#maladaptive schemas
Text
Healing Attachment: The Power of Attachment Repair & The Attachment Project
I have found two resources for people seeking information on attachment: Attachment Repair & The Attachment Project.
Attachment Repair offers guided practices, such as hypnosis/meditation, to calm anxieties & foster healthier attachment patterns. (One thing I'm interested in is their Healing Anxious-Preoccupied Attachment self-paced course.) Their weekly book club provides a collaborative environment for exploring attachment-related literature & engaging in discussions with peers.
The Attachment Project provides information on attachment & offers quizzes to determine attachment styles & maladaptive schemas. They also have a YouTube channel. The information offered can help individuals understand the root causes of attachment issues & work towards healing & transforming maladaptive patterns.
While Attachment Repair & The Attachment Project are resources with information to help individuals understand & work towards healing their attachment issues, it's crucial to recognize that these platforms are not a replacement for therapy. Seeking professional help from a qualified therapist is essential for addressing & resolving complex attachment issues.
#attachment#attachment theory#schemas#maladaptive schemas#hypnosis#meditation#Attachment Repair#The Attachment Project
0 notes
Text
going to my first therapy session in ages: see inside me there are two wolves. sam winchester and dean winchester. anyways -
#like the angel and the devil on your shoulder except it's. remnants from a rancid childhood#anyways meta analysing sam and dean thru the 18 early maladaptive schemas when#j.txt
8 notes
·
View notes
Text
Overcoming Early Maladaptive Schemas Through Stoicism
xr:d:DAGCFTzNeaw:2,j:2585490690809663052,t:24041105
Attachment theory has recently gained significant attention, shedding light on how our early relationships shape our interactions and emotional bonds. Similarly, Early Maladaptive schemes (EMS), a concept that may be unfamiliar to many, offer profound insights into our psychological makeup. EMS are not just abstract ideas; they are deeply…
View On WordPress
#Acceptance#Blogging#Cognitive Behavioral Therapy#Coping Mechanisms#Coping Strategies#Early Maladaptive Schemas#Emotional Control#Emotional Well-being#EMS#gratitude#Jeffrey Young#mental health#Mindfulness#Personal Growth#philosophy#Psychology#Relationships#Resilience#Schema Therapy#self-awareness#Self-Improvement#Stoic Practices#Stoicism#Therapy#virtue
1 note
·
View note
Text
Thwip Thursday
Oh yeah baby. It's happening. Enjoy an excerpt of my final paper for CBT where I treat our fun CBT dear professor Lasko. This is the funniest thing I've ever posted on my blog because yes, I am writing about redacted for a graduate school final paper for a grade. I will put it in the tag because I think it's funny.
(No read more necessary! Can you believe it! Just a warning though I did fill out his backstory and he did get hit with the transgenderification beam. sorry not sorry)
This case conceptualization addresses the hypothetical course of treatment for Lasko Moore, a character in a modern-fantasy audio narrative. Lasko Moore presented to treatment as a 30-year-old pansexual and transgender Indo-Caribbean man working as an administrator and adjunct professor at Dahlia Academy for Magical Novices for persistent anxiety symptoms. Upon intake, Lasko reported experiencing near constant racing thoughts that he was unable to “turn off”, panic attacks, and increased anxiety about social interactions at his work. He described spending a significant amount of mental energy preparing for and reviewing social interactions with colleagues such that he often avoids his colleagues in an effort to minimize his anxiety. Lasko reported that the anticipation around coworker interactions (meetings, socials, etc.) becomes quickly overwhelming as he becomes preoccupied with what he will say and do in an effort to try and minimize his tendency to become hyperverbal and overshare information as well as stuttering. He described this process as starting with embarrassment over previous interactions which leads to critical thoughts like “I shouldn’t be so anxious” which leads to rehearsal of potential outcomes of interactions. However, in the moment of social interactions he becomes so anxious as there “aren’t any objectives [or] any specific roles” to the conversations that he “word vomits” and becomes tangential and overshares until he runs out of breath and stops himself from talking due to his own critical thoughts and begins to isolate himself.
Lasko was initially diagnosed with Panic Disorder (F41.0) and Generalized Anxiety Disorder (F41.1) to capture his persistent anxious state with occasional intense bouts of extreme anxiety and panic. An initial long-term goal was collaboratively set as improving his coping strategies and tolerance of anxious affect to better network and create relationships. As this was Lasko’s first time utilizing mental health services, treatment began with inhibitory learning in combination with Acceptance and Commitment Therapy in order to facilitate willingness to experience interoceptive cues and extinguish avoidance due to fear of negative consequences. This was able to reduce his panic attacks as he felt more able to tolerate overwhelming anxious affect. Despite his clear engagement with treatment through attendance, homework, and skills practice, Lasko continued to struggle with critical thoughts and avoidance of coworkers which he identified as a major barrier to his continued professional development and potential non-academic relationships. Through collaborative exploration, a persistent early maladaptive schema relating to his critical thoughts emerged and treatment shifted to a goal of starting dialogue between schema modes to facilitate the use of coping strategies to build interpersonal effectiveness.
