to the kitchen.
In the kitchen, Namjoon grabbed a colander, a whisk , and a lid for one of their frying pans. After he collected the necessary items he made his way to the balcony using the door that’s in the living room.
Hoseok was concerned about the leader’s strange behavior, but didn’t really know what to do about it. He still couldn’t really speak above a whisper and he wasn’t sure he had the strength to drag the leader back in anyway. Hoseok did the only thing he could actually think of, throw a pillow at his nearest hyung, Yoongi.
Yoongi woke up fairly quickly after being pelted by the pillow, and glared at Hoseok, until he saw the worried expression on the younger’s face. “Seok-ah, what’s wrong?” Hoseok merely pointed at the door leading to the balcony.
Yoogi got up and stuck his head out the door, where saw Namjoon wearing a colander on his head, holding a frying pan lid in one hand, and a whisk in the other. Namjoon was swinging the whisk through the air at seemingly nothing.
“Namjoon-ah, what are you doing?” Yoongi asked, trying to figure out what exactly was happening.
“I’m fighting the walrus, hyung.” Namjoon stated as if it were completely obvious.
“And why are you fighting the walrus, might I ask?”
“The turtle says I can’t use the bathroom, and that I need to fight the walrus before I can fight him.” Namjoon was sounding completely serious with his explanation, which was just worrying Yoongi further.
“Joon-ah, come take a break, the walrus will still be there to fight later. Are you hungry?” Yoongi was fairly certain that Namjoon was delirious and needed to check the younger’s forehead. He hoped that by playing along, he could sway the younger to come inside.
Luckily for him, Namjoon’s stomach decided to growl at that exact moment, so he put down the whisk and came inside, but not before shooting a glare towards the non existent threat.
As soon as Namjoon got close enough, Yoongi put his hand on the younger’s forehead. His eyes widened at the heat coming off of him. He quickly ushered the sick leader inside and told Hoseok to wake Seokjin while he took the younger to the bathroom.
Yoongi quickly began to run a lukewarm bath and told Namjoon to strip down to his boxers. He then made Namjoon get in the bath. Soon after there was a knock on the door. “Yoongi-yah, Hoseok said that you brought Namjoon in here looking worried.”
Yoongi nodded, “Hyung, he spiked a fever and was hallucinating that the pillows on the chairs for the balcony were a turtle and walrus that needed to be fought.” Seokjin looked in concern as he grabbed the forehead thermometer and scanned that sick leader’s forehead.
“103.3, If it gets any higher, we’ll need to bring him to the hospital.” Seokjin sighed as he went to grab the fever reducers that he had left on the coffee table. When he returned, he was looking a bit guilty, Hoseok trailing behind him.
“While you were at the store, Namjoon came looking for some medicine, and I brushed him off. I assumed his complaints were from going on his computer even though I told him not to.” After Seokjin handed the medicine over to Yoongi, he checked Hoseok’s temperature, which seemed to have gone down.
“Hyung, no offence, but you’re an idiot.” Yoongi snorted at Hoseok’s comment. “Hoseok’s right, you knew that Namjoon was sick and didn’t do anything when he complained of worsening symptoms.” Yoongi then gave Hoseok a look, “Seok-ah, I’m glad it sounds like your voice is back, but you still shouldn’t be talking so you can put as little strain on your voice as possible.”
Hoseok did the motion of zipping his mouth closed and throwing away the key before heading back into the hall. Seokjin was still looking extremely guilty. Yoongi gave him a sympathetic look. “Hyung, why don’t you get lunch started. You can apologize to Namjoon when he’s doing better.”Seokjin nodded and went to the kitchen.
Yoongi made sure that Namjoon took the medicine then made him soak in the tub for several minutes until he decided enough time had passed. “Ok Joon-ah time to get out of the tub.” Namjoon nodded and got up. He got himself dressed then went to the kitchen with Yoongi.
Seokjin had made jook and ramen. He and Hoseok were already at the table eating. Yoongi and Namjoon were quick to join the other two and begaan eating. Lunch didn’t really have any issues, although Namjoon kept glaring at the balcony window. A clear sign that his fever was still high.
After lunch, Seokjin made Namjoon lie down on the couch and grabbed a bowl of ice water and washcloth. He dipped the cloth in the water, then gently placed it on the younger’s forehead. It wasn’t long for Namjoon to drift off to sleep.
Namjoon wound up sleeping for a good chunk of the afternoon, Yoongi and Seokjin keeping a close eye on his fever. They also made sure to keep checking on Hoseok, who was doing much better than he had that morning.
Namjoon woke up to the sound of the maknae line returning to the dorm. Namjoon was fairly coherent when he woke up, but was a bit surprised at Seokjin shoving a thermometer in his mouth when he sat up.
After a moment the thermometer beeped. Seokjin took the thermometer and looked at it, sighing in relief when it had gone down. “Good news Joon-ah, your temp went down and you’re out of the danger zone for now” Namjoon looked confused as he didn’t really remember what happened earlier.
Seokjin fully explained what happened, then began apologizing for not being a good hyung earlier. Namjoon accepted the apology. A moment later, Jungkook spoke. “Now that we’re all caught up on everything, I bought banana milk for everyone.” He began passing the cartons out to all of his hyungs, and they all settled down in the living room and turned on the tv to watch whatever was on that evening.
18 notes
·
View notes
Text
I copied and pasted this story from someone else but wanted to share so everyone can see how successful this drug is.
I want to tell my COVID-19 story. It has taken me awhile to get my head around all that transpired during my parents' and my journey with Covid and to know what words to say in the hopes I won't be censored. But I feel it's important to tell our story in the hopes that others may understand the truth and hopefully save another loved one's life.
While visiting my parents in Florida, I was extremely diligent about making sure to protect them from Covid-19 because of my Dad's diabetes and my mother's AFIB and their ages. I did not allow them to go to restaurants - always cooking at home - I did all the shopping and stayed six feet from everyone and wore my mask when we were in public places. I believe my one mistake was lunch with the my lifelong friends. Masks were not required while sitting at a table.
A couple of days later after our lunch, my one friend became sick and was tested for COVID. Five days later from her testing, I had lost my taste and smell. One day later, my mom had chest pains and was taken to the hospital because of her Afib and held over night for observation. While at the hospital, she was tested POSITIVE for Covid. The hospital called my dad at 6:00 the following morning and we were asked to come to the hospital for a rapid test where we both were positive. We all 3 were given chest x-rays, blood work and because everything looked normal - we were sent home to quarantine. I asked the ER doctor if my parents could take HYDROXYCHLOROQUINE to prevent further complications with their underlying health conditions and his words to me were exactly this,
"Even if I wanted to prescribe it, I am not allowed to dispense it."
We were sent home with NOTHING but worry as to what was to come.
My dad and I never had symptoms other than loss of taste for 3 days, but my mom developed a fever and cough and generally did not feel well. Here is where my story becomes important to tell. Four days after my mom was released from the hospital, I called her primary physician and told him of my concerns about her declining health and that I wanted her to be placed on Hydroxychloroquine. This was a Thursday morning. Her physician set up a video call with my mom and agreed to "dispense" not only Hydroxychloroquine, but an antibiotic and Zinc (which I was already giving them.) He sent the Rx immediately to CVS to be filled that day. I had watched videos of Hydroxy's success, I had just learned of a huge Ford Center study that had proven its success - cutting the death rate by 50%, and I had done my research enough to be very excited that her doctor agreed to prescribing it to her.
And here's where the story gets complicated. When I called the pharmacist at CVS to ensure he received her Rx - the pharmacist REFUSED to fill the Rx, stating its complications with the heart and that there is no proof it works. I was furious - had some very strong words for him and because of that, he did agree to fill the Rx but still begged me not to give it to my mother. I picked it up without hesitation. BUT - because I did share the pharmacist's argument with my parents, my mom was too afraid to take the drug. It wasn't until Saturday early afternoon that I could convince my mom to start the regimen because she was worsening, had a fever of 100.1 and her oxygen level was at 93%. This was Saturday afternoon that she began taking Hydroxy and she was able to get 2 pills in before bedtime. ON SUNDAY MORNING, she awoke with no fever and her oxygen was at 96%. HOWEVER, because her best friend had suffered terribly with COVID and had to be intubated at the same local hospital, we decided to take Mom to the ER for a chest x-ray just to be safe.
Because I knew that my mom MIGHT be admitted to the hospital or have an extended wait/stay in the ER, I put in her purse the Hydroxy and her antibiotic and Zinc that her physician had legally prescribed. I instructed her to make sure to take her doses as her doctor has prescribed. We truly feared the hospital would take it from her but thankfully they did not. This story continues to get even better.
After a chest x-ray in the ER, they determined my mom had Covid Pneumonia. We were devastated and frightened beyond words, and my Mother was admitted Sunday evening to Winter Haven Hospital (even though her oxygen remained at 97% and no fever). My dad and I would Facetime her often and I continued to remind her to take the Hydroxy and antibiotic. She took it exactly as her Doctor had prescribed. The hospital was giving her NOTHING and rarely checked in on her. BY MONDAY AFTERNOON - JUST ONE DAY AFTER BEING ADMITTED FOR PNEUMONIA, the doctors told her that she no longer had pneumonia and would be going home Tuesday morning afer one more night of observation! They were SHOCKED how quickly she recovered. It was "unheard" of! We never told the hospital she was secretly taking the Hydroxy and she was released to come home on Tuesday just 2 days after being admitted for pneumonia.
It wasn't until 14 days after my friend was tested, that we learned she was positive and most likely where we had gotten it.
The lessons I have learned during this journey:
!. HYDROXYCHLOROQUIN works! It saves lives but because it has become a political issue and is a cheap drug (Big Pharma doesn't like that) doctors are not using it to save lives. It's a travesty against the People. Videos from doctors that are touting the drug are being censored and the information is kept from patients. Pharmacists are scaring patients from taking it and people are dying.
2. Restaurants that have mask requirements while standing or walking through but not while seated at a table are a joke. And restaurants that have only 8 to a table are a joke as well. I got it from one person out of 4 at the table while not having to wear a mask while seated. This is completely misleading to the public and a facade to make people feel safer.
3. Taking 14 - 21 days to receive a test result is ludicrous and dangerous and definitely a public hazard. We are supposed to control the spread by testing more people and quarantining the sick. How are we to do that when results are taking so long to return. Had my mom not been taken to the hospital for her heart and been tested, my family could have been walking around in public - SICK. My parents and I had the 2 hour test because were in the hospital, otherwise we would have never known until my mom would have become much worse with pneumonia.
4. Many people have COVID and have no symptoms like my Dad and I and do very well with the disease - just like 99% of the others who survive it.
I know this was a long story - but I just want people to know that my mom is one of the lucky ones that was given Hydroxychloroquin and had amazing results. Thank God for my Mom's doctor who knew the drug worked, prescribed it without hesitation and who saved my mom's life. Her physician stated that had the pharmacist NOT scared her from taking it that Thursday, she might not have ever gotten the pneumonia or might not have had to have been hospitalized. Hopefully this information can save another life. My family is doing wonderfully and we are now able to give blood to save others (which my dad has already done). This is the part I love best.
God Bless.
You are welcome to share.
6 notes
·
View notes
Text
I copied and pasted this story from someone else but wanted to share so everyone can see how successful this drug is.
I want to tell my COVID-19 story. It has taken me awhile to get my head around all that transpired during my parents' and my journey with Covid and to know what words to say in the hopes I won't be censored. But I feel it's important to tell our story in the hopes that others may understand the truth and hopefully save another loved one's life.
While visiting my parents in Florida, I was extremely diligent about making sure to protect them from Covid-19 because of my Dad's diabetes and my mother's AFIB and their ages. I did not allow them to go to restaurants - always cooking at home - I did all the shopping and stayed six feet from everyone and wore my mask when we were in public places. I believe my one mistake was lunch with the my lifelong friends. Masks were not required while sitting at a table.
A couple of days later after our lunch, my one friend became sick and was tested for COVID. Five days later from her testing, I had lost my taste and smell. One day later, my mom had chest pains and was taken to the hospital because of her Afib and held over night for observation. While at the hospital, she was tested POSITIVE for Covid. The hospital called my dad at 6:00 the following morning and we were asked to come to the hospital for a rapid test where we both were positive. We all 3 were given chest x-rays, blood work and because everything looked normal - we were sent home to quarantine. I asked the ER doctor if my parents could take HYDROXYCHLOROQUINE to prevent further complications with their underlying health conditions and his words to me were exactly this,
"Even if I wanted to prescribe it, I am not allowed to dispense it."
