#glucagon-like peptide-1 (GLP-1)
Text

How does semaglutide works?
Semaglutide operates through its role as a glucagon-like peptide-1 (GLP-1) receptor agonist, closely emulating the actions of the natural GLP-1 hormone released post-meal. By binding to GLP-1 receptors on pancreatic beta cells, semaglutide stimulates insulin secretion, aiding in glucose uptake and lowering blood sugar levels. Simultaneously, it suppresses glucagon release, curbing liver-generated glucose output. The medication also slows gastric emptying, fostering prolonged fullness and controlled nutrient absorption. This is reinforced by heightened feelings of satiety and reduced appetite facilitated by semaglutide’s interaction with GLP-1 receptors in the brain. These mechanisms collectively contribute to improved blood sugar control, reduced appetite and sustainable weight loss, making semaglutide a valuable medication for both diabetes management and long-term weight management.
#polypeptide#weight loss#polypeptide.ltd#tirzepatide#semaglutide#tirzepatide vs semaglutide#semaglutide works#retatrutide weight loss#tirzepatide weight loss#glucagon-like peptide-1 (GLP-1)
1 note
·
View note
Text
Comprehensive Guide to Diabetes Medications
Welcome to this comprehensive guide on diabetes medications, where we shall explore the intricacies of various pharmacological agents that aid in effectively managing blood sugar levels and fostering a healthier life with diabetes.
1. Insulin Injections
Insulin, a paramount hormone synthesized by the pancreas, orchestrates the regulation of blood sugar levels, a critical facet for individuals…

View On WordPress
#biguanides#Blood Sugar Control#diabetes medications#DPP-4 inhibitors#edema#fluid retention#genital yeast infections#glucagon-like peptide-1 (GLP-1)#glucose regulation#glucose-dependent insulinotropic polypeptide (GIP)#heart disease#hypoglycemia#Incretin Hormones#injection site reactions#insulin injections#Insulin Sensitivity#intermediate-acting insulin#Liver Glucose Production#long-acting insulin#metformin#nephrons#pancreatic beta cells#Pancreatitis#Potential Side Effects#rapid-acting insulin#SGLT2 Inhibitors#short-acting insulin#sodium-glucose cotransporter 2 (SGLT2)#Sulfonylureas#Type 1 Diabetes
0 notes
Text

In recent years, a breakthrough in diabetes management has emerged in the form of Glucagon-Like Peptide-1 (GLP-1) analogs. These innovative medications have revolutionized the treatment landscape by providing improved glycemic control and additional benefits for individuals with type 2 diabetes.
Read More: https://cmibloggers.blogspot.com/2023/06/understanding-glucagon-like-peptide-1.html
#coherent market insights#Healthcare Industry#Pharmaceutical#Glucagon-Like Peptide-1 analogs Market#GLP-1 receptor agonists#Diabetes management#Type 2 diabetes#Glycemic control#Blood sugar regulation#Insulin therapy
0 notes
Link
Latin America Glucagon-like Peptide-1 (GLP-1) Agonists Market is poised to grow at CAGR of 2.5 % by 2027. Key players driving Latin America Glucagon-like Peptide-1 (GLP-1) Agonists Market are Novo Nordisk, AstraZeneca, Sanofi, Eli Lilly, Biocon among others.
#Latin America glucagon-like peptide-1 (GLP-1) agonists market#Latin America glucagon-like peptide-1 (GLP-1) agonists market size#Latin America glucagon-like peptide-1 (GLP-1) agonists market share#Latin America glucagon-like peptide-1 (GLP-1) agonists market report#Latin America glucagon-like peptide-1 (GLP-1) agonists market forecast
0 notes
Text
The global Glucagon Like Peptide-1 (GLP-1) Agonists market size is estimated to be worth US$ 8816.2 million in 2021 and is forecast to a readjusted size of US$ 21340 million by 2030 with a CAGR of 13.6% during the forecast period 2022-2030.
0 notes
Text
Because my most popular post is about weight loss and how it's a crock, I get a lot of questions about various things, including bariatric surgery--just posted the link to the post I did about that--but also Ozempic/Wegovy, the once-weekly injectable semaglutide medication that was developed for diabetes but was found to have independent benefits on weight loss.
I always said that weight loss was like Viagra: when a medication came along that actually worked, it would explode. We'd all hear about it. Fen-phen in the 90s worked, but it was bad for your heart. Stimulants, like meth, may cause weight loss, but they do it at the cost of heart health, and raise your likelihood of dying young. Over the counter weight loss supplements often contain illegal and unlisted thyroid hormone, which is also dangerous for the heart if taken in the absence of a real deficiency. Orlistat, or "Alli," works the same way as the Olestra chips Lays made in the 1990s--it shuts off your ability to digest fats, and the problem with that is that fats irritate the gut, so then you end up with fatty diarrhea and probably sharts. Plus Alli only leads to 8-10lbs of weight loss in the best case scenario, and most people are not willing to endure sharts for the sake of 8lbs.
