#diabetes technology
Text
Diabetes in Young Adults: Causes and Solutions
Addressing the rise of diabetes in young adults requires comprehensive strategies that promote healthy lifestyle choices, including regular physical activity, balanced nutrition, stress management, and increased awareness of diabetes risk factors.
Additionally, early detection through regular screenings and improved access to healthcare can help identify and manage diabetes at an earlier stage,…

View On WordPress
#blood sugar control#blood sugar monitoring#diabetes#diabetes advocacy#diabetes awareness#diabetes community#diabetes complications#diabetes counseling#diabetes diagnosis#diabetes education#diabetes in adolescents#diabetes lifestyle#diabetes management#diabetes medications#diabetes prevention#diabetes research#diabetes resources#diabetes risk factors#diabetes support#diabetes symptoms#diabetes technology#diabetes treatment#exercise for diabetes#family history of diabetes#gestational diabetes#glucose metabolism#glucose monitoring#healthy diet#healthy habits#healthy lifestyle
0 notes
Text
Embracing Time in Range: A Personal Journey to Managing Diabetes
Living with diabetes is a constant balancing act. It requires careful monitoring of blood glucose levels, making dietary choices, taking medications, and maintaining an active lifestyle. One crucial aspect is making informed decisions on the basis of your glucose data. In this article, I will share my personal experiences with Continuous Glucose Monitoring device data, including Time in Range…

View On WordPress
#blood glucose control#blood sugar management#Diabetes#diabetes control#Diabetes Diet#diabetes education#diabetes exercise#diabetes management#diabetes story#diabetes technology#personal journey#time in range (TIR)#type 1 diabetes#type 2 diabetes
0 notes
Text
Delving into the Nexus of Mental Health and Diabetes: Unpacking the Psychological Quagmire of Long-Term Illness Management
Dive deep into a holistic examination of the intricate emotional repercussions arising from diabetes management. From the taxing phenomenon of diabetes burnout to the often-underestimated specters of anxiety and depression, this article sheds light on coping techniques, the indispensable role of community and familial support, and the symbiotic relationship between diabetes enlightenment and…

View On WordPress
#anxiety and diabetes#Blood Sugar Fluctuations#caregiver support#chronic disease#community support#depression#diabetes burnout#diabetes education#Diabetes Management#diabetes technology#emotional support#emotional well-being#family role in diabetes#hyperglycemia#hypoglycemia#lifestyle balance#Mental Health#mindfulness practices#physical health#psychological challenges#resilience#self-advocacy#sleep disturbances#Social Support#stigma
0 notes
Link
Advances in Diabetes Management - Digital Tools - Diabetes Knowledge
#CGM#Continuous Glucose Monitors#Diabetes Technology#Digital Tools for Diabetes#insulin pumps#new diabetes technology
0 notes
Text
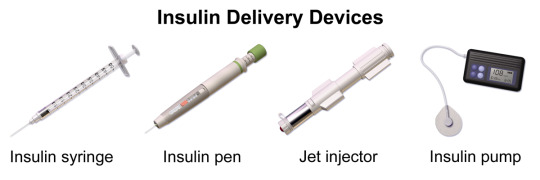
Insulin (medication)
#insulin#insulin delivery devices#wikipedia#wikipedia pictures#medicine#medcore#medicalcore#medicore#medical#tech#technology#techcore#technologycore#medical devices#diabetes mellitus#type 1 diabetes#type 2 diabetes#diabetes#insulin pump#insulin pen#insulin injection#syringe#jet injector
70 notes
·
View notes
Text
One of the things that's actually funny is that I have been eating SO MUCH more sugar (and carbs in general) since I did finally get appropriate treatment, with the supplemental insulin I've needed since at least 2008.
It's extra fun when you already have an ED history, and get plunged into that "you're obviously slowly killing yourself with knife and fork, but what would anyone expect from a lazy fat American?" mentality. Coming not least from the people who are supposed to be helping. The ED brainweasels were certainly having a party for too long, and I probably did my system some extra damage with restriction and overexertion. Whatever I did, it was not going to fix my fucked-up pancreas--and things just kept getting worse as more and more beta cells gradually died off.
