#what is the risk factor for lung disease?
Link
In addition, the Doctors of asthma Bhawan suggest various other therapies which help in to cure asthma attacks. Hence, it’s necessary to consult recommendations from doctors for good respiration throughout the monsoon to manage an asthma attack. Make an appointment. Call us Tel: +0141-2235005 or Mob: +91-93529 345315 and get more information about How to Manage Asthma during Monsoon?
#what stands for asthma?#world health organization (who)#how omicron virus affect asthma patient?#How to Improve Asthma in Winter- Precautions and Treatment#How it is Dangerous for Asthma PatientsNeoCov#How to Improve Child Immunity During Covid-19?#what can protect your child against covid-19#what is tomato flu or tomato fever? know its symptoms | causes | prevention#what did asthma patients need to know during covid-19?#what is the risk factor for lung disease?#asthma treatment#Best Asthma Treatment in Rajasthan#asthma disease#ASTHMA and COVID-19#lung disease#Why COVID-19 vaccine is important?#What Are The Long-Term Lung Problems After Covid-19?#How to Manage Asthma during Monsoon?#Does Smoking Cause Lung Cancer?#How Does Dostarlimab Cancer Drug Work?#triggers and tips to manage asthma#best asthma treatment#Best Asthma Treatment in India#tips to manage asthma#allergy#allergy symptoms#allergy treatment#summer disease#Skin Problems during Summer and their Prevention#summer skin disease
0 notes
Link
Dr. Nishtha Singh is one of the best-qualified pulmonologists and Asthma and Chest Specialists in Jaipur. She has special training in the prevention, diagnosis, and treatment of lung and respiratory diseases.
Book an appointment today or call us Emergency Line (+91) 946 1685 766
#what is cancer#lung cancer#lung cancer treatment#types of cancer treatment#how to prevent lung cancer#lung specialist#lung#lung disease#Risk Factors for Lung Cancer#smoking and lung disease#smoking#Seasonal Allergies Treatment in Jaipur#Chest disease Experts in India#Chest specialist in Jaipur#chest specialist in india#How Does Smoking Cause Lung Cancer?#Smoking Cause Lung Cancer?#What Are the Risk Factors for Lung Cancer?#asthma#asthma treatment#asthma specialist in jaipur#Coronavirus and Asthma#ASTHMA and COVID-19#How Summer Heat Affects Asthma Patients#Summer Heat Affect Allergy Patients#How you can prevent your Skin Problems in summer?#Skin Problems in summer#How does Summer Heat Affect Allergy Patients?#smoking and cancer
0 notes
Text
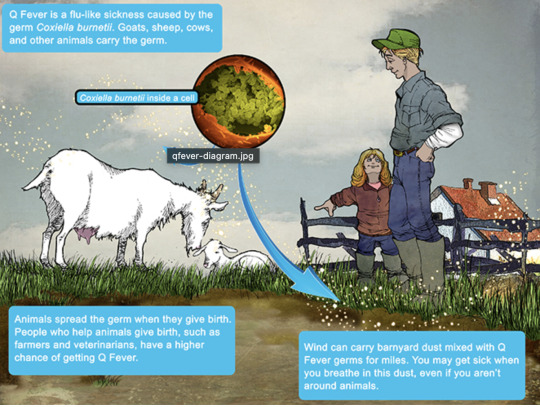
Q Fever
Aka, Query fever. What a weird name for a disease. Imagine telling people that's what you got.

in the 30s-40s, an Australian pathologist in QLD/Brisbane, came across an outbreak of the same or similar illness among abbatoir or slaughterhouse workers.
At the time, he called the disease "Q" fever or query as a temporary name until the pathogen could be identified. Unfortunately it stuck.
decades later, now nobel prize winner and virologist, MacFarlane Burnett isolated and identified the microbe responsible. I think this discovery contributed to his prize. i forget already.
Microbe responsible: Coxiella burnetti. Named for Burnett and HR Cox, the American bacteriologist who found the genus Coxiella where C burnetti falls under.
Initially they felt it was related to Rickettsia, responsible for Rocky Mountain Spotted Fever, but as science progressed, this was disproven.
Now for a Case Report
A 55 yo Italian man with a history of aortic valve replacement was diagnosed with pyrexia of unknown origin twice. Further signs included myalgias/splenomegaly/night sweats. The 2nd time he was admitted for PUO he deteriorated rather dramatically and was put on meropenem and teicoplanin.
A host of organisms was tested for on serological testing based on the man's travel and epidemiological history, all negative. Even a rheumatological panel was done, also less revealing. He also had a history of MGUS (a haem disoder), which is kind of a red herring here.
Cultures were negative, no vegetations were seen on a TTE - so they did consider IE. Which is an important differential for PUO.
Eventually a PET-CT was done (often favoured when investigations do not yield much for a sick patient with fevers), finally revealing a focus of infectious on his ascending aorta, where he'd also had previous surgery done. And in a round about way, they also further identified Coxiella Burnetti. He was treated doxycycline and hydroxychloroquine. As it's so rare in Italy, it wasn't really considered even though he mentioned rural travel.
Bottomline: Q Fever is an important consideration in the work up for culture negative IE. Further to this, always consider IE in the differentials for PUO particularly if they're at increased risk for IE (prosthetic valves, damaged valves, select congenital heart issues, previous IE). IE can present with night sweats, fevers, weight loss and splenomegaly. It can be insidious and chronic in nature. other risk factors can be more suggestive as we'll get into below.
Causative organism
Coxiella burnetti, it's a zoonoses - i.e. transmissible from animals. Special powers: very tough/hardy, can survive extreme environments (high temps and UV light etc.) over prolonged periods and is resistant to many common disinfectants/surface cleaners.
It's an intracellular pathogen and gram negative coccobacilli (PINK!)
name coccobaccili reminds me of cocopuffs.
it's mainly associated with farm animals, which the CDC so wholesomely displays on its website on Q fever (wtf).