And then came the GLP-1 agonists. GLP stands for glucagon-like peptide. Your body uses insulin to make cells uptake sugar. You can't just have free-floating sugar and use it, it has to go into the cells to be used. So if your body sucks at moving sugar into the cells, you end up with a bunch of glucose hanging out in places where it shouldn't be, depositing on small vessels, damaging nerves and your retinas and kidneys and everywhere else that has a whole lot of sensitive small blood vessels, like your brain.
Glucagon makes your liver break down stored sugars and release them. You can think of it as part of insulin's supporting cast. If your body needs sugar and you aren't eating it, you aren't going to die of hypoglycemia, unless you've got some rare genetic conditions--your liver is going to go, whoops, here you go! and cough it up.
But glucagon-like peptide doesn't act quite the same way. What glucagon-like peptide does is actually stimulating your body to release insulin. It inhibits glucagon secretion. It says, we're okay, we're full, we just ate, we don't need more glucagon right now.
This has been enough for many people to both improve blood sugar and cause weight loss. Some patients find they think about food less, which can be a blessing if you have an abnormally active hunger drive, or if you have or had an eating disorder.
However, every patient I've started on semaglutide in any form (Ozempic, Wegovy, or Rybelsus) has had nausea to start with, probably because it slows the rate of stomach emptying. And that nausea sometimes improves, and sometimes it doesn't. There's some reports out now of possible gastroparesis associated with it, which is where the stomach just stops contracting in a way that lets it empty normally into the small intestine. That may not sound like a big deal, but it's a lifelong ticket to abdominal pain and nausea and vomiting, and we are not good at treating it. We're talking Reglan, a sedating anti-nausea but pro-motility agent, which makes many of my patients too sleepy to function, or a gastric pacemaker, which is a relatively new surgery. You can also try a macrolide antibiotic, like erythromycin, but I have had almost no success in getting insurance to cover those and also they have their own significant side effects.
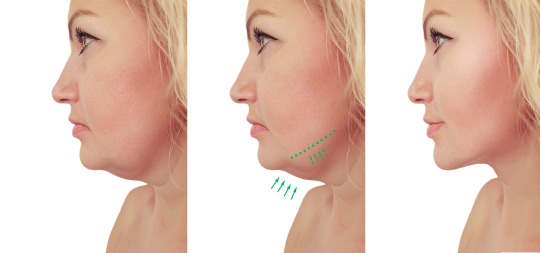
Rapid weight loss from any cause, whether illness, medication, or surgery, comes with problems. Your skin is not able to contract quickly. It probably will, over long periods of time, but "Ozempic face" and "Ozempic butt" are not what people who want to lose weight are looking for. Your vision of your ideal body does not include loose, excess skin.
The data are also pretty clear that you can't "kick start" weight loss with Ozempic and then maintain it with behavioral mechanisms. If you want to maintain the weight loss, you need to stay on the medication. A dose that is high enough to cause weight loss is significantly higher than the minimum dose where we see improvements in blood sugar, and with a higher dose comes higher risk of side effects.
I would wait on semaglutide. I would wait because it's been out for a couple of years now but with the current explosion in popularity we're going to see more nuanced data on side effects emerging. When you go from Phase III human trials to actual use in the world, you get thousands or millions more data points, and rare side effects that weren't seen in the small human trials become apparent. It's why I always say my favorite things for a drug to be are old, safe, and cheap.
I also suspect the oral form, Rybelsus, is going to get more popular and be refined in some way. It's currently prohibitively expensive--all of these are; we're talking 1200 or so bucks a month before insurance, and insurance coverage varies widely. I have patients who pay anything from zero to thirty to three hundred bucks a month for injectable semaglutide. I don't think I currently have anyone whose insurance covers Rybelsus who could also tolerate the nausea. My panel right now is about a thousand patients.
There are also other GLP-1 agonists. Victoza, a twice-daily injection, and Trulicity, and anything else that ends in "-aglutide". But those aren't as popular, despite being cheaper, and they aren't specifically approved for weight loss.
Mounjaro is a newer one, tirzepatide, that acts on two receptors rather than one. In addition to stimulating GLP-1 receptors, it also stimulates glucose-dependent insulinotropic polypeptide (GIP) receptors. It may work better; I'm not sure whether that's going to come with a concomitantly increased risk of side effects. It's still only approved for diabetes treatment, but I suspect that will change soon and I suspect we'll see a lot of cross-over in terms of using it to treat obesity.