I still have to nope right away from too many legit triggering conversations even among people with known autoimmune diabetes. No damned wonder we have like a 30% rate of diagnosable EDs, even on the "I did nothing to cause this, HONEST" autoimmune side of things. (I don't even need to get started on the misplaced Type Wars hierarchical BS again. Pisses me off even worse, as someone who nearly got killed by ending up on the "wrong" side of some terrible assumptions for way too long.)
And that 30% is mostly among people who did not already have disordered eating behavior (or significant scrupulosity problems) going in. It's positively encouraged--again, not least among professionals who are supposed to be helping. While being one of the fastest ways to cause your body serious mischief, especially once you throw supplemental insulin into the mix. If I am never exposed to another word about intermittent fasting or obsessive focus on carb counting with a moralistic tone, it will be way too soon.
Thankfully I have yet to hear one single goddamned word that's not genuinely medically appropriate about my weight or presumed eating habits since I did have that spectacular collapse, and then got to be clinically underweight enough that they have been repeatedly commenting on that--between the mistreated diabetes itself and the resulting GI damage from that final ketoacidosis crash. Regaining some weight and actually feeling hungry again more often, as I keep recovering from that bullshit and am consistently physically able to eat solid food again, has been sort of doing my head in lately. Not least because I do not want to get treated like garbage again, as I do recover and get back to a healthier weight. I have seen how that works, and really do not need a repeat.
There's still too much that's kinda triggering on an ongoing basis, but at least I am quite deliberately telling myself that I can eat whatever the hell I want and mostly actually DOING it. I am now decently equipped with insulin and a CGM to watch my blood sugar levels, and the world is my smörgåsbord at least as much as it is anyone else's.
I may actually go and get some ice cream in a little while. Because I want it, and I do have the technology.
#personal#venting#diabetes#disordered eating#eating disorders#scapegoating#look out honey csuse i'm using technology#medical fuckery#scrupulosity#my immune system is trying to kill me#weight mention#unintentional weight loss#medical fatphobia#alcohol mention
16 notes
·
View notes
Text
Hey could someone do me a favor and tell me exactly how my blood sugar was "so low" last night and this morning that my Dexcom kept waking me up with those terrifying URGENT LOW alarms (that I mostly just ignored and didn't treat because I felt absolutely fine), but now that I'm up and moving around (without eating), the sensor is reading in the low 200s?
(I don't sleep on my sensor, so it's not compression lows. Maybe just lack-of-blood-flow lows or let's-fuck-with-her-lol lows.)
#Dexcom#G7#t1d#Diabetes problems#I love this fucking CGM but technology sucks#Gotta remember that#First and foremost#Technology sucks
4 notes
·
View notes
Text
An implantable device could enable injection-free control of diabetes
The device contains encapsulated cells that produce insulin, plus a tiny oxygen-producing factory that keeps the cells healthy.
Anne Trafton | MIT News

One promising approach to treating Type 1 diabetes is implanting pancreatic islet cells that can produce insulin when needed, which can free patients from giving themselves frequent insulin injections. However, one major obstacle to this approach is that once the cells are implanted, they eventually run out of oxygen and stop producing insulin.
To overcome that hurdle, MIT engineers have designed a new implantable device that not only carries hundreds of thousands of insulin-producing islet cells, but also has its own on-board oxygen factory, which generates oxygen by splitting water vapor found in the body.
The researchers showed that when implanted into diabetic mice, this device could keep the mice’s blood glucose levels stable for at least a month. The researchers now hope to create a larger version of the device, about the size of a stick of chewing gum, that could eventually be tested in people with Type 1 diabetes.
“You can think of this as a living medical device that is made from human cells that secrete insulin, along with an electronic life support-system. We’re excited by the progress so far, and we really are optimistic that this technology could end up helping patients,” says Daniel Anderson, a professor in MIT’s Department of Chemical Engineering, a member of MIT’s Koch Institute for Integrative Cancer Research and Institute for Medical Engineering and Science (IMES), and the senior author of the study.
While the researchers’ main focus is on diabetes treatment, they say that this kind of device could also be adapted to treat other diseases that require repeated delivery of therapeutic proteins.
MIT Research Scientist Siddharth Krishnan is the lead author of the paper, which appears today in the Proceedings of the National Academy of Sciences. The research team also includes several other researchers from MIT, including Robert Langer, the David H. Koch Institute Professor at MIT and a member of the Koch Institute, as well as researchers from Boston Children’s Hospital.
