#that its HIGHLY comorbid
Text

short comic about not knowing you have anxiety until year 22 of ur life
#anxiety#the thing about adhd is#that its HIGHLY comorbid#and when ur doctor tells u that#you go ‘oh but not me though’#heres the thing.#it probably Is you#comic#comics#neurodivergent#adhd#this is not necessarily about centaurworld it just happened to be the thing. lots of showtunes ect ect. any ‘#any ‘cringe’ media#this is also v similar to RSD#& the whole. anyway you get it im tired of typing lmao
473 notes
·
View notes
Text
I think I’m gonna headcanon Subaru as ADHD precisely because of the sweet tooth thing now. Also that’s one more thing he’ll have in common with Yuni
#he's probably not normal anyway#he takes on everyone's expectations and must be the best and get ppl's recognition and approval?#the flip side of rsd#(avoiding rsd; and/or whatever its opposite was called - recognition responsive euphoria?)#(which okay they're both their own separate disorders but they're highly comorbid w adhd bite me i'm counting it)#he NEEDS ppl to like him but also his people-pleasing nature makes ppl like jun not like him (tho jun did come around)#also there's that whole needing an excess of pressure in order to do something#it's just mostly (or at least mostly talked about) w a deadline while it isn't here#his recklessness#he has a voice of reason he just doesn't care to listen to it. if he's never broken any bones it's a minor miracle#maybe he's audhd or something else along w the adhd#he's just the type where ppl might think you're a little weird/different but you mostly fly under the radar#def don't get diagnosed until adulthood if at all. you don't suspect no one else suspects#'oh well he's a volleyball genius - of course…' 'oh well he's mimura subaru - of couse…'#don't think about how that plays into the whole deification (aka 'not human') thing#2.43 seiin koukou danshi volley bu#mimura subaru#2.43#ebw.op
0 notes
Text
Female reproductive health terms you should know!
(terfs not welcome)
Dysmenorrhea: Period pain that isn't normal, i.e. any pain more than Mild cramping.
Dyspareunia: painful intercourse
Oligomenorrhea: lighter, shorter menstrual flow.
Menorrhagia: heavier, longer menstrual flow.
Ovarian cysts: a mass on or in one's ovary, can be resolved on its own, or can remain and cause complications such as a rupture.
Polycystic ovary syndrome: a chronic condition causing cysts to reoccur on the ovaries and enlarging them. Symptoms include:
Irregular periods
hormonal imbalance
facial hair
weight gain
painful periods/ ovulation
infertility
People with PCOS are at higher risk for endometrial cancer, type II diabetes heart problems and high blood pressure.
Endometriosis: A chronic condition in which a tissue similar to, but different than, the endometrial lining grows outside of the uterus instead of inside. During menstruation this tissue sheds and has nowhere to go, thus irritating surrounding organs.
Symptoms include:
Irregular periods
Dysmenorrhea
Widespread pain
Painful ovulation
Vomiting, fainting, chills, sweating, fever and brain fog during menstruation
Infertility
Severe bloating
This also puts people at a higher risk for endometrial and ovarian cancer. There are four stages to Endo as it is a progressive disease, with 3/4 being more severe. The average time it takes to be diagnosed is 7 years.
Adenomyosis: A chronic disease similar and comorbid to endometriosis in which a tissue similar to the endometrial lining grows inside of the uterine wall. Symptoms are nearly identical to endometriosis but more difficult to detect.
Many people are diagnosed post menopause, by fault of the medical system, but it can and does develop much before then.
Ovarian cancer: cancer of the ovary(ies).
Endometrial cancer: cancer of the endometrium, the inner lining of the uterus.
Endometrial cyst, or chocolate cyst: cystic lesions from endometriosis.
Tilted uterus: the uterus is positioned pointing towards the back or severely to the front of the pelvis instead of a slight tilt towards at the cervix. Can cause painful sex and periods.
Pelvic floor dysfunction: inability to control your pelvic muscles. Comorbid with many things and is highly comorbid with endometriosis. Can cause pain and incontinence.
Vulvodynia: chronic and unexplained pain at the opening of the vagina.
Interstitial cystitis: a chronic condition where cysts form on the inside of the bladder and urinary tract and cause symptoms similar to that of a UTI.
Pre-eclampsia: a condition occurring in pregnancy where the blood supply between the fetus and the pregnant person is affected and can cause irregular blood pressure, swelling, and in more severe cases headache, nausea and vomiting, a burning sensation behind the sternum, shortness of breath and potentially death if untreated.
Endometritis: an infection or irritation of the uterine lining. Is not the same as endometriosis and is treatable but can cause pain, bleeding, swelling, general discomfort and fever, and more.
Pelvic inflammatory disease: an infection of the reproductive organs
Ectopic pregnancy: a pregnancy that is attached to the outside of the uterus. Can be fatal if left untreated.
There are many more I could probably add but if you see something missing, please add it!
#reproductive health#endometriosis#adenomyosis#pcos awareness#reproductive health awareness#chronic illness#polycystic ovarian syndrome#ovarian cancer#reproductive rights
180 notes
·
View notes
Text
i'm on my aspd izaya bullshit again but like. thru this lens, isnt his arc a perfect encapsulation on how aspd negatively affects the person that has it? even to this day, many professionals do not believe that pwASPD suffer from aspd. like at all. to the point where aspd was specifically listed as an outlier to the "patient distress is what defines a disorder" rule in an abnormal psych textbook
(see why i don't respect the field?)
but... he does suffer! a lot! like- remember his speech to mikado at the end of the first arc? how you need to keep evolving, keep changing in order to escape the mundane? how you have to keep going and going and going, wether it be aiming high or low?
yeah. normal people don't need to do this, izaya. you are a broken person.
but why SHOULD he be content with the mundane? the things people usually have that make them content with daily life- friends, family, a purpose, a distinct lack of extreme chronic boredom that drives you to do completely insane shit- izaya doesn't HAVE any of that!
"wait, chronic boredom?" i hear yall thinking. maybe. "isnt that an adhd thing?"
more than one disorder can have the same symptom. theres like a billion that have "want to die" as a symptom. but i dont really blame you for not knowing, its not talked about much
studies have shown that aspd and adhd are both problems with the dopamine receptors in the brain. more specifically, adhd is a chronic deficiency of dopamine, whereas with aspd, when you DO get dopamine, your brain gives you quardruple the normal amount.
studies have ALSO shown there to be a sort of... adhd to aspd pipeline. the story goes like this: you have a kid with adhd. maybe they're born like that, maybe the symptoms developed from trauma (which can happen? apparently??) anyway. kid gets abused. kid develops conduct disorder as a result of that abuse, as a natural extension of the existing adhd symptoms. they're MORE impulsive, which leads to them hurting others- and if it sets off the dopamine receptors, an abused kid starving for happiness and power is gonna chase it, no matter what. theyre like, six, they dont know anything about like. morality. all they know is, theyre sad and this makes them happy. anyway kid never gets treated, abuse continues to exasperate the symptoms, and now you have an adult with aspd, AND the original adhd diagnosis! and ptsd, which is HIGHLY comorbid with aspd! and probably another personality disorder, because you're actually statistically more likely to have two of them!
anyway! that's ONE of the ways aspd can develop from trauma, which it is Known To Do.
does any of that sound pleasant to go through? at all?
let me ask you a question:
imagine you aren't getting dopamine. maybe it's your adhd. maybe you're depressed. either way, you try to get it any way you can. wether it's throwing yourself into a hobby or a job, so the sense of satisfaction gives you dopamine, or something like drugs or gambling.
now, imagine that "rush" you felt. was Four Times Stronger.
wouldnt that compel you to do increasingly dangerous and risky shit, just to feel okay? imagine if you had no friends. imagine if this was your only way to be happy. wouldnt you, eventually, stop caring about others and only care about yourself? after all, other people have thinga like friends and a family that you don't have. they have a fallback. you only have this.
and you might say, "i'd never do that!" but every addict says that, and most eventually cross that line out of sheer desperation. and this? effectively makes you into a dopamine addict. which is dangerous! you can't just STOP... gettng dopamine....! it's necessary! but you have no help so you keep doing what youre doing. (and how could you get help? its baked into the system that people like you don't suffer. why try if youll just get burned?
anyway, back to izaya.
he's lonely. he has one friend and he sucks. he feels compelled to do these things even though he KNOWS it'll hurt him.

