Text
Nursing, travel and babies
By Olivia Day
Current Bachelor of Nursing student
About me
I was born in West Virginia, USA to a nurse (my mother) and a neurosurgeon (my father).
Dad was offered a job in Wollongong, Australia, when I was around four years old, so my family made the decision to leave our little town in the US; it was just after the September 11 attacks in 2001.
I was raised in Wollongong and attended the same school from Kindergarten to Year 12. Thanks to my parents, I’ve been immersed in the medical world for my whole life, leading me to where I am today.
Why nursing?
I’ve always been fascinated with babies and birth – something of a departure from my Dad’s speciality and my Mum’s interest in cardiac scrub nursing.

In Year 11, I landed in a maternity placement for work experience. I couldn’t believe how much I loved it! I loved being with the patients and their little ones on a first-name basis.
Ever since, I’ve been working towards achieving this goal of becoming a nurse/midwife, and perhaps in the future a medical doctor.
Why UTS?
Because it offers the opportunity to combine the Bachelor of Nursing with a Bachelor of Arts in International Studies.
Even though Wollongong’s local university is much closer to home, once I’d learnt that I’d been accepted to my first choice of degree, I was set on studying at UTS.
I thought that commuting from Wollongong would be incredibly hard, but actually, being able to compact my timetable into 2-3 days a week and catching the train has been lovely - every day I have three hours to sleep, study or relax.
I’ve always loved travelling and aim to travel once I’ve gained more experience in nursing and midwifery.
So when I found out that this degree gave me the chance to live in another country for a year to learn the language, culture and attend another university, I jumped at it. I couldn’t believe that nursing could be combined with International Studies – it was the perfect degree for me.
The placements
The most rewarding aspect of the course is being able to apply what we learn in the labs, tutorials and lectures on real patients, in real wards, in real hospitals every semester.
I have already done two clinical placements – one in Orthopaedics at Royal Prince Alfred and more recently in Oncology and Neuromedicine at Sutherland Hospital.
In the next four years, I’ll get the opportunity to do many more placements and possibly attain an ‘Assistant in Nursing’ job.
I’ve had many amazing interactions with patients who trust us wholeheartedly, despite the fact that we are students. So many are impressed by what we can already do (in first year) that they believe we are already in final year and are about to start working full time!
Seeing a patient smile when they see your face in spite of the pain of their situation is an amazing feeling. Being that person to bring their day to a higher point is so much more rewarding than anything else I have ever experienced.
The support
One subject I particularly enjoyed was Assessments and Therapeutics 2 (a practical subject) with tutor Elizabeth Stoddart.
She was brilliant because she shared her stories from a lifetime of experience – from her time as a student nurse to being a Nurse Unit Manager (NUM).
In spite of her packed schedule, she was always excited to teach every class and came prepared to let us know what she thought was the most important content of every week.
We would also need to come prepared, because she wasn’t afraid to put us on the spot! I hope I have the pleasure of being taught by her in my remaining few years.

The future
I want more than anything to work with mothers and babies.
This dream can take me anywhere in the world to help any new mother and her little baby, and that’s what keeps me motivated.
After finishing this first degree, I’ll do my new graduate nursing year and then hopefully complete the Graduate Diploma in Midwifery in the following year.
My advice
Be prepared to study hard; talk to lots of strangers and staff on placement; make friends with people who share your strange medical interests; believe in your abilities and ask for help when you need it.
If you ever feel like you’re falling behind or you’re just not getting it, there’s hundreds of students in the course who probably feel the same way.
Don’t be afraid to do what you want to do. My parents wanted me to do medicine, but now I love that I’m doing nursing.
Follow your passion and see where it takes you.
3 notes
·
View notes
Text
Carbohydrates and Common Sense:
in the Dietary Management of Diabetes
By Roslyn Smith
Accredited Practicing Dietitian, 18 years
Senior Diabetes Dietitian, 15 years
What is the right diet for diabetes? Opinions abound!
Sugar-free, paleo, low GI, low carb...
Week by week the media churns out the latest dietary fads, leaving the average person with diabetes very confused.
In the quest for a quick-fix answer, one ingredient is often left behind. Common sense!
In truth, there is no one-size-fits-all diet for diabetes. How can there be? So many factors affect a person’s dietary needs. For example:
Type of diabetes and other health conditions
Medications
Food preferences
Social and emotional needs
Culture, work, physical activity and lifestyle
Type 1 verses Type 2 Diabetes
Take for example, Type 1 verses Type 2 diabetes.
In Type 1 diabetes, the pancreas cannot make insulin, the key hormone that controls blood sugar (glucose). Insulin is given via injections or pump device.
For good glucose control, insulin doses must be carefully matched to the amount of carbohydrate eaten. Knowing how much carbohydrate is in foods is critical. Healthy eating alone will not control blood glucose. Neither will exercising or losing weight.

Type 2 diabetes is different. Here, the body does not respond well to insulin.
This places the pancreas under stress, so it cannot make enough insulin in certain situations. The result is high blood glucose. Weight loss, exercise and healthy eating improve the body’s insulin response, so can lead to better glucose control for many people.
Two Carbohydrate Myths
Myth 1: People with diabetes should avoid all sweet foods

It is true that most people with diabetes need to limit foods with heavy sugar content, such as rich desserts & biscuits, cakes, soft-drinks and chocolates. (On occasions these are OK, but not on a regular basis).
Even so, not all sweet foods lead to problems...and some non-sweet foods can!
If someone carefully avoids putting 1 teaspoon of sugar in a cup of tea, but then eats 2 cups of rice for lunch, they are misguided.
Two cups of cooked rice will release the same as 20 (twenty!) teaspoons of sugar into the blood...and it doesn’t taste sweet.
In Type 2 diabetes, a better amount of rice for a meal will be one cup, not two.
Similarly, some people avoid sweetened yoghurts, milks and fruits, yet eat large amounts of bread.

However most fruits and milk products are low glycaemic index. This means glucose is released slowly into the blood.
In contrast, white, wholemeal and many other breads are high glycaemic index: fast glucose release.
This means fruits and milk products (including sweetened types) are less likely to lead to high glucose than the same amount of carbohydrate as wholemeal bread.
In Type 2 diabetes, a sensible amount of bread is often two slices at a meal (look for a low GI brand), followed 2-3 hours later by a tub of yoghurt or piece of fruit.
Myth 2: People with diabetes should follow a low carbohydrate diet
Low carbohydrate diets may improve weight and blood glucose in the short-term. However, the long term picture is unclear. Very little research has been done beyond 6-12 months.
For starters, most people cannot follow a low carb diet for longer than a few weeks. They get too bored...and often, constipated!
Imagine having no breads, cereals, pasta, potato, corn, rice, fruit or milk. In fact, most foods made from flours and grains are off limits in a low carb diet. This leaves mainly meats, eggs, cheese, oils, fats and certain vegetables.
As you can imagine, low carb diets are often inadequate in nutrients and fibre, yet high in protein and animal fats.
Animal fats can increase long-term risk of heart disease, kidney disease and insulin resistance. This means that even if glucose levels improve short-term, down the track they may worsen.
For Type 2 diabetes, a better approach is often ‘carbohydrate spreading’.
Instead of eating one or two big meals per day, carbohydrate is divided into small regular amounts. This puts less strain on the pancreas, and improves glucose levels.