We were sent home with NOTHING but worry as to what was to come.
My dad and I never had symptoms other than loss of taste for 3 days, but my mom developed a fever and cough and generally did not feel well. Here is where my story becomes important to tell. Four days after my mom was released from the hospital, I called her primary physician and told him of my concerns about her declining health and that I wanted her to be placed on Hydroxychloroquine. This was a Thursday morning. Her physician set up a video call with my mom and agreed to "dispense" not only Hydroxychloroquine, but an antibiotic and Zinc (which I was already giving them.) He sent the Rx immediately to CVS to be filled that day. I had watched videos of Hydroxy's success, I had just learned of a huge Ford Center study that had proven its success - cutting the death rate by 50%, and I had done my research enough to be very excited that her doctor agreed to prescribing it to her.
And here's where the story gets complicated. When I called the pharmacist at CVS to ensure he received her Rx - the pharmacist REFUSED to fill the Rx, stating its complications with the heart and that there is no proof it works. I was furious - had some very strong words for him and because of that, he did agree to fill the Rx but still begged me not to give it to my mother. I picked it up without hesitation. BUT - because I did share the pharmacist's argument with my parents, my mom was too afraid to take the drug. It wasn't until Saturday early afternoon that I could convince my mom to start the regimen because she was worsening, had a fever of 100.1 and her oxygen level was at 93%. This was Saturday afternoon that she began taking Hydroxy and she was able to get 2 pills in before bedtime. ON SUNDAY MORNING, she awoke with no fever and her oxygen was at 96%. HOWEVER, because her best friend had suffered terribly with COVID and had to be intubated at the same local hospital, we decided to take Mom to the ER for a chest x-ray just to be safe.
Because I knew that my mom MIGHT be admitted to the hospital or have an extended wait/stay in the ER, I put in her purse the Hydroxy and her antibiotic and Zinc that her physician had legally prescribed. I instructed her to make sure to take her doses as her doctor has prescribed. We truly feared the hospital would take it from her but thankfully they did not. This story continues to get even better.
After a chest x-ray in the ER, they determined my mom had Covid Pneumonia. We were devastated and frightened beyond words, and my Mother was admitted Sunday evening to Winter Haven Hospital (even though her oxygen remained at 97% and no fever). My dad and I would Facetime her often and I continued to remind her to take the Hydroxy and antibiotic. She took it exactly as her Doctor had prescribed. The hospital was giving her NOTHING and rarely checked in on her. BY MONDAY AFTERNOON - JUST ONE DAY AFTER BEING ADMITTED FOR PNEUMONIA, the doctors told her that she no longer had pneumonia and would be going home Tuesday morning afer one more night of observation! They were SHOCKED how quickly she recovered. It was "unheard" of! We never told the hospital she was secretly taking the Hydroxy and she was released to come home on Tuesday just 2 days after being admitted for pneumonia.
It wasn't until 14 days after my friend was tested, that we learned she was positive and most likely where we had gotten it.
The lessons I have learned during this journey:
!. HYDROXYCHLOROQUIN works! It saves lives but because it has become a political issue and is a cheap drug (Big Pharma doesn't like that) doctors are not using it to save lives. It's a travesty against the People. Videos from doctors that are touting the drug are being censored and the information is kept from patients. Pharmacists are scaring patients from taking it and people are dying.
2. Restaurants that have mask requirements while standing or walking through but not while seated at a table are a joke. And restaurants that have only 8 to a table are a joke as well. I got it from one person out of 4 at the table while not having to wear a mask while seated. This is completely misleading to the public and a facade to make people feel safer.
3. Taking 14 - 21 days to receive a test result is ludicrous and dangerous and definitely a public hazard. We are supposed to control the spread by testing more people and quarantining the sick. How are we to do that when results are taking so long to return. Had my mom not been taken to the hospital for her heart and been tested, my family could have been walking around in public - SICK. My parents and I had the 2 hour test because were in the hospital, otherwise we would have never known until my mom would have become much worse with pneumonia.
4. Many people have COVID and have no symptoms like my Dad and I and do very well with the disease - just like 99% of the others who survive it.
I know this was a long story - but I just want people to know that my mom is one of the lucky ones that was given Hydroxychloroquin and had amazing results. Thank God for my Mom's doctor who knew the drug worked, prescribed it without hesitation and who saved my mom's life. Her physician stated that had the pharmacist NOT scared her from taking it that Thursday, she might not have ever gotten the pneumonia or might not have had to have been hospitalized. Hopefully this information can save another life. My family is doing wonderfully and we are now able to give blood to save others (which my dad has already done). This is the part I love best.
God Bless.
You are welcome to share.
4 notes
·
View notes
Video
youtube
I Can't Stop Watching Contagion | Folding Ideas
Coping with crisis in the real world by confronting it in fiction
[O]ne purpose of fiction is that it allows us a space to practice intense emotions and states without exposing us to the complexities or harms of those states in reality. ... Watching a disaster film in a disaster, particularly one as sociologically driven as Contagion, is an extension of this. Rather than practicing intense emotional states before they happen, this instinct of exposing ourselves to what we’re already experiencing, amplifying existing emotional states, it works as a form of emotional inoculation. I am scared and anxious and uncertain, and so I will make myself more scared and more anxious and more uncertain, because it’s still fiction, it’s still safe, it still has an end. It is bounded. Things will get bad, things will then get worse, people will die. The world is unfair, it is unbalanced, it is unjust, and catastrophe will bring out both the best and worst of all of us. And then it will end.
...
There is an escapism to a story about horrible things, because that story is complete. It is bounded. It provides a framework to horror that doesn’t exist in the real present. Our future is uncertain, beset on all sides by devils, and we can come out better or we can come out worse or we can die and none of us knows which it will be and we’re all screaming at those in power to make the moral choice, to choose better.
...
On one hand I am deeply privileged to be in a position where I am and can remain isolated. On the other hand I can’t even think about the other hand.
Disease does not have a narrative meaning, it does not have an eye for poetry or twists or closure. The only meaning is in how we respond. So I watch Contagion over and over and over again. Because I need to practice emotions, and I need to live in a bounded world, and I need to believe we can choose better.
full video transcript under the cut:
[video is Dan Olson of Folding ideas lying on his couch, staring unmoving into the camera. scenes from Contagion are projected over him.]
VOICEOVER: This video is not an essay, it is a raw nerve.
Contagion is a 2011 film directed by Steven Soderbergh, starring an ensemble cast including Marion Cotillard, Matt Damon, Laurence Fishburne, Jude Law, Gwyneth Paltrow, and Kate Winslet. The film revolves around the origin, contraction, spread, and cure of the fictional MEV-1 virus, a highly contagious, aggressive, and fatal strain of hybrid bat and pig flu.
The initial patient, Beth Emhoff, played by Gwyneth Paltrow, contracts the virus in Macau after shaking hands with a casino chef who has recently handled an infected pig. She spreads the virus to several other people in the casino after they handle objects that she’s touched, such as gambling chips, a martini glass, and her cell phone. An important aspect of the film is that the fictional virus is highly transmissible via fomites, which are objects that an infected person has touched after touching their mouth or nose, coughing or sneezing on the object, or otherwise leaving infectious residue on an otherwise inert, non-biological object. A local waiter who handled her glass returns home, infecting members of his family before wandering into traffic in a fever-induced delirium where he is struck by a vehicle and killed. A Japanese businessman who shared chips with her returns to Tokyo where he falls ill rapidly, dying suddenly of a seizure on a crowded bus, infecting several bystanders who touch him or handrails that he touched. A Ukranian model who handled Beth’s phone flies to London where her symptoms also escalate rapidly while she transmits the disease to others via handling portfolios and riding in a cab.
Beth returns to America where she infects several people in Chicago, first her ex lover Jon who contracts it when they have sex while she is on layover, and a bartender at the airport who handles her credit card, before flying to Minneapolis where she infects the coworker who drives her home from the airport and her son Clark. A day or two later Beth’s husband, Mitch, played by Matt Damon, picks up Clark from school after Clark begins to exhibit a fever. While Beth and Mitch are talking in the kitchen Beth suddenly has a seizure. Mitch rushes her to the hospital, leaving Clark with a babysitter, but Beth’s condition continues to worsen, she fails to respond to treatment, and she dies. As a stunned Mitch is driving home he gets a call from the babysitter that Clark has possibly had a seizure and might not be breathing. Mitch tells her to call 911 immediately, but before anyone can get there Clark is already dead.
From there the story expands to encompass the doctors, politicians, reporters, hucksters, and ordinary people who are swept up in an all-encompassing pandemic that threatens to kill a quarter of the global population. The movie is an incredibly tense hundred minutes of society pushed to its breaking points, not as a fantastical disintegration into wastelands of leather-clad murder gangs or a zombie apocalypse, but one rooted in the historical reality of epidemics.
And I can’t stop watching it.
I have watched Contagion over fifteen times in the last two weeks. Several days I’ve just watched it on repeat two or three times. And I'm not alone. According to Netflix it is, at the time of writing, the second most watched thing in Canada. For weeks it has sat in the top ten.
Unlike many similar films, such as the 1995 film Outbreak starring Dustin Hoffman, the film is not about any one person, and there is no singular twist of victory. Rather it is an example of sociological storytelling. It’s about the systems and networks that these characters exist within, and how they both influence and are influenced by those systems, and what happens when those systems are placed under tremendous strain. Kate Winslet plays Dr. Erin Mears, a front line worker for the CDC who is sent to Wisconsin to track the transmission of the virus and contain its spread. Half way through the film she catches the virus herself, and then her condition worsens, and then she dies. It is unceremonious. It is not foreshadowed or paid off because it is not poetic, because pandemics are not poetic and don’t have a tight arc or an eye for narrative fulfillment. It doesn’t have meaning, the only meaning is in how we choose to respond.
Because this is sociological the movie doesn’t end when doctor Ally Hextall develops a vaccine. What would be the singular victory moment in most films is instead the beginning of a slow, painful march back to stability as first the vaccine needs to be mass produced, and then distributed to billions of people worldwide. It is a dangerous task that needs to be tightly controlled as it requires access to the isolated virus and thus is very slow to ramp up. The film trudges through the immense societal tension that is created when there is a cure, but it will take over a year to make and distribute enough for everyone, a situation that lays bare every societal privilege. Dr. Orantes, played by Marion Cotillard, is kidnapped and held ransom for the vaccine by Chinese villagers who are keenly aware that in the priority of global politics the poor, the rural, and the non-white are at the very back of the line. They are terrorists, but they’re not wrong, just desperate. They are at the back of the line, and the government throws them under the bus anyway. Despite the existence of a vaccine Mitch continues to keep his teenage daughter, Jory, under aggressive quarantine out of legitimate fear of the disease that has been amplified to paranoia by the trauma of losing Beth and Clark, the survivor’s guilt of being naturally immune, and the uncertainty of whether his daughter would share that immunity or not.
In December 2019 the coronavirus COVID-19 was identified by doctors in the city of Wuhan. Over the course of January and February the spread of the virus began to be identified in South Korea, Japan, and Italy and, gradually, most of the rest of the world. The disease itself is not exceptionally lethal when compared to epidemics such as the Black Death in the mid 14th century or the spread of Smallpox through indigenous populations following contact with Europeans in the 16th and 17th centuries, but, first of all, “better than the black death” is a pretty bad standard, and second on a global scale a mortality rate of 1-2 percent in an unchecked pandemic still means, in absolute terms, millions and millions of preventable deaths. This is compounded by the strain that mass illness, even one that is not terribly lethal, inherently places on an already strained society: crowding healthcare systems, disrupting infrastructure, and forcing people to choose between working while ill, and thus infecting others, or losing their jobs. A low mortality rate is often the result of adequate care, but the quality of care goes down as the number of severely ill goes up, as the number of infected healthcare workers reduces the number of people qualified and capable of administering that care. This, in turn, has a knock on effect where unrelated illnesses and injuries become more dangerous. A heart attack or broken leg that would be easily managed under normal circumstances becomes that much worse when there aren’t enough people to help, aren’t enough beds to go around. The more people who are exposed, the more need to roll the dice against that one to two percent, and the more are going to lose.