i stole this screenshot from some1 who insulted my friend once for something stupid <3 die
but it illustrates my point very well! does it look like he has much control over things?? he sure like to ACT like he does, but at the end of the day, he doesn't, really. he ends up spiraling more and more, doing increasingly risky and rash things, just to get his end goal... which is to die and ascend to the afterlife. a lofty goal.
aiming high, isn't he? a final, spectacular evolution.
or, it should have been.
but it wasn't.
izaya's impulses and deep desire to continue becoming more and more drastic, coupled with his lack of personal ties to anyone that could keep him from doing so....
it didn't make him ascend. it left him in a wheelchair, with chronic pain that will last his whole life.
THAT is where mental illness takes you. it doesn't make you a hollywood psychopath, reveling in the destruction you chose, of your own free will, wholly and truly, to cause. it makes you want More. no matter what, you need More. you see people content with lives worse than yours, everyone bound together with some sort of invisible thread, some sort of tie that keeps them together. a thread that missed you. your brain refuses to see people as people, thus you remain lonely forever, unsatiafied wirh company other than the superficial, because it's fun. that's all you're allowed to care about. an endless cycle of bigger and bigger actions, impulses slowly getting worse--
--and the worst part is, it tricks you into believing you ever had a choice. it tricks everyone into believing you had a choice. your suffering is worse than disregarded, to all the people you look at from your apartment, all the people you wish you could have been like.
it's nonexistant.
#durarara#izaya orihara#orihara izaya#🔥🔥 BE FUCKING NORMAL ABOUT ASPD ON THIS POST OR I SWEAR TO GOD I WILL BECOME THE JOKER ON YOUR ASS 🔥🔥#waposts#we r back with classic waposting complete w too many parentheses and paragraph breaks#peace and love on planet tumblr
115 notes
·
View notes
Text
So I've read a majority of the cass review now, and it definitely feels... weird? But that also could be that I'm not in research circles and the way in which things were expressed is simply a culture difference. However, I did find a lot of odd conclusions that seemed contradictory and a few items they used as a reference were generally extremely poor quality, such as the anonymous social-media shared survey on detransitioning. It felt like they were more critical of studies that produced pro-trans studies than of those that produced findings that agreed with their conclusions, but this may have been my own biases, so it's hard to say. It does repeatedly seem to associate that being trans is associated with mental health issues without much contextual references to the fact that living the trans experience being one that can cause those issues, and while it mentioned that dutch reports showed a lower incidence of comorbidities, it entirely failed to mention the culture differences that would result in trans youth in a more accepting area having fewer mental health issues, which... Idk, that feels worth mentioning in a section devoted to discussing the occurrence of gender dysphoria in youth and its high relation to mental health issues. It claimed that trans youth have a normal suicide rate 'when accounting for comorbidities," but only lightly discusses the source of those in relation to being trans. It also seemed weirdly highly focused on trans men, expressing over and over about how their numbers are increasing in extremely high numbers, but when information is compared to trans women, the numbers are relatively equal, so it's more about the amount of recent trans men than about the total numbers which feels weird. In some ways it does encourage better practices going forward, it's not wrong in the idea that transition is a really rough period for people, and mental health should be a standard practice of care alongside it, but it states that the mental health issues should be addressed prior to receiving any care, which feels particularly weird given its omission to the possible reasons for dutch comorbidities being so much lower as that has genuinely large implications for the rest of the fucking paper. It did seem weirdly obsessed with the ability of trans men to give birth, I'm not sure what's up with that.
Also learned that according to a study in 2011, autism made me gay, and they also had a chart about how social media causes depression, which I'll share below because it seems so simplistic as to be funny.

Do understand that this isn't my field, while I'm somewhat knowledgeable on the topic, I wouldn't take my interpretations as fact because I just do not have the experience to fully interpret the tone and content of this report. If you know anyone who does, I'd love to hear their take on it.
In trying to understand this report originally I went to news sources, and that was a fucking mistake, but I did get to hear some politician fear mongering about "Nearly 5000 trans youth this year!" (13-18) so I spent a few seconds to look up the total UK population 13-18, and it's ~3.65m, making this about .1% of the youth population in the UK. For context, on any given night, roughly 3500 UK youth experience unaccompanied homelessness.
14 notes
·
View notes
Note
Maladaptive daydreaming is likely in most cases a symptom of something else, rather than a standalone disorder.
What does that even mean though?
Where's the line between a symptom and a disorder? Delusions are symptoms of many psychotic disorders, but delusional disorder is still its own thing if that's the only symptom.
One could argue then that DID shouldn't be a disorder because it's closely associated with PTSD.
A lot of disorders were previously considered part of other disorders until they weren't. Compulsive Hoarding for instance used to be thought of as a symptom of OCD, for instance.
When exploring the comorbidity of Maladaptive Daydreaming, it was found that it was highly comorbid with ADHD and anxiety disorder with upwards of 70% for both, but I'd argue these aren't quite enough to say the maladaptive day dreaming is caused by either.
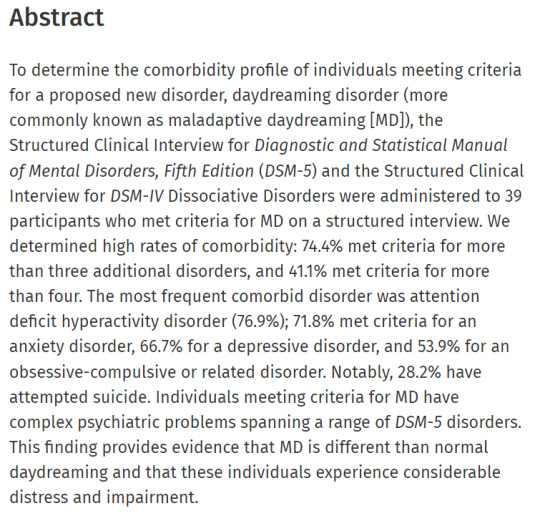
Not to mention that, while this might sound high, there are studies showing DID with a comorbidity with depression of 100%. (Granted, it was a small study with 14 people.)
Personally, I think there's a very strong case to be made that maladaptive daydreaming should be added to the DSM-6 as its own unique disorder.
#maladaptive daydreaming#mental health#psychiatry#psychology#mental illness#mental disorders#dsm#dsm 5#dsm v#madd
8 notes
·
View notes
Text
Making this its own post actually - I can't help but notice that some people, despite picking up on support needs language over functioning language...still can't get past the high-functioning/low-functioning dichotomy and judge it in others based solely on outward signs and just use "support needs" language as a synonym for the same flawed concept.