Low glycaemic index (low GI) carbohydrates can also help, by releasing glucose slowly into the blood.
Low GI foods include:
certain wholegrain breads, grains and cereals;
most fruits
most dairy products
most nuts and legumes (lentils and beans)
For more details, visit www.glycemicindex.com.
Getting personalised help
With so many factors in play, people with diabetes need personalised diet assessment and advice. This is best provided by an Accredited Practicing Dietitian (APD).
APD’s are university-trained in the science of nutrition, so are able to judge fact from fiction.
To find an APD, contact your local hospital or visit www.daa.asn.au.
Interested in becoming a Credentialled Diabetes Educator? Read more about our Graduate Certificate in Diabetes Education and Management
#diabetes#wdd#wdd2016#worlddiabetesday#nutrition#dietetic#dieticians#health#healthcare#healthcare practitioner#food
0 notes
Text
Hearing Voices
Fiona Orr
Director of International Activity and Mental Health lecturer at the University of Technology Sydney Faculty of Health
How did you get into mental health nursing?
I was at university studying special education but when I saw an ad promoting mental health nursing training.
So I decided to undertake a three year hospital-based training program to become a mental health nurse. Later I went on to do general nursing. I finished that course, but went back to mental health because I enjoyed the time we had to talk, sit and listen to patients and their families.
Nursing education was transitioning from hospitals to universities around 1990, so at that point in time I did a Bachelor in Health Science Nursing.
I then went on and did a Masters of Letters and Research in women’s studies, and my thesis looked at blaming mothers for schizophrenia. So that involved historiography and interviewing women parents who had adult children diagnosed with schizophrenia.
Simultaneously, I got into education in nursing. So UTS is the third university I’ve worked at, and I’ve been in the UTS Faculty of Health for eight years working as a Lecturer in Mental Health nursing.
What is it about mental health that piqued your interest?
I’m interested in people and people’s behaviour- why we think and act the way we do.
I like meeting people, listening to people and talking to people, so since starting that course, I’ve never looked back – I’ve always been glad I did mental health nursing.
I also grew up in an area of Sydney which had a reasonably large mental health hospital, and it intrigued me; I wanted to know, what happens to people in psychiatric hospitals - how do they get help, how do they recover or get better?
What practical experience do nurses gain in mental health care at UTS?
In every clinical nursing subject, students will go out on a clinical placement and experience working alongside mental health nurses in a range of health services - in hospitals and the community, in justice health settings and also in non-government organisations.
We prepare for those placements here at UTS through collaborations with consumers and being involved in a number of simulations and online learning experiences that actually involve working directly with consumers who inform the kind of materials we present in the module.
For example, our “Hearing Voices” module was actually developed by consumers who hear voices (see more on this later).
We also do things like live simulation in our third year elective. So, the students actually meet several consumers during the online learning modules, where they see me and another academics interacting with consumers, and this is designed to develop the students’ therapeutic communication skills.
And then they get to meet the consumers live. The students work in pairs with the consumer and they really learn about the lived experience of mental illness, talking to people who have sought help and can really comment on the kind of services that they’ve experienced and how they could have been better.
The consumer then gives feedback to the students about how the interaction went, about the therapeutic approaches they may have used and how they could develop that somewhat.
The consumers also really encourage students to use ‘recovery-focused’ communications, and to not see someone as a ‘diagnosis’ or a ‘condition’, but rather as a person, who happens to have experienced mental illness at a particular point in their life.
That person still has a whole range of goals, desires, achievements, strengths - they are much more than just their illness.
We find when students do this live interaction, the feedback has been overwhelmingly positive. Some say it’s one of the highlights of their degree.
To meet people before you go out on placement – to prepare and get feedback directly from that person – it’s just something invaluable that you can’t get any other way.
When students are out on placement, health consumers may not feel confident or comfortable enough to give that direct feedback in the clinical setting. But in the simulation, it works really well.
The ‘Hearing Voices’ simulation
The idea of this simulation originated in the USA and was developed by an academic called Patricia Deegan, a clinical psychologist who also hears voices – who has ‘lived experience’.
She and another group of people recorded simulated voices, sounds and experiences that they have when they hear voices.
So, in collaboration with a now-retired colleague of mine Kevin Kellehear, we worked with two others, Arana Pearson, an international educator with lived experience as a voice-hearer himself and Douglas Holmes who works at St Vincent’s Mental Health Service and also have lived experience as a voice-hearer. Both Arana and Douglas were trained by Patricia Deegan.

Photo (supplied): Arana Pearson, Douglas Holmes, Kevin Kellehear and Fiona Orr
Together we developed a simulation workshop that we thought would be useful to students, to give them some insight and some awareness about what it might be like to hear voices.
The simulation would encourage nurses to think about how an awareness of this lived experience may influence their practice.
So with some teaching grants we developed the ‘Hearing Voices’ workshop.
At the workshop, students listen to recordings on MP3 players for 45 minutes. Whilst they’re listening to the voices and sounds, they carry out a number of everyday activities, like getting a coffee or asking directions. So they get an idea of what it feels like and how it affects them.