As of March 2020 most of the United States and Canada have entered a period of uncertain quarantining. Non-essential businesses are closed, events are canceled, workers are being sent home or laid off, borders are being shut down,and the economy is in freefall. Every existing societal problem, from income inequality to housing inequality to healthcare, is being stressed and amplified by not only the virus but the complicity of our governments. News comes out hourly about warnings the people in charge received months ago, and the ways in which they were either ignored or exploited for personal gain. Several American politicians were briefed on the security risks of COVID 19 in late January, and then took to Twitter to decry public fear as a partisan hoax while they dumped their stocks in preparation for a crash that they knew was coming. People in government, their corporate donors, and their pundit allies are getting anxious, debating breaking quarantine and telling everyone to go back to work and roll the dice on whether or not they’re going to die for the economy. We are standing on the precipice of a very uncertain future, and we don’t know if that future is days, weeks, months, or years away. This could be the new normal for a very long time.
So why do I keep watching Contagion?
A dimension of narrative that I like to bring up pretty regularly is the idea that one purpose of fiction is that it allows us a space to practice intense emotions and states without exposing us to the complexities or harms of those states in reality. This is typically in the context of the fanciful: reckless stunts, wild sex, gun fights, or general risky behaviour. We talked about this with Fifty Shades and the idea of non-consent as a fantasy subject.
Watching a disaster film in a disaster, particularly one as sociologically driven as Contagion, is an extension of this. Rather than practicing intense emotional states before they happen, this instinct of exposing ourselves to what we’re already experiencing, amplifying existing emotional states, it works as a form of emotional inoculation. I am scared and anxious and uncertain, and so I will make myself more scared and more anxious and more uncertain, because it’s still fiction, it’s still safe, it still has an end. It is bounded. Things will get bad, things will then get worse, people will die. The world is unfair, it is unbalanced, it is unjust, and catastrophe will bring out both the best and worst of all of us. And then it will end.
Is there looting, and arson, and murder? Yeah. But it is, ultimately, out of the ordinary. People get paranoid, people get desperate, they riot under stress, but even when food supply lines break down, the world isn’t summarily turned over to those with the bullets and the willingness to use them. There is no Mad Max dystopia, no Fallout post-apocalypse, because at the end of the day humans are pro-social. The cooperative survive.
In 1349, in the midst of the black death, it must have looked like the end of the world. Entire households, entire villages, dying a gross, horrifying, pain ful death, month after month after month. Then for generations, every year wondering if this was the year the plague returned. Was this the year there would be no one left to bury the dead. But people survived. The working class, who bore the brunt of the disease and saw the bodies of their families, clans, and communities piled like cord wood, fought back against the aristocrats who isolated themselves in their towers and remote estates. It was messy, and bloody, and it took decades, but in the end serfdom was abolished. Europe lost upwards of sixty percent of its population over the course of five years, but it wasn’t Armageddon. Things kept going, people kept going, and Europe would go on to be absolute bastards to the rest of the world.
The disease in Contagion is not unrealistic, real diseases have been as deadly, or worse, but it is dramatic. It moves very, very quickly, is highly contagious, and kills a huge number of those who are infected. In reality this aggressiveness would kinda work against the disease, and, morbidly, would help responders limit the spread. It moves so fast and kills so quickly that there’s little question of who has it, and within a couple days everyone who has it is either recovered or dead. This was the aspect of the SARS epidemic that allowed response teams to effectively quarantine the virus where it burnt itself out. That said it’s not impossible that something could spread so aggressively, be so incredibly contagious, that it could spread like wildfire and become almost impossible to contain before anyone even knows what’s going on. But it’s undeniably dramatic and emotionally effective.
48 hours. We can contain two days in our head. A situation where things will get materially worse literally tomorrow or the day after if nothing is done right this second, that’s a comprehensible timeline. Forty eight hours is short enough that in a catastrophe, driven by adrenaline and stress and necessity, you can stay awake that long without even realizing it. COVID’s life cycle is closer to a month. By the time you get sick you’ve already been sick for two weeks, and now you’re in for hell for another two to four weeks. It’s just past the range where it really feels real. Two weeks isn’t long, but it’s still over the line into the indeterminate “future”.
This problem extends in both directions. There’ s only so much space in the mind for time. As the news ramps up, as things get worse, the present crowds out history. The distance between the irrelevant past and the now contracts. ’Days ago’ becomes distant. ‘Months ago’ is irrelevant. Years ago is ancient. By evening even earlier the same day is suspect in its relevance to the Now. We remember January but it has as much presence in the mind as childhood. Our lives become superliminal, displaced from time, as we wrestle with our own minds and how they try to process the chronology of our own existence. By Sunday, Friday no longer feels real, and yet every day’s news is the consequence of decisions made fourteen, twenty one, twenty eight days ago. Today’s responses won’t yield results until well into next month. This flaw in our meat is a gap into which charlatans, hucksters, and conmen can drive a wedge and pry us open, and pry they will try.
When I first saw Contagion in 2012 I thought the weakest element was what I considered at the time to be the demonization of online media. Jude Law’s character plays an online pundit and conspiracy theorist who preaches to an audience of millions about an herbal tincture of forsythia that he claims is the cure, a cure he just-so-happens to be selling. It is, in 2020, the realest element of the film. Herbal cures, hydrogen water, steam treatment, teas, magnets, suspensions of silver, tinctures, and tonics. We’ve got pastors standing at the pulpit telling their congregation it's all a hoax, that there’s no reason to suspend services, that their nebulous enemies are just trying to shut them down. We now live in a world where the US president told people based on a rumour that chloroquine, a drug used for treating malaria and lupus, was the cure, so a man in Arizona ate a packet of fish tank cleaner containing the chemical. He’s dead now. And that is, again, all part of it.
There is an escapism to a story about horrible things, because that story is complete. It is bounded. It provides a framework to horror that doesn’t exist in the real present. Our future is uncertain, beset on all sides by devils, and we can come out better or we can come out worse or we can die and none of us knows which it will be and we’re all screaming at those in power to make the moral choice, to choose better.
And I am in an absolute haze. My daily life has not much been impacted, overtly. I’m already an agoraphobic shut-in wh o worksonline and has a bad sleep schedule. But it’s too much. I’m tired all the time. I can’t pay attention to the news and Ican’t not pay attention to the news. Working is difficult. I have a long history of respiratory illness. I am at risk.
On one hand I am deeply privileged to be in a position where I am and can remain isolated. On the other hand I can’t even think about the other hand.
Disease does not have a narrative meaning, it does not have an eye for poetry or twists or closure. The only meaning is in how we respond. So I watch Contagion over and over and over again. Because I need to practice emotions, and I need to live in a bounded world, and I need to believe we can choose better.
[end transcript]
#i've seen a lot of posts like ''haha time to distract myself from irl horror with fictional horror!'' and i just wanted y'all to know#that that's a totally reasonable response to have; you're not weird for doing that. so this isn't precisely tma but i think it fits anyway#covid 19#coronavirus#tma#horror#contagion
10 notes
·
View notes
Text
If Morga and The Devil had a second child Headcanons 🐆 💕 🐐
Based on this post x and also my NSFW headcanons here x
• Morga couldn't even think about having another child for a very long time - not with all the regrets tormenting her because of Montag. Eventually though, the idea grew on her.
• "if this one turns out an idiot, you won't get another chance"
• She doubted she could even conceive at her age*. The Devil however insisted it won't be an issue.
• That night was different than their usual intimate encounters. He took her to the heart of the forest - a place soaked with ancient magic bound to fuel forgotten rituals of fertility he guided her through. Consuming nine raw rabbit hearts, wearing a cornflower wreath during the act... She found it challenging not to sneer at such details. He though made sure she was comfortable, and enjoyed every moment. It was slow and gentle, and he held her for hours afterwards, murmuring sweet nothings into her brow as she slept in his arms.
• Morga's pregnancy was a risky and grueling one one**. Aside from usual discomforts associated with such a state (which she obviously had gone through before), she suffered hom extreme swelling, headaches and shortness of breath, as well as exhaustion and constant nausea.
• She often found the experience emotionally overwhelming, for she was still afraid to become a mother once again despite her desire to - afraid to open her heart for unconditional love which has stabbed her in the back and of failing her secondborn the way she felt she failed Montag.
• The Devil on the other hand was extremely enthusiastic about their situation as well as affectionate towards her changing form. She often found it awkward and irritating, but it would ease her worries too.
• She would mindlessly place her hand over her growing stomach and let it linger even if she caught herself doing so (no, she did not talk to it, ever).
• The Devil insisted on never leaving her side for any reason - even if he had to shapeshift to stay out of sight. To her annoyance, he also became ten times fiercer in his protectiveness over her.
• Her chronic nightmares became a lot worse
• Her ailments also worsened towards the end of the pregnancy
• "If I don't pull through, you watch over it, and you raise it better than Monty... Swear to me you will, Djevel".
• She went into labor prematurely
• The labor itself wasn't smooth either - she suffered a severe hemorrage and a fever, but luckily the Devil was able to prevent seizures (since as I alluded with mentioned symptoms, she did have pre-eclampsia).
• At first she refused to hold the baby, delirious from blood loss, but later calmed down and fell asleep with her secondborn beside her, Papa Devil guarding them both.
• They had a girl - Hel. I have a sketch of her, I'll give her a bio of her own.
• Morga would catch herself smiling as she breastfed... unless it was in the middle of the night. Hel was a great sleeper though, at least compared to her older brother.
• She would hum old war songs as a lullabye to Hel.
• Little Hel woul crawl into bed with Morga. She didn't mind.
• Jæger is far more fond of Hel than of Lucio.
• The Devil was much more hands-on with Hel than he was with Lucio. He however is a far more lenient parent than Morga.
• Morga is determined not to repeat the same mistakes she feels she made with Lucio as well as deeply afraid to lose Hel (aside from Jæger and the Devil, she is the only close soul she has left), so she is extremely strict to her daughter.
I suppose I could try and develop more specific headcanons, but those tend to develop with plotline. 😅 I also have no idea how would Lucio react that he has a younger sister... Big Brother™ Lucio sounds kind of fun though... Not for Hel.
*Don't worry, she won't die when the kid is still young. As if the Devil would allow his wife/lover to ever die.
**I mean I could let it be smooth and easy, but where's the fun in that.
#the arcana#the arcana game#the arcana: a mystic romance#the arcana headcanons#the arcana ships#otp#the arcana morga#mama morga#the arcana devil#morga/the devil#the devil x morga#the arcana fanchildren#hel morgasdottir#otp headcanons#fanxhikdren headcanons#morga's second child#medical headcanons#pregnancy headcanons
29 notes
·
View notes
Photo

EBOLA VIRUS CASES IN THE UNITED STATES (August 10, 2017)
Four laboratory-confirmed cases of Ebola virus disease commonly known as "Ebola" occurred in the United States in 2014. Eleven cases were reported, including these four cases and seven cases medically evacuated from other countries. The first was reported in September 2014. Nine of the people contracted the disease outside the US and traveled into the country, either as regular airline passengers or as medical evacuees. Of those nine, two died. Two people contracted Ebola in the United States. Both were nurses who treated an Ebola patient. Both recovered.
On September 30, 2014, the Centers for Disease Control and Prevention (CDC) announced that Thomas Eric Duncan, a reportedly 42-year-old (later corrected by CDC reports as a 45-year-old) Liberian national visiting the United States from Liberia, had been diagnosed with Ebola in Dallas, Texas. Duncan, who had been visiting family in Dallas, was treated at Texas Health Presbyterian Hospital Dallas. By October 4, Duncan's condition had deteriorated from "serious but stable" to "critical". On October 8, Duncan died of Ebola.
The other three cases diagnosed in the United States as of October 2014 were:
October 11, 2014, a nurse, Nina Pham, who had provided care to Duncan at the hospital.
October 14, 2014, Amber Joy Vinson, another nurse who treated Duncan.
October 23, 2014, physician Craig Spencer, diagnosed in New York City. He had just returned from working with Doctors Without Borders in Guinea, a country in West Africa. He was treated at Bellevue Hospital in New York City.
Hundreds of people were tested or monitored for potential Ebola virus infection, but the two nurses were the only confirmed cases of locally transmitted Ebola. Public health experts and the Obama administration opposed instituting a travel ban on Ebola endemic areas, stating that it would be ineffective and would paradoxically worsen the situation.