goats, sheep, cattle typically (but many other animals, even birds, dogs and horses can be reservoirs)
in particular bodily fluids - amniotic fluid, placenta, faeces/urine, milk etc.
you can get it through unpasteurized milk and through inhaling it if it lands on dust in the area
ever visit a farm or petting zoo lately? OMG WASH YOU HANDS.

That said, it's typically inhaled in inorganic dust. You inhale it, it goes to the lungs, and then the bloodstream.
Increased risk for Coxiella burnetti (What to take on history of exposures and when to strongly consider it)
live on a farm or near one
exposure to a farm
work as a vet on a farm
farm worker, dairy workers, researchers on these animals/facilities
slaughterhouse/abbatoir
Also from CDC:
Clinical presentation
Most won't get sick after exposure and remain asymptomatic, a very small minority does. even though it is highly infectious.
incubation time is 2-3 weeks (consider this time in your history of exposure, did they work on the farm 2-3 weeks ago as opposed to yesterday).
Nonspecific acute infectious symptoms:
nonspecific systemic fevers/malaise/arthralgias/myalgias--> key is high fevers though and can be associated with headache and photophobia.
non specific GI - N/V/diarrhoea
respiratory ones - SOB or cough, consider it as atypical cause of community acquired pneumonia.
rare: hepatitis and jaundice (granulomatous) or encephalitis with neurological complications such as demyelinating disease or CN palsies, also haemolytic anaemia and HLH (yikes)

really it's the history of exposure that will lead you down the garden path to Q fever.
Chronic Q fever is perhaps worse, and can present as culture negative IE/PUO. Months/years later, as B symptoms as above above + LOW/LOA, night sweats. More likely to occur if you are predisposed for IE as above, have a weakened immune system for any reason, including pregnancy.
Chronic Q fever has a mortality of 10% if left untreated. About <5% of those with acute Q fever develop this if left untreated. Speculation is that it's more of an autoimmune process or abnormal immunological response to the bacteria.
To be honest, most who walk in the door with community acquired pneumonia get treated empirically for atypicals anyway, (standard course of doxycycline), so we hardly really ponder the question of Q fever in every patient. But if they present chronically and did not have atypical cover at the onset of acute symptoms, then it's something important to consider.
Other important conditions - can cause complications in pregnant women and 20% will get post Q fever syndrome. like chronic fatigue.
investigations
Serology! nice and easy. Look for IgG antibodies in the chronic presentation. Or PCR. Down side to serology - can take 2-3 days for the body to make said antibodies to the bacteria for detection. PCR can be done on any fluids/tissue sent.
Cultures useless, hence it fall under the umbrella of culture negative (hard to grow outside a host cell, it is an obligate intracellular pathogen).
Other hints on bloods (as serology/PCR takes time to return) - elevated or low platelet's, transaminitis with normal bili, opacities in CXR with hilar lymphadenopathy, CSF will show raised protein levels if done when encephalitis is suspected.
imaging can also support the diagnosis.. as illustrated by the case report.
Treatment
Acute disease - as standard for atypical bugs, doxycycline 100 mg BD for 14 days. Alternatives - TMP SMX or Clarithromycin.
Chronic Q fever or IE:
native valves: doxycycline and hydroxychloroquine (200 TDS) for 18 months
prosthetic: same but 24 months
why hydroxy: enhances the action of doxycycline (increases the pH of the phagolysosome)
Follow-up: look for 4 fold decrease in IGG
Sources:
CDC
Stat Pearls
Wiki as linked above
#australian history#medblr#medblrs#infectious disease#infectious diseases#q fever#coxiella#coxiella burnetti
68 notes
·
View notes
Text
i feel like i am going insane
this post was on my dash (screencapped bc don't go harass OP):
I'm not going to claim to be a TB expert, but any post talking about how we "have a cure" should be regarded as suspect. What happened in 1958 wrt TB treatment? I have no clue, and I just skimmed multiple reviews of the history of TB. If anyone knows, please tell me. In general the 1950s was the golden age of antibiotics, plus there was just a general better understanding of disease management in general, meaning fatalities from TB in Europe and North America tanked. But I could find no specific thing attributed to 1958.
What is the cure for TB? It's months of antibiotics, and even then clearance of the bacteria isn't going to be 100% of all patients. There's no specific miracle drug. There are vaccines (idk how effective, but they show up randomly in all sort of papers for having interesting and positive off-target effects, like improving blood glucose levels in diabetics), which is not a cure but IS a very important tool for stopping the spread and protecting people.
TB is tricky to manage. It can lay dormant in your lungs for decades. It's harder than the average bacteria to kill with antibiotics, and the course of antibiotics needed is so long that you end up with more logistical issues (what happens if you're in a remote area where you have limited supplies? how do you ensure patient compliance?). There are more and more antibiotic resistant strains appearing. A lot of effort and money and brilliant minds are dedicated researching TB and implementing strategies to manage it across the world. I'm sure there are ways to improve our approaches to managing and treating it, but TB is by no means a "neglected" disease. TB is not the example I would pick for how we have failed the world on a global level due to resource hoarding, unless you want to go into a much more nuanced discussion of why poverty is a huge risk factor for contracting it in the first place (due to things like overcrowding, poor living conditions, and poor access to healthcare, not because some specific miracle cure is being hoarded).
But I guess "the problem is we're not DISTRIBUTING the CURE" is much easier take for people to pat themselves on the back for having. TBH I think a lot of people feel safer when they think complex problems are secretly very simple ones that can be fixed by overcoming one singular evil.
33 notes
·
View notes
Text
The Myth of Normal: Trauma, Illness and Healing in a Toxic Culture (Gabor Maté, 2022)
“The gender gap in health is real, if underappreciated.
Women are more subject to chronic disease even long before old age, and they have more years of poor health and disability.
