#End stage renal failure
Text
Donate to a chronicall ill viking!
My friend Tony has been battling end stage renal faliure for 6 years since he was 22.
He is running a half marathon for Kidney care UK.
He braids is own viking beard, own five different mead tankards (of which he is a expert).
He is one of the coolest men I have ever met and for certain the most generous.
He is a qualified dialysis surgeon and he runs even after hes had multiple heart attacks. There is literally no stopping this man.
Donate to his run today !
https://www.justgiving.com/fundraising/tony-kay5?utm_source=copyLink&utm_medium=fundraising&utm_content=tony-kay5&utm_campaign=pfp-share&utm_term=034dd7ee39954e368f338cd6bf321152
2 notes
·
View notes
Text
I started dialysis a few months ago, after ending up in hospital with a creatinine of 15.4.
And I’m sitting here, looking at this machine that leashes me each evening, and it’s a little miracle of science that I’m alive, that I can continue to be alive, in the comforts of my own home, with a dedicated team of professionals available 24/7 to support me: I have doctors, nurses, a dietitian, a social worker, a finance/insurance coordinator…and then the transplant team is even bigger. It’s wild. Truck drivers who come into the house and stack boxes for me, even.
And in the U.S. it’s covered immediately with Medicare, by federal law. Because I’d die without it.
So it can be done. This could be how we handle diabetes. Cancers. This could extend to others, who will die without intervention.
So I am so very lucky(?) to have a terminal chronic disease that is handled like this. Don’t get me wrong, having any chronic illness is exhausting, and there are nights when I feel burdened at the thought of hooking up, but then I remind myself how damn lucky I am (for both the technology and the supports) and then I am enraged that it isn’t common sense for a government to not let its population just die from treatable things…
#dialysis#chronicillness#kidney disease#end stage renal failure#medical insurance#stupid government#it is not that hard#just give everyone medical insurance
1 note
·
View note
Text
Sickle cell nephropathy, a complication not to be ignored, through a Moroccan case by Asmaa Biaz in Journal of Clinical Case Reports Medical Images and Health Sciences

SUMMARY
Nephropathy is a major complication of sickle cell disease. Indeed, the kidneys are particularly sensitive organs to this disease.
We report a case of a patient with a major sickle cell syndrome; she was hospitalized in the nephrology department of Mohammed V Military Training Hospital, forend-stage renal failure. The family investigation revealed a composite S/O-Arab heterozygosity responsible for the severity of the clinical disorder.
Key words: Sickle cell nephropathy - End stage renal failure - Sickle cell major syndrome S/O-Arab.
INTRODUCTION
Sickle cell nephropathy (SCN) is a major complication of sickle cell disease. It manifest’s in various forms, including glomerulopathy, proteinuria, hematuria, and Renal tubular disorders, and frequently results in end-stage renal disease(ESRD). Hemolysis and vascular occlusion are the main factors promoting the manifestations of this disease. Dialysis and renal transplantation are the last resort for patient with SCN [1].
Through the case of a patient with a major sickle cell syndrome S/O-Arab complicated by end-stage renal failure, we will explain the pathophysiological mechanisms of this complication and emphasize the importance of biological monitoring.
CASE REPORT
The patient was 24 years old and was admitted to the nephrology department of the Mohammed V Military Training Hospital for incidental renal failure in the context of an impure nephrotic syndrome revealing sickle cell nephropathy. In his history, we retained a
follow-up since the age of 5 years in another hospital structure for a hemoglobinosis S treated by iterative transfusions with notion of acute renal failure during sickle cell crises.
The biological result showed an anemia at 7.7 g/dL, corrected serum calcium at 82 mg/L, serum phosphorus at 64 mg/L, intact parathyroid hormone 1-84 at 543 pg/L, Alkaline Phosphatase at 201 U/L.
Hemoglobin electrophoresis was ordered to this patient, but due to repeated transfusions, her electrophoretic profile remains uninterpretable (Figure 1). Therefore, hemoglobin electrophoresis (HBE) was performed in the parents as part of the hemoglobin phenotypic study. The HBE of both parents is performed on Capillarys (Sebia®) at alkaline pH followed by electrophoresis at acidic pH on Hydrasys (Sebia®) which showed a heterozygous Hb O-Arab variant in the mother (Figure 2) and a heterozygous hemoglobinosis S (A/S) in the father (Figure 3).