No one who contracted Ebola while in the United States died from it. No new cases were diagnosed in the United States after Dr. Spencer was released from Bellevue Hospital on November 11, 2014
FIRST CASE: THOMAS ERIC DUNCAN
Thomas Eric Duncan was from Monrovia, Liberia, to date the country hit hardest by the Ebola virus epidemic. Duncan worked as a personal driver for the general manager of Safeway Cargo, a FedEx contractor in Liberia. According to manager Henry Brunson, Duncan had abruptly quit his job on September 4, 2014, giving no reason.
On September 15, 2014, the family of Marthalene Williams, who later died of Ebola virus disease, could not call an ambulance to transfer the pregnant Williams to a hospital. Duncan, their tenant, helped to transfer Williams by taxi to an Ebola treatment ward in Monrovia. Duncan rode in the taxi to the treatment ward with Williams, her father and her brother.
On September 19, Duncan went to Monrovia Airport where according to Liberian officials Duncan lied about his history of contact with the disease on an airport questionnaire before boarding a Brussels Airlines flight to Brussels. In Brussels, Duncan boarded United Airlines Flight 951 to Washington Dulles Airport. From Dulles, he boarded United Airlines Flight 822 to Dallas/Fort Worth. He arrived in Dallas at 7:01 p.m. CDT on September 20 2014 and stayed with his partner and her five children, who lived in the Fair Oaks apartment complex in the Vickery Meadow neighborhood of Dallas. Vickery Meadow, the neighborhood in Dallas where Duncan resided, has a large African immigrant population and is Dallas's densest neighborhood
DUNCANS ILLNESS IN DALLAS
Duncan began experiencing symptoms on 24 September 2014 and arrived at the Texas Health Presbyterian Hospital emergency room at 10:37 pm on September 25. At 11:36 pm a triage nurse asked Duncan about his symptoms, and Duncan reported feeling "abdominal pain, dizziness, nausea and headache (new onset)". The nurse recorded a fever of 100.1 °F (37.8 °C) but did not inquire as to his travel history as this was not triage protocol at the time. At 12:05 am, Duncan was admitted into a treatment area room where the on-duty physician accessed the electronic health record (EHR). The physician noted nasal congestion, a runny nose, and abdominal tenderness. Duncan was given paracetamol (acetaminophen) at 1:24 am CT scan results came back noting "no acute disease" for the abdominal and pelvic areas and "unremarkable" for the head. Lab results returned showing slightly low white blood cells, low platelets, increased creatinine, and elevated levels of the liver enzyme AST. His temperature was noted at 103.0 °F (39.4 °C) at 3:02 am and 101.2 °F (38.4 °C) at 3:32 am. Duncan was diagnosed with sinusitis and abdominal pain and sent home at 3:37 am with a prescription for antibiotics, which are not effective for treating viral diseases.
Duncan's condition worsened, and he was transported on 28 September 2014 to the same Texas Health Presbyterian Hospital emergency room by ambulance. Duncan arrived in the emergency room at 10:07 am experiencing diarrhea, abdominal pain, and fever. Within fifteen minutes a doctor noted that Duncan had recently come from Liberia and needed to be tested for Ebola. The doctor described following "strict C.D.C. protocol" including wearing a mask, gown, and gloves.
At 12:58 p.m., the doctor called the CDC directly. By 9:40 p.m., Duncan was experiencing explosive diarrhea and projectile vomiting.[33] At 8:28 a.m. the next morning, the doctor noted that Duncan "appeared to be deteriorating." By 11:32 a.m., Duncan was suffering from fatigue severe enough to prevent him from using the bedside toilet. Later that day, Duncan was transferred to an intensive care unit (ICU) after all other patients had been evacuated. The next day, September 30, Duncan was diagnosed with Ebola virus disease after a positive test result.
Duncan's diagnosis was publicly confirmed during a CDC news conference the same day. That evening, Duncan reported feeling better and requested to watch a movie. The following morning, Duncan was breathing rapidly and complaining of "pain all over". By the afternoon, however, he was able to eat, and the doctor noted that he was feeling better. The next day, October 3, Duncan again reported feeling abdominal pain. That evening, the hospital contacted Chimerix, a biotechnology company developing Brincidofovir to combat the disease. The next day, Duncan's organs were failing, and he was intubated to help him breathe. In the afternoon, the hospital began administering Brincidofovir. Nurses Nina Pham and Amber Joy Vinson continued to care for Duncan around the clock. On October 7, the hospital reported that Duncan's condition was improving. However, Duncan died at 7:51 a.m. on October 8, becoming the first person to die in the United States of Ebola virus disease and the index patient for the later infections of nurses Pham and Vinson.
Contact tracing
On October 5, the CDC announced it had lost track of a homeless man who had been in the same ambulance as Duncan. They announced efforts were underway to find the man and place him in a comfortable and compassionate monitoring environment. Later that day, the CDC announced that the man had been found and was being monitored.
Up to 100 people may have had contact with those who had direct contact with Duncan after he showed symptoms. Health officials later monitored 50 low- and 10 high-risk contacts, the high-risk contacts being Duncan's close family members and three ambulance workers who took him to the hospital. Everyone who came into contact with Duncan was being monitored daily to watch for symptoms of the virus, until October 20, when health officials removed 43 out of the 48 initial contacts of Thomas Duncan from isolation. On November 7, 2014, Dallas was officially declared "Ebola free" after 177 monitored people cleared the 21 day threshold without becoming ill.
Reactions
On October 2, Liberian authorities said they could prosecute Duncan if he returned because before flying he had filled out a form in which he had falsely stated he had not come into contact with an Ebola case. Liberian President Ellen Johnson Sirleaf told the Canadian Broadcasting Corporation she was angry with Duncan for what he had done, especially given how much the United States was doing to help tackle the crisis: "One of our compatriots didn't take due care, and so, he's gone there and in a way put some Americans in a state of fear, and put them at some risk, and so I feel very saddened by that and very angry with him.…The fact that he knew (he might be a carrier) and he left the country is unpardonable, quite frankly." Before his death, Duncan brazenly claimed that he did not know at the time of boarding the flight that he had been exposed to Ebola; he said he believed the woman he helped was having a miscarriage, which contradicts corroborated accounts from family members who also helped transport the woman to an Ebola ward.
Duncan's family said the care Duncan received was at best "incompetent" and at worst "racially motivated". Family members threatened legal action against the hospital where Duncan received treatment. In response, Texas Health Presbyterian Hospital issued a statement, "Our care team provided Mr. Duncan with the same high level of attention and care that would be given any patient, regardless of nationality or ability to pay for care. We have a long history of treating a multicultural community in this area." The hospital spent an estimated $500,000 on Duncan's treatment. He had no health insurance.
Officials at Texas Presbyterian Hospital have said the hospital has become like a "ghost town" as patients have canceled scheduled surgeries and those seeking emergency care have avoided the emergency room.
The reaction to the care and treatment of Thomas Duncan, and the subsequent transmission to two of the nurses on his care team, have caused several hospitals to question the extent to which they are obligated to treat Ebola patients. Discussions on curtailing treatment are underway at Geisinger Health System, which operates hospitals in Pennsylvania, and Intermountain Healthcare, which runs facilities in Utah, according to their spokesmen. Their concern surrounds the reality that understaffed and poorly equipped hospitals performing invasive procedures, like renal dialysis and intubation, both of which Duncan received at Texas Presbyterian, could put staff at too much risk for contracting the virus. Emory University Hospital in Atlanta also used renal dialysis in treating patients at their biocontainment unit, but no health care workers became infected. In October 2014 Vickery Meadow residents stated that people were discriminating against them because of the incident.
SECOND CASE: NINA PHAM
On the night of October 10, Nina Pham, a 26-year-old nurse who had treated Duncan at Texas Health Presbyterian Hospital, reported a low-grade fever and was placed in isolation. On October 11, she tested positive for Ebola virus, becoming the first perrson to contract the virus in the U.S. On October 12, the CDC confirmed the positive test results. Hospital officials said Pham had worn the recommended protective gear when treating Duncan on his second visit to the hospital and had "extensive contact" with him on "multiple occasions". Pham was in stable condition as of October 12.
On October 16, Pham was transferred to the National Institutes of Health Clinical Center in Bethesda, Maryland. On October 24, the NIH declared Pham free of the Ebola virus. That day Pham traveled to the White House where she met with President Obama
Controversies and lawsuit
Tom Frieden, director of the Centers for Disease Control and Prevention, initially blamed a breach in protocol for the infection. The hospital's chief clinical officer, Dr. Dan Varga, said all staff had followed CDC recommendations. Bonnie Costello of National Nurses United said, "You don't scapegoat and blame when you have a disease outbreak. We have a system failure. That is what we have to correct." Frieden later spoke to "clarify" that he had not found "fault with the hospital or the healthcare worker". National Nurses United criticized the hospital for its lack of Ebola protocols and for guidelines that were "constantly changing". Briana Aguirre, a nurse who had cared for Nina Pham, criticized the hospital in an appearance on NBC's Today Show. Aguirre said that she and others had not received proper training or personal protective equipment, and that the hospital had not provided consistent protocols for handling potential Ebola patients into the second week of the crisis. A report indicated that healthcare workers did not wear hazmat suits until Duncan's test results confirmed his infection due to Ebola, two days after his admission to the hospital. Frieden later said that the CDC could have been more aggressive in the management and control of the virus at the hospital.
On March 2, 2015 The New York Times reported that Pham filed a suit against Texas Health Resources, her hospital's parent company, accusing it of "negligence, fraud and invasion of privacy". Pham was described as still suffering from numerous physical and psychological problems, listing lack of proper training as the reason for her illness
THIRD CASE: AMBER VINSON
On October 14, a second nurse at the same hospital, identified as 29-year-old Amber Vinson, reported a fever. Amber Joy Vinson was among the nurses who had provided treatment for Duncan. Vinson was isolated within 90 minutes of reporting the fever. By the next day, Vinson had tested positive for Ebola virus. On October 13, Vinson had flown Frontier Airlines Flight 1143 from Cleveland to Dallas, after spending the weekend in Tallmadge and Akron, Ohio. Vinson had an elevated temperature of 99.5 °F (37.5 °C) before boarding the 138-passenger jet, according to public health officials. Vinson had flown to Cleveland from Dallas on Frontier Airlines Flight 1142 on October 10. Flight crew members from Flight 1142 were put on paid leave for 21 days.
During a press conference, CDC Director Tom Frieden stated she should not have traveled since she was one of the health care workers known to have had exposure to Duncan. Passengers of both flights were asked to contact the CDC as a precautionary measure.
It was later discovered that the CDC had, in fact, given Vinson permission to board a commercial flight to Cleveland. Before her trip back to Dallas, she spoke to Dallas County Health Department and called the CDC several times to report her 99.5 °F (37.5 °C) temperature before boarding her flight. A CDC employee who took her call checked a CDC chart, noted that Vinson's temperature was not a true fever – a temperature of 100.4 °F (38.0 °C) or higher – which the CDC deemed as "high risk", and let her board the commercial flight. On October 19, Vinson's family released a statement detailing her government-approved travel clearances and announcing that they had hired a Washington, DC, attorney, Billy Martin. As a precaution, sixteen people in Ohio who had had contact with Vinson were voluntarily quarantined. On October 15, Vinson was transferred to the Emory University Hospital in Atlanta. Seven days later, Vinson was declared Ebola free by Emory University Hospital
Monitoring of other health care workers
As of October 15, 2014, there were 76 Texas Presbyterian Hospital health care workers being monitored because they had had some level of contact with Thomas Duncan. On October 16, after learning that Vinson had traveled on a plane before her Ebola diagnosis, the Texas Department of State Health Services advised all health care workers exposed to Duncan to avoid travel and public places until 21 days after their last known exposure
FOURTH CASE: CRAIG SPENCER
On October 23, Craig Spencer, a physician who treated Ebola patients in West Africa, tested positive for Ebola at Bellevue Hospital Center after having a 100.3 °F (37.9 °C) fever. Officials said he was hospitalized with fever, nausea, pain, and fatigue. He had flown to New York City from Guinea within the previous ten days, and contacted the city's Department of Health and Doctors without Borders after showing symptoms. Dr. Spencer traveled to Guinea to treat Ebola victims on September 16 and returned on October 16. He had been self-monitoring for symptoms of the disease, and began to feel sluggish on October 21, but did not show any symptoms for two days. His case was the first to be diagnosed in New York. The city was trying to find people who may have been in contact with Dr. Spencer between October 21 and 23.