I don't think these medications are going away. I also don't think they're right for everyone. They can reactivate medullary thyroid carcinoma; they can fuck up digestion; they may lead to decreased quality of life. So while there may be people who do well with them, it is okay if those people are not you. You do not owe being thin to anyone. You most certainly do not owe being thin to the extent that you should risk your health for it. Being thin makes navigating a deeply fat-hating world easier, in many ways, so I never blame anyone for wanting to be thin; I just want to emphasize that it is okay if you stay fat forever.
756 notes
·
View notes
Text
Materials engineers at Stanford University have developed a novel hydrogel drug delivery system that transforms daily or weekly injections of diabetes and weight control drugs like Ozempic, Mounjaro, Trulicity, Victoza, and others to just once every four months. In a new study, published Nov. 21 in Cell Reports Medicine, researchers believe that such a system will greatly improve management of both diabetes and weight, improve patient drug compliance, and help those with Type 2 diabetes improve long-term health outcomes.
These drugs all work by mimicking the hormone glucagon-like peptide 1 (GLP-1). But, as good as they are at helping people manage their diets and their weight, the typical daily or weekly injections are a burden for many patients.
“Adherence is one of the biggest challenges in Type 2 diabetes management,” said Eric Appel, associate professor of materials science and engineering at Stanford and principal investigator on the new hydrogel that allows the slow release of the diet control drugs over many months. “Needing only three shots a year would make it much easier for people with diabetes or obesity to stick with their drug regimens.”
Continue Reading.
91 notes
·
View notes
Text
Ozempic: Dying To Be Thin
I have recently been following a few stories and commentators as they have reported on the side effects of Ozempic. My typical literary niche is mental health, inspiration and motivation for self-development. While I don’t follow the latest trends in any area I had followed the Ozempic one for some reason.
I think the part that interested me the most was many of the people who interviewed were willing to buy the drug on the black market, unverified websites and the like. Don’t read what I’m not writing I think it’s important not to point fingers but to have a holistic view of the Ozempic side effects issue.
As I researched the stories I found most of the cases were in the United States and the UK. In the ever-evolving landscape of healthcare, understanding the implications of medications is paramount. Most people are aware who follow Ozempic know it’s used for type 2 diabetes.
It gained prominence for weight loss in the last few years. I reviewed some history and current lawsuits due to the side effects. I was not aware that the side effects can affect vital organs and cause other unsettling concerns. Some may not be aware that drugs can be researched and more information can be reviewed on the FDA’s website.
Another thing that consumers can do is explore if there are current lawsuits or recalls on drugs before they start taking them. I know most people trust their health care professional but we should do our due diligence as well.
Ozempic, a member of the glucagon-like peptide-1 (GLP-1) receptor agonist class, plays a pivotal role in regulating blood sugar levels. However, like many pharmaceutical interventions, its therapeutic benefits are accompanied by a spectrum of potential side effects. These side effects vary in intensity and occurrence, impacting individuals in diverse ways.
I’m a therapist, not a physician or a nurse. I have treated many clients who struggle with weight loss or menopausal weight gain. Most of the clients I have served have found it difficult to lose weight as they have gotten older.
I have referred them to their primary care doctor. With that said some people want a quick fix for whatever reason and I can see the frustration and all the concerns that go with trying to lose weight and obtain wellness.
My concern with the latest trend of those on Ozempic is the side effects and the those that may not be informed enough on those who are dying as a result of using Ozempic or the generic form of it.
Commonly reported side effects of Ozempic encompass gastrointestinal disturbances, with nausea and diarrhea being prevalent among users. These effects are often transient, diminishing over time as the body adjusts to the medication. Concurrently, injection site reactions, another common occurrence, may manifest as redness, swelling, or itching.
While these side effects are generally considered mild, their prevalence underscores the importance of patient awareness and proactive management. As I listened to story after story most of the people had other chronic illnesses as well.
Beyond the scope of common side effects lie more serious complications that demand heightened attention. Instances of pancreatitis, though rare, have been associated with the use of Ozempic. Pancreatitis, characterized by inflammation of the pancreas, necessitates immediate medical intervention and underscores the need for vigilant monitoring during Ozempic therapy.
Additionally, concerns have been raised regarding the potential association between Ozempic and thyroid tumors. Though the risk is deemed low, healthcare practitioners and users alike must remain vigilant, emphasizing the importance of regular health check-ups and communication between patients and their healthcare providers.
It is essential to recognize the symbiotic relationship between healthcare education and the communication of potential side effects. In the digital age, individuals often turn to search engines for health-related information.