Figure 1: Electrophoretic profile of the patient uninterpretable due to recent transfusion
Figure 2: Electrophoretic profile of the mother showing hemoglobinosis O-Arab in the heterozygous state
Figure 3: Electrophoretic profile of the father showing hemoglobinosis S in the heterozygous state
Referring to the phenotypic study of Hb performed in the parents, it is concluded that the patient has a composite heterozygosity S/O-Arab explaining the severity of the renal manifestations.
The evolution was marked by the absence of improvement of her renal function and the aggravation of the uremic syndrome motivating her setting in peritoneal dialysis. The patient was treated with erythropoietin ARANESP 30µg/ per 2 weeks with a blood transfusion of 2 packed red blood cells on average every two months.
The patient died at the age of 26 years before benefiting from either a hemoglobin genotyping study or a renal transplant.
DISCUSSION
Sickle cell disease is the most common hereditary hemoglobinopathy in the world. An estimated 300,000 children are born with this disease each year, three quarters of whom are born in sub-Saharan Africa [2]. It is characterized by extreme variability in terms of clinical manifestations, the most serious of which are renal manifestations.
The association S/O Arab is responsible for a major sickle cell syndrome, as in the case of our patient. Indeed, Hb O Arab stabilizes the intracellular polymerization of Hb S and leads to an irreversible sickle cell disease of red blood cells, thus expressing by a more severe clinical disorder. The clinical and biological manifestation of this association is similar to homozygous sickle cell disease and the association Hb S / Hb D Punjab. The onset is usually early, in infancy, and is marked by the classic triad of chronic hemolysis: anemia, jaundice and splenomegaly. Anemia is usually moderate outside of hemolytic attacks (Hb = 7 - 10 g/dL). The evolution is often marked by sickle cell complications. Osteoarticular complications are the most frequent, such as vaso-occlusive crises, septic arthritis and osteoporosis. Pneumonia, leg ulcers and vesicular lithiasis are also reported [3].
Sickle cell nephropathy is a major complication of sickle cell disease. The kidneys are particularly sensitive organs to the disease. Sickle cell disease substantially alters the structure and function of the kidneys and is the cause of several renal diseases and syndromes. Renal damage is more severe in SS homozygous patients than in other major sickle cell syndromes [4]. Approximately 5-18% of patients have SCN, thus increasing the risk of morbidity and mortality of the disease [5].
A number of studies have focused on this pathology, its evolution includes several stages; it starts with hyperfiltration, then the occurrence of microalbuminuria, then macroalbuminuria and finally the progression to renal failure. The prevalence of these complications increases with the age of the patients but can also be seen from a young age.
Two models have been proposed to explain the pathophysiology of SCN. Becker et al. showed that prostaglandin release following ischemic injury causes an increase in glomerular filtration rate (GFR). This increase leads to glomerular injury and eventually manifests as proteinuria and glomerulosclerosis [6]. Alternatively, Nath and Katusic [7] classified the manifestations of SCN into two different phenotypes: the hemolysis-endothelial dysfunction phenotype and the viscosity-vaso-occlusive phenotype. The hemolysis-endothelial dysfunction phenotype affects the renal cortex and leads to hyperfiltration and glomerulopathy; heme released due to intravascular hemolysis predisposes to proteinuria through its accumulation on the glomerular filtration barrier, which disrupts membrane selectivity by exerting cytotoxic effects on podocytes and endothelial cells [8]. On the other hand, the viscosity-vaso-occlusive phenotype is responsible for hematuria, papillary necrosis, and tubular acidosis [9].
Microalbuminuria, reflecting the early stages of renal damage, should be routinely sought in the follow-up assessment in this category of patients.
Decreased GFR, which suggests loss of kidney function, occurs with the progression of sickle cell disease and may be a sign of uncontrolled disease. Sickle cell patients have a higher risk of developing chronic kidney disease compared to the general population.
Specific treatment with an angiotensin-converting enzyme inhibitor or an angiotensin II
receptor antagonist should be considered in these patients in order to slow the progression of the renal disease. The prevention of microthrombosis and thus of renal damage requires the maintenance of a hemoglobin A level of more than 50% by regular blood transfusion as soon as sickle cell disease is diagnosed. The role of hydroxyurea in the prevention and/or treatment of renal function abnormalities in sickle cell disease remains to be studied [10].