#speed run#redacted#redactedasmr#redacted asmr#redacted audio#redactedverse#redacted lasko#POSTING THIS IN THE MAIN TAG IS SOOO FUCKING FUNNY TO ME OK
20 notes
·
View notes
Text
Btw this is how somebody might think compassionately without affective empathy.
Person A is upset because their didn’t get a job they wanted
When that happened to me I was also upset (*some might not remember exactly what they felt like but often people cognitively know they were upset*)
I do not feel what this person feels. I do not feel emotionally impacted by them though they are crying. However, I know from past experience that this is something that is upsetting. Even though I feel nothing for this person, I have a personal value that suffering should be eliminated, so I am going to do something to try to inact that value.
This process can be complicated by stuff. Ex. poor emotional regulation, maladaptive world schemas, etc. But with treatment (and sometimes without) this is possible.
Think before you say something about people with low empathy. Empathy is not the only lens through which to see the world.
18 notes
·
View notes
Text
Nurturing Healing: The Profound Impact of Therapy on Managing Borderline Personality Disorder (BPD)
Hey there, fellow BPD warriors and allies! Today, let’s embark on a profound exploration of the vital role that therapy plays in our journey of managing Borderline Personality Disorder (BPD).
Living with BPD often feels like navigating a tempestuous sea, where emotions crash against the shores of our minds with relentless force. But amidst the storm, therapy stands as a steadfast lighthouse, guiding us towards calmer waters and brighter horizons.
At the heart of therapy lies a transformative process of self-discovery and healing.
It’s a sanctuary where we can peel back the layers of our innermost selves, revealing the raw, unfiltered truth beneath the surface.
Through introspective dialogue and empathetic guidance, we unravel the tangled threads of our past traumas, illuminating the pathways to understanding and acceptance.
As we traverse the terrain of therapy, we encounter a myriad of therapeutic modalities, each offering unique insights and tools for growth. From the structured approach of Dialectical Behaviour Therapy (DBT) to the introspective lens of Schema Therapy, we cultivate a rich tapestry of coping mechanisms and self-regulation skills. Through experiential exercises, role-playing, and mindfulness practices, we learn to navigate the ebb and flow of our emotions with grace and resilience.
Yet, therapy is far more than a mere journey into the depths of our psyche.
It’s a dynamic exchange between therapist and client, grounded in trust, compassion, and mutual respect.
Within this sacred space, we find solace in the knowledge that our struggles are met with unwavering empathy, free from the weight of judgment or stigma.
As we traverse the terrain of therapy, we encounter a myriad of therapeutic modalities, each offering unique insights and tools for growth. Among the most commonly used therapies for managing BPD are:
Dialectical Behaviour Therapy (DBT): DBT is a structured form of therapy that focuses on building skills in four key areas: mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. It helps us learn to identify and change harmful behaviours, cope with intense emotions, and improve our relationships.
Schema Therapy: Schema Therapy delves into the deeply rooted patterns and beliefs that underlie our emotional struggles. By identifying and challenging maladaptive schemas—core themes about ourselves and the world—we can cultivate healthier ways of thinking, feeling, and relating to others.
Cognitive Behavioural Therapy (CBT): CBT targets the negative thought patterns and behaviours that contribute to our emotional distress. Through cognitive restructuring and behaviour modification techniques, we learn to challenge distorted thinking, develop coping strategies, and create positive change in our lives.
Psychodynamic Therapy: Psychodynamic therapy explores the unconscious conflicts and dynamics that shape our emotions and behaviours. By examining early life experiences and relationship patterns, we gain insight into the root causes of our struggles and work towards resolving unresolved issues.
Mindfulness-Based Therapies: Mindfulness-based approaches, such as Acceptance and Commitment Therapy (ACT) and Mindfulness-Based Cognitive Therapy (MBCT), emphasise present-moment awareness and nonjudgmental acceptance of our experiences. These practices help us cultivate inner peace, resilience, and self-compassion.
Yet, let’s not sugarcoat the reality:
therapy can be arduous, confronting, and downright messy at times.
We may stumble upon buried memories, confront the shadows of our past, or grapple with the weight of unspoken truths. In these moments of vulnerability, we find the courage to confront our inner demons, knowing that true healing lies on the other side of our fears.
Moreover, the journey of therapy isn’t confined to the walls of a therapist’s office; it extends into the fabric of our daily lives. Through homework assignments, journaling prompts, and real-world applications, we integrate the lessons of therapy into our everyday experiences, transforming theory into practice and insight into action.
In essence, therapy offers us a compass for navigating the complexities of BPD—a guiding light amidst the darkness, a beacon of hope in times of uncertainty. So, to all my fellow travellers on this winding road of healing, let’s honour the transformative power of therapy in our lives and embrace the journey with open hearts and unwavering resolve.