Like, compare two autistic people; many people will look at someone whose internet posts use choppy, "awkward" grammar and go "ah, high support needs!"...even if it turns out that a little bit of patience with communication difficulty is damned near the ONLY support need they have. Conversely, I'm "well-spoken" and don't have many strong, hard-to-avoid sensory aversions, the only real "typical" one I have is fluorescent lights and I'm pretty okay at masking that one most of the time; in fact I'm more inclined to seek stimulation than to avoid it, so...you hear I'm autistic, and, ah, low support needs, I only need to Buy Product (fidget toys, weighted blankets, chew jewelry, MAYBE earplugs for when euphoric overstimulation stops being euphoric) and I'm basically 100% abled! Right?
Nope! My interroception is basically nonexistent until a bodily need becomes immediately urgent and physically painful. I have almost every physical comorbidity in the book; generalized chronic pain, stomach issues, hypermobility, the works - and when my dyspraxia combines with my hypermobility, the result is me being so injury-prone that it's not even misleading to say I've been an on-and-off mobility aid user for nearly as long as I've been walking. Combine that with my lack of interroception making it hard for me to judge when I'm fatigued, and it's even worse. Sure, I have lots of highly-valued skills, both physical and intellectual; I'm an engineer, I fucking love designing and building things and do it on a personal and occasionally freelance basis, I get in the ZONE - but I can't get a steady long-term job with those skills because I'm very limited in how long I can do it for both mental and physical reasons, and no one around me wants to hire an engineer or welder or machinist or forklift operator or anything like that for a 16-hour max week, and many of the seemingly very few intense sensory aversions I do have are found in those environments (e.g., working with metals often means exposure to fire brick my beloathed) and way harder to deal with in a professional environment than on my own terms, and did I mention being ridiculously injury-prone? There are aspects of personal care I struggle with, and "cosmetic" procedures that would probably dramatically improve my life, for sensory reasons. My face-to-face social skills are...garbage, despite me having a strong interest in communication as a compensation Thing; I can fake my way through a conversation but I'm usually screaming on the inside, overthinking everything, for absolute terror that I'm getting a bad grade at human interaction, which REALLY sucks because I'm actually more extroverted than introverted, I want to spend time with people, I want to socialize more...but my brain is just out to kneecap me all the time. This isn't even getting into the ADHD side of things or other physical issues. In short, I outwardly seem...pretty "normal" even when only masking one (1) item, but in my private life...I hate to admit it sometimes because it makes people dismiss everything else I have to say, but I don't really function well. I'm lucky to have understanding people in my life, because the likely alternative for me would be, at best, moving back in with my parents for the rest of their lives, and at worst (or probably after that), an institution.
...really didn't think this was how my life would go, but the fact that no one expects someone with my strengths to have my needs, not even me until just a few years ago, well, that's part of WHY it is what it is.
Like. People like me, or indeed that fairly common other theoretical guy who prominently struggles with communication but not much else, are WHY we jettisoned high-functioning/low-functioning labels in favor of discussing support needs. "Low support/high support" wasn't supposed to be just a less clinical synonym for the exact same externally judged concept of how well someone can pass for abled and/or perform a function valued under capitalism.
Tl;dr: yes you've stopped using "functioning" LANGUAGE, but have you stopped THINKING of support needs in "high-function/low-function" terms?
#disability#serious tag#ill probably stop for now but i mean. i guess this is the month for disability seriousposting isnt it
47 notes
·
View notes
Note
Hello! (So sorry if this was asked several times, the page kept glitching and I wasn’t sure if it was sent)
I was curious about what mental/physical conditions the characters have, if any. (Of course, for some it’s somewhat obvious, but for others it’s a little less clear, so I just wanted to check)
Hope you have a lovely day/night! :)
It only sent the ask once, don't worry!
I'm assuming by the characters, you mean SCP-6118 and other keplers. And I would be more than happy to answer :)
Content warning for mentions of addiction, self-harm, and suicide.
In order of chronological appearance as per the Altitudes Hub:
Unit 5a82 / SCP-6118
Mentally, I'd say SPD (Schizoid Personality Disorder) and PTSD for absolute certain. (I plan to write more about them as well, though the latter has been touched on a lot already.)
He dealt with a self-harm addiction for an extensive period of time, on and off for some years to not get in the way of intensive physical training (as much as possible). He struggles with suicidal thoughts throughout the story, though never really acts on it, more like throwing himself into severe harm's way on purpose.
I've also seen people interpret him as having ADHD &/or ASD, though I've found this is highly dependent on the person reading him. I'm sure some of my own has unintentionally bled out onto the page so to speak.
Physically, he's albino and would probably qualify for a diagnosis of dwarfism. He has chronic pain and fatigue, mostly global and musculoskeletal related. In an upcoming Tale I plan to touch on more severe neurological issues like acephalgic (aura-only) migraines (why he gets nauseous when he's stressed) and perhaps cardiac issues.
Some kind of hormonal/gonadal difference or DSD like undervirilization could also easily be assumed.
-
The Handler
It has BPD (Borderline Personality Disorder) and a comorbid substance abuse disorder, as a way of self-medicating for the horrible and debilitating symptoms it has.
It also has ectodermal atrichia congenita, meaning it has absolutely no hair on its body, and never did. Otherwise it's physically unremarkable besides for having lighter skin and eyes (not to the point of albinism), and being slightly smaller than normal for a Two.
-
Unit 4b80
It struggles with survivor's guilt after everything it went through, and other guilt, just guilt all around.
Possibly some OCD behaviours as well, related or otherwise, but nothing concrete has been written so far about it.
-
Unit 7cb7
It has chronic pain-- mostly nerve pain-- in its lower limbs after losing them in the explosion, because while regen tanks can do an enormous amount, when regenerating that much tissue, it can be tricky to get all the nerves in the right place.
Also chronic fatigue, because bodies hold on to traumatic events (whether physically traumatic to the body or mentally/emotionally) and getting blown up is a really physically traumatic thing.
I've been pondering 7cb7 having below-knee prosthetics, but it hasn't become relevant in my writing yet.
-
Units 3f32 & 3f33
They are identical twins due to a mishap in the gestational process where the cloned cells doubled and divided into two organisms. Other than being slightly tall and more towards the hyperpigmented side, they're in surprisingly sound mental and physical health for Twos who joined the rebellion a while back.
-
That should be most of it. Feel free to send me additional asks with any follow-up questions (or comment/reblog this post). I know it was quite a wall of text, but I wanted to touch on all of the things.
I hope whatever time of day it is for you, it's going well! Thank you so much for the ask!
#ask response#kepler aliens#scp 6118#scp writing#informative#disabled characters#I saw the parched savanna of disability representation in the SCP community and watered it with my tears#Or something#I'm loopy
10 notes
·
View notes
Text


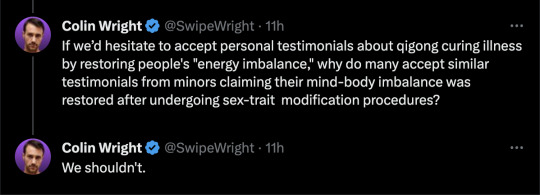

By: Colin Wright
Published: Aug 28, 2023
One might think the fact that the medical establishment is endorsing and performing experimental, irreversible, and often sterilizing medical procedures on children would be an immense journalistic discovery. But a recent New York Times article—investigating allegations made by Jamie Reed, a former case manager at the Washington University Transgender Center at St. Louis Children’s Hospital who blew the whistle on medical malpractice at the clinic traveling under the guise of “gender-affirming care”—downplays the results of that discovery in a way that privileges personal testimony over evidence.