CONCLUSION
Sickle cell nephropathy is a major complication of sickle cell disease. It must be systematically and early sought in all sickle cell patients to reduce the risk of morbidity and mortality of this disease.
The development of new biomarkers has become increasingly essential for the early detection of sickle cell disease in order to improve the survival of patients with sickle cell disease.
Declaration of interest:
The authors declare no conflict of interest.
For more information: https://jmedcasereportsimages.org/about-us/
For more submission : https://jmedcasereportsimages.org/
#Sickle cell nephropathy#End stage renal failure#Sickle cell major syndrome#S/O-Arab#Hemolysis#SCN#ESRD#hemoglobinosis#heterozygous#Asmaa Biaz#jcrmhs
0 notes
Note
I'm sorry you have to put down a pet ❤️❤️ I hope your last days with them are meaningful and you're able to find comfort in your memories and the knowledge that you're doing what has to be done for their own good
Thank you... i'm touched someone saw my tags and decided to send me an ask. it's really hard letting go of goop -- the time i've spent with her has been so special and i'm reminded of her every day, literally, just by logging into this site and looking at my activity page.
she truly is a special little cat and i'm glad that she will have a comfortable passing & burial plot in the family pet cemetery... almost five years ago, i left goop with my mom, who had papa pumpkin. i feel blessed that i got to care for her at the end. she has been very happy existing in the sunshine with her husband & sniffing fresh air through the window...
this is the only post i really want to make on the subject, and i won't be updating the original thread with this. there's no reason to sadden someone who isn't looking for the information of her passing. she will be going over the rainbow bridge this saturday, and pumpkin will be present during the appointment so she's not scared or lonely. she is a very beloved cat in many ways.
thank you again for the kind message, and goodbye & goodnight, mama goop

#before anyone asks me. she has late stage renal failure#so the informed decision has been made w/ the family vet to euthanize goop while she's not actively suffering#she has had a hard life and we want her to end on a high note
27 notes
·
View notes
Text
https://gofund.me/6732cec4
Behind every dope ass woman is one hell of a story💚🪄🌻
#black girl magic#national kidney foundation#chronic kidney failure#esrd#ckd#organ donation#kidney transplant#end stage renal disease#Pediatric Nurse#registered nurse#chronic illness#chronic pain#gofundme#fundrasier#john hopkins hospital#black nurses matter#black nurses rock
30 notes
·
View notes
Text
Frustrated by lack of relatable ESRD posts
I really really wish there were more posts about End Stage Renal Disease and everything related to it from other people who also live with it. Stuff about our experiences with kidney failure and dialysis and doctors and the diets they put us on and co-morbid illnesses and just everyday mundane stuff and what it's like to live with this condition. Cause most of the time when I'm looking up ESRD, I just find stuff about pets who have it, or posts from doctors or medical institutes or some study about some supposedly innovative thing in the nephrology world. I crave more relatable content from other humans who have ESRD, because it feels like there's hardly enough out there and I'm tired of it
#end stage renal disease#ESRD#chronic illness#disability#dialysis#life with kidney failure#kidneys#terminal illness
0 notes
Text
A kidney transplant is a surgical procedure that replaces a damaged or failed kidney with a healthy one.
#Kidney Transplant Surgery#kidney transplant Procedure#End-Stage Renal Disease#Chronic Kidney Failure#Success Rate of Kidney Transplants
0 notes
Text
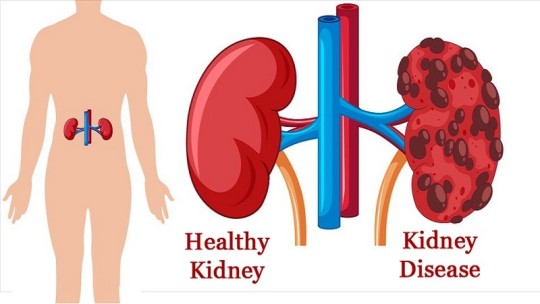
Kidney Diseases, Types and Diagnosis
Kidney Diseases, Types and Diagnosis
Kidney diseases can affect one or both kidneys, which are located on the left and right sides of the abdomen, in the middle of the back. They are bean-shaped and approximately the fist-sized. They are vital organs that remove toxins and extra water from the body.
What are kidney diseases?