“Women have it worse,” a leading U.S. physician wrote recently, pointing out that women are at much higher risk of suffering chronic pain, migraines, fibromyalgia, irritable bowel syndrome, and autoimmune conditions like rheumatoid arthritis.
As noted in chapter 4, rheumatoid arthritis strikes women three times more often than it does men, lupus afflicts women by a disproportionate factor of nine, and the female-to-male ratio of multiple sclerosis has been rising for decades.
Women also have a higher incidence of non-smoking-related malignancies. Even when it comes to lung cancer, a woman who smokes has double the chance of developing the disease.
Women also have double men’s incidence of anxiety, depression, and PTSD. (…)
Early childhood mechanisms of self-suppression are reinforced by persistent, gendered social conditioning.
Many women end up self-silencing, defined as “the tendency to silence one’s thoughts and feelings to maintain safe relationships, particularly intimate relationships.” This chronic negation of one’s authentic experience can be fatal.
In a study that followed nearly two thousand women over ten years, those “who reported that, in conflict with their spouses, they usually or always kept their feelings to themselves, had over four times the risk of dying during the follow-up compared with women who always showed their feelings.”
As at home, so on the job. Another study showed that for women with non-supportive bosses, the squashing of anger—a natural adaptation to an environment in which to self-express would be to risk the loss of employment—increased the risk of heart disease.
Recall from chapters 5 and 7 this array of self-abnegating traits that predispose to disease: a compulsive and self-sacrificing doing for others, suppression of anger, and an excessive concern about social acceptability.
These personality features, found across all autoimmune conditions, are precisely the ones inculcated into women in a patriarchal culture.
“I was denying myself as a person, denying my own desires, my wants,” the first responder Liz said.
“I was not paying attention to what I needed. Everyone else was far more important. My job was way more important than any concern that I had. I wasn’t listening to myself in any regard.”
That “not listening to self” in order to prioritize others’ needs is a significant source of the health-impairing roles women assume.”
18 notes
·
View notes
Photo

A couple of countries have managed an alternate route to lower emissions: Denmark and the Netherlands both have bicycle-focused transportation that gets many people out of cars entirely. An international team of researchers decided to look into what factors have enabled these countries to make that shift and what might happen if more countries adopted a similar transportation focus. The Dutch use bicycles to move around more than in any other country, cycling an average of about 2.6 kilometers (1.6 miles or 2.6km) a day. If the whole world biked as much, over 680 million tons of CO2 emissions could be avoided every year. That’s enormous — roughly equivalent to erasing one-fifth of CO2 emissions from passenger cars globally in 2015. Also, cycling can improve both physical and mental health, and can reduce the chances of experiencing many health problems. For instance, regular cycling stimulates and improves your heart, lungs and circulation, reducing your risk of cardiovascular diseases. Source: The Verge (link in bio) #bikes #climatechange #biking https://www.instagram.com/p/Ch7aD6nuU8Q/?igshid=NGJjMDIxMWI=
30 notes
·
View notes
Text
A few weeks ago several people I hang out with all got COVID around the same time. My partner and I were clearly exposed. But we didn't manifest normal 'sick' symptoms: no fever, no runny nose, no cough, no shortness of breath.
However my partner noticed she overheated more than normal when doing a more strenuous task on a cool morning. Similarly, I was doing heavy garden work on a cool morning and felt overly warm and tired, and took longer than normal to feel rested and bounce back.
I noticed repeatedly I had more trouble than normal, thermoregulating, over the next few days. It resolved quickly, I'm now back to normal in the thermoregulation department.
The last time we both had COVID, we noticed this same phenomenon during our recovery, even though that time we had a fever and she tested positive (I never did.) We each experienced unexpected episodes of heat exhaustion, she at work, and I on a walk on a hot afternoon.
I think trouble thermoregulating can be a symptom of COVID even in the absence of fever or other classic symptoms.
I wish people were studying this or talking about it. I searched and found nothing.
It seems plausible that what is going on is that COVID stresses the vascular system, which, among other things, is used to thermoregulate. You can have these symptoms even with no lung symptoms. People talk as if COVID is primarily a respiratory disease but for many people it primarily has cardiovascular manifestations. This may be why asthma is not a risk factor for death by COVID whereas heart disease is.
Our experience suggests that you can have very mild cases, borderline asymptomatic even, and never test positive, yet still have stress on your cardiovascular system.
Pay attention to this stuff. Check weather, and listen to your body. If you feel hot and others don't, or you're feeling hot and cold at the same time, especially if these reactions are not normal for you, especially if you may have been exposed to COVID, maybe take it easy. You may be more vulnerable to heat exhaustion or worse, during a brief recovery window, and you may also be contagious, who knows?
3 notes
·
View notes
Text
EXTRA; ABOUT COPD

disclaimer: i‘m no medical professional. this is based on research alone. please contact me if the information provided is untrue.

what is copd?
copd, short for chronic obstructive pulmonary disease, is a progressive type of lung disease, with the two most common contributors being emphysema (condition in which the alveoli at the end of the smallest air passages (bronchioles) of the lungs are destroyed) and chronic bronchitis (inflammation of the lining of the bronchial tubes, which carry air to and from the air sacs (alveoli) of the lungs). even thought it is a progressive disease which gets worse over time, it is treatable, allowing people to still achieve symptom control and a good quality of life.
sign and symptoms
signs and symptoms include shortness of breath, cough and exacerbations.
copd often also occurs alongside other conditions like cvd, skeletal muscle dysfunction, metabolic syndrome, osteoporosis, depression, anxiety and lung cancer.
complications
copd can cause various complications including respiratory failure, pulmonary heart disease, lung cancer, depression, anxiety and pneumothorax
risk factors
risk factors include exposure to tobacco smoke, exposure to dust and chemicals, exposure to fumes from burning fuel, pollution, asthma and genetics, the major genetic risk factor being aat deficiency.