Replacing injections
Most patients with Type 1 diabetes have to monitor their blood glucose levels carefully and inject themselves with insulin at least once a day. However, this process doesn’t replicate the body’s natural ability to control blood glucose levels.
“The vast majority of diabetics that are insulin-dependent are injecting themselves with insulin, and doing their very best, but they do not have healthy blood sugar levels,” Anderson says. “If you look at their blood sugar levels, even for people that are very dedicated to being careful, they just can’t match what a living pancreas can do.”
A better alternative would be to transplant cells that produce insulin whenever they detect surges in the patient’s blood glucose levels. Some diabetes patients have received transplanted islet cells from human cadavers, which can achieve long-term control of diabetes; however, these patients have to take immunosuppressive drugs to prevent their body from rejecting the implanted cells.
More recently, researchers have shown similar success with islet cells derived from stem cells, but patients who receive those cells also need to take immunosuppressive drugs.
Another possibility, which could prevent the need for immunosuppressive drugs, is to encapsulate the transplanted cells within a flexible device that protects the cells from the immune system. However, finding a reliable oxygen supply for these encapsulated cells has proven challenging.
Some experimental devices, including one that has been tested in clinical trials, feature an oxygen chamber that can supply the cells, but this chamber needs to be reloaded periodically. Other researchers have developed implants that include chemical reagents that can generate oxygen, but these also run out eventually.
The MIT team took a different approach that could potentially generate oxygen indefinitely, by splitting water. This is done using a proton-exchange membrane — a technology originally deployed to generate hydrogen in fuel cells — located within the device. This membrane can split water vapor (found abundantly in the body) into hydrogen, which diffuses harmlessly away, and oxygen, which goes into a storage chamber that feeds the islet cells through a thin, oxygen-permeable membrane.
A significant advantage of this approach is that it does not require any wires or batteries. Splitting this water vapor requires a small voltage (about 2 volts), which is generated using a phenomenon known as resonant inductive coupling. A tuned magnetic coil located outside the body transmits power to a small, flexible antenna within the device, allowing for wireless power transfer. It does require an external coil, which the researchers anticipate could be worn as a patch on the patient’s skin.
Drugs on demand
After building their device, which is about the size of a U.S. quarter, the researchers tested it in diabetic mice. One group of mice received the device with the oxygen-generating, water-splitting membrane, while the other received a device that contained islet cells without any supplemental oxygen. The devices were implanted just under the skin, in mice with fully functional immune systems.
The researchers found that mice implanted with the oxygen-generating device were able to maintain normal blood glucose levels, comparable to healthy animals. However, mice that received the nonoxygenated device became hyperglycemic (with elevated blood sugar) within about two weeks.
Typically when any kind of medical device is implanted in the body, attack by the immune system leads to a buildup of scar tissue called fibrosis, which can reduce the devices’ effectiveness. This kind of scar tissue did form around the implants used in this study, but the device’s success in controlling blood glucose levels suggests that insulin was still able to diffuse out of the device, and glucose into it.
This approach could also be used to deliver cells that produce other types of therapeutic proteins that need to be given over long periods of time. In this study, the researchers showed that the device could also keep alive cells that produce erythropoietin, a protein that stimulates red blood cell production.
“We’re optimistic that it will be possible to make living medical devices that can reside in the body and produce drugs as needed,” Anderson says. “There are a variety of diseases where patients need to take proteins exogenously, sometimes very frequently. If we can replace the need for infusions every other week with a single implant that can act for a long time, I think that could really help a lot of patients.”
The researchers now plan to adapt the device for testing in larger animals and eventually humans. For human use, they hope to develop an implant that would be about the size of a stick of chewing gum. They also plan to test whether the device can remain in the body for longer periods of time.
“The materials we’ve used are inherently stable and long-lived, so I think that kind of long-term operation is within the realm of possibility, and that’s what we’re working on,” Krishnan says.
“We are very excited about these findings, which we believe could provide a whole new way of someday treating diabetes and possibly other diseases,” Langer adds.
The research was funded by JDRF, the Leona M. and Harry B. Helmsley Charitable Trust, and the National Institute of Biomedical Imaging and Bioengineering at the National Institutes of Health.
Make sure to follow us on Tumblr!