I will say most of what I found were researchers on YouTube and science journals that are talking about the side effects of Ozempic a little more now. Thus, effective communication becomes a conduit for informed decision-making. Utilizing search engine optimization (SEO) strategies ensures that information about Ozempic’s side effects is readily accessible to those seeking it.
I’m a news buff and enjoy all things science and this story was disturbing because people were and are dying from one thing but the root cause was from taking Ozempic. I hope people will do their due diligence so not one more person has to die to be thin.
For those who may be interested in strategic keyword integration, such as “Ozempic side effects” or “Ozempic complications,” the dissemination of valuable information becomes more efficient and widespread.
Thank you for reading
Be Well!
#inspiration#self love#motivation#self help#self improvement#self care#glow up#glow up era#becoming that girl#manifesation#self confidence#self development#self awareness#personal growth#positive mindset#self growth#growth mindset#priorities
10 notes
·
View notes
Text
Do viruses “hijack” the body? “Viruses are more like cone snails than hijackers.” Cone shell venom, weaponized hormones, and predatory insulin overdose. Gila monsters and diabetes treatment. Mimicry. Totally unlike beings contain patches of intimate and detailed sameness. Bodies hold imprints of the other entities’ influence, like a shadow. Where does one creature end and another creature begin?
---
In the twentieth century, the word “hijacking” came to typify the explanation of what viruses do to the cells they infect. How commonplace it is to now say: the virus hijacks the host cell’s machinery in order to replicate itself. [...] However, viruses are not like spaceships, and cells are not just like twentieth-century semitrailer trucks, armored vehicles, or passenger jets whose resources can be plundered and whose operators can be coerced into unwanted journeys. [...] It appears to transparently explain things. But is this a good description of a virus and the creatures it is capable of infecting? [...]
Anthropomorphism and personification of microbial entities in the explanation of virology is a understandable tendency; in this way, viral action is domesticated to the human scale.
But maybe it’s time to practice some resolutely non-domesticating conid-amorphism, some conus-centrism, and see what happens if we forge a new avenue for thinking of viruses in terms of venomous cone snails.
---
Conidae is the taxonomic name for the family of gastropods known more colloquially as cone snails, or predatory sea snails. “One of the most successful lineages of marine animals,” the hundreds of species of Conidae are characterized by their use of complex venoms to capture prey. Some of these snails prey on worms, some on other snails, and some on fish. In 2015, researchers reported that Conus geographus uses an insulin overdose to disorient and disable its fish prey, releasing the toxin into the water.
Insulin appears to be a component of the nirvana cabal, a toxin combination in these venoms that is released into the water to disorient schools of small fish, making them easier to engulf with the snail’s distended false mouth, which functions as a net. If an entire school of fish simultaneously experiences hypoglycemic shock, this should directly facilitate capture by the predatory snail.
The released insulin does not affect the snail itself, because its venom insulin mimics fish insulin, not its own molluscan variety. Venomous snails that hunt worms in this fashion make a different insulin mimic, specific to worms.
---
This may seem like a weird aberration on the part of an obscure life-form, yet cone snails are only one kind of creature that roams the evolutionary space in which one being’s molecules evolve to participate in the physiology of another. There are enough examples of organisms employing these tactics that they are grouped together in scientific reviews of “weaponized hormones.” [...]
For example, the first diabetes therapy drug that works by mimicking the glucagon-like peptide hormone (GLP-1) was discovered by analyzing the venom of the Gila monster. GLP-1 is a hormone released by the gut after eating that stimulates insulin production and slows movement of food through the intestinal tract. The making of a drug that acts like GLP-1 was not a process of exactly copying human GLP-1. For that you wouldn’t need a Gila monster and thousands of years of coevolution between lizards and their prey.
Rather, scientists learned alternative molecular strategies for binding to the hormone’s receptor from the Gila monster venom component.
Perhaps viruses are equally “interested” in glucose control in their own noncognitive way, in that their replication and continued existence is vested in their hosts’ metabolisms. As noted above, they do not possess the means for making the proteins encoded by the genes in their genomes, but rather depend on the cells they infect to do that translation and transcription. [...]
They don’t have their own bodies; they only have their hosts’ bodies.
And bit by bit, through the endless nonillion-fold exploration of evolutionary space -- the space that makes the difference between persisting long enough to be replicated versus falling apart into the wash of biological decay -- it has turned out to be good practice to mimic your host’s cell cycle and metabolic hormones. Different viruses, different hosts, same strategy. [...]
---
If viruses are effective because they mimic human hormones or hormone receptors, this will drive the evolution and duplication of hormones over time because it is advantageous for them to change enough to not be good viral targets. Thus, it has been suggested that some features of human hormonal genes in the placenta arise from their function as viral “decoys” in this tit-for-tat of copying and changing.
It is for this reason that viruses could be thought of in terms of venomous cone snails rather than hijackers.