Then the students come back and we discuss the experience in a large group. I think students get a really good insight into what it’s like and people react in different ways – physically, emotionally and behaviourally.
Then in processing that, we get students to reflect on how, in practice, they might interact with people who hear voices and want to talk to you about it.
What impact has this had?
Personally, it led me to do my PhD study on voice hearing and the use of this simulation with a cohort of over 500 final year students. I was really looking at measuring students’ empathy and their self-efficacy – their confidence – to talk to people about voice hearing, because the literature suggests that a lot of health professionals aren’t so comfortable talking about that.
The results (the PhD will be finished this year!) show that students now know ‘how it feels’ to hear voices and this is related to the experiential nature of the simulation.
The students’ empathy increased but its highest level was approximately six months after the simulation. The students’ confidence also increased immediately after the simulation and was maintained six months later.
The importance of empathy in Mental Health Nursing
Empathy is absolutely essential. I don’t think you could be a mental health nurse or any health professional for that matter without being empathetic.
There is intellectual empathy: the cognitive processes that we might use to try and get in someone’s shoes and understand how someone else might think or feel, but it’s more than that too.
It’s about connecting with or identifying with the underlying emotion that the person is trying to convey to you, and finding ways within yourself to develop that capacity.
Nurses are the professional group that are with healthcare consumers for extended periods of time, so being able to interact and develop rapport is central to the role of the nurse, and empathy is essential in performing that role.
Without that rapport, that connection, you can’t expect someone to talk about personal experiences, such as voice hearing.
It’s about working with the person, developing the idea of a collaborative partnership - an equal partnership.
Whilst the healthcare professional has the clinical experience, the consumer has the lived experience and knows how a condition affects them.
Families and carers also play a really important role because they have experiences in providing care too.
It’s important to make sure you never forget that as a nurse, or nurse-to-be, you’re working with people
The whole reason you’ve come into a Nursing degree is to be with people, to assist, support and care. And remember to keep that care, compassion and empathy at the heart of what you’re doing.
That can be challenging in health systems which can be difficult places to work in, where people are very unwell with complex problems, and resources are often limited.
Also, when you’re out on placement, observe the system and think about potential areas where you might want to work… and don’t forget mental health nursing!
We always need more mental health nurses. And of course, people have mental health needs throughout the healthcare system and can become mentally unwell in any healthcare context.
Mental health needs are everywhere, so even if students don’t want to specialise in mental health, they will encounter it in their health careers.
What makes a good mental health nurse?
A sense of humour is a good start.
You also have to be real – health consumers appreciate getting to know us.
Of course there are professional boundaries, but to be a real person who has life experiences and stories, and can relate to another individual is important.
Good nurses look beyond the diagnosis or the illness and see the person.
They see the strengths in people, their positive attributes and are willing to work alongside consumers.
But believe in yourself that you can do it, and that you can make a difference - consumers and their families will tell you when you do that.
Find out more about the UTS Bachelor of Nursing
Byline: Jack Schmidt
#nursing#nursingstudent#mentalhealth#mental health#health#world hearing voices day#worldhearingvoicesday
0 notes
Text
What makes a great Olympic athlete?
By Alana Leabeater
Bachelor of Sport and Exercise Science student, University of Technology Sydney
Everyone knows that to be an Olympian, you need to be physically and mentally fit.
You need to achieve the highest level of performance by being the quickest, strongest, most enduring, or a combination of all three.
But what other, lesser-known qualities can lead an athlete to Olympic stardom?

PERSEVERANCE
Eric Moussambani was a swimmer in the 2000 Olympics who had never seen a 50m pool in his life. A wildcard entry into the Games, Eric was the only swimmer in his heat after his competitors were disqualified for false starts.
With only eight months training under his belt, the crowd rallied behind Eric – later to be called ‘Eric the Eel’ – as he dog paddled to the finish, a lone figure in the Olympic pool.
Eric may not have fit into the standard description of a great Olympic athlete, but his perseverance and determination earned him a special place in Olympic history.
CHARISMA
Usain Bolt is one of the world’s most well-known athletes, and while that may be because of his dominance in athletics, it also comes down to his light-hearted, personable nature that makes him relatable to the everyday person.
And, it certainly makes him an athlete of choice for big brands like Puma, Virgin Media and Visa.

Photo: drcliffordchoi on Flickr
Without sponsorship, athletes have very few options to earn a living without working a job as well, which adds extra pressure to their already busy schedules.
Bolt’s charismatic personality has not only brought him enough income to never have to work a day in his life again, it has also brought the fun back to athletics after the sport’s reputation took a hit withnumerous doping scandals.
It has also made him the household name of the century across the globe.
ATTITUDE
Surya Bonaly was a French figure skater who consistently placed second at world championships, despite what many felt were perfect presentations on the ice.
In her last Winter Olympics, Bonaly was injured but knew this was her last chance to make a name for herself on the world stage, so she performed an illegal backflip on the ice, landing on one skate.
The breathtaking move earned her a deduction from her points, but ensured she would be remembered as a daring and adventurous athlete for years to come.
RESILIENCE
This year’s Australian flag bearer, Anna Meares, a track cyclist, is one such athlete who has shown great tenacity throughout her Olympic career.
In January 2008, Meares suffered a horrific crash at the World Cup where she broke her neck and dislocated her shoulder.
Despite this, she was back on the bike 10 days later and was able to qualify for the Beijing Olympics, where she finished second in the sprint to Briton Victoria Pendleton.
Four years later, Meares again faced Pendleton in the final of the 2012 Olympics and came home with the gold.
Many athletes would have retired from the sport after a crash like Meares’, but she used this bad experience to fuel her recovery and return to form.
THE TAKEAWAY
While the Olympics may appear to be a contest of physical fitness, this is not always the case; sometimes it is an athlete’s intrinsic qualities that immortalise them in the record books.
#Sports#sport#exercise#olympics#rio2016#erictheeel#usainbolt#annameares#sportandexercise#sportsandexercise
0 notes
Text
The sports psychology secrets of Olympians you can use at uni
By Alana Leabeater
Bachelor of Sport and Exercise Science student, University of Technology Sydney
I once heard a leading Australian sports scientist say that the next frontier in sports science has nothing to do with the body.
“Sports psychology,” he said, “is where most of our future medals will be coming from”.

Photo: Agberto Guimaraes
The fact is, we have mastered many of the physical determinants of success in sport. We know how to train the athletes’ bodies – but training their minds is a whole new ball game.
The 2016 Summer Olympics in Rio will see an unprecedented number of sports psychologists joining the support team for the Australian delegation.
They will help the athletes overcome the unfamiliar environment of Rio and achieve success in their individual events.
As uni students and non-Olympians, what can we gain from this new field of sports psychology?
VISUALISE WINS AND CHALLENGES
One common technique used by many elite athletes is visualisation.
As well as being the most decorated Olympic athlete of all time, American Michael Phelps is well known for using visualisation techniques before his races.
Phelps mentally goes through a ‘database’ of potential scenarios – for example, his goggles falling off – and thinks about what he would do in each situation.
This way, he is prepared for the scenario should it ever occur, even though he has only practised his response in his head.
Research by the Cleveland Clinic Foundation in Ohio showed that just performing mental rehearsal fired the same electrical impulses and muscle movement patterns as doing the actual movement.

Photo: Michael Phelps, @aqatxswim Instagram
So come the night before an important exam, consider spending a few minutes on visualisation – mentally rehearsing how you will open the exam booklet, be calm about the questions, answer to the best of your ability and finish in a good mood.
It also works well for those students who may have to participate in practical exams. Even spending a short amount of time visualising how you will take blood pressure, dress a wound or analyse an anatomy model will make you feel calmer and more in control when you actually sit the exam.
MEDITATE YOUR WAY TO SUCCESS
Another sports psychology secret of Olympians is their use of meditation.
The benefits of meditation range from increased serotonin production (the same ‘feel-good’ chemicals you get from eating chocolate, but without the calories!) to increased creativity and emotional stability.
For athletes, it helps them focus before big events and block out any external distractions.
For uni students, setting aside some time to meditate each week will lower your stress levels and decrease any anxiety you may be experiencing, especially around exam time.
If you don’t know how to meditate or what it involves, you can drop into the free mindfulness meditation practice that runs on Tuesdays at 3.10pm in the Multi Faith Room, in UTS Building 3, Level 5, Room 008.
YOU’VE HEARD IT BEFORE – SET REALISTIC GOALS
Finally, successful Olympic athletes excel at setting realistic, specific goals. For many of these athletes, achieving a medal at the Games is just ticking off their long term goal.
In a similar way, as a uni student you should set goals for each subject you are studying – for example, an overall grade you want to achieve.
Or, you could set a goal mark for each assessment in the semester. Make these goals visible so you can see them while you’re studying.
It is important you hold yourself accountable for your progress.