diagnosis
the most common way to diagnose copd is through spirometry. doctors can also assess their patients through the mrc breathlessness scale and the copd assessment test.
treatment
many people with copd have rather mild forms and therefore only requiring little therapy.
copd can be treated by medication taken on regular basis such as bronchodilators, inhaled steroids, combination inhalers, oral steroids, phosphodiesterase-4 inhibitors, antibiotics and theophylline. further therapies are lung therapies like oxygen therapy and a pulmonary rehabilitation program. for people with severe emphysema surgery is also an option, like a lung transplant. lung volume reduction surgery or a bullectomy.
statistics
copd is the third leading cause of death worldwide. the five year mortality rate ranges from 40-70%, depending on the severity.
men are more likely to suffer from copd.
it is estimated that between 7-19% of the world population suffers from mild to severe copd.
most people are over 40 years old when their first symptoms develop. younger people developing copd are often linked to aat deficiency
smoking accounts for up to 8/10 copd-related deaths.

evanescent
/ɛvəˈnɛs(ə)nt,iːvəˈnɛs(ə)nt/ — “soon passing out of sight, memory, or existence; quickly fading or disappearing.”
mlist
#₊❏❜ ⋮evanescent#iwaizumi x reader#haikyuu x reader#haikyuu smau#haikyuu angst#hq smau#iwaizumi x you#iwaizumi hajime#haikyuu social media au#haikyuu imagines#hq x you#hq x reader
13 notes
·
View notes
Note
disability pride ask!!
1. 5. and 9.
Thanks!
mentions of disability down below
cw vomit
1. what disability/ies do you have? (and are they mental, physical, or both?)
I do have a whole catalogue of different kinds of disability - I call them my main three. Heart, Lungs, Esophagus.
I have esophageal atresia. Basically my esophagus was disconnected from my stomach and was also connected to my windpipe instead. Had to be artifically stretched and widened. Nearly doesnt bother me anymore but i have slight problems eating and a scar on my stomach from the feeding tube i used to have.
I have 3rd degree asthma and only one side of my lung working proberly; also caused through the first disabilty and a lung collapse i had. Also have a chronic cough.
Heart is well the main thing. I have 4 different kinds of heart diseases. They cause low blood pressure, circulatory problems and an underdeveloped heart muscle. I at times have problems moving my arms to a certain extend without them hurting. Because of one of those heart diseases i am at high risk for strokes and brain bleeding.
And well on top of that depression and dermatillomania.
5. if you have multiple disabilities: do they affect each other? how?
People with esophageal atresia have commonly heart diseases so this goes hand in hand. My lungs are shit thanks to it as well and complications during the operation. Everything is connected. When i have circulation problems I am very often nearly throwing up as well. Aka exhaustions makes me vomit
9. how do you measure your energy? (spoons, battery, something else?)
I dont have a fancy name for it. My energy levels changes from day to day and also are influenced by weather and temperature and other factors. But i think its more like a battery for me - but some that can be recharged.
5 notes
·
View notes
Text
Content warning: weight and fitness related talk as they pertain to medicine.
Got another Medscape email which was about this. Basically an article describing some research study linking VO2max to cancer risk and mortality (specifically: colon cancer risk, and lung and prostate cancer mortality- also specifically only in men)
Okay, cool, it’s fun knowledge to have but imo i can’t see the Curbsiders calling this research particularly practice changing. Overall help messaging too- cardio exercise is in fact good!! And thankfully they did factor in other variables (although using self report for some of them) like additional disease/comorbidities, smoking (self report based on a categorical # of cigs a day), dietary habits (self report of general good/poor rating, not standardized), and somehow they added BMI in there too.
But here is something I really dislike… they use vo2max which is based on weight but then also say they adjusted for BMI in the models.
The fact is, BMI - and body fat - play a role in vo2max. I’m not joking; fat mass is actually a better predictor of vo2max than your physical performance on a cardio test.
Admittedly I haven’t looked into HOW they adjusted for BMI (like, I’d need to more about the math behind the adjustments), but it seems extra silly to make your main “risk groups” something that is weight dependent and then say you adjusted for a variable that is also weight dependent later on.
I need to do more reading about the topic of maximal oxygen uptake and fitness- but atm I’m curious what would happen if we ran studies not based on vo2max per body mass but per “fat free” or lean body mass. Otherwise I feel like we always have some strong lurking variables that hide in the vo2max measurement itself.
(It’s kind of like how when body fat% ranges were being set, some researchers set values not based on health criteria, but based on correlation with BMI…. And then we ran with those numbers… and then we claim body fat% is a better indicator of health than BMI. It’s recursive)
2 notes
·
View notes
Link
Make an appointment with your doctor if you have any persistent signs or symptoms that concern you. If you don’t have any signs or symptoms, but are worry about your risk of cancer, discuss your concerns at Best Lung Cancer Treatment In India. Hence, call us Tel: +0141-2235005 or Mob: +91-93529 345315 and get more information about What is Dostarlimab Cancer Cure? How Does Dostarlimab Cancer Drug Work?
#what is dostarlimab cancer cure#How Does Dostarlimab Cancer Drug Work?#lung disease#treatment of lung cancer in india#Best Lungs Cancer Diagnosis in Rajasthan#Best Lungs Cancer Diagnosis in India#Cancer Diagnosis Centre in Jaipur#Cancer Diagnosis Centre in India#cancer#Dostarlimab Cancer Cure#Cancer Drug#Cancer Cure#Childhood Asthma: Symptoms Diagnosis and Treatment | Asthma and Lung Cancer Treatment Center#cancer treatment#Asthma#omicron virus#coronavirus#what can protect your child against covid-19#what is tomato flu or tomato fever? know its symptoms | causes | prevention#what is the risk factor for lung disease?#what did asthma patients need to know during covid-19?#What Are The Long-Term Lung Problems After Covid-19?#Smoking Treatment in Jaipur#Smoking Treatment in Rajasthan#Why COVID-19 vaccine is important?