#therapy#bpd support#bpd#bpd safe#bpd thoughts#psychology#bettersoonx#community support#emotional wellness#mental health#self care#actually bpd#bpd vent#actually borderline#fp bpd#bpd journey
3 notes
·
View notes
Text
Developmental Psych and TUA
A conversation shared with a colleague, because I am coming to realize that most TUA fans pick one sibling and try to act like "this sibling has it the worst and here's why," and I just don't think that mindset works. Let me try to use some developmental psych terms I've had to learn in my line of work (I'm in higher ed and I work with a lot of special needs students), which derive both from Object Relations Theory and Cognitive Behavioral Therapy:
-------------
Me
Today at 6:51
i found someone who agrees with me on this and replying to them helped me realize where Luther's consent issues, when he is being coercive with Viktor or Klaus or Five or someone else, come from. he has to believe it's okay to physically and emotionally bully someone into doing something that triggers them, because REGINALD DID THAT TO HIM, so if he doesn't believe it's necessary "for the cause/family," then he has to face the fact that Reginald abused him (changing his body, sending him to the moon but honestly especially the body thing) for no good reason. and that's scary for him. too scary, right now. hopefully not always, but right now.
in fact ALL the other siblings (to varying degrees) have issues with consent, and also, with being too fearful of changing their own childhood "roles" and "identities" as adults. so as klaus grows and changes through the 3 existing seasons, they have to disregard it or they have to face that they could change for the better too, and it's hard scary work.
Friend
Today at 6:58 PM
Yeah, Luther is also the last of them to finally start to come to terms with the fact he was abused; he hung onto Reginald's lies the longest, and honestly idk if he would have ever begun to acknowledge his abuse if Reginald hadn't killed himself. He probably would still be under Reginald's thumb. I think that's really sad
Me
Today at 7:03 PM
It is!
it's also sad that Reginald hurt his kids so much that they continue to hurt each other and not even understand what they're doing wrong, years after he died, and even when he's back and demonstrably their mortal enemy.
Friend
Today at 7:06 PM
Yeah. It doesn't help that it seems they were extremely isolated from the rest of the world unless they could sneak out. That, I imagine, makes Reginald and their issues even harder to grapple with.
They really don't have a healthy model anywhere. To most of them, I feel like they think their behavior is relatively "normal".
Me
Today at 7:12 PM
yep, that's their world schema
they think it's reality when in fact it's a highly insular, dysfunctional premise for identity and relationships
the damage done in childhood trauma can be somewhat reversed, but your "core beliefs," the way you think the world works and people in it are meant to interact, is formed in the first 5-10 years. Your first caretaker is your model for ALL subsequent relationships. if love is transactional and conditional with them, it is with everyone else, unless you put in INTENSIVE hard work unlearning and healing.
that is what they're dealing with
that's why klaus uses substances to numb, and shrinks away from conflict. that's why diego represses and protects. that's why allison controls. that's why viktor molotovs and keeps secrets. that's why five obsessively plans and calculates. why luther has a rigid sanctimonious world-view and tries to take charge. why ben scolds and emotionally manipulates. every single one of them copes maladaptively based on that premise
#Klaus Hargreeves#Luther Hargreeves#Allison Hargreeves#Ben Hargreeves#Viktor Hargreeves#Five Hargreeves#Diego Hargreeves#TUA#meta#The Umbrella Academy
25 notes
·
View notes
Text
today's strange moods sponsored by am-i-going-to-be-sick-or-just-exhausted uncertainty, taking online maladaptive schema quizzes and diving into the bts discography for the first time bc why not
#top score on the quiz is unsurprisingly abandonment#songs are catchy and charming#i get the appeal#i would really appreciate not getting sick now thank you
2 notes
·
View notes
Text
If you ask for signs of personality disorder (PDO), you're probably going to hear things like "difficult person," "entitlement," and "dependency." While these are not wrong per se, they're better categorized as symptoms of particular PDOs. These can also be fleeting experiences, such as during an episodic illness or at points in life, like adolescence.
Believe it or not, you don't necessarily have to be well-versed in the specific personality pathologies to recognize whether a patient, employee, friend, or loved one may be suffering from a personality disorder.
While someone's maladaptive interactional habits/traits, like those mentioned above, may lead you to wonder about a possible personality disorder, there are other things to consider as well. By the same token, even if one does not have an astute eye for diagnostic criteria, noticing more general things can indicate a personality disorder is possibly at play.
First, let's examine what a personality is and the basic meaning and foundation of personality disorder.
What is a Personality?
Personality is essentially our relational style; how we view and interact with ourselves, the world, and others. This is dictated by a combination of temperament and character. The former is a collection of genetically-inherited components known as traits, and the latter consists of learned material we call habits (Shannon, 2013).
Some researchers use the concept of a core schema to explain how people learn to see and interact with the world. (e.g., Martin & Young, 2003; Shannon, 2019). For example, some people grow up in an environment where independent thinking isn't encouraged and is perhaps even punished. It isn't surprising that some of them develop a core belief that they are incapable of thinking for themselves and must rely on others to make their decisions. This typifies the dependent personality.
Components of a Disordered Personality
It has generally been agreed upon that disordered personalities have a long-standing baseline presentation of significant impairment across several domains. These are the person's thoughts, moods, matters of impulse control, and interpersonal relationships (e.g., Yudofsky, 2005; Shannon, 2019; APA, 2022.) This is exemplified in borderline personality disorder (BPD).
People with borderline personality traits are hypersensitive to rejection/abandonment. At the slightest perception (thought) of rejection, such as someone not calling them on time, they flare with anger (mood). Given an inherent propensity for amygdalar hypersensitivity, meaning they defensively and angrily react in rapid form upon threat perception (lack of impulse control), the person with BPD lets their acquaintance have a piece of their mind.