On October 22, the day before he had symptoms, Dr. Spencer rode the New York City Subway, walked on the High Line park, went to a bowling alley and a restaurant in Brooklyn, took an Uber to his home in Manhattan, and took a 3-mile (4.8 km) jog in Harlem near where he lived. Three other people who were with Dr. Spencer in the previous few days were quarantined as well. Dr. Spencer's apartment and the bowling alley he went to were cleaned by hazmat company Bio Recovery Corporation. Health officials stated it was unlikely that Dr. Spencer could have transmitted the disease through subway poles, hand railings, or via bowling balls.
New York hospitals, health-workers, and officials had conducted weeks of drills and training in preparation for patients like Dr. Spencer. Upon arrival at the hospital, he was put in a specially designed isolation center for treatment. Not many details about the treatment were given, except that he participated in decisions relating to his medical care. On October 25, the New York Post reported that an anonymous source had said that nurses at Bellevue had been calling in sick to avoid having to care for Spencer. A hospital spokesperson denied there was a sick out. On November 1, his condition was upgraded to "stable", and on November 7 the hospital announced he was free of Ebola. Spencer was released from the hospital on November 11. He was cheered and applauded by medical staff members, and hugged by the Mayor of New York, Bill de Blasio as he walked out of the hospital. The Mayor also declared: "New York City is Ebola free".
As a result of Dr. Spencer's Ebola case, U.S. Senator Charles Schumer (D-NY), proposed an Ebola fund in an omnibus bill to be considered in fiscal year 2015. Schumer said the funds were needed to compensate New York City, as well as other cities treating Ebola patients, in the same way the federal government covers communities that suffer after a natural disaster. Schumer said Dr. Spencer's care at Bellevue Hospital involved around 100 health care workers. In addition, the city's health department established a 24-hour-a-day operation involving 500 staffers to keep track of the approximately 300 persons from West Africa hot spots who arrive in New York every day
2 notes
·
View notes
Text
Physiotherapy Services Oakville
Back pain is a symptom caused (in most cases) by an injury in one or more parts of the spine. It can be located in the upper, middle, and/or lower back.
This article will talk about the most common: Lower back pain, also known as “lumbago”.
It affects nearly 60% to 80% of people throughout their lifetime. This means that 6 to 8 people out of 10 will experience low back pain. It’s the most common cause of disability in young adults: in the U.S. only, an estimated of 149 million work days are lost yearly due to low back pain, costing $100 to $200 billion a year. It’s a costly condition with repercussions in the patient’s life, the overall productivity, and the healthcare system.
It can be caused by numerous reasons, but the root cause is usually a bad posture. Other causes include accidents, sports injuries, and aging. Even though the low back pain can be disabling, it usually improves without surgery in 90% of the cases.
Anatomy Of The Back
To understand the causes of low back pain, let’s make a brief review of each part of the back:
Vertebral Column/Spine. It’s a column formed by approximately 33 bones called “vertebrae”. The spinal cord travels throughout the column. It’s divided into regions:
Cervical: This corresponds to the neck. It has 7 vertebrae.
Thoracic: Corresponds to the chest and the middle back. Has 12 vertebrae.
Lumbar: Corresponds to the lower back. Has 5 vertebrae.
Sacrum: It’s located in the pelvis. Has 5 fused vertebrae.
Coccyx: It’s at the end of the sacrum, where our tail used to be millions of years ago. Has 3-4 fused vertebrae.
Vertebrae. These are the building blocks of the column.They go from the base of the skull to the bottom end of the spine. They protect your spinal cord and help you stand straight. The lumbar vertebrae are the biggest ones. They support most of our weight and are responsible for most of our mobility.
Inter-vertebral disk. These are cushions placed between each vertebra. They have a gel-like nucleus, surrounded by a fibrous ring. They are shock absorbers and help with the mobility of the body.
Spinal cord. It’s a long, thin collection of neurons that goes from the brain to the end of the column. The nerves that go to the upper and lower limbs leave the spinal cord through a hole between each vertebra.
Nerves. They’re a collection of neurons that send and receive instructions from one place to another in the form of electrical impulses, acting like cables.
Muscles. These are the ones responsible for our movements. Each muscle is made of thousands of fibers that fusion themselves to form a cord called “tendon”. The tendon attaches to the bone. When the fibers contract, they pull the bone they are attached to, generating movement.
Ligaments. These are tough, fibrous bands attached to two consecutive bones. They restrict the movement, stabilizing the joints.
Symptoms
The related symptoms of low back pain will depend on the cause, and may include:
Sharp, stabbing, mild, dull, severe, intermittent, and/or constant pain.
Symptoms in one buttock/hip/leg, such as muscle weakness, tingling, numbness, burning sensation.
Worsening with bending, lifting, sitting, standing, and/or walking.
Sciatica symptoms: Pain from the low back down the glute and leg of one side, numbness, tingling, and/or muscle weakness.
Causes Of Back Pain
Back pain can be caused by numerous factors:
Poor Bio mechanics
Human bio mechanics can be defined as the way our joints, muscles, bones, and related structures work together to do what our bodies are supposed to do: Move. Good bio mechanics are translated into a healthy body. Movement allows the proper distribution of blood throughout the body, aiding the transport of the nutrients every cell needs to function.
Poor bio mechanics can occur for a number of reasons, and all of them can cause low back pain:
BAD POSTURE. In our present lifestyle, static postures are kept for long periods of time, i.e. working on a computer or standing all day. The body adapts to that posture overtime, perceiving it as “normal”. Finally, that can cause conditions or injuries like herniated disks or spinal stenosis, which will be described later.
SCOLIOSIS. It’s an abnormal curve of the vertebral column, causing deformity in severe cases. An individual can be born with scoliosis, or develop it through childhood or teenage years. Patients with arthritis can develop scoliosis as well.
OTHER CAUSES. Obesity and flat foot include changes in the biomechanical distribution of the body for long periods of time. Both are risk factors for low back pain.
Disk Injury
The intervertebral disk can get injured as well, causing low back pain and other related symptoms. The most common type of disk injury is the disk herniation:
It’s also known as “slipped” or "ruptured" disk. It happens when the gel-like center of the intervertebral disk pushes against the fibrous ring that surrounds it, squeezing its way through. In early phases of the herniation, the disk has a "bump" that could compress the spinal cord. As it advances, the nucleus can spill into the spinal canal, increasing the compression of the spinal cord and the nerves.
This is a common consequence of a bad posture. The bad posture compresses the intervertebral disk unevenly, e.g. does more pressure in the anterior part of the disk. This pushes the gel-like center backward, forcing its way through and creating the bump in the weakest area of the fibrous ring.
Other causes of disk herniation include:
Accidentally with lifting, pulling, bending, or twisting with heavy loads.
Wear and tear. As we age, the intervertebral disks gradually “dry”, losing their shock-absorbing properties and making them susceptible to injury.
The symptoms of a disk herniation may vary depending on many factors such as: exact place and size of the bump, area of the nerve injured, age... to name a few. They can range from mild to severe low back pain, and often include muscle weakness, tingling, numbness, and/or burning sensation in one leg, as well as gait impairment. Symptoms can last from weeks to even years.
Spinal Stenosis
A stenosis is an abnormal narrowing of a canal within the body. Therefore, a spinal stenosis is an abnormal narrowing of the spinal canal, where the spinal cord goes through.
A common cause of a spinal stenosis is the collapsing of intervertebral disks. This is common with age due to “wear and tear”. The disks lose their normal height and get closer to each other, narrowing the space of the spinal cord. This is also referred as “osteoarthritis”.
The body might respond to this by growing new bone on the edges of the vertebrae - called “spurs”- which worsen the stenosis condition and could compress more nerves.
Symptoms of spinal stenosis resemble the ones of a herniated disk: mild to severe low back pain, and include tingling, burning, weakness or numbness sensations in one limb.
Traumatic Event
Specific movements like bending, lifting, or twisting with heavy loads could cause low back pain. These are usually related to muscular spasms and should cease after 48-72 hours. The pain is commonly accompanied by stiffness and soreness.
Sports Injury
Direct contact sports like rugby or football may cause low back pain. Also, over-activity can cause muscle soreness in the low back muscles. Besides the low back pain, other symptoms include stiffness and soreness that goes away in 2-3 days.
Other Causes
A stressful environment, depression, anxiety, and smoking are risk factors for low back pain.
Red Flags
If you have the following medical history or if you are experiencing the following symptoms with your low back pain, please consult a healthcare professional:
Osteoporosis.
History of cancer.
Constant pain, that doesn’t decrease despite your position or activity level.
Fever, chills.
Unexpected/unintentional weight loss.
Numbness, tingling or weakness in the groin area, both arms or both legs.
Increase of pain with coughing or sneezing.
Burning sensation while urinating.
Problems with bowels/bladder control.
Pain that prevents from sleeping.
Unresponsive back pain therapies.
Treatment
Most of the cases of low back pain -and its emotional and economic consequences- can be prevented with physical activity and an active lifestyle.
For the ongoing cases of low back pain though, physical therapy and massage therapy are two of the best options for a non-invasive treatment to this disabling condition. Both help to reduce pain, improve mobility, and enhance the overall recovery in the short-term:
Physical therapy has shown to be very effective in patients with low back pain. Furthermore, physical therapy treatment in the first two weeks of experiencing lower back pain substantially reduces costs and healthcare resources over a 2-year period. This means quality-life improvement for the patient, reducing or even avoiding painkillers and going back on track faster. (7)
Regardless of how long you’ve been experiencing low back pain, physical therapy without pharmacologic treatment is recommended as the first option of treatment. (8)
Massage therapy has shown to provide significant benefits, including relaxation, pain reduction in the short-term, and increase of mobility. (9)
Pharmacologic therapy is recommended for patients without positive outcomes of these therapies. The last resort will always be surgery.
References
Elrich, G. Low back Pain. Bulletin of the World Health Organization. 2003;81:671-676. Available at:http://www.who.int/bulletin/volumes/81/9/Ehrlich.pdf
Duthey, B. Background Paper 6.24. Low Back Pain (2004). World Health Organization. Available at: http://www.who.int/medicines/areas/priority_medicines/BP6_24LBP.pdf
Hoy, D., March, L., Brooks, P., et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Annals of the Rheumatic Diseases 2014;73:968-974. Available at: http://ard.bmj.com/content/73/6/968
Most Americans Live With Low Back Pain - and Don’t Seek Treatment. From the American Physical Therapy Association. Alexandria, VA. April, 4, 2012. Available at: http://www.apta.org/Media/Releases/Consumer/2012/4/4/
Low Back Pain. American Association Of Neurological Surgeons. Available at: http://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Low-Back-Pain
Low Back Pain. American Academy Of Orthopaedic Surgeons. Last reviewed: Dec, 2013. Available at: https://orthoinfo.aaos.org/en/diseases--conditions/low-back-pain/
Child, J., Fritz, J., Wu, S., Flynn, T., Wainner, R., Robertson, Eric., et al. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC Health Services Research. 2015, 15:150. Available at: https://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-015-0830-3
Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive Treatments for Acute, Subacute, and Chronic Low Back Pain: A Clinical Practice Guideline From the American College of Physicians. Annals of Internal Medicine. 2017;166:514–530. Available at: http://annals.org/aim/fullarticle/2603228/noninvasive-treatments-acute-subacute-chronic-low-
Visit our website www.elitephysiocare.ca
#are you suffering with low back pain? do you want to live with out back pain#visit out website#www.elitephysiocare.ca
2 notes
·
View notes
Text
COVID-19
I’m not convinced there are enough words in the English language to explain how angry I am. Angry about how the government is handling this outbreak. Angry about US health insurance and care. Angry at middle-aged women who buy out entire grocery stores in their neighborhoods. Angry that NO ONE IS ABLE TO GET TESTED FOR COVID-19. Yep. You heard it here first, folks - no one will test you for corona virus, even if you present with all the symptoms. Isn’t that fun?