Not all these mimicry techniques target metabolic processes; many viruses famously encode other proteins that allow them to evade immune detection by attempting to look like parts of the immune system rather than its targets. But there is a theme here. The virus takes on some aspects of the shape of the body that ensures its continuity. This gives rise to totally unlike beings containing patches of intimate and detailed sameness, molecules that bear the same precise contours to fit into a particular hormone receptor, yet perhaps bear no common genetic heritage. Viruses, like cone snails, evolve to be more like what sustains them. It is an uncomfortable form of relatedness, this predatory metabolic convergence, but it cannot be denied that it generates amazing patterns of likeness across biological kingdoms without everything having to be descended from the same line of direct genetic inheritance.
Where does hormone end and hormone-like begin?
If the mimic converges on the original, and places the original under evolutionary pressure to diverge, what is left is a seesawing mirrored relationship of competitive difference and similarity, not an original and a mimic. Even if something has evolved to get away from its mimic, it holds the imprint of that entity’s influence in its difference, like a shadow.
In practical terms, looking into cone snails and viral genomes suggests new ways of making drugs, which are human-made mimics that seek to manipulate physiology by augmenting or suppressing the action of the molecule that has been mimicked.
In philosophical terms on the other hand, that cone snail or amphibian venom gets enrolled in the diabetes epidemic by becoming a blood sugar–controlling drug indicates that anthropomorphic concepts such as hijacking may possibly be the least illuminating explanatory tactic for understanding what viruses do, and are, in relation to their bodies. (Yes, their bodies. That means us).
---
Text by: Hannah Landecker. “Viruses Are More Like Cone Snails Than Hijackers.” e-flux. October 2022. [Bolded emphasis and italicized first paragraph added by me.]
70 notes
·
View notes
Text
It turns out she’s down about ten pounds and happy about it. “Somebody once told me I had a size-zero personality, and they assumed that I was thinner than I was,” she tells me. “We don’t talk about it, but everybody knows it. Thin is power.”
Allison isn’t alone in seeming to be suddenly, unaccountably slimmer of late. She admitted to me — with the provision that I not use her real name — the reason, one that is increasingly common if still not quite openly discussed. For the past month, she’s been jabbing herself every week with Ozempic, the heavily advertised (“Oh, oh, oh, Ozempic,” to the tune, none too subtly, of the ’70s classic-rock hit “Magic”) diabetes miracle drug, which works by mimicking a naturally occurring hormone, GLP-1 (glucagon-like peptide one), to manage hunger and slow stomach emptying.
For diabetics, it lowers blood-sugar levels. It also subdues the imp of appetite. The pounds fly off. That’s why Allison, who is not diabetic, prediabetic, or even overweight, is on it. Doctors have wide latitude to prescribe drugs off label for anyone they think may medically benefit, and many patients have found doctors — or, failing that, nurse practitioners or medi-spas — ready to certify that they would. Or some, like Allison, find it through a peddler not particular about a prescription or in the web’s dark morass.
To get hers, Allison calls up a Los Angeles–based provider she has never seen or met, sends over $625, and is shipped a monthly supply. What she calls Ozempic is not the brand-name product pre-packaged in a sky-blue injector pen by Novo Nordisk, the Danish pharmaceutical company that makes and markets the drug. She receives generic semaglutide, the active ingredient in the medication, and has to mix and prepare it for injection herself, which — since semaglutide is under patent by Novo Nordisk until 2032 in the U.S. — suggests her meds are likely coming from a compounding pharmacy or a vendor selling research-grade ingredients. The lower price is also a tell: Ozempic retails for about $900 a month if your insurance doesn’t cover it.
17 notes
·
View notes
Text
Mounjaro
Mounjaro: A Revolutionary Treatment for Type 2 Diabetes
Type 2 diabetes is a chronic condition that affects millions of people worldwide. It is a condition that occurs once the body either does not produce enough insulin or cannot utilize the insulin it produces effectively. If left untreated, type 2 diabetes can result in serious health complications such as heart disease, stroke, kidney damage, and blindness. Fortunately, there are buy mounjaro to help manage the problem, and Mounjaro is one such treatment which has recently received FDA approval.
What is Mounjaro?
Mounjaro is a once-weekly injection that is FDA approved for the treating type 2 diabetes. It is just a combination of two hormones, liraglutide and exenatide, that work together to help control blood sugar levels. Liraglutide is really a glucagon-like peptide-1 (GLP-1) receptor agonist that helps to increase insulin secretion, suppress glucagon secretion, and decelerate gastric emptying. Exenatide is really a GLP-1 receptor agonist that works similarly to liraglutide but has a slightly shorter duration of action.