5 notes
·
View notes
Text
There's a pilot project in this hospital for a touch-screen TV at every bed that has all kinds of apps to play games, browse the web, watch streaming platforms, and use social media. It's free!
It has a link to a survey to fill out about one's stay and experience as well as a link to the hospital's website for whatever info one may need (compliments/complaints possibly.)
There is also a link to a dictionary of medical terminology so that patients can be informed about their care in case they forget to ask their doctor what something means when the doctor forgets to explain. Which happens a lot lol.
Oh! I can do video calls from it and it has a reading light!!!
Edit: It's called myHealthHub and it is Canadian.
3 notes
·
View notes
Text
Scientists Have Reached a Key Milestone in Learning How to Reverse Aging
Loss of epigenetic information as a cause of mammalian aging
Scientists Have Reached a Key Milestone in Learning How to Reverse Aging
Highlights from the Study
Cellular responses to double-stranded DNA breaks erode the epigenetic landscape
This loss of epigenetic information accelerates the hallmarks of aging
These changes are reversible by epigenetic reprogramming
By manipulating the epigenome, aging can be driven forward and backward
“Underlying aging is information that is lost in cells, not just the accumulation of damage,” says Dr. David Sinclair, a professor of genetics and co-director of the Paul F. Glenn Center for Biology of Aging Research at Harvard Medical School. His latest results seem to support that theory.
All living things experience entropy manifested as a loss of genetic and epigenetic information. Genetic information is the hardware and the epigenome is the software. We think aging is due to corrupted software, that can be rebooted to restore youth.
It’s similar to the way software programs operate off hardware, but sometimes become corrupt and need a reboot. But by showing that we can reverse the aging process, that shows that the system is intact, that there is a backup copy and the software needs to be rebooted.”
In the mice, he and his team developed a way to reboot cells to restart the backup copy of epigenetic instructions, essentially erasing the corrupted signals that put the cells on the path toward aging. They mimicked the effects of aging on the epigenome by introducing breaks in the DNA of young mice. - Once “aged” in this way, within a matter of weeks Sinclair saw that the mice began to show signs of older age—including grey fur, lower body weight despite unaltered diet, reduced activity, and increased frailty.
The rebooting came in the form of a gene therapy involving three genes that instruct cells to reprogram themselves— These genes came from the suite of so-called Yamanaka stem cells factors—a set of four genes that Nobel scientist Shinya Yamanaka in 2006 discovered can turn back the clock on adult cells to their embryonic, stem cell state so they can start their development, or differentiation process, all over again. Sinclair didn’t want to completely erase the cells’ epigenetic history, just reboot it enough to reset the epigenetic instructions. Using three of the four factors turned back the clock about 57%, enough to make the mice youthful again.
Using a system called “ICE” (Inducible Changes to the Epigenome), we show the act of repairing DNA breaks accelerates aging at the physiological, cognitive, & molecular levels, including erosion of the epigenetic landscape, loss of cell identity, senescence & increased epi-age ... "We show these changes can be reversed by OSK-mediated rejuvenation. With an ability to drive aging in both the forward and reverse directions, we conclude that loss of epigenetic information is a cause of aging in mammals."
“We haven’t found a cell type yet that we can’t age forward and backward.”
In 2020, Sinclair reported that in mice, the process restored vision in older animals; the current results show that the system can apply to not just one tissue or organ, but the entire animal. He anticipates eye diseases will be the first condition used to test this aging reversal in people, since the gene therapy can be injected directly into the eye area.
"If correct, it means that cancer, diabetes and Alzheimer's might have the same underlying cause that can be reversed to treat or cure age-related conditions with a single treatment. Experiments in the lab are testing this."
Even before that happens, the process could be an important new tool for researchers studying these diseases.
"The age-reversal technology -- virally-delivered genes (Oct4, Sox2, Klf4, aka, Yamanaka factors), which turn on an embryonic program -- is being tested at @lifebiosciences in non-human primates. Results out in a few months from Bruce Ksander's lab & http://lifebiosciences.com"
#age reversal technology#dr david sinclair#aging#alzheimers#diabetes#diabetic#technology#blindness#cancer#harvard#genetics#biology#Inducible Changes to the Epigenome#STEM#science#epigenome#entropy#epigentic entropy#reprogramming#DNA#DNA damage#DNA loss#harvard medical school#eye disease#genetic#epigenetic#shinya yamanaka#stem cells#mammalian#mammals
2 notes
·
View notes
Text

Don't allow diabetes prevent you from living a fulfilling life.