A kidney disease does not occur overnight but develops over a period of time and in stages. Kidney disease…
View On WordPress
#ammonia#creatine#creatinine#end-stage renal disease#Kidney cysts#Kidney Disease#kidney failure#Polycystic kidney disease Polycystic kidney#Stones in the kidney#urea#uric acid#Waste products
0 notes
Text
The text for all of the screenshots below will be included after the screenshots at the end of this post.






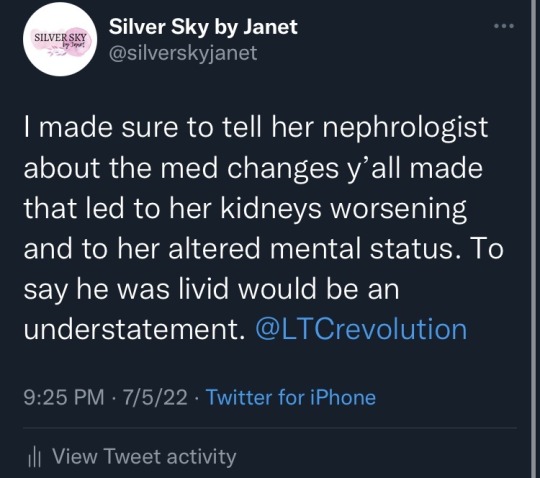

Between 3:27 and 3:37 PM CDT on July 4, 2022, while at my mom’s bedside in the emergency room of Huntsville Hospital, I made and updated a thread about my mom’s stay at Whitesburg Gardens, a Signature HealthCARE facility and how their actions led to my mom needing to be at the emergency room.
At 3:27:
I’m not saying the @LTCrevolution rehab my mom has been at for almost two weeks has made her kidneys, heart, and lungs significantly worse, but I’m not saying it hasn’t.
(Her labs that they twiddled their thumbs on ordering are totally saying it though.)
When we kept asking when they’d get her back on her medicine, they had to wait for a pharmacy to fill it. They still haven’t got her on one BP med and her bicarb medicine dose is too low vs what she’s supposed to be on.
When we kept asking when they’d check her creatinine, potassium, CBC, etc., they’d tell us “probably tomorrow” until the dietician ordered it—6 days into the stay.
When they got the CBC back, the next morning they sent her to get a blood transfusion. They didn’t monitor her closely after she got back.
When mom was lethargic on Saturday, a symptom that her CKD is worsening and/or that she may have respiratory acidosis, it took me calling the front desk TWICE to get them to call an ambulance.
An. Hour. After. I. Called. The. Last. Time.
When she couldn’t breathe and was coughing last night, the nurse refused to check on her. All. Night. Long.
She sent a message for mom to sit up through a CNA. Sitting up didn’t help. Two nebulizer treatments this morning didn’t help.
Now mom is at the ER (for the third time in a week and the second in three days) because she couldn’t oxygenate properly.
Her creatinine is up to 4.4 from 3.5 the day she went in.
Her CO2 went up by 4, into the high territory within the first week.
Her ProBNP is at 5055 pg/mL. Higher than at discharge.
Her potassium is high enough for her to probably need a potassium binder.
Her kidneys are now bad enough that she may need dialysis and I am so beyond pissed. One of her previous roommates made a comment last week that “it’s like they’re trying to kill us” and it kinda feels like they are.
At 3:37:
There have been incidents where they would stand in front of her and mock her for being unable to stand up. She was having trouble standing because CKD, heart, and lung problems cause muscle weakness and fatigue.
They responded at 8:32 AM CDT on July 5, 2022:
Silver Sky by Janet, we at Signature take all of your concerns very seriously, and we work hard to serve you, our residents, and their families. The care of our residents is our top priority. Please contact our CAREline at (888) 392-8886 -Sincerely, Signature HealthCARE
I responded at 9:42 PM CDT on July 5, 2022:
The name is Janet, but I’m not surprised you have a form response/bot for your replies @LTCrevolution since that was the same way that y’all apparently handled 1-star reviews on Google reviews for Whitesburg Gardens.