1 note
·
View note
Text
Op-Ed: We're starting to understand 'long COVID.' We can fight it - Los Angeles Times

...While its incidence among adults who have been infected has been estimated at 5% to 40%, a recent study that tracked symptoms before infections and compared participants to controls has given us one of the best snapshots to date. It indicated that 1 in 8 people who have had COVID experience prolonged symptoms over many months.
With vaccinations and different variants, the incidence may be lower, but even if it were half as many (6% of adults who have been infected), and we assume two-thirds of adults have had COVID, that would equate to more than 10 million Americans who have endured persistent symptoms that interfere with their daily life activities, frequently impairing their ability to return to work.
One of the mysteries: As opposed to those most likely to get severe COVID, the vast majority of people affected by long COVID are younger (30 to 50 years old) and previously healthy. The typical symptoms include marked fatigue, exercise intolerance, difficulty breathing, brain fog, muscle pain and weakness, chest pain, headaches and fast heart rate. While the list of troubling symptoms is long, the number of proven therapies is very short — zero.
...A combined team from Yale and Mount Sinai used artificial intelligence to determine what, of so many factors, may be of central importance in determining whether a COVID patient develops lingering symptoms. There was a singular driver — low cortisol in the blood — a particularly intriguing finding.
...While these studies have helped illuminate potential biomarkers, we still do not have one that has been validated in large numbers of people with long COVID, which is essential to provide an objective measure. Large studies will also be needed to determine effectiveness of treatments inspired by these findings.
...The “long” in long COVID has not been emphasized enough. A new report from more than 1.25 million people with COVID showed an increased risk of developing brain fog, dementia, seizures and psychosis over two years. Similarly, follow-up at one year or longer has shown an increased risk of heart and blood vessel diseases, diabetes, clotting disorders, and lung and kidney damage, even among people who had only mild to moderate COVID and were not hospitalized. Such risk appears to be cumulatively increased with reinfections, including infections that break through vaccinations.
While we await a validated biomarker and effective treatments, what can we do about long COVID? First off, we can drop the skepticism and denial. Long COVID is real, and it takes a real toll. In the latest study, which followed patients and controls for an average of 400 days, there is a very close tracking of self-reported symptoms with objective markers — in fact 94%.
The recent relaxation of mitigation measures by the Centers for Disease Control and Prevention is premature, at a time when COVID hospitalizations are at a plateau for adults at more than 40,000, four times what they were in April, and still rising for children. Fortunately, children are at very low risk for long COVID, but the rare cases are linked with a doubling of some serious sequelae such as cardiovascular events.
...Too many people are indeed living with chronic COVID, detracting from their daily lives. As we eventually emerge from this pandemic, long COVID will be the enduring, major public health complication that we failed to address in a timely and aggressive manner. It’s not too late to invest in understanding and combating it.
6 notes
·
View notes
Photo










National Take the Stairs Day
National Take the Stairs Day is celebrated every second Wednesday in January. You know what that means: celebrate the day by hitting the stairs. Elevator? What elevator? If you’re interested in taking things up a notch, run around the block or cycle to work. It doesn’t matter what you do, as long as you keep that heart rate up.
Lung health is more important now than ever before. Did you know that over 3.7 million Americans live with chronic lung diseases like asthma or lung cancer? We’re not moving as much as we should. To top it, the air we breathe gets increasingly unhealthy. Some factors may be beyond our control, but staying fit and healthy is entirely in our hands. Take the first steps towards a healthier life today. What matters eventually are the choices we make.
History of National Take the Stairs Day
The first mention of Take the Stairs Day was in 2016. A dedicated stair-running group likely organized it, although there’s not much documentation on the event.
On the other hand, National Take the Stairs Day is a recent initiative by the American Lung Association. The goal is to improve our lung health by choosing a life of movement over convenience.
Stair walking is excellent exercise and one of the easiest things to do. It’s gentler on our joints and muscles compared to HIIT or gym workouts, with almost similar benefits. It’s an activity to seriously consider if you’re looking to lose weight, tone muscle, and enhance overall cardiovascular health.
Taking charge of our health can sometimes feel daunting. Where does one begin? The good news is you don’t need to make drastic alterations to your lifestyle, unless medically advised. The key lies in little but consistent steps each day. They really do go a long way. Small changes such as choosing to take the stairs instead of an elevator can significantly reduce the risk of chronic diseases.
National Take the Stairs Day hopes to encourage Americans to make changes to their lifestyle. By taking part, you also show support for the millions of people who live with debilitating lung disease. If a few minutes of climbing stairs can make your lungs explode, imagine what it’s like for those with chronic pulmonary disease. It can be a humbling reminder of how lucky we are to be alive. We hope everyone takes the stairs today and every other day.
National Take the Stairs Day timeline
8000 B.C. - 2000 B.C. The First Ornate Staircases
As human civilization progresses, the people of ancient Mesopotamia build magnificent staircases in their homes.
2016 A Day For Taking Stairs
The internet first hears of Take the Stairs Day.
2019 Backed By Science
Researchers at McMaster University find that short bursts of stair climbing throughout the day can boost cardiovascular health.
2020 A Guinness Record For Stair Climbing
On November 18, Ryoji Watanabe from Japan breaks the world record for the fastest vertical mile stair climbing, at one hour, six minutes, and 58 seconds.
National Take the Stairs Day FAQs
When is National Take the Stairs Day?
Organized by the American Lung Association, National Take the Stairs Day takes place on the second Wednesday in January each year. The association encourages Americans to improve their lung health by taking the stairs instead of an elevator.
What are the benefits of stair climbing?