The acquaintance, naturally, is stunned/feels attacked and avoids the person or returns fire out of defense, and thus a tumultuous interpersonal cycle has begun. This happens across relationships and settings to one degree or another, creating a self-fulfilling prophecy regarding rejection/abandonment, maintaining the very thing they fear most.
What Is Personality?
Find a therapist near me
The Three Key Signs
Perhaps more importantly, and even more telling than specific symptoms associated with particular disorders, are matters of duration, rigidity, and globalism of the vexing behaviors.
A chief sign or two of a particular PDO in one setting, with only particular people, or at only one point in time isn't enough to warrant a PDO diagnosis. It's crucial to remember the edict of Emil Kraepelin, father of modern psychiatric diagnostic conceptualization, that “A single symptom, however characteristic it may be, never justifies a diagnosis by itself…” (Spitzer et al., 2002, page 487).
For example, a patient observed to be moody and triangulate staff while hospitalized isn't enough to warrant a BPD diagnosis, and an inmate exhibiting questionable morals and refusing to take responsibility doesn't clinch an antisocial personality profile.
A PDO diagnosis must include the following regarding the behaviors:
Personality Essential Reads
Source: adjaeargoptura/Pixabay
1. Baseline behavior: Assessing the history of the package of troubling behaviors is essential. According to PDO expert Joseph Shannon, Ph.D. (2013), personality is solidified no later than age 13. To be considered a disorder of personality, the pervasive traits/characteristics must be consistent and long-standing, as in years.
While someone with a PDO may experience an exacerbation of symptoms during stressful periods, it is crucial to make sure that someone's problematic interactional style isn't isolated to stressful periods, such as during a depressive spell or in the case of an adjustment disorder with mixed disturbance of mood and conduct.
Further, teens commonly exhibit narcissism and histrionic characteristics. If there was no evidence of these before adolescence, there's probably no need to become alarmed that they're evolving into the next Miranda Priestly (Meryl Streep's character in The Devil Wears Prada).
2. Inflexibility: People with a personal disorder may recognize that their life is fraught with complicated interpersonal matters, but they nonetheless adhere to a maladaptive modus operandi and don't learn from their mistakes. They project blame and complain that the problem is everyone else. This is perhaps best illustrated with pathological narcissism, which is often compensation for fragility associated with shame (e.g., McWilliam, 2013; Burgos, 2015.)
If there's any possibility of appearing damaged, it topples the sense of superiority that they rely on so much. Hence, they are not likely to seek psychotherapy, as that's for people with flaws. That said, McWilliams (2013) pointed out that some may indeed initiate therapy because they see it as an opportunity to perfect themselves.
3. Global complications: Just because someone presents challenging behaviors to certain individuals doesn't mean they are personality-disordered. There needs to be pervasive relating complications across relationships. For example, many teens and young adults I evaluate are oppositional/defiant and reactively irritable in the home environment.
At first glance, this could be seen as a budding passive-aggressive personality. However, upon talking to school personnel, coaches, and providers, they present no such challenges and report feeling good about relationships outside the home. A personality-disordered individual would exhibit passive-aggressive behaviors wherever they went. There would be consistent peer drama, school infractions, and a sense that others in general are against them.
Cheat Sheet Summary
A personality disorder is only when thoughts, moods, and impulse problems are pervasive, long-standing/inflexible, and wreak havoc on the person’s ability to have satisfying relationships across settings.
7 notes
·
View notes
Text
OTIONAL REASONING: Letting your feelings guide your interpretation of reality. “I feel depressed; therefore, my marriage is not working out.”
CATASTROPHIZING: Focusing on the worst possible outcome and seeing it as most likely. “It would be terrible if I failed.”
OVERGENERALIZING: Perceiving a global pattern of negatives on the basis of a single incident. “This generally happens to me. I seem to fail at a lot of things.”
DICHOTOMOUS THINKING (also known variously as “black-and-white thinking,” “all-or-nothing thinking,” and “binary thinking”): Viewing events or people in all-or-nothing terms. “I get rejected by everyone,” or “It was a complete waste of time.”
MIND READING: Assuming that you know what people think without having sufficient evidence of their thoughts. “He thinks I’m a loser.”
LABELING: Assigning global negative traits to yourself or others (often in the service of dichotomous thinking). “I’m undesirable,” or “He’s a rotten person.”
NEGATIVE FILTERING: You focus almost exclusively on the negatives and seldom notice the positives. “Look at all of the people who don’t like me.”
DISCOUNTING POSITIVES: Claiming that the positive things you or others do are trivial, so that you can maintain a negative judgment. “That’s what wives are supposed to do—so it doesn’t count when she’s nice to me,” or “Those successes were easy, so they don’t matter.”
BLAMING: Focusing on the other person as the source of your negative feelings; you refuse to take responsibility for changing yourself. “She’s to blame for the way I feel now,” or “My parents caused all my problems.”