I should probably start at the beginning of my story. From February 16-18, I travelled by plane to Missouri (which was awesome, btw). About 2 weeks after I returned home, I started having a scratchy throat and a pretty hefty cough. This was around the time COVID-19 was starting to pick up in the US and I was feeling pretty anxious about my newly found symptoms. Instead of googling and self diagnosing, I called a local urgent care to ask what the odds are that I’d contracted COVID-19 and what I should do to keep my loved ones safe. The Urgent Care said that I had reason to be nervous, and recommended that I call the Ontario County Department of Health right away, as they were not equipped to test for COVID-19. I spoke with the nurse from DOH, who said that because I had not travelled to Italy, China, etc. and because I didn’t have a fever, I would not qualify to be tested and I probably just had the flu. I said okay, and went about my business.
About 3 days later, my symptoms worsened and I had developed a pretty high fever and a cough that rattled my entire body (and because I’m in a sharing mood, often left me wetting my pants after each cough). I became more concerned and decided to go to urgent care to get everything settled. The provider at urgent care diagnosed me with bronchitis after the flu test and the strep test each came back negative. The provider prescribed some antibiotics and cough medicine, and sent me on my way. My wonderful husband picked them up from Wegman’s and we went home, where I stayed for several days. Symptoms continued to escalate...my fever would not settle, cough was worse and I was very achey. I scheduled a tele-med appointment for a second opinion, and the provider on my phone camera believed I had pneumonia. I should remind you that COVID-19 is often confused for pneumonia. My parents began to worry and made a few calls for me, insisting that it was important I be tested for the corona virus. I mean, I had just attended a conference with people from all over the country and flew on a plane 4 separate times. After speaking with 3 different providers, it was determined that despite my very serious symptoms, I was not able to be tested for COVID-19. Each provider stated that if my symptoms worsened, I should go to the ER. Finally, I spoke with the nurse from DOH again, who suggested I go back to urgent care to determine whether or not I actually had pneumonia. She said that if they believed I didn’t have pneumonia, she would consider testing me for COVID-19. I headed back to urgent care asking for a chest x-ray and another flu test. After the flu test came back negative (again) and after reviewing the X-ray, they determined I did indeed have pneumonia and that I should just continue to take antibiotics and stay home to rest. Fine. I was on the mend and things seemed to be settling. If I did indeed have COVID-19, I knew I had done everything I could to be safe and proactive by staying home and calling ahead of time. This one was not on my shoulders.
This week, I feel much better, but my sweet husband, Jamil, has begun showing symptoms. His symptoms started with severe body aches and a small cough. I thought it may be best to stay on top of it and suggested he go to urgent care to see if they’d prescribe him antibiotics so he can move through the symptoms quickly. Jamil’s insurance has a $3000 deductible, so when he went to urgent care that day, he paid $120 for a nurse to tell him that his symptoms were not severe enough and they would not prescribe any medication. They told him to come back if his symptoms progressed. After a few days, Jamil’s cough became worse and his aching became almost intolerable and he began having a fever. We decided to make another appointment at our local doctors office to see if they would refer him to be tested for COVID-19. He showed up, was tested for the flu (which came back negative) and was told to go home. The provider mentioned again that if things got worse, he should go to the ER. I called the ER to see if they were providing testing for COVID-19...which, surprise, they were not. They recommended that we call the COVID-19 hotline for more information...super helpful.
Today, after Jamil’s fever spiked to 102.2, I called back the doctors office asking if there was anyway they would prescribe him an antibiotic for pneumonia, as that’s what I had last week and was treated for. The nurse said there was nothing more they could do and that they couldn’t prescribe something without him coming back in. I was not satisfied with this answer and decided to call back urgent care, where we had both previously been treated. The woman there said that Jamil needed to call the COVID-19 hotline before coming in, as it sounded like he had the virus. I explained that NOT ONE SINGLE provider in this area would test Jamil for COVID-19 and that I wanted him to come in, have an X-ray done to see if he had pneumonia and have something (read: anything) prescribed to try to help him manage his symptoms. After some push back, she agreed. We showed up at urgent care, where we were told to call the hotline again. I humored them...maybe something had changed in the last 4 days?
NOPE
After waiting on the line for 20 minutes, the provider from the hotline said it sounded like Jamil had a “mild case” of COVID-19, but he did not qualify to be tested, as he was not immunocompromised and did not travel outside the country in the past month. The hotline said we should go home and if things got worse, call the ER. I relayed this information to the woman at urgent care and demanded he be seen. Jamil was given an X-ray and it was determined that he has pneumonia, but the provider was very concerned and wrote a referral for Jam to be tested for COVID-19 at a local testing area. The nearest testing center is in Rochester (about an hour away). They said we should leave immediately. I asked if the referral meant he would be guaranteed a test, and they said it should, so we drove.
Upon arrival, we drove up to a white tent and spoke with a doctor. He gave us the green light to head to the second tent where they’d determine whether or not Jamil would be tested. Upon driving up to the second tent, we were quickly met by a woman who said that Jam’s symptoms were not extreme enough, so she would not test him, and that we should self quarantine for 14 days. Without a test taken, we drove away. I sobbed. I called my parents who were in disbelief.
THIS is what is happening in NYS right now. I know that there is a shortage of tests in the Rochester area, but they are literally turning people away who are showing symptoms without a second thought. Before Jamil and I showed symptoms, we were out and about and working. I understand that Joe Shmoe who recently had a lung transplant has priority to testing, as he is immunocompromised, but Jesus Christ, how many people in my life are immunocompromised who now don’t get to know whether or not they’ve definitely been exposed to someone with COVID-19?? How many people have Jamil and I been in contact with over the last 3 weeks that will surely be impacted - and how sad that we can’t confirm we’ve actually had the virus and that they need to be quarantined?! This is why I am ANGRY.
I am overwhelmed with anger that I can’t tell my dad, who has Multiple Sclerosis, whether or not he has been exposed to COVID-19. I am irate that Jamil had to tell his work that he probably has a mild case (whatever the fuck that means) of COVID-19, and that he’ll need to take 14 days off from work/will need to work from home without any paperwork or documentation. I am ENRAGED that a bill was passed to ensure that all workers affected by COVID-19 are provided 2 weeks paid sick leave, but I am 98% sure that if they haven’t been tested, they likely won’t be entitled to that paid time off. I am FURIOUS that Trump has told all of America that if they feel sick, they can get tested anytime/anywhere, when that is CLEARLY NOT THE CASE. I am FUMING that the US is short on tests because the government wants to make it look like our confirmed cases number is low, while people are struggling and sick and feeling foolish for thinking they may have COVID-19, but can’t get a solid answer. I am heartbroken that low income families/people from impoverished areas will not be taken seriously when they go to their doctor with illness and symptoms and will not be given an answer that’s helpful or affirming. I am SEETHING that healthcare providers/workers are being put in a situation where they have to choose who is more important for testing, when there are countries administering hundreds of tests daily to keep citizens safe. I am PISSED OFF that there are still people going out and about when there is a LITERAL PANDEMIC happening.
For fuck’s sake, just stay in your house. And call your representatives to let them know that WE ARE NOT BEING TESTED and that people’s lives are at risk. Thanks for coming to my Ted Talk. Just had to get that off my chest.
3 notes
·
View notes
Text
Important: How to Use Antimicrobial Herbs to Heal Your Gut
Antimicrobial herbs are the top natural treatment for gut issues, like SIBO, dysbiosis, parasites and yeast overgrowth.
Here’s all you need to know and how to use them.
Antimicrobial Herbs 101
Herbal therapies have been used for centuries as the preferred “drugs” of choice for addressing illness—from stomach aches, viruses, colds and flu’s.
Long before researchers mentioned the words “gut microbiome,” people knew there was powerful healing in nature’s medicine for reversing disease.
Types of Antimicrobial Herbs
Some of these powerful herbal agents include:
Peppermint
Berberine
Garlic (Alicin)
Olive Leaf
Oregano Oil
Grapefruit Seed Extract
Pau d’arco
Black Walnut
Resveratrol
Licorice
Echinacea
Goldenseal
Oregon grape
Barberry
Wormwood
Thyme
Stinging Nettle
Uva Ursi
Yerba Mansa
Caprylic Acid
Cat’s Claw
Manuka honey
Tea tree oil
Curcumin
Clove
Cinnamon
Astragalus Root
Colloidal silver
“Antimicrobial” protocols—herbal therapies—are often part of a “healing” gut protocol if dysbiosis (too much or too little gut bacteria), SIBO, fungal or yeast overgrowth, parasites or gut infections are identified as a “root cause” behind poor health. Treatment of these “gut issues” typically a two-stage treatment approach:
Eradicate or reduce pathological organisms
Restore a healthy gut microbiome
In most cases of dysbiosis, except for significant fungal overgrowth, a short period of antimicrobials (30-60 days) commences, followed by a more significant focus on restoring the healthy gut microbiome.
Generally speaking, a blend of botanical herbs in supplement form is recommended for most cases of dysbiosis for a “broad spectrum” approach to healing. However, depending on the certain pathogenic organisms identified on a stool or SIBO breath test, some people find treating specific organisms with research-backed specific agents may be effective (such as grapefruit seed extract for the overgrowth pseudomonas aeruginosa).
Lastly, given the fact that antimicrobial herbs can be powerful, is also recommended you combine antimicrobial treatment with adjunct supports to aid in both complete eradication/reduction of pathogenic organisms, as well as the preservation of any healthy bacteria you do have. Support agents for an antimicrobial protocol include:
Antimicrobial Treatment: Support Agents
Quality probiotic & symbiotic (a probiotic + prebiotic).
To maintain a healthy gut microbiome as some bacteria die off. (Ideally taken away from antimicrobial herbs; particularly a soil-based bacteria). Medium-chain fatty acids extracted from coconut oil that are antiparasitic in addition to being antifungal, antiviral, and antibacterial. Great for boosting immunity and warding off yeast.
Biofilm Disruptor.
Pathogenic bacteria can form biofilm around their outer layer—sort of like “steel armor” for preventing destruction. Biofilm may be one of the primary drivers of resistance and treatment failure in multiple disease, antimicrobial and/or antibiotic treatments. Biofilm disruptors help break up biofilm to allow your other antimicrobial agents to work. (ex. NAC, Cranberry, Biocidin, Colloidal silver, Xylitol, Manuka honey, Interfase Plus)
Least Restrictive “Real Food” Diet.
Many people go on an “anti-candida,” ketogenic or “no carb” diet while “healing their gut.” However, these can be counterproductive to resetting your gut microbiome, given the fact that some starchy plants and pre-biotics are needed to feed healthy gut bacteria and bring pathogenic bacteria “out to play.” Prebiotics found in starchy plants and veggies help your antimicrobials work even better (so there is bacteria for them to target). Aim for 1 to 2 servings per day of starchy plants and/or prebiotic fibers while on an antimicrobial herbs protocol.
“But isn’t medicine more powerful?”
Herbal therapies are at least as effective as rifaximin—the typical conventional antibiotic treatment for resolution of gut dysbiosis (i.e. SIBO, candida, parasites and IBS)—if not more. In one study, 104 patients diagnosed with SIBO with the lactulose breath test were treated either with Rifaximin (1,200 mg) or a cocktail of herbal antimicrobials (see below) for 4 weeks before repeating the lactulose breath test.
The study showed that 46% of the patients treated with herbal antimicrobials were successfully treated while only 34% were free of SIBO after taking Rifaximin (1).
Recommended Antimicrobial & Support Agents to Buy
Here are my top recommended supplements for using in your “gut healing protocol.”
Antimicrobial Herbs
Biotics FC Cidal + Dysbiocide
Roasted Garlic
Symbiotic Probiotic
Seed Probiotic
Soil Based Probiotic
Terra Flora
Monolaurin
Lauricidin
Biofilm Disruptor
Interfase Plus
-or-
Biocidin
Sample Antimicrobial Protocol
Pre-Breakfast:
Symbiotic Probiotic (probiotic + prebiotic)
Breakfast
Antimicrobial Herbs (broad spectrum supplement)
Monolaurin
Mid-Morning
Biofilm Disrupter
Lunch
Soil Based Probiotic
Mid-Afternoon
Biofilm Disrupter
Dinner
Antimicrobial Herbs (broad spectrum supplement)
Monolaurin
Post Dinner
Herbal Tea (optional)
Antimicrobial Protocol Treatment Timeline
Dysbiosis-Pathogenic (high amount of pathogenic and/or commensals bacteria): 60 Days
Dysbiosis-Healthy Overgrowth (high amount of “beneficial” bacteria on stool test and possibly yeast markers): 30 Days
Insufficiency Dysbiosis (lack of healthy bacteria with a few pathogenic bacteria): 30 Days, followed by emphasis on Probiotics & Prebiotics
Parasites: 60 Days
SIBO: Low/Mild: 30 Days, Moderate: 60 Days, High: 90 Days
Beware: Herx (“Healing”) Reactions May Happen
A die-off reaction, also called a Herxheimer reaction or “Herx reaction”, can occur whenever you first start a new supplement or antimicrobial protocol—often a sign of a “detox” or die off of certain bacteria.