So, update your goals when you receive results to see how you’re going, and set new goals if you need to.
As you watch the Olympics these next few weeks, take a second to appreciate the mental strength of the athletes, and try and utilise some of their secrets in your everyday life.
#Sports#sport#psychology#olympics#olympian#athletes#student#student life#sport and exercise#sports and exercise#inspirational#goals#mindfullness#meditation#visualisation#winning#science#sport & exercise
0 notes
Text
“Tofli, Jasadi”: My Child, My Body
Infant Feeding beliefs and practices of Arabic mothers in Australia
By Amanda Rehayem

UTS:Midwifery students Rachel, Judy and Amanda (Source: Anna Zhu)
The theme of World Breastfeeding Week in 2016 focuses on how breastfeeding encourages us to think about how to value our well-being from the start of life, how to respect each other and care for the world we live in.
Breastfeeding has long attracted the interest of health researchers around the world.
Popular topics of research include the long and short-term benefits of breastfeeding for mother and child; how breastfeeding affects the mother-child bond; and how breastfeeding is practised by mothers from diverse cultural backgrounds.
As a large multicultural society, there is an ever-increasing need for culturally based healthcare research in Australia.
In particular, minimal research exists on Australian Arabic women and their beliefs and practices on infant feeding.
My project sought to delve into this topic, recruiting mothers from the Lebanese Muslim Association (Lakemba), St Joseph’s Maronite Church (Croydon) and St Charbel’s Maronite Church (Punchbowl) in Western Sydney.
I conducted three focus groups, discussing attitudes to infant feeding with a total of 17 attendees.
Photo: Dharmacat on Flickr
Most of the participants expressed a strong desire to breastfeed their child, revealing that breastfeeding is considered “natural” and “normal” within their families.
Participants also described how, in Arabic culture, “fatter” babies are perceived as healthier, particularly in the eyes of older Arabic women. This perception can lead to over feeding the infant or even introducing formula at an early age.
Another key finding was the importance of Arabic mothers’ relationships with their close female relatives.
Arabic mothers readily seek education and knowledge from their own mothers, grandmothers, aunts and mothers-in-law.
In this sense, infant feeding is a kind of “women’s business”. Breastfeeding mothers are strongly supported by trusted women in the family.

As one mother said:
“Breastfeeding comes with experience, and these women had babies! They didn’t have one or two – they had six, or seven, or eight or thirteen in my grandmother’s case. So it comes with real knowledge of child-raising, and there is a level of trust and respect that you’ve got to give. So as much as I respect my GP, I will also listen to my grandmother and what she says, definitely.”
It’s clear that breastfeeding really does impact a woman’s life.
Women don’t feel comfortable if they feel that no one understands their beliefs or practices, especially in that vulnerable position of just having had a baby.
I hope out of this research - as clinicians, as midwives, as nurses, policy makers and lactation consultants - we can work towards increasing culturally competent care.
#wbw16#wbw2016#breastfeed#breastfeeding#baby#infant#feeding#arabic#muslim#maronite#women#womens health#midwifery#health#Healthcare#utshealth
2 notes
·
View notes
Text
Tips from a Midwife: top reasons to breastfeed
By Rosemarie Hogan
Director of Midwifery Studies and Course Coordinator for the Bachelor of Midwifery at UTS
When it comes to food, the science is clear – there’s nothing better than breast milk for your baby. The benefits of breastfeeding extend well beyond basic nutrition.

Photo: David Leo Veksler on Flickr
1. Breastmilk provides all the food and drink a baby needs for about the first six months of life.
2. During breastfeeding the ‘love hormone’ oxytocin is released, which enhances attachment between mother and baby.
3. Breastmilk provides the baby with resistance to disease via antibodies and other components, which fight infections.
4. There is a decreased risk of breast and ovarian cancer in women who breastfeed. Breastfed babies have a lower risk of childhood cancers such as leukaemia and Hodgkin’s disease.
5. There is an association between breastfeeding and intelligence, with breastfed babies having improved performance in intelligence tests.
6. Breastfed babies have less orthodontic issues later in life if they have been breastfed for nine months or more.
7. Common allergies such as asthma, eczema and food allergies are less common in babies breastfed for at least four months.
8. Breastfed babies have fewer dirty nappies compared to formula fed babies.
9. Breastfeeding is convenient – readily available and at the right temperature, day or night.
10. Breastfeeding may lower a baby’s risk of Sudden Infant Death Syndrome (SIDS).
Remember:
Breastfeeding, while natural, is still a learned skill, at least for the mother.
Help with breastfeeding can be sought from a midwife or from organisations such as the Australian Breastfeeding Association.
Babies can be breastfed anywhere and anytime. Under the federal Sex Discrimination Act 1984 it is illegal in Australia to discriminate against a person either directly or indirectly on the grounds of breastfeeding.
Partners can help by being enthusiastic, supportive and knowledgeable. Research shows that when partners are more supportive and positive about breastfeeding, it has a strong influence on getting started and how long it lasts.
3 notes
·
View notes
Text
Heparin, pigs and vampire bats: What are you really administering?
By Dr Tamara Power, Director of Health Simulation at the UTS Faculty of Health

Photo: Anna Zhu
The next time you are out on clinical placement, pick up a vial of Heparin Sodium Injection and have a good look at it.
Heparin is an anticoagulant, used (among other things) for prophylaxis (prevention) and treatment of thromboembolic disorders such as pulmonary embolism or venous thrombosis (DVT) (MIMS Australia 2016).
Heparin comes as a clear solution for injection in 5,000 and 25,000 unit ampoules.
But where does it come from?
If you investigate, just a little, you will find that Heparin is actually prepared from the lungs or intestinal mucosae of pigs. When you look at the bottle you will see it is labelled porcine mucosa (MIMS Australia 2016).
But the plot thickens (or the blood thins) when you also consider that a glycoprotein found in the saliva of vampire bats is currently being investigated as an anticoagulant to treat ischaemic strokes and myocardial infarction (Low 2013).
Named Draculin (yes really), it is also being tested for use as a blood thinner to prevent heart attacks.