Reed’s allegations were numerous. She claimed that the clinic was inundated with requests for transition services without adequate protocols to handle them, that patients were hastily approved for transitioning despite notable mental-health comorbidities, that individuals were not fully briefed on the risks and side effects of their prescribed medications, and that any opposition within the clinic was quelled. As Leor Sapir observes, the Times investigation corroborated most of Reed’s claims. A discerning reader who cuts through the article’s euphemisms and sidesteps the author’s political asides would discern as much.
Indeed, the newspaper of record has verified concerns that critics of “gender-affirming care” have raised for years. The current influx of trans-identified youth, primarily girls with no previous gender-related distress, symbolizes a fresh patient group exhibiting a new and as-yet-unstudied form of gender dysphoria. Gender-affirming care is experimental, with no long-term, rigorous studies demonstrating its advantages over the many obvious risks.
Yet throughout, the Times article alludes to the realities of pediatric gender medicine, while simultaneously obscuring them. Consider some representative quotes.
[A]ccording to an internal presentation from 2021, 73 percent of new patients were identified as girls at birth. Gender clinics in Western Europe, Canada and the United States have reported a similarly disproportionate sex skew that has bewildered clinicians.
Here, the Times concedes that the children currently fueling the unprecedented surge in gender-clinic referrals differ significantly from the group (natal males) that the original, ostensibly more cautious, “Dutch protocol” for pediatric sex-trait modification was intended to serve. As a Reuters investigation recently revealed, U.S. gender clinics aren’t adhering even to the Dutch approach. Instead, they’re adopting a less rigorous, highly medicalized “gender-affirming” model, which entails automatic social transition and on-demand puberty blockers, cross-sex hormones, and surgeries. Considering that this form of gender dysphoria is new and rapid, it would seem prudent to gather more data about its possible causes before offering medical interventions.
Pediatric gender medicine is a nascent specialty, and few studies have tracked how patients fare in the long term, making it difficult for doctors to judge who is likely to benefit.
This dramatic understatement amounts to an admission that the current practice of “affirming” a child’s cross-sex identity with hormones and surgeries is completely experimental. It follows that advocates’ claims that such interventions are beneficial or “life-saving” are not based on any high-quality research. Those who have meticulously monitored the data have been aware of this from the beginning, and systematic reviews conducted in Sweden, Finland, and the U.K. support this view. Yet, despite such evidence, U.S. medical organizations, including the American Academy of Pediatrics, have obstinately maintained a pro-affirmation stance.
It’s clear the St. Louis clinic benefited many adolescents: Eighteen patients and parents said that their experiences there were overwhelmingly positive, and they refuted Ms. Reed’s depiction of it.
This particularly jarring statement showcases the post hoc, ergo propter hoc (“after this, therefore because of this”) fallacy: it presumes a causal relationship between phenomena merely because one follows the other. Being cautious of this fallacy, especially in the realm of human health, is fundamental to evidence-based medicine.
Few deny that many individuals are genuinely satisfied with the results of their hormonal or surgical transition. I’ve heard heartfelt accounts from minors stating that their mental well-being improved after gender-affirming treatment, and I don’t question their sincerity. However, modern medicine doesn’t—or shouldn’t—gauge the success of a treatment based purely on a patient’s personal testimony. Without comprehensive long-term-outcomes data and controlled experiments—which Ghorayshi acknowledges do not exist—it remains impossible to know whether the “positive” outcomes mentioned by the patients she references flow from the gender-affirming procedures or if the same contentment could have been achieved without resorting to body-altering hormones and surgery.
The Times article inadvertently suggests the importance of evidence-based medicine. Evaluating the effectiveness of a drug or surgery solely based on patient satisfaction constitutes a significant departure from its fundamental objectives. Were observers to start taking personal testimonies as sufficient evidence for the success of a medical treatment, the FDA would become obsolete. We’d all be forced to embrace the extravagant and pseudoscientific assertions of any self-styled health guru or medical quack.
Compare the use of testimony to support gender-affirming care at the St. Louis hospital with the Minnesota-based “healing center” known as Spring Forest Qigong (SFQ). SFQ champions the use of an ancient Chinese ritual called “external qigong” to heal the afflicted. According to its website, illnesses, or “dis-eases,” as they are fancifully labeled, are the result of “energy blockages within the body.” SFQ asserts that qigong is the magical wand that dispels these obstructions, thereby restoring the body’s “natural balance.” This involves the enigmatic Qigong Master Chunyi Lin waving his hands over one’s body, channeling energies and dissolving said blockages. If the idea of driving all the way to Minnesota for treatment seems tedious, fear not: Master Lin generously offers to transmit these energies and conduct qigong sessions over the phone.
The SFQ site provides links to several “scientific” articles from the Journal of Holistic Nursing and The American Journal of Chinese Medicine. These papers, apparently, endorse external qigong as an antidote for chronic pain. But for novices to the mystical realm of SFQ and qigong, the site offers glowing testimonials from satisfied SFQ customers.
One says: “I’ve tried different medicines. They gave relief but didn’t cure me. This season I’ve lived allergy free and I credit it to the [Spring Forest Qigong] Active Exercises I've been doing [for the past six months]. I didn’t take even one pill. Since there weren’t any other changes in my lifestyle, diet, or anything, I credit the [SFQ] active exercise. Channels were cleared, immune system adjusted and here I am, happy and allergy free.”
Another: “I was breathing into the shoulder and seeing the pain turn to air or smoke each night before I went to sleep, and it got better and better and better. I went back to the doctor months later and showed him the improvement. He said, ‘There is no way you should be able to do what you’re doing. You should be in excruciating pain. I can’t explain how you can do it, but whatever you’re doing, don’t stop.’”
Still another: “Chunyi Lin and Spring Forest have had an amazing impact on my life. It’s given me a way to live life more fully, happier. To me it’s a God send. The practice of Qigong is something everyone can benefit from. Once you have had an experience with Qigong you want to keep it a part of your life.”
One woman even says that qigong eradicated her Stage 4 breast cancer: “I rejected conventional cancer treatments from your classically trained oncologists because they didn’t work the first time. This time it was my life that hung in the balance and I was resolved to find alternative measures to find healing. And, fast forward, after six, seven months of both medical treatments and visiting with Master Lin in the Spring Forest Qigong Center I am completely healed. My cancer’s gone. My doctors call me a ‘walking miracle.’”
Should doctors and scientists view these “overwhelmingly positive” experiences as clear proof that Qigong Master Chunyi Lin healed these patients by simply waving his hands over their bodies (or through the phone) to dispel their energy blockages? Should we confidently endorse external qigong for people with Stage 4 breast or liver cancer? Probably not. Instead, we’d likely advocate for rigorous testing of external qigong through randomized control trials, demanding tangible evidence of its benefit before suggesting it could treat even minor ailments.
But if we’d be hesitant to accept these testimonials about how qigong cured some people’s energy imbalance, then why are many political progressives so quick to accept similar testimonials from minors who claim their mind-body imbalance was corrected after undergoing sex-trait modification procedures? Why is such testimony taken as definitive proof of these procedures’ benefits? Ideology couldn’t possibly be the reason—right?