As you read through that list of distortions, it’s easy to see how somebody who habitually thinks in such ways would develop schemas that revolve around maladaptive core beliefs, which interfere with realistic and adaptive interpretations of social situations. Learning about cognitive distortions is especially important on a college campus. Imagine being in a seminar class in which several of the students habitually engage in emotional reasoning, overgeneralization, dichotomous thinking, and simplistic labeling. The task of the professor in this situation is to gently correct such distortions, all of which interfere with learning—both for the students engaging in the distortions and for the other students in the class. For example, if a student is offended by a passage in a novel and makes a sweeping generalization about the bad motives of authors who share the demographic characteristics of the offending author, other students might disagree but be reluctant to say so publicly. In such a case, the professor could ask a series of questions encouraging the student to ground assertions in textual evidence and consider alternative interpretations. Over time, a good college education should improve the critical thinking skills of all students.
Critical thinking is also needed to recognize and defeat “fake news.”It is not acceptable for a scholar to say, “You have shown me convincing evidence that my claim is wrong, but I still feel that my claim is right, so I’m sticking with it.” When scholars cannot rebut or reconcile disconfirming evidence, they must drop their claims or else lose the respect of their colleagues. As scholars challenge one another within a community that shares norms of evidence and argumentation and that holds one another accountable for good reasoning, claims get refined, theories gain nuance, and our understanding of truth advances.
1 note
·
View note
Text
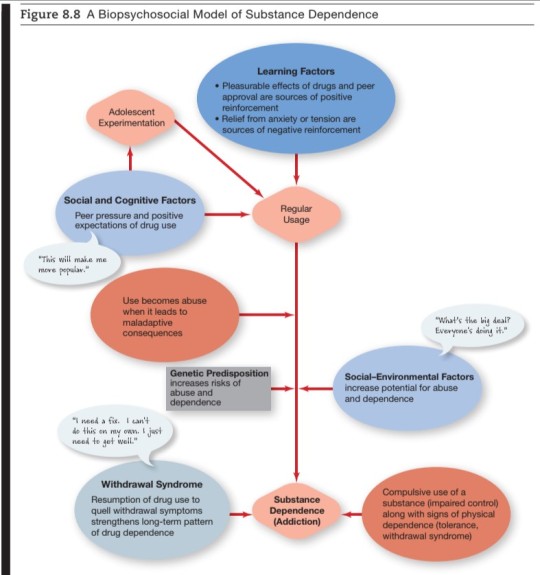
Psychopathology, Ch. 8 notes
{Note: I really do not like the term “substance abuse” because I think it’s weird to equate your personal health choices, even if they are self-destructive, with abuse. That’s the term I need to know and use for my upcoming exam, so it’s used throughout this post, but I’d like to avoid it when I can. Having a drug problem is hard on you and often hard on the people around you, but it doesn’t make you an abuser.}
I.
Identify the major types of substance-related disorders in the DSM-5 and describe their key features.
The DSM-5 classifies substance-related disorders in two major diagnostic categories: substance-induced disorders and substance use disorders.
Substance-induced disorders: a category of substance-related disorders induced by using psychoactive substances.
Substance intoxication: a type of substance-induced disorder characterized by repeated episodes of intoxication.
Substance withdrawal: a type of substance-induced disorder characterized by a cluster of symptoms following the sudden reduction or cessation of use of a psychoactive substance after physical dependence has developed.
Tolerance: physical habituation to a drug in which frequent use leads to higher doses being needed to achieve the same effects.
Withdrawal syndrome: a cluster of physical and psychological symptoms that arises following abrupt withdrawal from use of a psychoactive substance.
Substance use disorders: substance-related disorders characterized by maladaptive use of psychoactive substances, leading to significant impairment of functioning or personal distress.
Describe nonchemical forms of addiction or compulsive behavior.
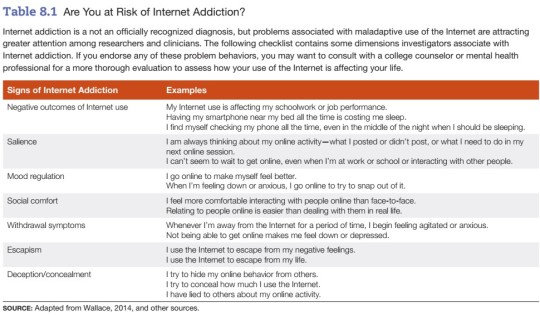
Patterns of compulsive behavior, such as compulsive gambling and shopping, and perhaps even excessive Internet use, may represent non-chemical forms of addiction. These behavior patterns are associated with classical signs of drug dependence or addiction, including impaired control over the behavior & withdrawal symptoms, such as anxiety or depression upon abrupt cessation of use.
{Note: I’m skeptical about calling compulsive behavior patterns “addiction”, because I think those behavior patterns are probably a symptom of something else, but compulsive substance use is ALSO usually a symptom of something deeper, so maybe it’s an accurate label. If we’re going to use this schema of “non-chemical addiction,” I hope that it leads to less stigma around compulsive drug use, not more stigma around compulsive behavior (because of association with addicts).}
Explain the difference between physiological dependence and psychological dependence.
Physiological dependence: bodily changes resulting from regular use of a drug, as denoted by the development of tolerance and/or a withdrawal syndrome (also called “chemical dependence”).
Addiction: impaired control over the use of a chemical substance, despite the harmful consequences it causes.
Psychological dependence: compulsive use of a substance to meet a psychological need.
Identify common stages in the pathway to drug dependence.
1. Experimentation: During this stage, the drug temporarily makes users feel good, even euphoric. Users feel they are in control and believe they can stop at any time.