In fact many common medications are sourced from animal products.
The gelatin used in capsules is usually sourced from cows or pigs, and many exogenous hormones and anti-neoplastic (cancer) agents are manufactured using Chinese Hamster Ovary cells.
Influvac, a flu virus vaccine is prepared from a virus grown in a cavity of embryonated eggs.
Horses provide the source of many anti venoms.
Even lanolin, that everyday cream that we use on our patient’s cracked and broken skin comes from fat extracted from sheep’s wool (Department of Health 2013).
But apart from the “ewww” factor, what does this mean for us as nurses?
Maybe not a lot - but it could be important to our patients.
Some people for cultural or religious reasons may wish to avoid even traces of animal products in their medications. It is important to respect these beliefs and provide information to allow them to reach an informed decision.
If animal products are an issue for your patient, have them discuss synthetic alternatives with their doctor. In some cases the medication has been so altered from the original source that it may no longer be an issue.
The particular adherence to a belief will also vary from individual to individual.
But an informed patient is an empowered patient (Department of Health 2013).
Department of Health 2013, Medicines/pharmaceuticals of animal origin, Government of Queensland.
Low, DHWea 2013, 'Dracula's children: Molecular evolution of vampire bat venom', Journal of Proteomics, vol. 89, no. 26, pp. 95-111.
MIMS Australia 2016, Heparin Sodium Injection, viewed 6th June 2016.
0 notes
Text
Avoiding compassion fatigue
By Dr Tamara Power and Carolyn Hayes
The majority of students enter nursing because they are altruistic and wish to help people.

However, studies have shown that through constant exposure to people’s trauma and suffering, nurses can become both physically and psychologically burnt-out and suffer compassion fatigue (Ledoux 2015).
Compassion fatigue can manifest as feelings of anxiety, anger, cynicism and vulnerability and nurses can become detached from the care they provide (Ledoux 2015).
This is unhealthy for the nurse and impacts on patients’ health and wellbeing (Ledoux 2015).
The key to remaining compassionate is caring for yourself (Mills, Wand & Fraser 2015).
Here are some things to consider [adapted from Boyle (2015)]:
Make an effort to separate work from home. Talk to your family about your mood when you return from work or clinical placement. They will be sensitive to any changes in your overall mood
Take opportunities to debrief after confronting shifts with your peers and team leaders. For making sense of very traumatic events you may wish to speak to a counsellor
Make sure you schedule some ‘me’ time. This isn’t selfish but necessary. Take yourself for a walk, or disappear into a book. Schedule a massage or take a bubble bath
Spend time doing things you enjoy with people you care about.
Look after your physical health through ensuring you get enough sleep, exercise and good nutritious foods
Look after your spiritual health through practicing mindfulness. There are many free online courses and application.

All of these things will contribute to your physical and emotional wellbeing and make you more resilient.
Remember you can’t care well for others if you aren’t well and cared for yourself.
References:
Boyle, D 2015, 'Compassion fatigue: The cost of caring', Nursing, vol. 45, no. 7, pp. 48-51.
Ledoux, K 2015, 'Understanding compassion fatigue: Understanding compassion', Journal of Advanced Nursing, vol. 71, no. 9, pp. 2041-50.
Mills, J, Wand, T & Fraser, JA 2015, 'On self-compassion and self-care in nursing: Selfish or essential for compassionate care?', International Journal of Nursing Studies, vol. 52, no. 4, pp. 791-3.
1 note
·
View note
Text
The other side of sport
By Alana Leabeater
Current student, UTS Bachelor of Sport & Exercise Science

We hook our subject – a fellow classmate – into tubes and monitors, power up the computers and various other pieces of technology and monitor him as he starts to run on the treadmill.
First slow. Then fast. Faster still, to maximum speed until, finally - he taps out.
And like predatory birds, we flock to him as he struggles to stand, pricking him with blood lactate photometers, taking heart rate and perceived effort scores, analysing multiple displays on the computer and sucking our subject dry of any quantifiable data.
This is a V02 max test, a test that estimates maximal oxygen consumption (so is literally designed to make you fail), and it costs a couple of hundred dollars to run.
We are the lucky second-year students who get to run these tests on each other for free – with no guarantee that we’re going to do it right!
No tutorial in the Sport & Exercise Science degree is the same as the next.
Over the past three semesters that I have been studying at UTS, I have had to analyse the angular kinematics of playing on a see-saw; measure the ground reaction force produced when I jump; drink a few litres of Gatorade during the course of a tutorial to see the effect on my kidneys; dissect plenty of animal parts in the name of anatomy study, and more often than not, I find myself running, deadlifting, jumping, coaching, sprinting, hopping or throwing, to better understand and apply the theory of my degree.
Being the nerd that I am, one of my favourite subjects was first-year anatomy.
In our first tutorial, our tutor stood in front of a desk that was piled high with vertebrae models.
(For your information, we have 33 vertebrae in our spine, including the sacrum and coccyx).
Behind his back, he picked up a vertebrae model, felt its features without looking and would tell us what number vertebrae it was – say, C3 or T5.
To us newbies, this skill was beyond belief – how could he tell the difference? Aren’t all vertebrae pretty much the same?
It only took us two weeks to learn our tutor’s tricks.
Another subject I enjoyed was Exercise Physiology. As well as the V02 max test I mentioned earlier, we also looked at the basics of an exercising human body: how we convert the food we eat into kinetic energy, how we take in and use oxygen and what the anatomical difference between an elite sprinter like Usain Bolt and a recreational triathlete like myself is.
For any weekend warriors out there, we also looked at your old friend – lactic acid.
Here’s a hot tip: it’s not actually lactate that’s burning in your legs after you’ve climbed those hills or hit the leg press. It’s excess hydrogen which is interfering with your basic level of muscle contraction.

The good news is, all you have to do is keep training at or near this level of burn and soon you’ll be able to push your blood lactate tolerance further!
Sport & Exercise Science is a hands-on, get-involved degree that appeals to anyone who wants to be on the other side of sport – the people who analyse, diagnose, coach and encourage the star athletes and players.
At the moment, my dream career is in elite sport, running those V02 max tests, collecting data, interpreting it and translating it into athlete-friendly and coach-friendly terms.
This degree definitely feeds into that, while also giving me a broad range of skills in areas such as biomechanics, nutrition, psychology and management.
If you’re anything like me, once you’ve been studying Sport & Exercise science for a while you will start to analyse the sportspeople you see: scrutinising a friend’s gait as they run, hypothesising what sort of ligament sprain an NRL player is suffering from as they’re stretchered off the field or even poring over your own data sets from your Fitbit or Garmin.
As a sports enthusiast, this suits me down to a tee (excuse the pun).
0 notes
Text
Nursing, midwifery, or both?
UTS has a range of Health degrees on offer and, for many, choosing one can be a difficult decision.
What’s the difference?
The role of a nurse is to provide care for patients in a variety of healthcare settings.
Nurses are able to help people maintain health and well being or to care for those who are unwell or going through an adverse stage in their life.
Nurses can specialise in areas like emergency, theatre, paediatrics, community and primary care, aged care, mental health care and indigenous health and well being.
The range of core subjects and electives on offer at UTS allow students to tailor their degree and pursue areas of healthcare that are of particular interest to them.
The role of a midwife is to provide support for women and their families throughout pregnancy, labour and birth, and then for up to six weeks after the birth of a baby.
Midwives consider pregnancy, childbirth and early parenting to be healthy processes that are a normal part of life for many women.