==

By the way, this is intentional. It's part of the postmodern goal of deconstructing objective reality.
#Colin Wright#sex trait modification#genderwang#gender ideology#queer theory#medical scandal#anecdotal evidence#argument from anecdote#anecdote#Qigong#external qigong#alternative medicine#religion is a mental illness
16 notes
·
View notes
Text
Samantha Crafts Unofficial Autism Checklist for AFAB's
I just came across this resource and though I would share it. All but maybe 2 of these things apply to me and it is very validating/eye-opening.
A couple disclaimers:
1. This is not a diagnostic tool, its the result of an Autistic persons gathering and compiling the lived experience of Autistic afabs and so it may be valuable in a clinical setting as well as in ones personal journey.
2. Any reference to intelligence is not exclusive to IQ or academic capabilities or acheivement
3. Craft uses she/her pronouns in this work but as an afab agender person I believe it is relevant to most if not all afab people on with autism (self diagnoses included). I will leave it up to trans women and trans feminine people to decide how relevant it is to them.
4. Craft has historically used the term Aspergers and has a book including that word, she seems to have made some attempts to adjust her language in the present but is choosing not to do so retroactively. This choice does not align with my values and I have taken pains to make sure the version here excludes that language. If one got through, I apologize.
~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~~
(Section A consideration/prolific artist in place of writer and/or both.)
Section A: Deep Thinkers
A deep thinker
A prolific writer drawn to poetry
*Highly intelligent (Highly intelligent does not relate to IQ levels. Autistic individuals are often dyslexic and have dysgraphia and other learning disabilities but can be highly intelligent about particular subject matters, out-of-the-box thinking, and verbal fluency/fluid intelligence capacities.)
Sees things at multiple levels, including her own thinking processes
Analyzes existence, the meaning of life, and everything, continually
Serious and matter-of-fact in nature
Doesn’t take things for granted
Doesn’t simplify
Everything is complex
Often gets lost in own thoughts and “checks out” (blank stare)
Section B: Innocent
Naïve
Honest
Experiences trouble with lying
Finds it difficult to understand manipulation and disloyalty
Finds it difficult to understand vindictive behavior and retaliation
Easily fooled and conned
Feelings of confusion and being overwhelmed
Feelings of being misplaced and/or from another planet
Feelings of isolation
Abused or taken advantage of as a child but didn’t think to tell anyone
Section C: Escape and Friendship
Survives overwhelming emotions and senses by escaping in thought or action
Escapes regularly through fixations, obsessions, and over-interest in subjects
Escapes routinely through imagination, fantasy, and daydreaming
Escapes through mental processing
Escapes through the rhythm of words
Philosophizes, continually
Had imaginary friends in youth
Imitates people on television or in movies
Treated friends as “pawns” in youth, e.g., friends were “students” “consumers” “members”
Makes friends with older or younger females more so than friends her age (often in young adulthood)
Imitates friends or peers in style, dress, attitude, interests, and manner (sometimes speech)
Obsessively collects and organizes objects
Mastered imitation
Escapes by playing the same music over and over
Escapes through a relationship (imagined or real)
Numbers bring ease (could be numbers associated with patterns, calculations, lists, time and/or personification)
Escapes through counting, categorizing, organizing, rearranging
Escapes into other rooms at parties
Cannot relax or rest without many thoughts
Everything has a purpose
Section D: Comorbid Attributes
OCD (Obsessive Compulsive Disorder)
Sensory Issues (sight, sound, texture, smells, taste) (might have synesthesia)
Generalized Anxiety
Sense of pending danger or doom
Feelings of polar extremes (depressed/over-joyed; inconsiderate/over-sensitive)
Poor muscle tone, double-jointed, and/or lack in coordination (may have Ehlers Danlos Syndrome and/or Hypotonia and/or POTS syndrome)
Eating disorders, food obsessions, and/or worry about what is eaten
Irritable bowel and/or intestinal issues
Chronic fatigue and/or immune challenges
Misdiagnosed or diagnosed with a mental illness
Experiences multiple physical symptoms, perhaps labeled “hypochondriac”
Questions place in the world
Often drops small objects
Wonders who she is and what is expected of her
Searches for right and wrong
Since puberty has had bouts of depression (may have PMDD)
Flicks/rubs fingernails, picks scalp/skin, flaps hands, rubs hands together, tucks hands under or between legs, keeps closed fists, paces in circles, and/or clears throat often
Section E: Social Interaction
Friends have ended friendship suddenly (without female with AS understanding why) and/or difficult time making friends
Tendency to overshare
Spills intimate details to strangers
Raised hand too much in class or didn’t participate in class
Little impulse control with speaking when younger
Monopolizes conversation at times
Brings subject back to self
Comes across at times as narcissistic and controlling (is not narcissistic)
Shares in order to reach out
Often sounds eager and over-zealous or apathetic and disinterested
Holds a lot of thoughts, ideas, and feelings inside
Feels as if she is attempting to communicate “correctly”
Obsesses about the potentiality of a relationship with someone, particularly a love interest or feasible new friendship
Confused by the rules of accurate eye contact, tone of voice, proximity of body, body stance, and posture in conversation
Conversation are often exhausting
Questions the actions and behaviors of self and others, continually
Feels as if missing a conversation “gene” or thought-filter
Trained self in social interactions through readings and studying of other people
Visualizes and practices how she will act around others
Practices/rehearses in mind what she will say to another before entering the room
Difficulty filtering out background noise when talking to others
Has a continuous dialogue in mind that tells her what to say and how to act when in a social situation
Sense of humor sometimes seems quirky, odd, inappropriate, or different from others
As a child it was hard to know when it was her turn to talk
Finds norms of conversation confusing
Finds unwritten and unspoken rules difficult to grasp, remember, and apply
Section F: Finds Refuge when Alone
Feels extreme relief when she doesn’t have to go anywhere, talk to anyone, answer calls, or leave the house but at the same time will often harbor guilt for “hibernating” and not doing “what everyone else is doing”
One visitor at the home may be perceived as a threat (this can even be a familiar family member)
Knowing logically a house visitor is not a threat, doesn’t relieve the anxiety
Feelings of dread about upcoming events and appointments on the calendar
Knowing she has to leave the house causes anxiety from the moment she wakes up
All the steps involved in leaving the house are overwhelming and exhausting to think about
She prepares herself mentally for outings, excursions, meetings, and appointments, often days before a scheduled event
OCD tendencies when it comes to concepts of time, being on time, tracking time, recording time, and managing time (could be carried over to money, as well)
Questions next steps and movements, continually
Sometimes feels as if she is on stage being watched and/or a sense of always having to act out the “right” steps, even when she is home alone
Telling self the “right” words and/or positive self-talk (CBT) doesn’t typically alleviate anxiety. CBT may cause increased feelings of inadequacy.