Join forces to combat diabetes on this World Diabetes Day.
Because there are no guarantees in life, it's crucial to keep in mind that each moment deserves to be appreciated.
Regard yourself with care this 𝐖𝐨𝐫𝐥𝐝 𝐃𝐢𝐚𝐛𝐞𝐭𝐞𝐬 𝐃𝐚𝐲.
2 notes
·
View notes
Text
Understanding the Differences and Similarities Between Type 1 and Type 2 Diabetes
Introduction: Diabetes is a chronic condition characterized by elevated blood sugar levels, affecting millions of people worldwide. While both Type 1 and Type 2 diabetes share the commonality of high blood sugar, they are distinct conditions with unique causes, risk factors, and treatment approaches. In this blog, we'll delve into the differences and similarities between Type 1 and Type 2 diabetes, providing insight into these complex conditions.
Type 1 Diabetes: The Role of Autoimmunity Type 1 diabetes, formerly known as juvenile diabetes or insulin-dependent diabetes, is an autoimmune condition in which the body's immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, individuals with Type 1 diabetes are unable to produce insulin, the hormone responsible for regulating blood sugar levels. This necessitates lifelong insulin therapy to manage blood sugar and prevent complications.
Key Characteristics of Type 1 Diabetes:
Typically diagnosed in childhood or adolescence, but can occur at any age.
Requires insulin therapy for survival.
Cannot be prevented.
Risk factors may include genetic predisposition and environmental triggers.
Accounts for approximately 5-10% of all diagnosed cases of diabetes.
Type 2 Diabetes: Insulin Resistance and Lifestyle Factors Type 2 diabetes, on the other hand, is characterized by insulin resistance, where the body's cells become less responsive to insulin's effects. This results in elevated blood sugar levels, as the body struggles to regulate glucose uptake and utilization. While genetics play a role in Type 2 diabetes, lifestyle factors such as poor diet, sedentary lifestyle, obesity, and aging also contribute to its development.
Key Characteristics of Type 2 Diabetes:
Typically diagnosed in adulthood, but increasingly seen in children and adolescents.
May initially be managed with lifestyle modifications, including diet and exercise.
Oral medications and/or insulin therapy may be required as the disease progresses.
Can often be prevented or delayed through healthy lifestyle choices.
Accounts for the majority of diagnosed cases of diabetes worldwide.
Shared Challenges and Complications: Despite their distinct causes and mechanisms, both Type 1 and Type 2 diabetes share common challenges and complications. These may include:
Elevated blood sugar levels leading to complications such as heart disease, stroke, kidney disease, nerve damage, and vision problems.
The need for frequent monitoring of blood sugar levels, medication management, and lifestyle modifications.
The potential for hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar) episodes, requiring prompt intervention and management.
The importance of ongoing education, support, and self-care to prevent complications and maintain overall health and well-being.
Empowering Individuals Living with Diabetes: Whether Type 1 or Type 2, receiving a diabetes diagnosis can feel overwhelming. However, with proper education, support, and self-management strategies, individuals with diabetes can lead full and active lives. By working closely with healthcare providers, adopting healthy lifestyle habits, and staying proactive in managing their condition, individuals with diabetes can minimize complications, optimize blood sugar control, and thrive.
Conclusion: Type 1 and Type 2 diabetes are distinct conditions with unique characteristics, yet they share common challenges and complications. Understanding the differences between these two types of diabetes is essential for effective management and treatment. By raising awareness, promoting education, and fostering a supportive community, we can empower individuals living with diabetes to take control of their health, embrace self-care, and live life to the fullest.
0 notes
Text
Pioneering muscle monitoring in space to help astronauts stay strong in low-gravity - Technology Org
New Post has been published on https://thedigitalinsider.com/pioneering-muscle-monitoring-in-space-to-help-astronauts-stay-strong-in-low-gravity-technology-org/
Pioneering muscle monitoring in space to help astronauts stay strong in low-gravity - Technology Org
Astronauts have been able to track their muscle health in spaceflight for the first time using a handheld device, revealing which muscles are most at risk of weakening in low gravity conditions.