SO HOW EXACTLY DOES Mounjaro Work?
Mounjaro functions by mimicking the consequences of the natural hormones that regulate blood sugar in your body. When injected, the liraglutide and exenatide in Mounjaro activate the GLP-1 receptors in the pancreas, which stimulates the release of insulin and suppresses the release of glucagon. This helps to lower blood sugar levels and reduce the risk of hyperglycemia. Mounjaro also slows down the rate of which food leaves the stomach, which can help control appetite and reduce the risk of overeating.
What Are the Benefits of Mounjaro?
Mounjaro has several benefits that make it a stylish treatment option for people with type 2 diabetes. Firstly, this is a once-weekly injection, which means that it is more convenient than a number of the other treatments available that want daily injections or frequent monitoring. Secondly, it has been shown to be impressive at controlling blood sugar, with some studies reporting a significant reduction in HbA1c levels. Finally, it includes a relatively low risk of side effects, which makes it a safe and well-tolerated treatment option for many people.
What Are JP Weight Loss Center of Mounjaro?
Like all medications, Mounjaro can cause side effects in some people. The most common side effects of Mounjaro include nausea, vomiting, diarrhea, constipation, and headache. These side effects are usually mild and go away on their own within a few days. In rare cases, Mounjaro can cause more serious side effects such as pancreatitis, kidney failure, or allergies. If you experience these side effects, you need to seek medical assistance immediately.
Conclusion
Mounjaro is really a revolutionary treatment for type 2 diabetes which has recently received FDA approval. It is just a once-weekly injection that combines two hormones, liraglutide and exenatide, to help control blood sugar levels. Mounjaro is highly effective at managing type 2 diabetes and contains a relatively low risk of side effects. If you are living with type 2 diabetes, you should speak to your doctor to see if Mounjaro is a suitable treatment option for you personally.

4 notes
·
View notes
Text
The Ozempic Face: A Comprehensive Analysis
Ozempic (semaglutide) is a well-known medication used in the treatment of type 2 diabetes. Apart from its efficacy in managing blood sugar levels, it has also been associated with a unique side effect known as the "Ozempic Face." This article sheds some light on the phenomenon of Ozempic Face, exploring its definition, potential causes, symptoms, and management, as well as its relevance in the context of diabetes treatment.
Understanding Ozempic
Ozempic is a glucagon-like peptide-1 (GLP-1) receptor agonist, a class of drugs that mimics the action of incretin hormones, leading to increased insulin secretion, decreased glucagon release, delayed gastric emptying, and reduced appetite. Semaglutide, the active ingredient in Ozempic, has been shown to be highly effective in improving glycemic control and promoting weight loss in patients with type 2 diabetes.
What is Ozempic Face?
The term "Ozempic Face" is not an official medical term but rather a colloquial expression used by patients and some healthcare professionals to describe a distinct change in facial appearance observed in individuals taking Ozempic. Reports suggest that patients undergoing Ozempic treatment may experience subtle alterations in facial appearance, such as fuller cheeks and a more youthful look. These effects are attributed to the medication's impact on subcutaneous fat and have garnered considerable attention in online diabetes communities and social media platforms.
Potential Causes
The exact mechanism behind Ozempic Face is not yet fully understood, and research in this area is limited. However, it is believed to be related to the medication's impact on adipose tissue, which is the body's fat-storing tissue located beneath the skin. Semaglutide's activation of GLP-1 receptors may affect adipocytes (fat cells) in a way that promotes fat storage and decreases fat breakdown, particularly in facial areas. Nevertheless, more research is needed to elucidate the underlying biological processes responsible for this phenomenon.
Symptoms of Ozempic Face
Patients who experience Ozempic Face typically report changes in facial features that include:
Fuller cheeks: One of the most commonly reported symptoms is a plumper appearance in the cheeks, giving a rounder and more youthful look.
Smoother skin: Some individuals notice a smoother texture to their facial skin, possibly due to increased subcutaneous fat.
Diminished wrinkles: There have been reports of reduced facial wrinkles or lines, contributing to a more rejuvenated appearance.
It is crucial to emphasize that these effects may vary between individuals, and not everyone taking Ozempic will experience Ozempic Face. Additionally, the intensity of these changes may differ from person to person.
Management and Relevance
There are no specific guidelines or recommendations regarding the management of Ozempic Face. Since it is considered a cosmetic change rather than a medical concern, many individuals do not seek treatment for this side effect. If the changes in facial appearance become bothersome to the patient, they may consider discussing alternative treatment options with their healthcare provider. However, it is essential to weigh the potential benefits of Ozempic's efficacy in managing diabetes and promoting weight loss against any cosmetic side effects.