Knowing she is staying home all day brings great peace of mind
Requires a large amount of down time or alone time
Feels guilty after spending a lot of time on a special interest
Uncomfortable in public locker rooms, bathrooms, and/or dressing rooms
Dislikes being in a crowded mall, crowded gym, and/or crowded theater
Section G: Sensitive
Sensitive to sounds, textures, temperature, and/or smells when trying to sleep
Adjusts bedclothes, bedding, and/or environment in an attempt to find comfort
Dreams are anxiety-ridden, vivid, complex, and/or precognitive in nature
Highly intuitive to others’ feelings
Highly empathetic, sometimes to the point of confusion
Takes criticism to heart
Longs to be seen, heard, and understood
Questions if she is a “normal” person
Highly susceptible to outsiders’ viewpoints and opinions
At times adapts her view of life or actions based on others’ opinions or words
Recognizes own limitations in many areas daily, if not hourly
Becomes hurt when others question or doubt her work
Views many things as an extension of self
Fears others opinions, criticism, and judgment
Dislikes words and events that hurt animals and people
Collects or rescues animals (often in childhood)
Huge compassion for suffering (sometimes for inanimate objects/personification)
Sensitive to substances (environmental toxins, foods, alcohol, medication, hormones, etc.)
Tries to help, offers unsolicited advice, or formalizes plans of action
Questions life purpose and how to be a “better” person
Seeks to understand abilities, skills, and/or gifts
Section H: Sense of Self
Feels trapped between wanting to be herself and wanting to fit in
Imitates others without realizing it
Suppresses true wishes (often in young adulthood)
Exhibits codependent behaviors (often in young adulthood)
Adapts self in order to avoid ridicule
Rejects social norms and/or questions social norms
Feelings of extreme isolation
Feeling good about self takes a lot of effort and work
Switches preferences based on environment and other people
Switches behavior based on environment and other people
Didn’t care about her hygiene, clothes, and appearance before teenage years and/or before someone else pointed these out to her
“Freaks out” but doesn’t know why until later
Young sounding voice
Trouble recognizing what she looks like and/or has occurrences of slight prosopagnosia (difficulty recognizing or remembering faces)
Feels significantly younger on the inside than on the outside (perpetually twelve)
Section I: Confusion
Had a hard time learning that others are not always honest
Feelings seem confusing, illogical, and unpredictable (self’s and others’)
Confuses appointment times, numbers, and/or dates
Expects that by acting a certain way certain results can be achieved, but realizes in dealing with emotions, those results don’t always manifest
Spoke frankly and literally in youth
Jokes go over the head
Confused when others ostracize, shun, belittle, trick, and betray
Trouble identifying feelings unless they are extreme
Trouble with emotions of hate and dislike
Feels sorry for someone who has persecuted or hurt her
Personal feelings of anger, outrage, deep love, fear, giddiness, and anticipation seem to be easier to identify than emotions of joy, satisfaction, calmness, and serenity
Difficulty recognizing how extreme emotions (outrage, deep love) will affect her and challenges transferring what has been learned about emotions from one situation to the next
Situations and conversations sometimes perceived as black or white
The middle spectrum of outcomes, events, and emotions is sometimes overlooked or misunderstood (all or nothing mentality)
A small fight might signal the end of a relationship or collapse of world
A small compliment might boost her into a state of bliss
Section J: Words, Numbers, and Patterns
Likes to know word origins and/or origin of historical facts/root cause and foundation
Confused when there is more than one meaning (or spelling) to a word
High interest in songs and song lyrics
Notices patterns frequently
Remembers things in visual pictures
Remembers exact details about someone’s life
Has a remarkable memory for certain details
Writes or creates to relieve anxiety
Has certain “feelings” or emotions towards words and/or numbers
Words and/or numbers bring a sense of comfort and peace, akin to a friendship
(Optional) Executive Functioning & Motor Skills This area isn’t always as evident as other areas
Simple tasks can cause extreme hardship
Learning to drive a car or rounding the corner in a hallway can be troublesome
New places offer their own set of challenges
Anything that requires a reasonable amount of steps, dexterity, or know-how can rouse a sense of panic
The thought of repairing, fixing, or locating something can cause anxiety
Mundane tasks are avoided
Cleaning self and home may seem insurmountable
Many questions come to mind when setting about to do a task
Might leave the house with mismatched socks, shirt buttoned incorrectly, and/or have dyslexia and/or dysgraphia
A trip to the grocery store can be overwhelming
Trouble copying dance steps, aerobic moves, or direction in a sports gym class
Has a hard time finding certain objects in the house but remembers with exact clarity where other objects are; not being able to locate something or thinking about locating something can cause feelings of intense anxiety (object permanence challenges) (even with something as simple as opening an envelope)
End
This unofficial checklist can be copied for therapists, counselors, psychiatrists, psychologists, professors, teachers, and relatives if Samantha Craft’s name and contact information remain on the printout. This list was created in 2012 and updated in May 2016.
Disclaimer: This is one person’s opinion. It is not meant to replace the DSM-V Autism Spectrum condition definition, nor is this list meant to serve as an official diagnostic tool. 1000s and 1000s of individuals around the globe have used this list, in conjunction with the DSM-IV or DSM-V and a professional mental health professional’s guidance. It has been an important tool for females, particularly, but individuals across the gender spectrum identify with the list. The list has been translated into different languages. It is based on over 8 years of communicating, almost daily, with those that are diagnosed or self-diagnosed Autistic. It is not all-inclusive. Some will fit into categories and not be Autistic. This is meant as a springboard for discussion and more awareness.
Author’s Note: I am diagnosed as Autistic/gifted-intellect, and have dyslexia, dyspraxia, GAD, PTSD, hEDS, POTS, fibromyalgia, and other chronic pain conditions. I am not unusual in my presentation; many Autistic adults have many coexisting conditions. This post was originally composed when A***********s Syndrome was a stand-alone diagnosis. At that time, not much was written or discussed about females on the autism spectrum.
In 2022, I was diagnosed ADHD, OCD, and complex-PTSD.
#autism#neurodivergent#asperger was a nazi#hans asperger was a nazi#autism in women#autism in afab people#audhd#actually autistic#ocd#ocd awareness#queer autistic#agender#samantha craft
20 notes
·
View notes
Text
10 Surprising Facts About Eating Disorders
surprising facts about eating disorders.
The Most Common Eating Disorder: OSFED
1. The most common eating disorder diagnosis is “Other Specified Feeding and Eating Disorder” (OSFED). OSFED is a diagnostic category that captures disorders of eating that don’t meet the strict criteria for one of the primary eating disorder categories, like anorexia, bulimia or binge eating disorder. It’s fortunate that there is a diagnosis that represents the many different ways that disordered eating can present – because we know how varied and diverse all of our experiences can be and that people can be struggling even though their difficulties don’t fit neatly in a box.
2. Atypical anorexia nervosa is also a very common eating disorder diagnosis. Research shows that the psychological and medical characteristics of atypical anorexia nervosa and anorexia nervosa don’t differ. The only difference is the individual’s starting weight. Those with the diagnosis of atypical anorexia restrict their food intake, fear weight gain, and suffer the effects of weight suppression even though their body mass index (BMI) is considered by typical standards to be in a “healthy” range.
3. 8 out of 10 people with an eating disorder do not seek treatment. That means, 80 percent of people with eating disorders fail to pursue critical professional help. There are various reasons for this astounding statistic, including the stigma associated with eating disorders, limited access to treatment, inadequate resources, and lack of recognition of signs and symptoms.
The Annual Cost of Eating Disorders
4. Eating disorders cost individuals in the United States over 65 billion dollars per year. This number refers to the economic costs alone including treatment expenses and loss of work for both patients and caregivers/supports.
5. Children can develop eating disorders as young as ages 9 and 10. Previously, it was believed that the typical age of eating disorder development was 13 to 19. In recent years, sadly, this number has significantly shifted lower.