Are nurses and midwives classified differently?
Yes. There are two classifications of nurses recognised by the Nursing and Midwifery Board of Australia.
They are:
1. Registered Nurses (RN); and
2. Enrolled Nurses (EN)
The UTS Bachelor of Nursing prepares you to become a RN.
ENs are supervised by RNs and need to have completed an approved qualification.
For midwives, there is one recognised classification: Registered Midwives (RM).
The UTS Bachelor of Midwifery and Graduate Diploma in Midwifery prepare you to become a RM.
What if I want to do both Nursing and Midwifery?
You can become both a qualified nurse and a qualified midwife within five years at UTS, and it doesn't matter which degree you start with first.

If you do the Bachelor of Nursing first, you can follow it up with a Graduate Diploma of Midwifery (five years total for both degrees).
And, if you start with the Bachelor of Midwifery, you can follow it with the Accelerated Bachelor of Nursing (also five years total for both degrees).
Also, if you’re an EN or have a prior health qualification you can do an Accelerated Bachelor of Nursing degree (two years full time).
MidStART – pathway to midwifery
MidStART (Midwifery Student Applications for Recruitment and Training)
is a career pathway established by NSW Health to help registered nurses become registered midwives.
The program provides employment for student midwives in NSW public health facilities whilst they are studying a postgraduate midwifery degree at a recognised university like UTS.
You’re eligible for the MidSTART program if you:
are an Australian citizen or permanent resident; and
hold a current registration as a Registered Nurse; and
are enrolled in a recognised midwifery degree (like the UTS Graduate Diploma of Midwifery).
MidStART offers a great opportunity for RNs looking to gain extensive hospital experience while they study midwifery at university.
Applications for the 2017 MidStART program close 15 June 2016.

Byline: Jack Schmidt
#nursing#nursing school#nursing student#nurses#midwife#midwifery student#midwifery#midstart#nswhealth
0 notes
Text
How to make it in the sport and exercise industry
#UTSCareers today hosted an instalment of The Job Truth Series, with leaders in the sport and exercise industry as panellists.

The special guests included:
Dr Andrew Walshe: Director of High Performance for Red Bull (Los Angeles)
Matthew Jeffriess: Strength and Conditioning Coach and Rehabilitation Coordinator for the NRL Referees (Sydney)
Michael Rennie: Strength and Conditioning Coach with the Sydney Swans
Matthew and Michael are also UTS:Sport and Exercise PhD candidates, working with our #utshealth academics Professor Aaron Coutts and Dr Job Fransen.
So what’s their advice to aspiring sport and exercise science and management students?
Get lots of practical experience across as many domains as possible Don’t expect a 9am-5pm job
Look for an alternate income stream to ensure you earn on the side, because it can take a while to make it
BUT, it’s a booming global industry, so keep an eye out for international opportunities (sometimes they pay double!)
Look at different sectors within the industry, such as health innovation, data analytics and health science
The sport industry in Australia is very competitive, so doing further study after your undergrad course such a Honours or PHD can really help
Diversify your interpersonal and communication skills - things like travelling and being in social situations can really help you work with others
Drive and improve any artistic skills (if you have them!)
Throw yourself out there, especially UTS:Health students, who are based at the UTS Moore Park precinct and are surrounded by elite athletes!
Ask your lecturers about volunteering to help UTS PHD research students, as this will open up opportunities
Explore psychology and mindfulness training, because the industry is beginning to really focus on this
Gain some skills in Excel
Get a good understanding of the companies you would like to work for
Once you know the company, find the gaps in the skills they need and then do whatever you need to do to get those skills
Most of all - get involved, diversify your skills (Excel!) and once you land a job hold onto it, because there’s a long line of people behind you.

0 notes
Text
Infertility and public health
By Associate Professor Alex Wang, Director of Research Studies in the Faculty of Health at UTS

Infertility remains a major public health problem in Australia, with 4.4% of all babies born using Assisted Reproductive Technology (ART) in 2013 (1).
What is infertility?
The World Health Organisation (WHO) defines infertility as the inability of a couple to achieve conception after one year of unprotected intercourse.
Infertility is shared equally among men and women, and one in six Australian couples suffer primary or secondary sub-fertility. It may be treated by medical or surgical techniques, or lifestyle changes.
The cost of ART
Although ART is an effective sub-fertility treatment, it comes at a great cost to couples.
The assessment and treatment of sub-fertility represents a significant economic activity in Australia with $244 million in Medicare Benefits Scheme benefits paid in 2013 alone (1).
Internationally, there is growing recognition of the impact of health complications and downstream costs associated with the maternal care of high risk and multiple gestation pregnancies, adverse events and the perinatal care of pre-term infants as a consequence of using ART.
One ART treatment is in-vitro fertilisation, or IVF, which the research team here at the UTS Faculty of Health has recently competed research on.
The risks of IVF
We found that these increased risks of adverse events vary between clinical procedures, patient groups, and potentially over time:
5-fold increase in multiple births following ART cycles compared to all births.
1.3-fold increase in gestational diabetes compared to non-ART mothers.
1.2 fold increase in gestational hypertension and preeclampsia compared to non-ART mothers
1.5-fold increase in fetal death for births following double embryo transfers (DET) compared to single embryo transfers (SET).
1.6-fold increase of low birthweight for liveborn singletons following fresh embryo transfers than frozen transfers.
1.3 fold increase of preterm birth for liveborn singletons following fresh embryo transfers compared to frozen transfers.
1.5-fold increase in perinatal mortality compared to all births.

IVF and ectopic pregnancies
Approximately one to two percent of pregnancies in Australia are ectopic, which means that the embryo attaches outside of the uterus.
But this rate is much higher in pregnancies that result from assisted reproductive technology such as IVF, with the rate being as high as 10%.
Here at the UTS Faculty of Health we have looked at the best IVF treatment to reduce the risk of ectopic pregnancy.
We found a single frozen Day 5 embryo has the lowest risk of ectopic pregnancies.
The reason is because in a fresh treatment, the uterus environment is negatively impacted by the hormone stimulation, whereas in a frozen embryo transplant, the uterus environment is like a natural conception.
See more on our research here
IVF and gestational surrogacy
Another study (3) we conducted has found that single-embryo transfers should be advocated for all gestational surrogacy arrangements.
In our study of 360 gestational carrier cycles, we found little difference between the rates of clinical pregnancy and the rates of live delivery for single-embryo transfer (SET) or double-embyro transfer (DET).
However there were less babies born pre-term (13%) with SET than there were with DET (31%).
Furthermore, the chance of twin-birth was higher with DET (5 in 22) compared to SET (0 of 48).
See more on our research here
Other resources:
Australian Institute of Health and Welfare. Australia’s mothers and babies 2013—in brief. Perinatal statistics series no. 31. Cat no. PER 72. 2015: Canberra, AIHW.
The Fertility Society of Australia
0 notes
Text
Keeping Australia Alive - only requires men?
By Caroline Homer and Vanessa Scarf
Centre for Midwifery, Child and Family Health, Faculty of Health, University of Technology Sydney
Having worked in the Australian health system for more than 30 years we both looked forward to "Keeping Australia Alive" series on the ABC.
Health care in Australia is complex with its governance and provision being managed by eight state and territory governments, multiple for profit and not for profit organisations and in cities with millions of people through to some of the remotest places on earth.
Understanding, recognising and celebrating the people who work in these systems is essential if they are to flourish.
We expected the series to at the very least show the health workforce as it really is - hard working, ethnically diverse and predominantly female.
In Episode 1 the ‘workers’ in the background doing ward rounds, getting handovers, talking and caring for patients and supporting families were predominantly nurses and midwives who were evidently female.
And yet those who talked to camera and got a by-line that identified their name and role were doctors who were, as you might have guessed, men.