I made sure to tell her nephrologist about the med changes y’all made that led to her kidneys worsening and to her altered mental status. To say he was livid would be an understatement. @LTCrevolution
As of around 11:30 PM CDT on July 5, her creatinine is still at 4.4 mg/dL and her potassium has gone up to 5.4 mmol/L. Her systolic blood pressure and diastolic blood pressure keep taking turns on the systolic being high with the diastolic being normal and the systolic being normal with the diastolic being high. She’s having trouble with her vision and her hearing that she wasn’t having before. She cannot feel areas of her body she could feel before two days ago. She is confused. She struggles with words. She is scared. She is combative. I don’t know if this is a temporary mental status change. I don’t know if her kidneys will rebound. I don’t know what will happen next, but I know that all of these changes in her labs and her personality and her new status as an end-stage renal disease patient are a result of the actions taken at Whitesburg Gardens.
Update (July 6, 2022 at 5:51 pm CDT): She has developed pancytopenia as a result of the mismanagement of her CKD. This means her red blood cell, white blood cell, and platelet counts are too low, and her body can no longer produce the erythropoietin needed to protect her blood cells from being attacked. She will need a second surgery for her dialysis fistula sometime soon and she may need emergency access while that heals.
#kidney failure#end stage renal disease#elder abuse#nursing home#caregiver#signature healthcare#skilled nursing facility#family#disabled#disability#neuropathy#twitter#hypertension#heart failure#whitesburg gardens#huntsville#alabama#ckd
0 notes
Text
Gonna be a bummer for a bit! (CW fish illness)
Lucy started pineconing slightly a few hours ago and I feel really shitty about it because I don't know what I could have done for this to not have happened, but I'm sure there was something.
Her fin rot visibly and dramatically worsened over the weekend despite a second dose of the antibiotic treatment I was using, and I even had a second medication arrive today, but she was already lethargic and not really eating. She's just been floating in the front corner of the tank where I usually feed her with her belly somewhat swollen, not really moving except to take breaths every once in a while. And then as of the past couple of hours, her scales are popping up a bit, which, in combination with the belly swelling, pretty much guarantees end-stage renal failure resulting in fluid retention, which is a death sentence for a fish.
She's always been such a lively fish full of way more personality than you'd expect from, y'know, a little aquatic creature, and I have been so convinced that she'd live a good life of at least 4-5 years of chasing shrimp around, but here I am with her probably-dead barely a year and a half into her life. It just feels shitty, because this isn't, like, a random death - there's clearly a disease process happening - but I don't know how to fix it or what I should have done to prevent it, except maybe realize that it was happening earlier. I still don't know if the red splotches she developed months and months ago were signs of a latent bacterial infection or just her changing colors like bettas sometimes do.
I've done water changes. Her water parameters are pristine. There's a thriving and reproducing population of adult and baby shrimp in her tank, which are all notoriously bad at handling crappy water. There's no other fish in there to stress her. There are so many plants. I only feed the highest quality betta food I could find based on extensive reviews. I added shrimp for enrichment and snacks. The water is heated. Even a few hours ago, I was convinced that I could get her through this. What happened?
I guess now I just mostly feel bad because barring a miracle, I'm probably going to find her dead tomorrow and it's going to be fucking horrible. Her poor fins look so awful right now. At least she's in a comfortable and familiar place. She's moving around a little more, now, and the pineconing is less obvious in the new light...I'm going to at least hope that I'm wrong about this.
Swim in peace, Lucy, if you don't make it the night.

26 notes
·
View notes
Text
love waking up to accusations of never having an addict in my family bec I said the rehabilitation Feysand used was an abuse of power. literally my entire childhood got destroyed bec of meth and alcohol abuse. my mom drank while she was pregnant with me, she got terminal end stage renal failure at 33 and died at 39 when I was 21 (maybe 22). I went to rehab with my mom at 8 years old after I went across town at midnight to use the phone at a gas station to call my mentor for help bec my mom had been awake for days and had a psychotic break and was paranoid about her kids being taken away from her. my step-dad beat my terminally ill mother while she was hooked up to her dialysis machine while he was high on meth. I watched him break her nose. I went with my mom to the hospital where she was crying and afraid I'd leave her bec of him. my step-dad locked us all in the house and ripped the phones off the walls to trap us in with him while he was violent and hurting us. I went to my neighbors house in the middle of the night to call the cops and repeatedly got in trouble for protecting my mom and my little brother to the point I'm still afraid of asking authority figures for help. I have a very intimate, and long, history with addicts that aren't the """"socially acceptable"""" bougie addicts
sorry I'm just 😤 this is the ONE accusation that makes me instantly angry and pissed off. if there is ONE thing I can clock from a mile away it is an ADDICT and quite frankly Nesta is not a fucking addict bec she wasn't written like one or actually effectively treated like one JESUS Christ above
#a court of thorns and roses#acotar#nesta archeron#anti rhysand#sjm critical#sorry yall im just AAAAAAAHHH#anti feysand#maybe yall should be looking closer at M*r and her drinking and self harm habits#Nesta is not an alcoholic send tweet
37 notes
·
View notes
Text
So, I'm sleepless at 1am and I'm tired and I'm upset so I'm going to get out the shit that has been going on for me the past month and a half, because it keeps leaking out in tags and I guess maybe I should not do that. This is going to be long and it's a huge bummer. I just don't feel like I can come out and talk about it directly to anyone because it is indeed a huge bummer and I just. can't deal with like. the feeling of unloading this on someone and then what.