6. Picky eating in its extreme form may be considered an eating disorder. Also known as avoidant restrictive food intake disorder (AFRID), this condition was only recently recognized as an official eating disorder in the DSM. Of course, it’s common for children to be picky eaters, but in ARFID, the rigidity is severe and interferes with social functioning and/or normal, healthy growth and development.
More Surprising Facts About Eating Disorders
7. Restrictive diets are one of the strongest risk factors for developing an eating disorder. Diet culture is pervasive in our society. Don’t be fooled by intermittent fasting and other trending eating patterns. Despite the success stories you may hear, research tells us that 95 percent of diets fail. And we know that dieting is the most common gateway to developing an eating disorder. EDs often start with innocent efforts to “get fit” or “slim down.” Unfortunately, many people with eating disorders can trace the onset back to these early efforts that morphed into severe and debilitating conditions.
8. Disordered eating behaviors are often used to manage uncomfortable emotions. EDs are really not about thinness. Behaviors like restricting, binge eating, and purging serve an emotion regulation function, meaning that, in the short term, people can experience relief, avoidance, or escape from aversive emotion when engaging in these behaviors. For this reason, treatment often focuses on teaching skills for coping that are health-affirming and effective in lieu of using destructive behaviors that worsen quality of life.
9. 95 percent of individuals with eating disorders also have at least one other psychiatric illness, such as anxiety or depression. This astounding number means that clinicians who treat eating disorders also need to be highly skilled in treating these common comorbidities.
10. Eating disorders are one of the most deadly psychiatric illnesses. In fact, someone dies from an eating disorder every 52 minutes.
#10 surprising facts about eating disorders#eating disorder survivor#eating disorder awareness week 2023
12 notes
·
View notes
Text
Female reproductive health terms you should know!
Dysmenorrhea: Period pain that isn't normal, i.e. any pain more than Mild cramping.
Dyspareunia: painful intercourse
Oligomenorrhea: lighter, shorter menstrual flow.
Menorrhagia: heavier, longer menstrual flow.
Ovarian cysts: a mass on or in one's ovary, can be resolved on its own, or can remain and cause complications such as a rupture.
Polycystic ovary syndrome: a chronic condition causing cysts to reoccur on the ovaries and enlarging them.
Symptoms include:
Irregular periods
hormonal imbalance
facial hair
weight gain
painful periods
ovulation infertility
Women with PCOS are at higher risk for endometrial cancer, type II diabetes heart problems and high blood pressure.
Endometriosis: A chronic condition in which a tissue similar to, but different than, the endometrial lining grows outside of the uterus instead of inside. During menstruation this tissue sheds and has nowhere to go, thus irritating surrounding organs.
Symptoms include:
Irregular periods
Dysmenorrhea
Widespread pain
Painful ovulation
Vomiting, fainting, chills, sweating, fever and brain fog during menstruation
Infertility
Severe bloating
This also puts women at a higher risk for endometrial and ovarian cancer. There are four stages to Endo as it is a progressive disease, with 3/4 being more severe. The average time it takes to be diagnosed is 7 years.
Adenomyosis: A chronic disease similar and comorbid to endometriosis in which a tissue similar to the endometrial lining grows inside of the uterine wall. Symptoms are nearly identical to endometriosis but more difficult to detect.
Many women are diagnosed post menopause, by fault of the medical system, but it can and does develop much before then.
Ovarian cancer: cancer of the ovary(ies).
Endometrial cancer: cancer of the endometrium, the inner lining of the uterus.
Endometrial cyst, or chocolate cyst: cystic lesions from endometriosis.
Tilted uterus: the uterus is positioned pointing towards the back of the pelvis instead of sitting upright. Can cause painful sex and periods.
Pelvic floor dysfunction: inability to control your pelvic muscles. Comorbid with many things and is highly comorbid with endometriosis. Can cause pain and incontinence.
Vulvodynia: chronic and unexplained pain at the opening of the vagina.
Interstitial cystitis: a chronic condition where cysts form on the inside of the bladder and urinary tract and cause symptoms similar to that of a UTI.
Pre-eclampsia: a condition occurring in pregnancy where the blood supply between the fetus and the pregnant woman is affected and can cause irregular blood pressure, swelling, and in more severe cases headache, nausea and vomiting, a burning sensation behind the sternum, shortness of breath and potentially death if untreated.
Endometritis: an infection or irritation of the uterine lining. Is not the same as endometriosis and is treatable but can cause pain, bleeding, swelling, general discomfort and fever, and more.
Pelvic inflammatory disease: an infection of the reproductive organs
Ectopic pregnancy: a pregnancy that is attached to the outside of the uterus. Can be fatal if left untreated.There are many more I could probably add but if you see something missing, please add it!
#stole this because it said “terfs unwelcome” and the post originally said “pregnant people”.#TRAs gtfo
4 notes
·
View notes
Text
btw hot take but i think that the endogenic issue in general is also the fault of fake claimers who like to ignore how other disorders and illnesses interact w and affect systemhood. like a psychotic and autistic polyfragmented DID system will be substantially different than an OSDD system w anxiety ptsd and depression but that doesnt invalidate either system or their experience. like yes we also know a good portion of endos, especially in the early days, literally were just using it as a gotcha for being "better" or more valid or whatever else for not having icky trauma (!!!) but its also true that a lot of newly discovered or just young systems who do really. REALLY have trauma and a disorder that would bring about a system are being convinced they arent really a traumatized system, no theyre really endo. you know what most often causes these systems to fall into endo circles?? fucking fake claimers doing what they do and making people whos disorder already works to make you doubt having it question and doubt themselves and become more anti recovery (!!!!!) bc YOU think somehow that these many disorders (bc its not just DID and OSDD actually has many types so its not even one disorder ur fake claiming weirdos) are 100% cookiecutter so therefore everyone who experiences smth thats undocumented in a highly understudied handful of disorders that has almost no research into comorbidities or intersections w other disorders at all, is clearly faking it! every ex endo weve ever known has agreed that it was fakeclaimers who pushed them towards those ideals in the first place before they realized or were educated or w/e to get them out of those circles and away from the anti recovery mindset. and i dont think EVERY endo or even ex endogenic is like this obviously but my point is less systems would needlessly fall into anti recovery spaces in general if people used their damn brains to think for half a second that maybe you dont know everything. or to mind ur own business!
#i have hotter takes abt how different disorders interact w them as well but im openly a psycho so lol#dont want to be dismissed yet#syscourse tw#im NOY a syscourse blog this is just a personal blog im not accepting silly asks at this time#im just tagging this so i dont force beloved mutuals to wotness shit they arent in the mood for#ive never identified as endogenic bt we held some anti recovery ideals bc endogenic morality gave us some brain rot#and our ex was slowly pushing more and more towards endogenic and we recently learned they do id w endogenic#and they put weird morality shit in our brain abt merging and dormancy and shit
14 notes
·
View notes
Text
Management on Non-Sustained Ventricular Tachycardia:
Definition – The most common definition is three or more consecutive ventricular beats, a heart rate of greater than 100 beats per minute, and a duration of arrhythmia of less than 30 seconds.
●Symptoms – Patients with nonsustained ventricular tachycardia (NSVT) are usually asymptomatic, although some patients may notice symptoms associated with episodes of NSVT. Symptoms may include palpitations, chest pain, shortness of breath, syncope, or presyncope. Symptoms may vary depending upon the rate and duration of the NSVT along with the presence or absence of significant comorbid conditions.