Typically, Herx symptoms develop within a couple of hours to several days after treatment and last anywhere from a few days to several weeks or months—depending on the severity of the underlying pathology you are treating. However, depending on the location of the bacteria, symptoms may develop later. The Herxheimer reaction is especially seen during antimicrobial treatments (gut healing protocol) because antimicrobials destroy numerous microorganisms and bacteria.
Although the Herxheimer reaction is typically not harmful, it does frequently cause temporary pain, discomfort, and worsening of symptoms. Symptom severity is often indicative of the level of inflammation triggered by the immune system.
Common symptoms that may develop or worsen due to a Herxheimer response include:
Bloating
Brain Fog
Chills
Cold Sweats
Constipation
Cramps
Diarrhea
Fatigue
Fever
Headaches
Irritability
Joint Pain
Lethargy
Muscle Pain
Nausea
Skin Irritation
Sore Throat
Because of the sudden worsening of symptoms, it is common for patients to feel that the severity of their condition has increased due to the treatment. However, even though treatment causes a temporary increase in symptom intensity due to greater release of toxins the condition ultimately improves. The body responding in this way usually means that the treatment is actually working effectively.
Nevertheless, even though a Herxheimer reaction indicates that treatment is working effectively, it doesn’t make the patient’s condition any more comfortable in the immediate.
Fortunately, there are several ways of limiting the symptoms of a Herxheimer reaction without inhibiting treatment efficacy. The following suggestions can and should be used when detoxing, using antibiotics, or being treated for infections and other forms of chronic disease to limit Herxheimer intensity, including:
How to Deal with HERX Reactions
Drink H20. Drink plenty of fluids to aid in the removal of toxins and help cleanse the GI tract.
Get Your Zzzz’s. The body conducts many restorative processes while at rest that it cannot accomplish when it is awake. When experiencing a Herxheimer reaction due to greater toxicity, it is best to allow more time for quality sleep.
Sweat. Sweat it out with heated yoga, sauna and daily movement—a natural essential for detoxification.
Try Dry Brushing & Rebounding. Two lymphatic “cleansing” tactics to help flush the lymphatic track.
References
Chedid, V., Dhalla, S., Clarke, J. O., Roland, B. C., Dunbar, K. B., Koh, J., Justino, E., Tomakin, E., … Mullin, G. E. (2014). Herbal therapy is equivalent to rifaximin for the treatment of small intestinal bacterial overgrowth. Global advances in health and medicine, 3(3), 16-24.
The post Important: How to Use Antimicrobial Herbs to Heal Your Gut appeared first on Meet Dr. Lauryn.
Source/Repost=>
https://drlauryn.com/gut-health/antimicrobial-herbs-heal-gut-naturally/ ** Dr. Lauryn Lax __Nutrition. Therapy. Functional Medicine ** https://drlauryn.com/
10 notes
·
View notes
Text
Sicknesses and Diseases in Forgotten Curse
Name: Vocal sickness.
Symptoms:
Whenever the sufferer tries to speak, it's replaced with something else, such as: Screaming, singing, sneezing, or some other form of sickness.
In more severe cases the diseased may get spots all over them, though this shows up later in the case.
Cause, Diagnosis, and Prognosis:
Usually induced by a curse or magical item, but it has been known to happen from going where you shouldn't, or eating the green and yellow striped mushrooms known as sound shrooms. It's usually diagnosed rather early on, as it's hard not to notice random singing or screaming or other such things mid sentence or conversation. Generally the affected goes and gets help before it comes to the more severe spotted stage. Though if they do not, or cannot get help, they may reach the point where they cannot speak other than the screaming, singing, sneezing, or other such vocal effect they got. This is generally when they begin to get spots, and if allowed to stay around for long enough, may become incurable. Or at least, the effects would stick around much more easily.
Cure:
A poultice on the throat made of boiled sound shrooms, blue berries, and Spinivy fruit juice, replaced about every 24 hours until the symptoms are gone, or in more severe cases, dulled.
Name: Walking shadow
Symptoms:
Joint pain,
shadow desyncronization,
loss of shadow,
a voice in your head not your own
Cause, Diagnosis, and Prognosis:
Usually occurs after a soul related spell gone wrong, or heavy magic trauma. The first symptom is joint pain, barely noticeable for the first week, then getting worse in the following weeks after that. After about three weeks, the individual may notice shadow desynchronization. This gradually gets worse, until after about seven weeks, where the shadow starts to develop it's own voice. Eventually, the shadow may detach from the affected, and depending on the relationship established, it may stick around, or it may go somewhere else. Fortunately this is a fairly rare disease.
Cure:
There is none, have fun with your shadow, you aren't getting that piece of your soul back.
Name: Magic overload
Symptoms:
Headaches,
fever,
nausea,
nose bleeds,
mood swings,
hallucinations,
wild magic,
and loss of emotions.
Cause, Diagnosis, and Prognosis:
Usually occurs after magical trauma, though some have claimed it brought on by other things. Magic overload is an excess of magic that causes your emotions to first swing wildly, then eventually, dampen, or completely disappear. The extra magic of this sickness is often wild and uncontrollable, and comes with headaches, fever, nausea, nose bleeds, hallucinations, and mood swings. Though these symptoms decline as the affected loses their emotions.
Cure: Generally love and affections can help bring about feelings again, but they'll never be quite as great as they were unaffected. With help, wild magic can be tamed, though it will still occasionally lash out.
Name: Sparking sickness
Symptoms:
mood swings,
sneezing,
fever,
yellowing of selcras,
narrowing of pupils,
reddening of irises,
discolouration of the skin,
hot flashes,
and sparks when the afflicted sneezes
Cause, Diagnosis, and Prognosis:
The cause of this uncommon disease is not certain, but believed to have something to do with sparkweed. Sparking sickness usually gets to the phase where the eyes start changing colour before it's diagnosed. The sickness, left untreated, continues to worsen to the point where the victim reaches the trademark sparks of the sickness. The afflicted is often bedridden at that point.
Cure: Sparkweed, burnt and ground up, mixed with blackberries, and the mixture is drunk. Some of the features of the sickness may stick a little bit after being cured.
Name: Blinding blitz
Symptoms:
Dizziness,
migranes,
hallucinations,
blurring of sight,
and blindness
Cause, Diagnosis, and Prognosis:
A curse, likely gained by pissing off a spellcaster, it's not particularily specific in it's symptoms at first, so it's not often caught until it's enough to see a doctor about. It starts off with dizziness or migranes, though sometimes both, the symptoms getting worse over the course of a month. If the affected completes a full year without fufilling the requirements of the curse to be broken, they go blind.
Cure: Fufill the given requirements of the curse.
Name: Greyscale
Symptoms:
Discolouration of afflicted,
flaking skin/shedding,
weakness in grey areas,
loss of limb
Cause, Diagnosis, and Prognosis:
Greyscale is a quick running sickness that leaves the afflicted discoloured and potentially without a limb, there is no known cause. It's fairly easy to spot early on, as a victim's entire hand or foot may be discoloured within the first few days of the sickness. The sickness runs for about a week, and may disable an entire limb of the victim.
Cure: You have to just wait it out I'm afraid.
#worldbuilding#vocal sickness#walking shadow#magic overload#sparking sickness#blinding blitz#greyscale#None of these would be fun to catch
5 notes
·
View notes
Text
Rheumatoid Arthritis Affecting Your Movement?
What is it
Rheumatoid arthritis is a chronic and degenerative disease that is characterized by causing inflammation of the synovial membrane (membrane that nourishes, protects and covers the cartilage) of the joints and surrounding tissues. Sometimes arthritis can have an extra-articular behavior and damage organs and systems such as the heart, kidney and lung. For this reason, rheumatologist in Delhi describe it as a systemic disease.
The inflammation of this membrane is responsible for the pain, the clearly visible swelling, the sensation of stiffness that patients can feel in the mornings and the loss of joint mobility.

According to the best rheumatologist in Delhi, it affects joints more intensely than others, mainly the more mobile ones such as the hands and feet, the elbows, the shoulders, the hips, the knees and the ankles. There are some that are never affected.
If the swelling remains in a sustained and not controlled can end up damaging the bones, the ligaments and the tendons there around the joint. This can cause a progressive deformity of the joints and the loss of the ability to perform daily movements and tasks. All this affects the quality of life of patients, says top rheumatologist in Delhi.
Incidence
According to arthritis specialist in Delhi, it is estimated that worldwide this pathology affects between 0.5 and 0.8 percent of the population, that is, approximately five people per thousand worldwide. However, there are still many people who are not diagnosed.
According to arthritis doctor in Delhi, in India there are more than 1,000,000 people with rheumatoid arthritis and each year 20,000 new cases are diagnosed. "This is a remarkable figure because rheumatoid arthritis is the most disabling of rheumatic diseases," best arthritis specialist in Delhi explains.
Its incidence is greater in women than in men. In fact, for every 3 diagnoses in women, only one is performed in men. Although it can affect any person and appear at any age, it usually manifests itself more frequently in women from 30 to 50 years old.
Within the same geographical area there is a tendency to greater occurrence in urban versus rural areas.
Causes
The cause of the onset of this disease is unknown. Infectious agents such as bacteria or viruses have been studied and, although suggestive data have been found in some cases, there is still no evidence to confirm their involvement.
Rheumatologist in Delhi believes that it may have a genetic origin since the immune system attacks the joints because they do not recognize them as their own and therefore become inflamed. What is known as autoimmune disease. Likewise, it is believed that certain proteins that are transmitted in a hereditary way could predispose to the disease.
The differences in the frequency of the disease make the arthritis specialist in Delhi also suggests that there are environmental factors that intervene in the onset of the disease.
Symptom
As indicated by the best rheumatologist in Delhi, the disease begins slowly and insidiously with general manifestations that present other diseases, such as fever or asthenia.
However, the main symptom of this disease is the involvement of the diarthrodial joints. Initially there is an inflammation that is noticeable to the naked eye and causes pain in the individual who suffers. Along with inflammation, other manifestations may appear, such as increased volume, stiffness after night time rest that gradually disappears as the patient exercises daily activity, muscle weakness and limited mobility.
Also, hard lumps (rheumatoid nodules) may appear in areas of skin friction such as the elbows, the back of the fingers and toes, which can also be located inside the body.
If the disease is at an advanced stage, the patient may have some deformity due to the progressive deterioration of the affected joints. In addition, it can evolve and affect vital organs such as the kidney or lung.
It often causes dryness of the skin and mucous membranes. This causes inflammation and subsequent atrophy of the glands that generate tears, saliva, digestive juices or vaginal discharge (Sjögren's syndrome).
It can also cause some fever and, sometimes, inflammation of the blood vessels (vasculitis), which causes nerve injuries or sores on the legs (ulcers). Other symptoms are inflammation of the membranes lining the lungs (pleuritis) or the envelope of the heart (pericarditis), or inflammation and scarring of the lungs can cause chest pain, difficulty breathing and abnormal heart function.
"In the long term, the consequences of the disease left to its evolution are the limitation and incapacity for the realization, initially, of the work activities and, later, of the daily life of the subject who suffers it.
Prevention
Currently there is no measure to help prevent the onset of rheumatoid arthritis. However, Joint pain specialist in Delhi recommends regular physical activity to promote the use of all joints.
In addition, once rheumatoid arthritis has been diagnosed, they recommend following arthritis treatment in Delhi appropriately to prevent the progression of the disease.
Diagnosis
Although there are no specific tests, the diagnosis of this pathology is relatively simple if the patient goes to the rheumatologist on suspicion of having some of the symptoms already described.
If the disease is in an initial phase, the diagnosis can be more complicated since all the symptoms may not appear in the laboratory tests, since the assessment of the disease is mainly clinical. "It is done in the presence of a series of signs and symptoms in the joints in the form of polyarthritis (arthritis of multiple joints) of symmetrical nature), chronic course (more than 6 weeks) and with practically constant involvement of hand joints", specify by top rheumatologist in Delhi.