It's important to note that Ozempic Face is not a reason to discontinue Ozempic treatment, especially if the medication is effectively controlling blood sugar levels and promoting weight loss, which are critical factors in managing type 2 diabetes.
As with any medication, it is essential for patients to be aware of potential side effects and to have open discussions with their healthcare providers about their experiences. If patients are concerned about Ozempic Face or any other side effects, they should seek guidance from their healthcare professionals to make informed decisions about their diabetes treatment plan. Overall, Ozempic remains a valuable option in managing type 2 diabetes, and its potential side effects should be weighed against the benefits it offers in improving patients' quality of life and overall health.
2 notes
·
View notes
Text
5 Best peptides for Weight Loss

1 Best Peptide for Weight Loss: Semaglutide
Semaglutide belongs to a class of medications known as glucagon-like peptide-1 receptor agonists, or GLP-1 RAs. It mimics the GLP-1 hormone, released in the gut in response to eating. The Semaglutide injection works by slowing down how quickly food leaves your stomach and allows you to feel full for a longer period of time. By reducing hunger, lowering your appetite and increasing feelings of fullness, it will reduce your calorie intake and allow you to lose weight, 1-2 pounds a week.
2 Peptide for Weight Loss: Tirzepatide
Tirzepatide is a novel medication that is FDA approved for the treatment of type 2 diabetes mellitus. Given its potent weight loss properties, tirzepatide be used off-label for obesity treatment. It works as a dual GLP-1 agonist and GIP agonist to maximize similar benefits that are seen with GLP-1 medications such as semaglutide. It is currently implemented as a second-line diabetes medication, similar to GLP-1 medications, and given as a once-a-week subcutaneous injectable.
3 Peptide for Weight Loss: Liraglutide
Liraglutide, is an anti-diabetic medication used to treat type 2 diabetes, and chronic obesity. It is a second line therapy for diabetes following first-line therapy with metformin. Its effects on long-term health outcomes like heart disease and life expectancy are unclear. It is given by injection under the skin.
5 Peptide for Weight Loss: Retatrutide
Retatrutide is an agonist of the glucose-dependent insulin otropic polypeptide, glucagon-like peptide 1, and glucagon receptors. As can be expected, such a significant reduction in body weight in overweight and obese people also resulted in an improvement in blood pressure, cholesterol, and glucose parameters.
How do Peptides for Weight loss Work?
Most of the peptides, if not all, work via a common mechanism of action. They increase the release of Growth Hormone from the anterior pituitary gland, which leads to systemic effects. This is primarily seen in peptides used explicitly for muscle growth and endurance.
As far as weight loss peptides are concerned, it gets pretty interesting!
Some of these peptides work by increasing growth hormone levels. The growth hormone, in turn, targets specific sites like adipocytes and hepatocytes, causing raised cellular metabolism and fat burning.
Besides this, most peptides also work by rapidly increasing the process of lipolysis and simultaneously inhibiting excess lipogenesis from occurring. This leads to a net loss of fat.
A few peptides also work by regulating hormones responsible for glycemic control, like insulin and glucagon. With more insulin, glucose is transported inside the cells for energy expenditure. This subsequently aids in further weight loss.
热推
#bodybuilding#peptides#loss weight#health#benefits#Semaglutide#Tizepatide#liraglutide#retatrutide#injection#growth#energy#fat
2 notes
·
View notes
Text
Interesting Dosages of Semaglutide between Three Brands

1. What is Semaglutide?
Semaglutide, sold under the brand names Ozempic, Wegovy and Rybelsus.Semaglutide is a synthetic derivative based on the naturally occurring GLP-1peptide, which is known for its ability to reduce blood sugar levels and enhance insulin secretion. Recent research suggests that Semaglutide may also have positive effects on heart, liver, and lung function. And it could potentially slow down or prevent the progression of Alzheimer’s disease.
2. How does Semaglutide work?
Semaglutide works as a GLP-1 agonist, meaning it mimics the effects of a hormone called glucagon-like peptide-1 (GLP-1) in the body. GLP-1 is naturally released by the intestines in response to food intake and plays a crucial role in regulating blood sugar levels and appetite.
When semaglutide is injected, it binds to and activates GLP-1 receptors on various cells in the body, including pancreatic cells. This activation leads to several beneficial effects. First, semaglutide increases insulin release from the pancreas, which helps lower blood sugar levels by facilitating the uptake of glucose into cells for energy. Increased insulin also helps to reduce the production of glucose by the liver. Second, semaglutide suppresses the release of glucagon, a hormone that raises blood sugar levels. By reducing glucagon levels, semaglutide further contributes to the overall control of blood sugar.