Stair climbing comes with tremendous health benefits. A few minutes of stair climbing throughout the day improves lung capacity, heart function, and blood circulation. It also reduces the risks of developing chronic heart diseases, cancer, diabetes, and hypertension.
How many stairs should I climb for a good workout?
Try climbing up and downstairs on 10 to 12 steps for about 30 minutes. Climb one step at a time and progress to skipping steps once you’re comfortable. For intense calorie burn, climb up and down a 10-story building five times.
National Take the Stairs Day Activities
Take the stairs
Design a stairs-climbing challenge
Climb stairs for a killer cardio burn
Wherever you can, choose to take the stairs today. Find opportunities throughout the day: on a lunch break, coffee run, or en route to the break room.
The good thing about stairs is you’ll find them everywhere. Gather everyone for a stairs-climbing challenge at the office or apartment complex. It can be a surprising way to bond. Take care to offer support to anyone who may be struggling.
Start incorporating stair climbing into your workout. Jog up a few flights each day, increasing the pace as you go along. Level up by skipping one step or carrying a heavy backpack on your way up.
5 Facts About Exercising That Will Blow Your Mind
Let the music take control
Exercising is good for the brain
Bring on the muscles
Slows down aging
Variety is super important
Listening to music during a workout can improve performance by 15%.
Cardio-intensive exercises help create new brain cells, improving brain power and memory.
People with more muscle mass burn more fat amounts while resting.
Those who exercise for 45 minutes, three times a week can significantly reduce signs of aging.
Compared to those who cross-train, people who don’t switch up their workouts are more susceptible to injury.
Why We Love National Take the Stairs Day
It challenges us
Gratitude for our lungs
A community endeavor
The comfort of familiar things lulls most of us into complacency. When was the last time you challenged your body and mind? It’s time today to get up and move. If not now, when?
Breath is life, but we don’t notice it at all. When we take the stairs, we are reminded of how hard our heart and lungs work. That exploding sensation in the chest? It means we’re alive.
Staying fit and healthy can be a lonesome road. National Take the Stairs Day recognizes the importance of the community's rallying around better health. It’s easier when everyone’s in it together.
Source
#Sonoma State Historic Park#Denver#California#Colorado State Capitol#USA#summer 2022#architecture#cityscape#Domaine Carneros#travel#North Window Arch#Arches National Park#landscape#Utah#Earthquake Fault#Mammoth Lakes#Freemark Abbey Winery#St. Helena#Hess Collection Winery#National Take the Stairs Day#11 January#NationalTaketheStairsDay#original photography
3 notes
·
View notes
Text
Interview by Stephanie Desmon
Until now, people who suffered mild or asymptomatic COVID-19 were thought to have dodged the brunt of the virus’s brutal side effects. But new evidence has revealed that anyone infected with COVID is at higher risk for heart issues—including clots, inflammation, and arrhythmias—a risk that persists even in relatively healthy people long after the illness has passed.
In this Q&A, adapted from the March 9 episode of Public Health On Call, Ziyad Al-Aly, director of the Clinical Epidemiology Center and chief of Research and Education Service at Veterans Affairs St. Louis Health Care System, talks with Stephanie Desmon about COVID-19 and the heart, including his recent study, which found a significant risk of heart problems in people a year after being diagnosed with COVID.
You just published a study that says that in some people who’ve had COVID, heart issues can persist for a year or more. What does this mean and what did you study?
We've known for a while that during the acute phase—the first 30 days of COVID-19—people who have severe disease and need to be admitted to the hospital or ICU may develop heart complications. We didn't know what happened to people's hearts in the long term—six months to a year out—or what happened to people who had mild disease and did not need hospitalization or ICU care.
We did this study to evaluate the one-year risk of heart problems in people who got COVID-19, compared to nearly 11 million controls of people who did not.
What did you find?
The major finding was that people with COVID-19 have a higher risk of all sorts of heart problems at one year. That included arrhythmias (irregular heart beats or the heart beating too fast or too slow) and atrial fibrillation (a fast heart rhythm in a particular pattern). We found evidence of an increased risk of stroke, of blood clots in the legs and the lungs, and of heart failure and heart attacks. The increased risk of a broad spectrum of heart problems was evident.
I went into it thinking that [the risk] was going to be most pronounced and evident in people who smoked a lot or had diabetes, heart disease, kidney disease, or some [other] risk factors. What we found is that even in people who did not have any heart problems start with, were athletic, did not have a high BMI, were not obese, did not smoke, did not have kidney disease or diabetes—even in people who were previously healthy and had no risk factors or problems with the heart—COVID-19 affected them in such a way that manifested the higher risk of heart problems than people who did not get COVID-19.
It was really eye-opening that the risk was also evident in people who did not have severe COVID-19 that necessitated hospitalization or ICU care. People who got COVID-19 and were asymptomatic, or got COVID-19 that was so mild that they were able to nurse it at home, without going to the doctor still developed an increased risk of heart problems a year out.
What's going on in the body?
A lot of different things could be happening. It's possible that the virus itself and the immune response to it cause an intense inflammation that subsequently hits the heart and results in some of the manifestations we've seen here. It's possible that COVID-19 may attack the endothelial cells that line the vessels of the heart. Some of these cells might die and eventually facilitate the formation of blood clots and blockages of the arteries or vessels of the heart.
There are several other mechanisms that revolve around something called the ACE receptor. The virus has something called a spike protein, which is like a key that engages a lock—the ACE receptor. That allows the virus into cells, including heart cells.
Why would SARS-CoV-2, the virus that causes COVID 19, which we all thought about as a respiratory virus, attack the heart up to a year down the road? That’s likely one of the explanations.
This study was done before vaccination was widely available. Is there any indication that, for example, breakthrough infections would have a different result long term?
Yes. We are [studying] this, but I think the jury is still out. We're certainly very interested in addressing that publicly as soon as we can.
You studied Veterans Administration records, and that population is mostly men, white, and older. Do you feel that [the findings] apply to the entire population?