The problem in diagnosing it is that there are other rheumatic diseases, such as lupus or psoriatic arthritis that in the early stages can be confused with rheumatoid arthritis.
During the evaluation, the rheumatologist in Delhi can perform a series of complementary examinations to facilitate the diagnosis:
Blood test.
Rheumatoid factor tests.
Test to detect antibodies against citrullinated peptides. These antibodies are present in two thirds of patients with this condition.
X-rays to detect the presence of erosions.
Treatments
Rheumatoid arthritis is a chronic disease that currently has no treatment to cure the disease. However, pharmacological therapies and treatment strategies are very effective and allow good control of the disease.
The best arthritis treatment in Delhi includes two types of drugs: those used to relieve pain (anti-inflammatories and corticosteroids), and those that serve to modify the disease in the long term. The latter can be effective weeks or even months after treatment. They are not effective in one hundred percent of patients, according to arthritis specialist in Delhi, so the doctor usually prescribes several sequentially to find one that is more effective and better tolerated by the patient.
The mainstay of the therapy is the antirheumatic drugs that modify the disease (Fames). Among them, the most used is methotrexate. Other drugs would be sulfasalazine, leflunomide or gold salts (now disused).
According to the arthritis doctor in Delhi, the early prescription of these treatments is essential to reduce to the maximum the joint inflammation and the progression of the disease.
In cases where the Fames do not work properly, the joint pain specialist in Delhi treats the pathology with biological therapies. These are drugs designed with complex formulas that include the TNF antagonists (etanercept, adalimumab and infliximab), abatacept and rituximab. These drugs have been shown to be very effective in improving pain and inflammation and in preventing joint destruction.
Both biological therapies and Fames can have side effects, but in general they are quite safe and patients tolerate them well.
If the disease is very advanced, the patient may need surgery.
Other data
Relationship with tobacco
Numerous studies have shown that there is an association between tobacco consumption and the development of the disease. However, best arthritis specialist in Delhi indicates that the causal relationship between smoking and the development of pathology is complex.
On the other hand, studies have also shown that patients who smoke suffer from the disease more severely than those who are not smokers.
Forecast
The prognosis of the disease is very variable, since in some cases there are benign diseases that can be controlled with a simple treatment and others in which the disease evolves very quickly and the prognosis is fatal in a short time.
If joint pain treatment in Delhi is not done properly, it is usual for the disease to evolve towards irreversible joint destruction with a deterioration of the important lung capacity. This prognosis varies if it is approached with the optimal treatment.
In addition, there are risk factors that worsen the prognosis: the onset of the disease at young ages, smoking, the existence of citrullinated antiprotein antibodies or rheumatoid factor or the involvement of other organs, for example.
Living with the disease
The first step that a person diagnosed with rheumatoid arthritis should take to adapt to their illness is to avoid a hectic life, sudden movements and try to sleep an average of 10 hours.
In addition, it is advisable that these patients avoid those jobs that require intense physical exercise. During the workday, they should maintain a straight position in the seat and avoid remaining with the neck or back flexed for a long time. Also, during the rest it is convenient to maintain a proper posture, avoid bending the joints and keep the arms and legs stretched.
Regarding footwear, arthritis specialist in Delhi advises that it be elastic, firm and leather. The heel should be attached, the wide toe and the instep high enough so that chafing does not occur.
The obesity can cause an overload on joints, therefore, try to lead a healthy and balanced diet and avoid gaining weight.
#arthritis treatment in Delhi#best arthritis treatment in Delhi#rheumatologist in Delhi#top rheumatologist in Delhi#best rheumatologist in Delhi#joint pain treatment in Delhi#joint pain specialist in Delhi#arthritis doctor in Delhi#arthritis specialist in Delhi#best arthritis specialist in Delhi
1 note
·
View note
Text
Bipolar Disorder
Bipolar disorder is a mental health disorder characterised by periods of depression and periods of mania.
Potential symptoms of mania include:-
Erratic, impulsive behaviour
Rapid, uninterruptible speech
Poor decisions based on unrealistic ideas
Short attention span
Reduced sleep
Racing thoughts
Elevated mood
Irritability
To be classifed as mania, the symptoms need to be present for at least 1 week and must impair an individual’s ability to work and/or socialise.
There are 4 types of Bipolar DIsorder.
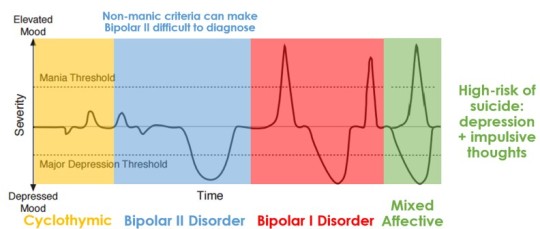
Cyclothymic
Sequential periods of minor depression and hypomania
Hard to diagnose as patient may not realise they are having an episode
Bipolar II
Sequential periods of depression and hypomania
Easily mistaken for depression due to less obvious manic symptoms
Bipolar I
Sequential period of depression and mania
Mixed Affective
Simultaneous depression and mania
Low mood from depression combined with impulsiveness from mania leads to a greatly increased risk of suicide.
Bipolar Disorder is difficult to diagnose as there are no chemical markers. Tests can be done to rule out other possible conditions, but diagnosis generally relies on history taking by the patient and friends/family. The first symptoms that present are usually depressive symptoms so it can easily misdiagnosed as depression.
Aetiology
Bipolar Disorder has both genetic and environmental factors that may contribute to its cause. However, it is not fully understood how these are linked.
Genetic Factors
60% to 80% of patients are related to someone with Bipolar Disorder
~67% chance of developing Bipolar Disorder if identical twin has Bipolar Disorder
~19% chance of developing Bipolar Disorder if non-identical twice has Bipolar Disorder
There are some candidate risk genes that are thought to increase someone’s chance of having Bipolar DIsorder
Environmental Factors
Early life stress such as trauma or abuse may increase a person’s chance of having Bipolar Disorder
Kindling Hypothesis
The Kindling Hypothesis suggests that whenever someone with a genetic predisposition to Bipolar Disorder experiences a stressful event, the stress threshold at which their mood changes is gradually decreased until episodes can start spontaneously
Pathophysiology
Neuroanatomy
Enlarged Lateral and 3rd Ventricles
Decreased brain size
Smaller hippocampi
Decreased grey matter
Neurotransmitters
Increased activity/levels of Noradrenaline, Serotonin and Dopamine
Neurotrophic Factors
Biological elements that direct growth/maturation
Decreased levels of Brain-Derived Neurotrophic Factors
Treatment
Therapies for Bipolar Disorder include Lithium, Anticonvulsants, Antipsychotics, Cognitive Behavioural Therapy and Electroconvulsive Therapy.
Pharmacological
Lithium
Mechanism of action not fully understood, but it decreases Noradrenaline release and induces the synthesis of Serotonin
Important side effects include:-
Nephrotoxicity
Teratogenic
Hypothyroidism
Dehydration
Does not induce mania in non-bipolar patients
Anticonvulsants
Called mood stabilisers when used in Bipolar Disorder
e.g., Carbamazepine
Causes a blockade of Voltage-Gated Sodium Channels
Can only treat the episodes of Mania
Can cause Agranulocytosis
e.g., Sodium Valproate
Thought to cause a blockade of Voltage-Gated Sodium Channels
Thought to increase levels of GABA
Can only treat the episodes of Mania
Teratogenic
e.g., Lamotrigine
Causes a blockade of Voltage-Gated Sodium Channels
Causes a blockade of Voltage-Gated Calcium Channels
Antagonise 5-HT3 receptors
Can be used to treat both the Manic and Depressive episodes
Teratogenic
Antipsychotics
Only the Atypicals (2nd Generation) can be used as the Typicals (1st Generation) are more anti-mania rather mood stabilisers and so may worsen depressive episodes
e.g., Clozapine, Olanzapine, Risperidone, Aripriprazole
Olanzapine most commonly prescribed
Antagonise D2 and 5-HT2A receptors
Side effects include:-
Extrapyramidal side effects
Extrapyramidal tracts act to modulate and regulate movement
Controlled by the nigrostriatal pathway in the basal ganglia
Slow movement, and slow initiation of movement
Spasms of neck and face muscles
Motor restlessness
Antipsychotic Malignant Syndrome
Life threatening
Muscles cramps
Tremor
Fever
Unstable autonomic nervous system
Increased prolactin secretion
Prolactin promotes milk production
Blockade of tuberohypophyseal pathway
Breast swelling
Lactation
Period cessation
Weight gain
May antagonise H1 receptors
Increase appetite via stimulating production of AMP-activated protein kinase
Decreased lipolysis
Decreased thermogenesis
Sedation
May occur due to D2 receptor antagonism in the mesocortical pathway
May occur due to central H1 receptor antagonism
Hypotension
May antagonise α1 adrenoreceptor
Vasodilation
Anticholinergic effects
May antagonise muscarinic acetylcholine receptors
Dry mouth
Blurred vision
Constipation
Urinary Retention
Cognitive Behavioural Therapy
Based on the concept that thoughts, feelings, physical sensations and actions are interconnected, and that negative thoughts and feelings can create a vicious cycle.
Help deal with overwhelming problems in a more positive way by breaking them down into smaller parts.
Looks for practical ways to improve your state of mind on a daily basis.
Electroconvulsive Therapy
‘Restarts’ the brain
Only used in severe cases where symptoms are debilitating and other treatments have not worked.
#bipolar#mental health#medicine#treatment#health#bipolar disorder#psychology#depression#mania#hypomania#Bipolar I#cyclothymia#Bipolar II#uni#mental disorder
15 notes
·
View notes
Text
Scientists discover COVID-19 antibodies present in survivors 3 months after infection
Previously unknown immunity behavior revealed as researchers study immune memory factors in survivors of mild COVID-19 infection.
I am one of 113 million mild COVID survivors worldwide. The research about antibody presence after COVID infection has only reviewed severe and critical hospitalized patients, leaving immunity information about the largest COVID survivor demographic relatively unknown.
It had been a difficult spring. I was diagnosed with COVID-19 at the beginning of March 2020 and a few days later the World Health Organization declared an official global pandemic. The chills, fevers, incessant coughing, shortness of breath, asthma attacks, headaches, bone deep fatigue and weakness, chest pain, intense nausea and loss of appetite, fluctuating heart rate, brain fog, and the lost sense of taste went on from March until May. Twice a day for 1.5 months, I was monitored at home by my local hospital clinical COVID response team through phone and video conferencing with them urging me into the Acute Respiratory Clinic (ARC) whenever my symptoms worsened and then into the Emergency Room (ER), whenever I showed signs of blood clots or respiratory discomfort. During my infection, I was in the ARC and ER 6 times. Despite the intensity of my symptoms, my infection was considered mild-moderate, and after my PCR COVID-19 tests finally came back negative in mid-May, I worried if my body made antibodies to keep me protected for the rest of the pandemic as new variants were emerging. I never wanted to be that sick again.
Researchers in Seattle, Washington had similar concerns about antibody development in survivors of mild COVID infection. The Pacific Northwest had experienced the earliest cases of COVID-19 in the USA.
LB Rodda and a team of researchers in the Department of Immunology at University of Washington School of Medicine studied a group of mild COVID survivors comparing them to people who never had COVID infection. The researchers compared blood samples of both groups over a 3 month period at two checkpoints to see if the COVID survivors had COVID -specific antibody presence immediately after their infections and monitored if that presence would remain in their bodies.
Rodda and his team discovered that mild COVID survivors developed antibodies to both the binding receptor domain and to the spike protein of SARS-CoV-2, the virus that causes COVID-19. This means that their immune systems recognized the surface protein of the the virus and developed antibodies against the virus, as well as, built antibodies against the fragment of the virus that binds to our body’s ACE 2 receptors, meaning it could prevent the virus from entering human cells. The study further showed that the mild COVID survivors continued having these antibodies present in their blood for 3 months after their infection. This suggests that lasting immune memory of the pathogen is present and will most likely continue on in these survivors.
These findings are promising and a sigh of relief for the million of mild COVID survivors as we continue on into the pandemic, and it provides deeper understanding of how our immune systems are responding to this novel virus and disease.
0 notes