3. Benefits of Semaglutide
Improved blood sugar control. Semaglutide, as a GLP-1 receptor agonist, helps regulate blood sugar levels in individuals with type 2 diabetes. It stimulates insulin release from the pancreas, which leads to better glucose utilization by the body’s cells. By reducing glucagon secretion and slowing down gastric emptying, semaglutide helps lower blood sugar levels and maintain better glycemic control.
Weight loss. Semaglutide has been found to promote weight loss when used for weight management in individuals with obesity or excess weight. By suppressing appetite and inducing a feeling of fullness, it can help reduce calorie intake and contribute to sustainable weight loss when combined with a reduced-calorie diet and exercise.
Cardiovascular risk reduction. In individuals with type 2 diabetes and established cardiovascular disease, semaglutide (specifically Ozempic) has been shown to reduce the risk of major cardiovascular events like heart attack or stroke. This benefit can provide additional protection to individuals with both diabetes and cardiovascular conditions.
Potential benefits in cognition. Semaglutide has shown potential benefits in improving cognitive function, particularly in individuals with mildl cognitive impairment or mild dementia caused by Alzheimer’s disease. It has been found to protect against amyloid-ß plaques, which are associated with cognitive decline in Alzheimer’s disease. Preclinical studies and ongoing clinical trials are evaluating semaglutide’s impact onl cognitive function. Results from these trials will provide more information about semaglutide’s effectiveness in improving cognitive abilities in Alzheimer’s disease.
4. Side effects of Semaglutide
Side effects from semaglutide injection might occur. If any of these symptoms are severe or do not go away, let your doctor know right once:
Vomiting
Nausea
Diarrhea
abdominal pain
Constipation
Heartburn
Burping
5. Dosages of Semaglutide (For Type 2 Diabetes Mellitus)

(1) Ozempic (semaglutide injection):
Initial Dose: 0.25 mg subcutaneously once weekly for 4 weeks.
Maintenance Dose: After the initial 4 weeks, increase the dose to 0.5 mg subcutaneously once weekly.
Further Dose Adjustment: If glycemic control is not achieved after at least 4 weeks on the 0.5 mg dose, the dose can be increased to 1 mg once weekly.
Maximum Dose: If needed, the dose can be further increased to 2 mg once weekly, but it should not exceed 2 mg per week.
(2) Rybelsus (oral semaglutide tablets):
Initial Dose: 3 mg orally once daily for 30 days (intended for treatment initiation, not for glycemic control).
Maintenance Dose: After 30 days on the 3 mg dose, increase the dose to 7 mg orally once daily.
Further Dose Adjustment: If additional glycemic control is needed, the dose can be increased to 14 mg orally once daily.
Note: Taking two 7 mg tablets to achieve the 14 mg dose is not recommended.
(3) Switching between Ozempic and Rybelsus:
Switching from Rybelsus to Ozempic: Start with 0.5 mg subcutaneously once weekly on the day after the last Rybelsus dose.
Switching from Ozempic to Rybelsus: Start with 7 mg or 14 mg orally once daily, up to 7 days after the last Ozempic injection. There is no equivalent oral dose for the 1 mg Ozempic dose.
2 notes
·
View notes
Text
Semaglutide for weight loss - What you need to know
①.What is Semaglutide?
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that helps to regulate appetite and insulin. It works by stimulating GLP-1 receptors in the brain, which causes the body to feel full after eating smaller portions of food. It also helps reduce fat levels in the body by increasing insulin sensitivity, helping to control blood sugar levels. It is the first FDA-approved drug since 2014 for chronic weight management in overweight adults or adults with general obesity.
②.Here are five reasons to consider semaglutide for weight loss.
1.Semaglutide helps you lose weight gradually and safely.
Semaglutide works by reducing your hunger and cravings by lowering your appetite and slowing down digestion, making it easier for you to stick to a low-calorie diet. It also helps reduce the amount of fat stored in your body, leading to gradual and safe weight loss.
2. Semaglutide can help you keep the weight off.
Unlike other weight loss medications, which only work while they’re in your system, semaglutide has been shown to promote lasting weight loss by helping you stick to a healthy diet and lifestyle even after discontinuing the medication.
3.Semaglutide helps improve metabolic health.
In addition to helping you lose weight, semaglutide also reduces your risk of developing type 2 diabetes by improving your body’s ability to use insulin, as well as reducing inflammation and cholesterol levels.
4.Semaglutide is generally well-tolerated.
Most people who take semaglutide experience minimal side effects, such as nausea, headache, and constipation. The most common side effects are usually mild and can often be managed with lifestyle modifications or over-the-counter medications.
Please click to learn more.https://www.polypeptide.ltd/
#weight loss#semaglutide#peptides#health#drug blog#injection#benefits#type 2 diabetes#exercise#healthcare#insulin
3 notes
·
View notes