but throwing it into the tumblr void and hiding it behind cuts feels less like I'm throwing a bunch of gross stuff at someone's feet so like, yeah.
Content warnings for uh, facing the mortality of aging parents, the American healthcare system being a fucking nightmare, mentions of strokes, infections, and other huge medical problems, and basically stuff being awful.
I have lived with my mom as her caregiver for the past three years, since losing my job during covid. She is six years in remission from breast cancer, diabetic, and in end stage renal failure, meaning her kidneys don't work and she needs hemodialysis 3 days a week. I came in mostly to do things like shopping, the majority of cooking and cleaning, be present in case of falls, things like that. It's worked out, mostly. It sucks that she had to move to AZ to live near her brother simply due to the fact that her cozy little house in MT that she got remodeled to her needs has no dialysis centers within an hour's drive and the closest ones had no open seats anyway, not even for a summer stay, because of the nationwide nursing and technician shortage in healthcare. So she lives in AZ and goes to dialysis 10 minutes away. It works out, sorta.
But.
Since August 1st:
she had a stroke, which affected the language centers of her brain and made speech, writing, and complex communication difficult
she spent a week in neuro ICU for follow up; this was at a hospital 20 miles away in Phoenix. yes I drove there every day to see her.
she was transferred to a rehabilitation center after that week, where she had several good days but then started to experience severe lower back pain.
the back pain got so severe that she was crying and even screaming when being helped into/out of bed, or having the head of the bed elevated so she could eat.
myself and her other present family were very upset about this, because she was in pain! and also it was preventing progress in her PT/OT after the stroke! we wanted them to do something and find out what was going on!
an xray was done. "no significant findings."
we asked for a CT scan or MRI if an xray found nothing.
it didn't happen. maybe insurance said no, maybe assumptions were made that it wasn't necessary.
but mom spent the rest of her 15 days at that rehab facility on tylenol and then oxycodone.
she was then discharged, and yet in no state to come home.
we found a short-term care facility for her that she'd actually stayed at after her initial ER stay that discovered her renal failure. we thought that she'd do okay there.
she didn't. she declined. she was still in severe pain. MWF for her dialysis, she was basically just, done. and they had scheduled her dialysis at 6am. so. the day was just over, no ability for therapy.
they still just gave her oxycodone so even on good days she was sleeping a lot and very out of it.
we asked to speak to the physician and her case worker. we were not able to.
we asked for her to get further testing instead of just this pattern of throwing narcotics at her and watching her decline. it didn't happen.
at the end of her second week there, she was becoming less responsive and more inclined to just sleep.
she wasn't eating. I tried so hard to encourage her to eat, I even fed her. she still would eat a few bites and then be uninterested in more.
one day she only ate a cup of yogurt.
then she was so badly out of it and barely responsive that I demanded that they do something. so they gave her narcan. because maybe she was too lost in the oxycodone sauce. didn't help, they gave her more. didn't help. they called EMTs.
she ended up in the ER, where they did a CT, MRI, and bloodwork.
(this was a week ago)
turns out she has an infection in her spine. which is osteomyelitis, an infection in the bone and bone marrow that just constantly hurts. oh also numerous pressure sores, including a bad one on her heel, and a bad one on her lower back. either could have introduced the infection into her spine.
that infection has spread to her blood. yeah she's got sepsis.
she also has had at least one additional stroke and her speech has degraded even further.
she spent several days in the ICU and it was very touch and go.
it is still very touch-and-go but she's now in progressive care (pcu) which is a downgrade from ICU in terms of how serious.
but yeah. sepsis is very dangerous for young and relatively healthy people. she is 74. her diabetes means her healing is very slow. her renal failure means that her system can't handle a heavy load of antibiotics so they have to be given more spaced out and in lower doses.
it. sucks.