NASA astronaut using the Advanced Resistive Exercise Device (ARED) onboard the ISS. Credit NASA
An international research team, including the University of Southampton and led by Charité University in Berlin, monitored the muscle health of twelve astronauts before, during and after a stay on the International Space Station (ISS).
Findings published in Nature Scientific Reports indicate that the astronauts’ daily exercise regime was effective in preserving most muscle groups, but crucial lower leg muscles showed signs of deterioration.
The technology and assessment protocol used in space could also bring about a step-change in healthcare back on Earth, allowing healthcare professionals to better monitor muscle health in neuro-musculoskeletal conditions, such as Parkinson’s Disease and stroke, and in patients in critical care.
“Being able to perform inflight muscle health checks will allow the astronauts to see which muscles are losing strength and adjust their exercise programme accordingly,” says Professor Maria Stokes OBE, UK lead of the project, from the School of Health Sciences at the University of Southampton. “Being able to personalise exercises like this will be crucial on future long-duration missions to the Moon and Mars.”
Muscle loss in space
Microgravity conditions during spaceflight mean astronauts’ bodies aren’t subjected to the workload they are used to on Earth, meaning muscles don’t have to work very hard to perform functional tasks onboard the spacecraft. This puts astronauts at risk of muscle weakness and bone loss, with up to a 20 per cent decrease in skeletal muscle mass over a month.
To counteract this, astronauts onboard the ISS perform an exercise programme for around two hours a day, six or seven days a week. Until now, monitoring the effectiveness of this programme has only been possible with pre- and post-flight checks due to a lack of appropriate equipment.
Handheld device
The MyotonPRO is a smartphone-sized device which measures the properties of superficial skeletal muscles, tendons, ligaments, adipose tissue (fat), and skin. It’s non-invasive and uses a ‘tap and listen’ method, sending a precision impulse causing the tissues to oscillate and recording the way the tissue responds to compute various characteristics, such as stiffness, tone and elasticity.
The device was used to measure specific points on the astronauts’ bodies throughout their mission, before the flight, during a 4 to 11-month stay onboard the ISS, and up to three months post-flight. Researchers were particularly interested in measuring passive muscle stiffness, as it reflects muscle strength, which is not possible to measure in multiple muscles in space.
“People tend to associate stiffness with poor flexibility and mobility, but an adequate degree of passive stiffness is needed to maintain joint stability and posture,” says co-lead author Paul Muckelt, a research fellow at the University of Southampton. “Stiffness provides support during movement, preventing excessive stretching of muscles and reducing the risk of injury. It also contributes to the efficiency of movement by storing and releasing elastic energy during activities, such as walking or running.”
Passive muscle stiffness can shift throughout the day, so recording conditions needed to be standardised to ensure accuracy.
Weakening of crucial leg muscles
The team found that the astronauts’ exercise programme was effective in preserving muscle stiffness in most sites measured, including the shoulders, neck, back and thigh. But crucially, the tibialis anterior showed signs of waning in all 12 astronauts. The tibialis anterior, located in the front of the lower leg, lifts the foot upwards towards the shin. This movement is essential for walking and running.
The soleus and gastrocnemius muscles in the calf act in opposition to the tibialis anterior, pointing the foot downward. The soleus also showed a decrease in stiffness compared to preflight, but it did increase gradually over time on the ISS. The gastrocnemius increased in stiffness, indicating it might take over most of the function of the calf.
The Achilles tendon (attached to both muscles) also decreased in stiffness compared to preflight measurements. Monitoring the Achilles is important as sudden reloading, such as that induced by a change in gravitation force, could result in injury or even rupture.
Professor Dieter Blottner at the Charité -Universitätsmedizin Berlin, Germany, who led the Myotones Project said: “These lower leg muscles have a vital role in gait and ankle joint stabilisation. Impaired function could hinder performance on missions during planetary excursions and risk injury on return to Earth’s gravity, so exercises which target these muscles should be included in the astronauts’ exercise regimes going forward.”
Use on Earth
Measuring muscle health in this relatively simple way in space could translate to everyday life back on Earth – in healthcare settings, sports, remote communities and even people’s homes.