Image: Keeping Australia Alive, ABC
So, we decided to watch each episode with an analysis template examining gender and discipline mixes.
The gender and discipline inequity was glaring in Episode 1 - women worked busily in the background while every single health professional that spoke to camera was male.
Even the midwife was male – good for him, but given that 99% of midwives are female and the rest of the episode was an all male affair, a female midwife was surely not too much to ask for.
Sadly, this situation continued in all but one other episode.
While we recognise and accept that doctors are a critical component of the health system, they are not the only ones ‘Keeping Australia Alive’.
Image: Keeping Australia Alive, ABC
According to the Australian Health Practitioner Regulation Authority, 76% of the health workforce are women.
This is especially notable in the disciplines of nursing and midwifery (where it is in the order of 90% women) but also in the allied health professions and now in medicine where more than 50% of those entering medical school are now women(1)(2)(3)(4)(5)(6)
Sadly, with Episode 1 the die was cast.
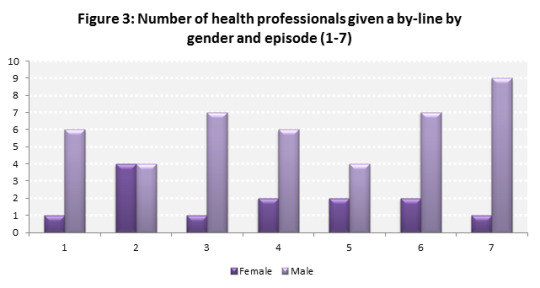
The proportion of women health professionals who were interviewed to camera and proffered with a by-line ranged from 14% women in Episodes 1, 3 and 7, 29% in Episodes 4, 5 and 6 and reaching more than half (57%) only in Episode 2 (see Figure 3).
Nurses and midwives make up the largest proportion of the health workforce, but the proportion of nurses and midwives who were interviewed to camera and proffered with a by-line ranged from 0% in two episodes, 14% in one episode, 29% in three episodes and 43% in one episode.
Overall, 23% of the health professionals who were interviewed to camera and given a by-line were women and 18% were nurses or midwives.
So, where were the women? Where were the women doctors, nurses, midwives, allied health professionals and managers?
Women play senior and junior roles in every aspect of health care – where were they?
Maybe they were too busy doing the work to be interviewed or maybe the producers of the show were displaying an unconscious bias that should be named and confronted.
Not for a moment do we contend that the significant gender imbalance of the programme was intentional.
Years of habit, inculcation and exclusion can lead even the best of us to miss what is in plain sight – a system overwhelmingly staffed and run by women who are barely recognised and for most of the programme, largely ignored.
Gender equity across Australia in all walks of life and work has a long way to go and judging by the Keeping Australia Alive series, the ABC is no exception.
All health care professionals are essential but how is it that an esteemed broadcaster like the ABC and a program clearly with considerable resources could get the numbers so wrong?
What message does this send to the young women in our community considering a health care profession?
What message does it send to the thousands of women and men considering a career in the important and necessary disciplines of nursing and midwifery?
We think it says – yes, you are important … but not important enough to give you a name … to give you a title, a by-line, … to highlight your critical role in the Australian health care system.
We love the ABC, which makes writing this analysis all the more painful.
But calling everyone on gender equity is, for us, essential.
And it’s just as essential for the ABC to look at the objective data on this and other programmes and not fall into the trap of perpetuating gender myths that have no place in 21st Century Australia.
[1] http://www.nursingmidwiferyboard.gov.au/About/Statistics.aspx
[2] http://www.medicalboard.gov.au/News/Statistics.aspx
[3] http://www.dentalboard.gov.au/About-the-Board/Statistics.aspx
[4] http://www.pharmacyboard.gov.au/About/Statistics.aspx
[5] http://www.physiotherapyboard.gov.au/About/Statistics.aspx
[6] http://www.occupationaltherapyboard.gov.au/About/Statistics.aspx


#health#nurses#nursing#midwives#midwifery#hospitals#australia#abc#australianbroadcastingservice#keepingaustraliaalive#women#gender equality#healthcare#healthcare practitioner
1 note
·
View note
Text
Being Aboriginal is about soul, not colour
What part are you?
My name’s Angela Phillips, I’m a Wiradjuri woman.
I am a registered nurse, nursing lecturer and the Aboriginal and Torres Strait Islander Faculty Health Advisor here at UTS:Health.
All my life, people would say - “You’re too white to be Aboriginal.”
People would see my Dad (an Aboriginal man) and people would see me, and they’d ask “What part are you?”. I didn’t understand the connotation of what ‘part’ meant.
It wasn’t until I did my own research that I understood that assimilation policy was actually based on the idea that you’re ‘part’ – there was a negative connotation to it. It was a form of genocide because they were trying to breed people out.
So, when I hear people say, “What part are you?”, I say, “I’m not part – I am what I am.” My mother was non-Indigenous, my Dad was Aboriginal, and I’m very proud of that, I relate to that, I understand that, so, I am a “Philllips” and I am aboriginal.
I don’t see that I am a “part” something. I am.

You’re just a nurse
I remember talking to my husband and saying, “I want to be able to do something about this.”
But people were saying, “You’re just a registered nurse.”
So my husband said, “Well, do an education course.”
I enrolled in a Bachelor of Education degree. I started talking to other registered nurses and I realised that they already had ideas about Aboriginal people; it was coming from their school curriculums. And I wanted to change things, but I knew I needed more.
So I went on to do a Masters degree.
We created a safe space
When I first came here in 2000, there were no Aboriginal students at all in nursing or midwifery at UTS. We’d had a couple enrol, but they’d been unsuccessful in their studies. To begin with I rang the unsuccessful students to find out why they felt they couldn’t continue.
So, I started working very closely with the UTS Jumbunna Indigenous House of Learning. We created a safe space for the students to feel safe in their studying and we organised for Jumbunna to come out for a support day one day a week.
We started recruiting - going out into the community to talk to them about nursing, talk to the hospitals where there were some Aboriginal and Torres Strait Islander enrolled nurses, and we increased our numbers.