I still go to see her every day and talk to her even if she's not responding. I sing songs she knows. I put on videos of the church services in her hometown for her to listen to. - it. sucks. so. much.
oh yeah also her place here in AZ is in a retirement park and I can only be here because she resides here. so if something happens even in terms of her moving her permanent residence elsewhere I can't stay here.
I have no income I basically just lived here with her and she covered my expenses as my pay for being her caregiver. so like. looks at the potential need to get independent housing, looks at bank account with $30 in it, laughs darkly and decides I can't think about that.
besides I need to think about how this could be the last time I have left with my mom.
it. sucks.
14 notes
·
View notes
Text
Here's something that I doubt everyone knows about the disability crisis in the United States. For a civilian to get disability payments, they have to be "totally" disabled; in other words, you have to prove you cannot get any job in any industry based on Department of Labor statistics in your state, not *just* that you have a debilitating condition. For a veteran to get disability payments, they have to prove a percentage of how disabled they are, and getting 100% disability as a veteran is no easy task wording is critical in the documentation if anyone at any point in your medical history intentionally or not downplays your disability you will get percentage points taken off how much pay you get as a disabled veteran. This is particularly difficult for people with any pride or dignity left because, in both civilian and veteran cases, you must explain just how awful it is in explicit terms and quantifiable, dehumanized ways to sate the court's interest, or you will not get "total" disability. Furthermore, until you are considered "permanently" disabled, you must repeat this process every 3-5 years. Yet, again no one anywhere can talk about you improving or you're out (for civilians), or your disability percentage amount is reduced (for veterans.) Also, if you manage to prove a "permanent" disability, you still get checked every seven years to make sure it's still "permanent." Finally, to get your student loans discharged as a civilian, you must prove your disabled status is both "total and permanent," guess what if one of those changes? Those loans come right back. Also, your loans go into forbearance if you're" totally disabled" and not considered "permanent" or "short-term" (more than 2 weeks, up to a year). Yes, that is the one that accrues interest. Not deferment. For short-term disability, you can defer, but if you're long-term, non-permanent, you forbear. Most people on long-term disability are medically permanently disabled but not in the eyes of the law because of their age, even if it is a chronic or progressive disease. This is why people die waiting for total disability, let alone permanent. My disability attorney said straight to my face 10 years ago, "You should get disability because you have a chronic disabling condition in two systems, but it's going to be a fight because you are so young." I was 28, by the way. She said if I had "just Lupus" or "just medication-resistant dysthymia and generalized anxiety," I wouldn't have stood a chance. My cousin "just" had Lupus and was in end-stage renal failure, it took her 3 years to get disability, and by then, she had a kidney transplant. She was in her 20s and on her parents' insurance. I have a friend whose veteran husband couldn't get 100% VA disability because some doctor at some VA clinic years ago had written down "mild back pain" when describing the pain he felt from degenerative disc disease and 2 herniated discs. It took years to get that one note out of his file. No matter what any other doctor said. So when I say you can't comprehend the disability crisis in the United States, I'm talking about this. Thanks for coming to my TED Talk.
18 notes
·
View notes
Text
Announcing it here because I don’t even know where else I’d put this, and it’s screaming in my head so loud it’s been my singular thought for who knows how many hours now
A little bit ago I announced my cat was sick and how that had delayed a lot of the hype and teasers I’d meant to put around re:mhny2′s release. Unfortunately, we receive confirmation that my cat is in stage 4 renal failure. There is no recovery from renal failure. There’s no reason for it. Sometimes it just happens. I did everything I could. I did 20 hour days with her. Feeding her via plunger syringe. Hydrating her via IV. Every single day. And she was getting better. And her doctor was shocked she was even still moving, and told us that it didn’t need to be now, but when she started showing certain signs, it would be time. That was 3 weeks ago, and she was still getting better
This week, she is declining steadily. My cat will not be recovering. My cat is dying. At the end of the month, or sooner, she will not be here anymore. My cat is dying and will not be here anymore, and I won’t get to see her anymore, and I won’t ever hear her calling for me in the other room in a noise that can only best be described as an inquisitive, two syllable “Mom?”
Anyways if anyone would like to share what sentimental things they did with their pets after they had passed, please feel free to share. I’m already drowning in my grief and trying to deal with it by focusing on logistics.