{Note: at this stage, they probably are and they probably can!}
2. Routine use: During the next stage, a period of routine use, people begin to structure their lives around the pursuit and use of drugs. Denial plays a major role at this stage, as users mask the negative consequences of their behavior to themselves and others. Values change. What had formerly been important, such as family and work, comes to matter less than drugs.
{Note: it’s difficult to stop at this stage, unless you catch yourself early, but you can probably quit cold turkey here.}
3. Addiction/dependence: Routine use becomes addiction or dependence when users feel powerless to resist drugs, either because they want to experience their effects or to avoid the consequences of withdrawal. Little or nothing else matters at this stage.
{Note: it’s very difficult to stop at this point and you may not survive quitting cold turkey; you would want help at this stage, even if you rejected help during the previous one.}
II.
Describe the effects of depressants and the risks they pose.
Depressant: a drug that lowers the level of activity of the central nervous system.
- effects include intoxication, impaired coordination, slurred speech, and impaired intellectual functioning
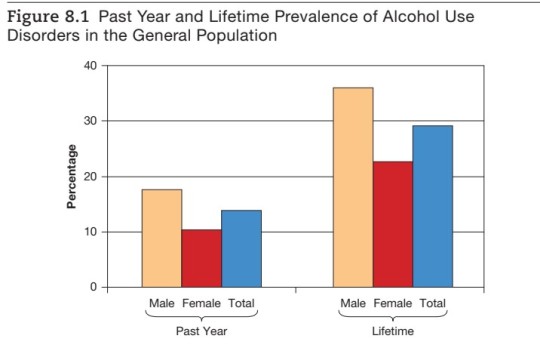
Alcoholism: alcohol addiction or dependence resulting in serious personal, social, occupational, or health problems.
- Chronic alcohol abuse is associated with health risks, including Korsakoff’s syndrome, cirrhosis of the liver, fetal alcohol syndrome, and other physical health problems.

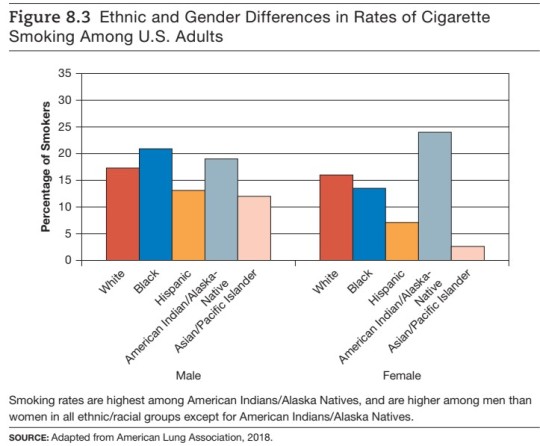
* Risk Factors for Alcoholism *
1. Gender
2. Age
3. Family history
4. Sociodemographic factors
5. Antisocial personality disorder
Barbiturates: sedative drugs that are depressants with high addictive potential.
- used medically for short-term relief of anxiety and treatment of epilepsy, among other uses
- can impair driving ability and can cause a fatal overdose, especially when combined with alcohol
Narcotics: drugs that are used medically for pain relief but also have strong addictive potential.
Endorphins: natural substances that function as neurotransmitters in the brain and are similar in their effects to opioids.
Morphine: a strongly addictive narcotic derived from the opium poppy that relieves pain and induces feelings of well-being.
Heroin: a narcotic derived from morphine that has strong addictive properties.
Describe the effects of stimulants and the risks they pose.
Stimulants: psychoactive substances that increase the activity of the central nervous system.
- Repeated use of nicotine (a mild stimulant found in tobacco) leads to physiological dependence.
Amphetamines: a class of synthetic stimulants that activate the central nervous system, producing heightened states of arousal and feelings of pleasure.
Amphetamine psychosis: a psychotic state characterized by hallucinations and delusions, induced by ingestion of amphetamines.
Cocaine: a stimulant derived from the leaves of the coca plant.
- Habitual cocaine use can lead to a variety of health problems, and an overdose can cause sudden death.
Crack: the crystallized, smokeable form of cocaine.

Describe the effects of hallucinogens and the risks they pose.
Hallucinogens: substances that distort sensory perceptions cause hallucinations.
- category includes LSD, psilocybin, and mescaline
- other drugs with similar effects include cannabis and phencyclidine; the latter can induce a state of mental confusion or delirium
- Hallucinogens do not lead to physiological dependence, but psychological dependence may occur.
- There are concerns about potential brain damage impacting learning & memory in heavy users of marijuana. {note: the studies I’ve seen on this topic indicate that using marijuana frequently starting in your teens/early 20’s has this impact, but it might not have the same effect if a person starts later in life. I’d be curious to know whether or not that’s true.}
Marijuana: a hallucinogenic drug derived from the leaves and stems of the plant Cannabis sativa.
III.
Describe biological perspectives on substance use disorders and explain how cocaine affects the brain.