We established an alternative entry program where we can review Aboriginal and Torres Strait Islander Nursing students.
They may not have the requirements or the HSC mark, but we can see their potential for success if they receive the support that they need. So we conduct assessments on them every year.
We’ve now got a new project called the Galuwa project, which gives Indigenous high school students a taste of what it’s likely to study health at UTS. Last year we had twenty students attend, so it was really successful.
In my role I also look at the curriculums and see where Indigenous health education fits in.
One of our great achievements happened in 2010, when we were able to integrate a core subject (Contemporary Indigenous Health and Wellbeing) into the Bachelors of Nursing and Midwifery at UTS.
I’m very proud of those little things and the little steps we’ve been able to create.
Three years ago I started my PhD with the support of the faculty, so I’m very thankful. It looks at Indigenous content in undergraduate health degrees, so it’s close to my heart and it fits really well.
The outcome that I’m hoping for is that we can create a model that can be embedded across the university.
How much has actually changed?
Since the Federal Government’s Closing the Gap 2010 report on Indigenous disadvantage, how much has actually changed? Where are we breaking the cycle?
Statistically, Indigenous males in this day and age have a life expectancy of 55.
The state of mental health and suicide is one of the saddest things. Since the NT intervention, we’ve had the largest number of removal of children, even since assimilation policy - comparatively the largest numbers.
We’ve had increased incarceration. And we know with increased incarceration we have increased suicide.
It’s not going to change until we actually stop incarcerating people so easily. 75% of juvenile justice is made up of Indigenous youth and we only represent 3% of the population.
So to make up 75% of the system… that’s unheard of. We know that we’re setting them up to fail. Statistically speaking, we know that an Indigenous male is more likely to be incarcerated on his first offence than anyone else.
And since the system has removed the funding for the Aboriginal legal service, incarceration of Indigenous youth has tripled since then and I don’t see it getting any better with that system in ealth be known. One of the discussions we have with students (international and domestic) is ‘what do you know about Aboriginal people and what’s your understanding’? There’s such a wide range of levels of awareness and education, so it’s so important to have those discussions.

0 notes
Text
Nurses: A force for change
The following has been summarised from the International Council of Nurses’ (ICN) International Nurses Day 2016 Kit.
International Nurses Day (IND) is celebrated on May 12, the anniversary of Florence Nightingale’s birth.

Each year the IND provides a comprehensive examination of how nurses can contribute to the annual focus (the theme).
This year, the theme is ‘A force for change: improving health systems’ resilience’.
So what does that even mean?
Firstly, a word from the heads of the ICN:
You may wonder how you as a nurse can help to strengthen health systems around the world. As a member of the single largest group of health professionals, with a presence in all settings, nurses can make an enormous impact on the resilience of health systems. Every decision that you make in your practice can make a significant difference in the efficiency and effectiveness of the entire system.
- Judith Shamian (ICN President) and Frances Hughes (Chief Executive Officer)
Secondly, a re-cap of what resilience actually means:
“Resilience: the capacity to recover from difficulties” - Oxford English Dictionaries
So how does ‘resilience’ relate to the health sector?
“The resilience of a health system is its capacity to respond, adapt, and strengthen when exposed to a shock, such as a disease outbreak, natural disaster, or conflict.”
- Campbell et al (2014)
The ICN are an international organisation, so we’re talking public health on a global scale.
There are currently 17 Sustainable Development Goals (SDGs) that the United Nations (UN) Member States (including Australia!) are trying to achieve:
These global goals will transform our world:

Read more about the goals
Nurses need to lead by example
In the ICN’s report, they state that:
Nurses and nursing are subject to growing pressures, including regular reviews and reorganisations, coping with changes to service delivery and models of care, financial pressures, expanding scopes of practice and enhanced expectations of what a nurse workforce should achieve (ICN 2015b, 2015c).
If we develop a better understanding of the relationship between personal resilience and our ability to provide care, then by extension this helps us to extend our skills outwards to support improved personal resilience in the wider population.
So what they’re saying is that we need to ensure good working environments for nurses, but also that nurses who demonstrate personal resilience will be beacons of hope or leaders for the general populace and their resilience.
So what can you personally do?
We’ve summarised what the ICN states you can do personally into a handy graphic:

We hope this summary inspires you to be a force for change.
Read more about the International Council of Nurses here
Happy International Nurses Day 2016!
#nurses#nursing#nursing student#change#change agents#public health#global health#international council of nurses#international nurses day#IND2016#florence nightingale
0 notes
Text
The heart of midwifery
By Professor Caroline Homer
As the International Day of the Midwife approaches on 5 May 2016, our Associate Dean (International and Development) for UTS:Health reflects on its theme: 'Women and Newborns: The Heart of Midwifery'.

As a midwife, you certainly use both your head and your heart.
You need your head, because every day you need to make good clinical decisions, provide sound evidence-based advice and guidance to women, collaborate with other disciplines, plan, evaluate and reflect on practice and understand and keep within the legal, professional and ethical standards that direct midwifery practice.
Midwives also have an amazing capacity to influence the psyche of women throughout pregnancy, labour and birth and after the birth.
One of the most important ways to build on women’s inherent strengths is to build their confidence in their ability to grow a baby, give birth to a baby and mother a new baby.
Walking alongside women and providing care, support and information through the experience means that midwives are in the best position to support women to achieve the best for them.
For many women that will be a normal birth and for some it will be a caesarean section. It is the role of the midwife to ensure that regardless of how women give birth, they feel strong and confident in the decision making process and have control over their experience and choices.
But, in midwifery, there is also the heart – the passion for what we do, the desire for every woman to have the best pregnancy, labour and birth and postnatal experience she can have so that she starts motherhood strong and confident.
The heart is the joy of seeing a woman see and hold her baby for the first time and the delight at getting to know this amazing human being that her body grew.

The heart is also walking alongside women in their darkest moments – those that are filled with unmeasurable grief and loss.
Being a midwife is rarely grey – it is joyful bright white most of the time, but there are moments of blackness – and these extremes can tear at your heart.
In the 25 years since I became a midwife, we have become so much more focussed on the woman, her baby and her partner.
I have seen a real shift; from being taught how to practice according to the rules of the institution, to focussing on being in a partnership with the woman – making sure she is kept at the centre of care.
It is not yet perfect and there are sadly still plenty of rules put in place – many to service the institution rather than the woman – but the focus certainly has changed.
In the past 25 years there has also been a huge shift to recognising the importance of continuity of care.
There is now very good evidence that midwife-led continuity of care is the gold standard of maternity care and should be available to all women.
I am very proud that my PhD work contributed to this evidence and I know how satisfying it is to work in this way as a midwife and how beneficial these models of care are for women.

The other area that I think has changed is a focus on the midwife being well educated, well informed, being resilient and having emotional intelligence.
We need to make sure that midwives have all these qualities so that they can provide quality care that is thoughtful, respectful to women and satisfying for them.
Being a midwife is the most rewarding role that anyone could have. It is filled with opportunities and amazing experiences.
It is an extraordinary privilege to share this special time with a woman and her partner as they grow and welcome and new person into the world.
I hope that every midwife never forgets that for the family she is attending, this is a most special and important experience and never to lose the wonder of the time.
#midwifery#student midwife#midwife#pregnancy#pregnant#womens health#birth#labour#antenatal#postnatal#heart#heartsofhealth#idm2016
10 notes
·
View notes