11 notes
·
View notes
Text

Shoutout to my GOD-mama for my cup! It’s most definitely a coffee ☕️ kind of day.
https://gofund.me/6732cec4
#ThisNurseNeedsAKidney#ClickTheLink#DonateLife#ShareYourSpare#PediatricNurse#black girl magic#black girls rock#black nurses matter#black nurses rock#esrd#ckd#chronic kidney disease#kidney failure#end stage renal disease#dialysis#john hopkins hospital#atypical hus#Atypical Hemolytic Uremic Syndrome#chronic pain#chronic illness#spoonie#gofundme#healing#happy juneteenth#juneteenth#support black people#support black women#registered nurse#organ donor#organ donation
12 notes
·
View notes
Text
Something I see online that's frustrating to me is you'll get people telling the vegan activists who promote veganism as a universal ideal that there are disabled people who can't have a vegan diet, but then a lot of the people who point this out don't seem to know what conditions actually cause that. And then you end up having arguments about that so I want to actually point out a few examples
I think the number one example where there's no way to safely, healthfully avoid having to consume animal products is haemodialysis for kidney failure. People on dialysis need more protein than other people because they lose protein and blood cells during the dialysis process, and they are required to have a low potassium diet because their kidneys can't filter potassium. This means legumes and soy aren't viable alternatives. [x] "Renal dietitians encourage most people on haemodialysis to eat high-quality protein because it produces less waste for removal during dialysis. High-quality protein comes from meat, poultry, fish, and eggs." [x] If you can't meet your protein needs with these foods for whatever reason, you'll be prescribed whey protein powder, which is made from dairy. [x]
Ketogenic diets are also high in animal proteins. They're innately low carb and high in fat, which means legumes and other meat alternatives aren't a great fit. "The ketogenic diet can boost insulin sensitivity and cause fat loss, leading to significant health benefits for people with type 2 diabetes or prediabetes." [x] PCOS, a common condition effecting about 10% of people who menstruate, is also often treated with a low carb, high protein diet because it involves insulin resistance. [x]
Ketogenic diets may also be recommended to treat seizures in epilepsy. [x] It is most frequently used for focal seizures in children, infantile spasms, Rett syndrome, tuberous sclerosis complex, Dravet syndrome, Doose syndrome, and GLUT-1 deficiency. In these conditions, ketogenic diets can reduce or even eliminate seizures.
People with food allergies can find it difficult to afford safe and healthy food in general. [x] The inability to rely on cheap, plant-based proteins like canned beans or dried lentils can be a general hardship, especially when disabilities themselves can limit job opportunities or the capacity to work.
Intestinal disorders are another factor that can make vegan diets difficult. Foods high in insoluble fibre, like beans and other legumes, as well as nuts and seeds, can cause Crohn's flare ups in some people. [x] Seeds, nuts, and legumes can also be trigger foods for people with ulcerative colitis. [x] IBD flare ups are not like a run-of-the-mill case of intestinal discomfort. They can land people in the hospital and require major surgery. [x]
For allergies, the main factor that can make a vegan diet difficult isn't allergy to specific vegetables, but to specific plant proteins. Someone who is allergic to soy, peanuts, or other legumes will have more limited options for meeting their daily protein requirements on a vegan diet. People with allergies to a broad spectrum of legumes may not have any reasonable substitution options. Substitutions can also increase the price point and make a vegan diet too expensive for people in poverty who also have allergies. Poor people with food allergies may find it difficult in general to afford a safe and healthy diet. [x]
For some people, including some disabled people, a vegan diet may in fact be ideal. Vegan diets can certainly be part of a healthy diet when trying to reduce bad cholesterol [x], treat high blood pressure [x], or treat earlier stages of kidney disease. [x] And while insulin resistance may be best treated with a ketogenic diet in some people, others do seem to benefit from a plant-based diet instead. [x] A person's diabetes specialist and trained dietitians can help them figure out which is best for them, potentially based on other factors like whether or not they have high blood pressure or bad cholesterol, or whether their diabetes risks are linked to PCOS or other known metabolic conditions.
Achieving sustainable food production and equal access to a safe, nutritious, well-balanced diet is fundamental to us all. But there's simply no one-size-fits-all ideal human diet, and that's something everyone needs to take into account.
30 notes
·
View notes