Assessing stiffness and other muscle characteristics helps in managing neurological disorders, like Parkinson’s disease and stroke. Currently, clinical assessments involve subjective methods, rating stiffness as mild, moderate or severe.
MyotonPRO offers objective measurements for a more accurate and sensitive assessment of the effects of different treatments. In the future, devices like this could be used by patients to monitor drug effects at home, akin to self-testing blood in diabetes.
Dr Martin Warner, co-senior author of the research paper from the University of Southampton said: “This technology and the use of passive muscle stiffness as a muscle health indicator could be used by many health professionals during clinical assessments. Widespread uptake could revolutionise healthcare in neuro-musculoskeletal, critical care and geriatric medicine, rehabilitation and precision medicine.”
Libby Moxon, Exploration Science Officer for Lunar and Microgravity at the UK Space Agency (UKSA), said: “As we approach increasingly ambitious missions that will see us travel deeper into space for longer, it’s imperative we fully understand how space travel impacts human muscle properties, so we can protect astronauts’ muscle health on long-duration missions.
“The University of Southampton’s fascinating research, supported by the UK Space Agency, demonstrates how innovative technology can support this goal, taking advantage of the microgravity environment to provide insights that will also help improve healthcare in space and back on Earth.”
Muscle stiffness indicating mission crew health in space is published in the Nature journal Scientific Reports and is available online.
The study was funded through the UK Space Agency (UKSA), the German Aerospace Agency (DLR), the European Space Agency (ESA) and the Science Technology Facilities Council (STFC).
Source: University of Southampton
You can offer your link to a page which is relevant to the topic of this post.
#aerospace#approach#assessment#astronaut health#astronauts#berlin#blood#calf#change#Developments#devices#diabetes#Disease#disorders#drug#earth#effects#efficiency#energy#Environment#equipment#ESA#European Space Agency#Exercise#Facilities#fat#Featured life sciences news#Featured Space news#Featured technology news#flight
1 note
·
View note
Text
Headsets, Hackers and Health Tech Busts
This month’s episode of “News You Can Use” on HealthcareNOWRadio features news from the month of March 2024
News You Can Use with your Hosts Dr Craig Joseph and Dr Nick van Terheyden
The show that gives you a quick insight into the latest news, twists, turns and debacles going on in healthcare withmy friend and co-host Craig Joseph, MD (@CraigJoseph) Chief Medical Officer at Nordic Consulting…

View On WordPress
#apple vision pro#Ask Me Anything#book recommendation#change healthcare#diabetes management apps#Digital Health#digital health solutions#DigitalHealth#education#excel spreadsheets#Healthcare#healthcare data analytics#healthcare news#Healthcare Reform#Healthcare Security#Incremental#Incremental Healthcare#IncrementalHealth#Innovation#Medical Devices#News#ransomware attack#sci-fi novels#Security#Social Media#technology review#TheIncrementalist
0 notes
Text
Belly Button Exercises for Hernias Yes, Please! Gentle Moves to Strengthen Your Core and Minimize Bu
#health #herniarepair #hernia #surgery #medicalstudents #medicalprofessionals #DrAtefAhmed
#MedicalMystery #DoctorReacts #MentalHealthAwareness #ChronicIllness #HealthTips #Wellbeing #FitnessMotivation #MedicalSchool #Nutrition #HealthyLifestyle #DiseasePrevention #FirstAid #Anatomy #Healthcare #MedicalTechnology #PatientStories #DoctorLife #MedStudent
Atef’s Notes In Hernia for Medical…

View On WordPress
#AI in medicine#anxiety#cardiac surgery#clinical rotations#diabetes#endoscopy#gastrointestinal medicine#healthcare technology#hernia#infectious diseases#laparoscopy#medical ethics#medical school tips#medical specialties#minimally invasive surgery#neurology#Neurosurgery#oncology#orthopedic surgery#palliative care#patient communication#physician burnout#psychiatry#Public health#residency application#robotic surgery#schizophrenia#telemedicine#usmle prep
0 notes
Text

Insulin (medication)
#insulin#insulin injection#insulin pen#wikipedia#wikipedia pictures#medicine#medical#meds#med#medcore#medicalcore#medicore#tech#technology#pharmacore#diabetes#diabetes mellitus#type 1 diabetes#type 2 diabetes#gestational diabetes#medical care#injection#needles
22 notes
·
View notes