Yes and no. I think we have to be cognizant that this study comes from one system, the VA system, but that needs to be put into a larger context. This is a study of nearly more than 11 million people. People tell me most vets are males, but 10% are females—meaning our study has more than 1 million females. Similarly, 20% [of study participants] are Black—more than 2 million people.
In addition to this, we did subgroup analyses to see what would happen in only women, only men, only Black people or white people, people younger than a certain age or older than a certain age. Across the board we saw an increased risk of heart problems. This tells us that it doesn't matter if you are a female or male, Black or white, older or younger, diabetic, a smoker, have chronic kidney disease or other cardiovascular risk factors, or not. The risk was across the board, and it’s driven by COVID-19. It really spared no one.
The jury's still out on all of the things that long COVID might encompass. Would this fit into that category?
Absolutely. Long COVID is the umbrella term that describes all the post-acute manifestations that happen as a result of COVID-19. It could be things that started in the acute phase that lingered and persisted into the long term, or it could be new things attributable to SARS-CoV-2 that have happened three, four, or five months out. When you have that definition in mind, it's very clear that the heart manifestations we described in our report are part and parcel of the broader picture of long COVID.
Long COVID can give you fatigue and brain fog and result in new-onset diabetes, kidney problems, and heart problems. All of that collectively forms a multilayered, multifaceted long COVID. That's not to say one patient will have all of these things.
Are we going to have a lot of people who have some form of long COVID and are chronically ill? Will it be a strain on government resources? What do you see as the future?
I think that's why talking about it is very important. We think long COVID can affect anywhere between 4% and 7% of people. That seems really small, but it’s not if you multiply that number by the huge number of people infected with COVID in the U.S., more than 80 million people and counting. We think that will translate into millions of people with long COVID in need of care, and broadly speaking, our health systems need to be prepared. People running health systems or clinics need to start preparing for the tide of patients that are going to hit our doors with heart problems and other long COVID problems.
On a government level, I think we definitely need to be prepared for this. We cannot move on from the pandemic and disregard its long-term consequences. Arguably the long-term consequences are going to be even more profound and stick with us and scar a lot of people around us for generations.
A lot of the manifestations we're describing in this report are chronic conditions that will [affect] people for a lifetime. For example, heart failure isn't something that you wake up tomorrow and all of a sudden don't have. That's not how it works. We're no longer talking about things that might improve tomorrow—we're seeing chronic conditions that will require care for a long time. People, health systems, and governments need to be prepared for that.
1 note
·
View note
Text
Exercising during Pregnancy
Exercise may not be very high on the agenda of a lot of people, however if you want to exercise during pregnancy , it is important to know that it is completely safe. Just remember to consult your gynaecologist before commencing any exercise regime.
The best time to start exercising during pregnancy is any time after the first trimester. The American College of Obstetricians and Gynaecologists (ACOG) recommends 30 minutes of moderate intensity exercise on most or all of the days of the week. However, if you have not exercised for a long time, you can start with small bouts of exercises (e.g. 15 minutes) and then gradually increase the duration of exercise.
You can keep your exercising up until the day of delivery, that is if your pregnancy is complication free. It depends completely on your comfort or whatever your doctor advises.
Remember comfort first when deciding what to wear while exercising. Loose clothes might come in your way while tight ones may be uncomfortable. So, find your balance.
Why should you consider exercising during pregnancy?
Pregnancy is no picnic so adding exercise to the mix may seem daunting in the start but it has its own benefits. Exercise:
Maintains healthy blood sugar levels and keeps blood pressure in check.
Eases and prevents body aches and injuries.
Speeds up your recovery process post-delivery and prevents post-partum musculoskeletal dysfunctions.
Boosts mood and reduces fatigue.
Improves blood supply to the baby and ensures better brain growth and oxygen levels during pregnancy.
Enables better performance during labour and delivery.
Exercise with caution, in case of:
Anaemia
Pregnancy induced high blood pressure.
Any other risk factors
And do not exercise if you have the following complications during your pregnancy:
Certain types of heart and lung diseases
Cervical Insufficiency
Placenta previa after 26 weeks of pregnancy
By The Womans Company
2 notes
·
View notes
Text
The Critical Role of Asbestos Re-Inspection Surveys in Ensuring Safety and Compliance
Asbestos, once hailed for its durability and resistance to heat, has become synonymous with health risks and stringent regulations. Understanding and managing asbestos risks is crucial for ensuring safety in buildings. This guide delves into the importance of asbestos re-inspection surveys, explaining their purpose, process, and benefits.

What is Asbestos?
Definition and Common Uses
Asbestos is a group of naturally occurring fibrous minerals known for their heat resistance, strength, and insulating properties. Historically, asbestos was used extensively in construction materials such as insulation, roofing, and flooring.
Historical Context of Asbestos Use
Asbestos was widely utilized throughout the 20th century, but its adverse health effects led to regulations and bans in many countries. Despite its decline in use, many buildings still contain asbestos materials.
Health Hazards of Asbestos Exposure
Respiratory Diseases
Inhaling asbestos fibers can cause severe respiratory diseases, including asbestosis, a chronic lung condition characterized by scarring of lung tissue.
Long-Term Health Effects
Prolonged exposure to asbestos increases the risk of lung cancer and mesothelioma, a rare and aggressive cancer affecting the lining of the lungs or abdomen.
The Purpose of Asbestos Re-Inspection Surveys
Legal Requirements
Regulations mandate regular asbestos inspections to ensure ongoing safety and compliance. Failing to adhere to these laws can result in hefty fines and legal consequences.
Maintaining Safety Standards
Regular re-inspections ensure that any asbestos-containing materials (ACMs) remain intact and safe. This prevents the release of harmful fibers into the environment.