●Physical examination – By definition, the pulse rate is greater than 100 beats per minute.
Few physical examination findings are unique and specific for NSVT.
If the physical examination coincides with an episode of NSVT, this can reveal evidence of atrioventricular (AV) dissociation, including marked fluctuations in blood pressure, variability in the occurrence and intensity of heart sounds (especially S1), and cannon A waves.
●Evaluation – All patients with suspected NSVT should have a 12-lead electrocardiogram (ECG), although NSVT is frequently identified on continuous telemetry monitoring, in which case only one or two leads may be available for review.
•Reversible causes – Once identified, reversible causes of NSVT should be sought, including electrolyte imbalances, myocardial ischemia, hypoxia, adverse drug effects, anemia, hypotension, and heart failure.
•Single asymptomatic episode – Often, for these patients, no further investigation is required.
•Multiple or symptomatic episodes – For patients with multiple episodes or with symptoms felt to be related to NSVT, a thorough diagnostic evaluation to exclude structural heart disease is warranted, including cardiac imaging and ambulatory ECG monitoring for most patients and invasive electrophysiology studies (EPS) only on rare occasions.
●Treatment
•Asymptomatic patients – In general, asymptomatic patients do not require any specific therapy directed toward the NSVT.
However, some asymptomatic patients with NSVT who are found to have infarct-related cardiomyopathy with significantly reduced left ventricular systolic function may be evaluated for implantable cardioverter-defibrillator placement for primary prevention of sudden cardiac death related to sustained ventricular tachyarrhythmias.
•Symptomatic patients
-Initial therapy – For the initial treatment of patients with symptomatic NSVT, we suggest beta blockers rather than calcium channel blockers or antiarrhythmic medications (Grade 2C).
For patients with NSVT who remain symptomatic in spite of beta blockers, or who are unable to tolerate beta blockers due to side effects, we suggest adding a nondihydropyridine calcium channel blocker (ie, verapamil or diltiazem) rather than an antiarrhythmic medication (Grade 2C).
-Alternative therapy – For some patients who have frequent, highly symptomatic NSVT not adequately suppressed by beta blockers or calcium channel blockers, the addition of antiarrhythmic medications (table 1) may be helpful. We suggest amiodarone as the initial choice, rather than other antiarrhythmic drugs, based on its efficacy (Grade 2C).
In patients with very frequent symptomatic monomorphic NSVT not controlled by medications or who are unable or unwilling to take medications, catheter ablation can be effective for reducing or eliminating NSVT and associated symptoms.
3 notes
·
View notes
Text
This is only something I've heard recently from my psychologist… but why is nobody talking about how specific manifestations of ADHD—particularly those with both high levels of emotional dysregulation and rejection-sensitive dysphoria, and the ability to mask the more 'stereotypical' ADHD symptoms—can be similar to, or even identical to, disorders such as BPD? It all ultimately comes down to the root causes of the issues. And until the correct diagnosis is provided based on the underlying reasons, regardless of the symptoms, the disorder will most likely be treatment-resistant.
When I learned this, my own experiences felt validated. Often, I brought up to my psychologist, "Are you sure I don't have BPD? I feel like there are things that aren't adding up, considering the disorders I have." And the thing was, I did have all the symptoms of BPD. I would qualify for a diagnosis of BPD. But the root cause of the symptoms wasn't BPD. It was ADHD. Learning that the two disorders had the potential for the same presentation, my situation made complete sense.
I'm not suggesting that one can't be diagnosed with both disorders. ADHD and BPD are highly comorbid, after all. And by the by, the distinction between the two is not based on trauma. Someone with, for lack of a better term, 'borderline-presenting ADHD' can experience the same amount of trauma as someone with traumagenic BPD, and the diagnosis wouldn't change based on that.
I'm also not saying this to suggest something such as "ADHD people should have the right to enter BPD spaces," so don't suggest that of me; I'm making a point about:
How two disorders can present almost identically,
The importance of considering the origins of a mental disorder and not solely the symptoms, and
How little we know about ADHD and its different presentations.
I'm not trying to be provocative or start a debate. I just wanted to share the facts I learned.
This post has been fact-checked by my psychologist.
2 notes
·
View notes
Text
someone in my MALS group had a high quality CT scan done, and he shared it bc although he DOES have the anatomy for a certain vascular compression, he found out that he's actually got slipping rib syndrome- his "false ribs" are totally disconnected and stabbing shit they shouldn't be and causing terrible upper abdominal and chest pain!!!
THE EXACT THING I COMPLAINED OF TO MY DIAGNOSING DOCTOR. The very same exact thing to which she said "that's not MALS" and then didn't offer an alternative.

THIS IS ALMOST WORD FOR WORD THE COMPLAINTS THAT I WENT IN WITH!!! I said doc it's so extremely postural. I can ONLY get relief on my back. I can't fucking move or bend or reach across my chest or set my hand on my belly button or wear pants without a stretchy waist because it HURTS. and she just said "that's not MALS" and changed the subject.
what's funny is right before I got DX'd my gastro also said "that could be costochindritis" and I said ah yes, well, I have hypermobile joints, and he went, ah, yes, indeed.
GUESS WHO FUCKING GETS SLIPPING RIB SYNDROME.... It's not people who's ribs stay in place!! I'll tell you that much!!!
In any case I, too, have the vascular compression anatomy... whether that's what's causing my pain is what remains to be seen. But this whole journey since getting diagnosed with MALS has just repeatedly pointed me back to EDS since it's highly suspected that MALS is caused by EDS, seeing as it's... Literally a slipped ligament...
This though???? This is game changing information. And I can't stress enough that like... Yes, the longer I prolong surgically addressing MALS, the worse it gets. That's guaranteed. What's not guaranteed is whether surgery will fix the pain. Bc if you have MALS, but you ALSO have 3-4 other vascular compressions that don't get addressed, only fixing the MALS makes the others worse. If you have nerve damage and the nerve bundle isn't addressed, you need revision surgeries later. If you have MALS but you also have some other complex issue that can only be diagnosed via process of elimination (i.e. gallbladder dysmotility), addressing the MALS will improve your blood flow and possibly your health, but not your pain levels/ability to eat.
There are SOME people who got the MALS dx, got surgery, and got their life back, no qualifiers. But there are many more whose MALS was comorbid with lots of other weird, complex shit that flew under the radar until long after their MALS surgery(ies) failed.
And on top of that I'm gonna be going out of state for a lot of this- I can do CTAs and other scans close to home, but the specialists are all elsewhere.
On the one hand yes I am in unbearable, unbelievable pain every day and it's only getting worse. On the other hand, I'm real glad I'm taking this time to research MALS before choosing a specialist... Its presentation varies wildly from patient to patient, but all of what I've heard tracks. Ykw I mean? It ALL fucking tracks. For the first time in a decade things are actually starting to make sense and fall into place.
That just makes me wonder, do I try and find an EDS specialist before speaking to a MALS one? Cus that's the kicker... Both are "rare" even if they're very frequently comorbid with each other. EDS docs won't necessarily know about MALS and MALS docs won't necessarily know about EDS. hardly anyone takes a holistic approach. But if I can find someone to confirm/deny shit like EDS or SRS, that's still something I very much want to know before I go in for a MALS release, and I absolutely don't want anyone touching one compression before we can confirm/deny others.
I s2g if it was my ribs this whole time I'm gonna scream
2 notes
·
View notes