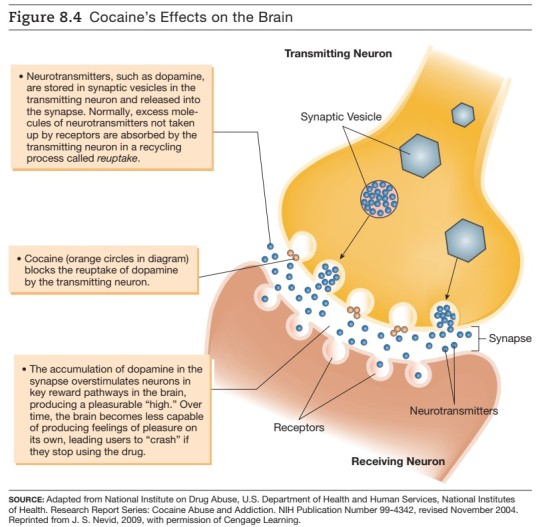
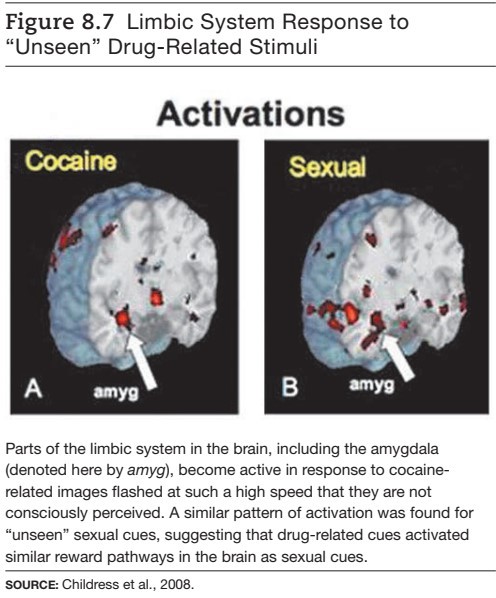
The biological perspective focuses on uncovering the biological pathways that may explain mechanisms of physiological dependence. The biological perspective spawns the disease model, which posits that alcoholism and other forms of substance dependence are disease processes. Cocaine blocks the reuptake of dopamine by the transmitting neuron, which means that more dopamine remains in the synaptic gap, creating a euphoric high by overstimulating receiving neurons in brain networks that regulate feelings of pleasure.

Describe psychological perspectives on substance use disorders.
A. Learning Theory Perspectives: view problems with substance abuse as learned patterns of behavior.
- operant conditioning
- alcohol and tension reduction
- negative reinforcement & withdrawal
- the conditioning model of cravings
- observational learning
B. Cognitive Perspectives: focus on roles of attitudes, beliefs, and expectancies in accounting for substance use/abuse.
C. Psychodynamic Perspectives: view problems of substance abuse, such as excessive drinking and habitual smoking, as signs of an oral fixation.
D. Sociocultural Perspectives: emphasize the cultural, group, and social factors that underlie patterns of drug use, including the role of peer pressure in determining adolescent drug use.
IV.
Identify biological treatments of substance use disorders.
Detoxification: the process of ridding the system of alcohol or other drugs under supervised conditions.
- Disulfiram
- Smoking cessation drugs
- Nicotine replacement therapy
Methadone: a synthetic opiate that does not produce a pleasurable high when used properly, but which can avert withdrawal symptoms in people with heroin addiction when they stop using heroin.
Naltrexone: a drug that blocks the high from alcohol as well as from opiates.
Identify factors associated with culturally sensitive approaches to treatment.
- using counselors from a person’s own ethnic group
- providing social support
- incorporating culturally specific values and indigenous forms of healing in the treatment program
- drawing upon clergy and church members
Identify a non-professional support group for people with substance use disorders.
A leading example is Alcoholics Anonymous, which promotes abstinence within a supportive group setting. {Note: I’m aware AA is controversial; some people love it and say it saved their life. Other people say it’s a cult and it got in the way of their recovery. I have no experience with AA either way, so I’m open to hearing everyone’s perspectives on them.}
Identify two major types of residential treatment facilities for people with substance use disorders.
Residential treatment approaches include hospitals that provide specialized services for substance abusers and therapeutic residences in the community.
Describe the psychodynamic treatment of substance abusers.
Psychodynamic treatment focuses on uncovering and working through the inner conflicts originating in childhood that may lie at the root of substance abuse problems.
Identify behavioral approaches to substance use disorders.
A. Self-control strategies
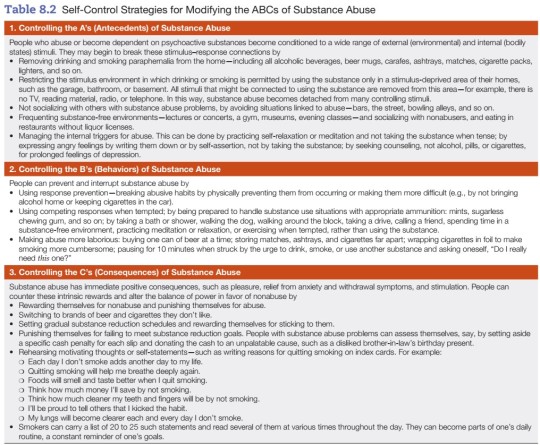
B. Contingency management programs
C. Aversive conditioning
D. Social skills training
E. Controlled drinking: a viable goal?
Describe relapse-prevention training.