Monitoring the Condition of ACMs
Over time, ACMs can deteriorate due to factors like age, environmental conditions, or physical damage. Re-inspections help monitor these materials and address any issues promptly.
Key Components of Asbestos Re-Inspection Surveys
Reviewing Previous Inspection Data
Inspectors begin by reviewing historical data to understand the condition and location of known ACMs. This helps in planning the current inspection.
Visual Inspection of ACMs
A thorough visual inspection identifies any visible signs of damage or deterioration in ACMs. Inspectors use tools to assess hard-to-reach areas.
Sampling and Testing Procedures
If new or suspicious materials are found, samples are taken and sent to a lab for analysis to confirm the presence of asbestos.
How Often Should Asbestos Re-Inspections Be Conducted?
Factors Influencing Frequency
The frequency of re-inspections depends on factors such as the type of ACMs, their condition, and the building's usage. High-risk areas may require more frequent checks.
Industry Recommendations
Authorities like OSHA and the EPA provide guidelines on inspection intervals. Typically, annual or biennial inspections are recommended, but this can vary based on specific circumstances.
Choosing a Qualified Asbestos Inspector
Required Certifications and Experience
A qualified asbestos inspector should have certifications from recognized bodies and extensive experience in conducting asbestos surveys.
Tips for Selecting a Reliable Professional
Look for inspectors with positive reviews, verifiable credentials, and a solid track record in asbestos management. It's also beneficial to seek recommendations from trusted sources.
The Re-Inspection Process Explained
Pre-Inspection Preparations
Inspectors prepare by reviewing previous reports, gathering necessary tools, and planning their inspection strategy. Building occupants are informed to ensure safety and minimal disruption.
Conducting the On-Site Inspection
On-site, inspectors visually assess all known ACMs and any newly discovered materials. They document their findings with photographs and detailed notes.
Post-Inspection Analysis and Reporting
After the inspection, a comprehensive report is generated, detailing the condition of ACMs, any changes since the last inspection, and recommended actions.
Interpreting the Results of an Asbestos Re-Inspection
Understanding Inspection Reports
Inspection reports provide a clear overview of the ACMs' condition and any potential risks. It's crucial to understand these findings to make informed decisions.
Recommended Actions Based on Findings
Based on the report, actions may include regular monitoring, repairs, or removal of damaged ACMs. These recommendations prioritize safety and compliance.
Challenges in Conducting Asbestos Re-Inspections
Accessing Hard-to-Reach Areas
Some ACMs are located in inaccessible areas, posing challenges for inspectors. Specialized equipment and techniques are often required to inspect these areas thoroughly.
Consistency in Inspection Methods
Ensuring consistency in inspection methods is crucial for reliable results. Standardized procedures help maintain the quality and accuracy of inspections.
Keeping Accurate Records
Maintaining detailed records of each inspection is essential for tracking the condition of ACMs over time. Accurate documentation aids in effective asbestos management.
Technological Advances in Asbestos Surveys
Modern Tools and Techniques
Advancements in technology, such as drones and infrared cameras, enhance the efficiency and accuracy of asbestos inspections, especially in hard-to-reach areas.
Benefits of Digital Reporting Systems
Digital reporting systems streamline the documentation process, making it easier to track findings, maintain records, and ensure regulatory compliance.
Case Studies: Effective Asbestos Management
Residential Case Studies
In residential settings, regular re-inspections have successfully prevented asbestos exposure by addressing deteriorating ACMs before they pose a risk.
Commercial and Industrial Success Stories
Commercial and industrial buildings have benefited from comprehensive asbestos management programs, resulting in improved safety and compliance.
Legal and Regulatory Framework
Key Asbestos Regulations
Laws like the Asbestos Hazard Emergency Response Act (AHERA) and the Control of Asbestos Regulations set strict guidelines for asbestos management and inspections.
Consequences of Non-Compliance
Non-compliance with asbestos regulations can result in significant fines, legal action, and increased health risks. Regular re-inspections help avoid these issues.
Benefits of Regular Asbestos Re-Inspections
Ensuring Health and Safety
Regular inspections ensure that ACMs remain safe, protecting building occupants from exposure to harmful asbestos fibers.
Regulatory Compliance
Staying compliant with asbestos regulations demonstrates a commitment to safety and avoids legal penalties.
Long-Term Cost Savings
Proactive asbestos management through regular re-inspections can prevent costly remediation by addressing issues early.
Common Misconceptions About Asbestos Re-Inspections
Myths vs. Reality
Many believe that asbestos is only a concern in older buildings or that it doesn't need to be monitored if undisturbed. Regular re-inspections debunk these myths, highlighting the importance of ongoing vigilance.
Educating the Public on Asbestos Safety
Public awareness campaigns can help dispel misconceptions and promote the importance of regular asbestos management.
Conclusion
Asbestos re-inspection surveys play a vital role in maintaining safety and compliance in buildings containing ACMs. By understanding their importance and following a structured approach, property owners and managers can ensure a safe environment for occupants and meet regulatory requirements.
FAQs
How often should asbestos re-inspection surveys be conducted? Re-inspections should typically be conducted annually or biennially, depending on the type and condition of ACMs and the building's usage.
What should I do if asbestos is found in my building? If asbestos is found, follow the recommendations in the inspection report, which may include monitoring, encapsulation, or removal by a licensed professional.
Can I perform an asbestos inspection myself? No, asbestos inspections should be conducted by certified professionals to ensure accuracy and safety.
What are the costs associated with asbestos re-inspection surveys? The cost varies based on the size of the property, the extent of ACMs, and the complexity of the inspection. It's best to obtain quotes from qualified inspectors.
How can technology improve asbestos re-inspection processes? Technology like drones and digital reporting systems can enhance the efficiency, accuracy, and documentation of asbestos inspections.
Contact Us.
Name: SQN
Address: 236A Bush Road, Rosedale, Auckland 0632, New Zealand
Phone: +64 800 333 287
0 notes