Regardless of the initial success of a treatment technique, relapse remains a pressing problem in treating people with substance abuse problems. Relapse-prevention training employs cognitive behavioral techniques to help recovering substance abusers cope with high-risk situations and prevent lapses from becoming relapses by interpreting lapses in less damaging ways.
V.
Describe the key features of gambling disorder.
Gambling disorder: an addictive disorder characterized by a pattern of habitual gambling and impaired control over the behavior.
- frequently comorbid with substance use disorders and mood disorders
Describe ways of treating gambling disorder.
Promising treatment approaches for compulsive gambling have been developed, including anti-depressants and mood-stabilizing drugs and cognitive behavioral therapy, which is used to correct cognitive biases that may contribute to compulsive gambling. Many compulsive gamblers participate in peer support groups, such as Gamblers Anonymous, that help them gain insight into their self-defeating behavior and change their compulsive behavior patterns.
#abnormal psychology#psychopathology#psychology#my notes#study blog#cw: drugs#cw: gambling#cw: alcohol#cw: smoking#cw: death#cw: addiction
2 notes
·
View notes
Text
"Schema therapy is a type of therapy that targets schemas, maladaptive patterns of thinking that could cause someone to engage in unhealthy behavior or struggle to maintain adult relationships."
— PsychologyToday (2022)
0 notes
Video
youtube
Overcoming Early Maladaptive Schemas Through Stoicism
0 notes
Text
so my psych wants to focus on schema therapy with me which like. makes sense that’s chill. except also SCARY. anyway my homework rn is to identify when i’m using a maladaptive response??? idk the proper words but basically my main struggles are things like feeling inherently defective/broken and social isolation and unrelenting self standards. and i tend to respond to those schemas by avoiding/overcompensating/giving up which like yeah that Tracks. but it almost feels like i am Always responding to those things like i can’t isolate a specific circumstance idk. much to think about i Suppose !! wait is this me literally avoiding/giving up man what the fuck. i hate therapy sometimes
#they got me gal !!!#no i think it’ll be good for me. it’s hard to put much effort into improving myself and my mental health when i feel like i will always be#fundamentally broken and that im not worth being happy and healthy#so working on fixing those internalised assumptions is Important#but very daunting
1 note
·
View note
Text
Me and the polish baddie I pulled by having a robust variety of maladaptive schemas

0 notes
Text
Navigating the Path to Healing: Therapy's Transformative Role in Managing BPD
Welcome, fellow travellers, to a journey of healing and self-discovery. In the labyrinth of emotions that is Borderline Personality Disorder (BPD), therapy stands as a beacon of hope, guiding individuals through the twists and turns toward healing. Join us as we explore the profound impact of therapy in managing BPD and discover the transformative journey it offers.
Dialectical Behaviour Therapy (DBT): Finding Resilience Amidst the Storm
A journey where mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness are the compass points guiding the way.
This journey is DBT, a therapeutic approach renowned for its effectiveness in treating BPD. Through individual sessions and group skills training, individuals embark on a voyage of self-discovery, learning to navigate the stormy seas of their emotions and relationships with newfound resilience and grace.
Cognitive Behavioural Therapy (CBT): Illuminating the Path to Self-Awareness
In the vast landscape of the mind, CBT acts as a map, illuminating the hidden pathways of negative thought patterns and behaviours.
By shining a light on the connection between thoughts, feelings, and actions, individuals with BPD gain insight into their inner workings, paving the way for lasting change.
With CBT, the journey becomes a quest for self-awareness and empowerment, as individuals learn to rewrite the script of their lives one thought at a time.
Schema Therapy: Healing the Wounds of the Past
Deep within the recesses of the psyche lie the roots of BPD—maladaptive schemas and core beliefs that shape our perceptions of ourselves and the world.
Enter schema therapy, a journey into the heart of the matter, where past wounds are healed and distorted perceptions are untangled. Through exploration and reflection, individuals reclaim their narrative, shedding light on the shadows of the past and forging a path toward wholeness.
Mentalisation-Based Therapy (MBT): Navigating the Complexities of Relationships
As we journey through life, our relationships serve as guiding stars, illuminating the path ahead.
In MBT, individuals learn the art of mentalising—the ability to understand their own thoughts and emotions, as well as those of others.
Through dialogue and reflection, individuals with BPD develop a deeper understanding of themselves and their relationships, fostering connections rooted in empathy, compassion, and mutual respect.
Supportive Therapy: Finding Sanctuary Amidst the Storm
Amidst the trials and tribulations of the journey, there exists a sanctuary—a space of unconditional acceptance and understanding.
In supportive therapy, individuals find refuge from the storm, as therapists offer a listening ear and a compassionate heart. Through validation and empathy, individuals with BPD find the strength to weather life's storms, knowing they are not alone on their journey.
Conclusion:
As we embrace therapy as a cornerstone of our recovery journey, we open ourselves to the possibility of healing, growth, and self-compassion, one step at a time. In the tapestry of life, therapy weaves a thread of healing, connecting individuals with BPD to a sense of purpose, belonging, and empowerment. Together, let us embark on this journey of healing and transformation, guided by the transformative power of therapy.
#bpd support#bpd#bpd safe#bpd thoughts#psychology#bettersoonx#community support#emotional wellness#mental health#self care#therapy
0 notes